Published online Mar 14, 2024. doi: 10.3748/wjg.v30.i10.1358
Peer-review started: November 15, 2023
First decision: December 14, 2023
Revised: December 27, 2023
Accepted: January 31, 2024
Article in press: January 31, 2024
Published online: March 14, 2024
Processing time: 120 Days and 1.7 Hours
Percutaneous endoscopic gastrostomy (PEG) and laparoscopically inserted gastrostomy have become the gold standard for adult patients and children, respectively, requiring long-term enteral nutrition support. Procedure-related mortality is a rare event, often reported to be zero in smaller studies. National data on 30-d mortality and long-term survival rates after gastrostomy placement are scarce in the literature.
To study the use of gastrostomies in Sweden from 1998-2019 and to analyze procedure-related mortality and short-term (< 30 d) and long-term survival.
In this retrospective, population-based cohort study, individuals that had received a gastrostomy between 1998-2019 in Sweden were included. Individuals were identified in the Swedish National Patient Register, and survival analysis was possible by cross-referencing the Swedish Death Register. The cohort was divided into three age groups: Children (0-18 years); adults (19-64 years); and elderly (≥ 65 years). Kaplan-Meier with log-rank test and Cox regression were used for survival analysis.
In total 48682 individuals (52% males, average age 60.9 ± 25.3 years) were iden
The annual use of gastrostomies in Sweden increased during the study period, with a shift towards more minimally invasive procedures. Although procedure-related death was rare, the overall 30-d mortality rate was high (10%). To overcome this, we believe that patient selection should be improved.
Core Tip: In this large population-based cohort of 48682 individuals, the use of gastrostomies in Sweden increased during the 22-year study period, from 13.7/100000 to 22.3/100000 individuals. Percutaneous endoscopic gastrostomy more than doubled, while a 10-fold increase was seen in laparoscopic gastrostomies. Although the procedure-related mortality was low (0.1%), a 10% 30-d mortality was seen. The latter, however, decreased from 11.6% in 1998-2009 to 8.5% in 2010-2019. One-year and ten-year survival rates for children, adults, and elderly were 93.7%, 67.5%, and 42.1% and 79.9%, 39.2%, and 6.8%, respectively. The most common causes of death were malignancies and cardiovascular and respiratory diseases.
- Citation: Skogar ML, Sundbom M. Time trends and outcomes of gastrostomy placement in a Swedish national cohort over two decades. World J Gastroenterol 2024; 30(10): 1358-1367
- URL: https://www.wjgnet.com/1007-9327/full/v30/i10/1358.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i10.1358
In modern health care, gastrostomies play a crucial role in the management of patients that require long-term enteral nutrition support[1]. Dysphagia due to stroke, neurodegenerative diseases like Parkinson’s or Alzheimer’s, and head and neck cancers are among the most common indications[2]. A gastrostomy may also be placed for stomach decompression to resolve persistent nausea and vomiting (e.g., as a palliative procedure in patients with malignant bowel obstruction)[3].
The technique for placing a gastrostomy has evolved significantly over the years with several approaches available today. In 1980, percutaneous endoscopic gastrostomy (PEG) was introduced as a minimally invasive approach[4]. The low complication rates associated with PEG has led to widespread acceptance, making PEG the gold standard for enteral access in patients that require long-term enteral nutrition support[5]. Other available techniques include radiologically inserted gastrostomy and insertion by open surgery or laparoscopic surgery. Radiologically inserted gastrostomy, percutaneously placed under radiological guidance, is a good alternative when endoscopy is contraindicated (e.g., obstructing pharyngeal or esophageal cancer). Today, open surgical gastrostomy is mostly reserved for specific situations where endoscopic or radiological approaches are not feasible or during emergent surgery for stomach decompression. Finally, laparoscopically-inserted gastrostomy has become standard in children at many institutions because of less complications as compared to PEG in children[6,7].
Long-term survival and quality of life outcomes following gastrostomy have been the subject of extensive research. In short, gastrostomy has been associated with improved nutritional status, reduced hospitalizations[8], and enhanced overall quality of life[9] in patients that require long-term enteral nutrition support. Furthermore, studies have shown that timely gastrostomy placement is associated with improved survival rates and fewer complications when compared to delayed placement[10-12]. However, in patients with dementia, there is no evidence that enteral tube feeding improves survival or quality of life[13]. This underlines the importance of choosing the right indication to treat patients who actually benefit from a gastrostomy. In addition, a delayed intervention leads to loss of benefit and greater harm, which is illustrated by higher rates of morbidity and mortality[2].
This paper aimed to provide an overview of the use of gastrostomies in Sweden by studying the trends during the last two decades. In addition, we analyzed data pertaining to procedure-related mortality as well as short-term (< 30 d) and long-term survival after a gastrostomy procedure. The purpose was to assist physicians in the risk-benefit assessment of a gastrostomy procedure in the clinical setting.
This retrospective population-based cohort study included all patients that had a gastrostomy between January 1, 1998 to December 31, 2019 in Sweden, according to the Swedish National Patient Register (NPR). NPR stores sex, age, name of hospital, admission and discharge dates, and principal and additional diagnoses on all inpatient care and outpatient visits at hospital-based clinics. Diagnoses and surgical procedures[14] are coded according to the Swedish version of the International Statistical Classification of Diseases and Related Health Problems (ICD)[15] with a validity of 85%-95% in general[16]. Data from NPR were cross matched with data from the Swedish Death Register, which added information about date of death and cause of death. All data was anonymized. The study was conducted in accordance with the ethical standards of the Helsinki Declaration.
Individuals were identified in the NPR by the codes for gastrostomy, i.e. JDB 00 (gastrostomy inserted by open surgery), JDB 01 (laparoscopically-inserted gastrostomy), and JDB 10 (PEG). Calculation of annual operative volumes per 100000 inhabitants was performed. For analysis of time trends, the cohort was halved into an early group (receiving gastrostomy in 1998-2009) and a late group (receiving gastrostomy in 2010-2019). The cohort was further divided into three age groups: Children (0-18 years); adults (19-64 years); and elderly (≥ 65 years).
The indication for gastrostomy was based on the principal ICD-10 diagnosis, or if not applicable (e.g., dysphagia-R13), indication was searched in the additional diagnoses at the time of gastrostomy. Indication was then grouped into four main categories: (1) Malignancy; (2) Neurological diseases; (3) Cerebrovascular lesions (CVL); and (4) Non-malignant gastrointestinal conditions (e.g., gastric, duodenal, or other bowel perforations, fixation of large hiatal hernias, bowel obstruction without concomitant gastrointestinal malignancies).
Procedure-related mortality was defined as having a surgical complication as the cause of death (ICD10-code: T80-T88) within 30 d. Short-term mortality was defined as death within 30 d, while long-term survival was analyzed until 10 years after the insertion of the gastrostomy.
Independent sample t test and χ2 test were used as univariate analyses for continuous and categorical variables, respectively. Kaplan-Meier with log-rank test was used for survival analyses. Multivariate adjusted survival analyses were performed using Cox regression, adjusting for differences in sex, age group, type of gastrostomy, and time period and presented as hazard ratios (HR) with 95% confidence intervals (CI). All P values were two-sided, and P < 0.05 was considered statistically significant. All analyses were done using IBM SPSS Statistics version 28.
In total, 48682 patients had a gastrostomy during the study period, with 23500 (48.3%) in the early time period. The cohort consisted of 52% males, and the average age was 60.9 ± 25.3 years. A population-based increase in the use of gastrostomies during the study period was observed, from 13.7/100000 to 22.3/100000 individuals (P < 0.001).
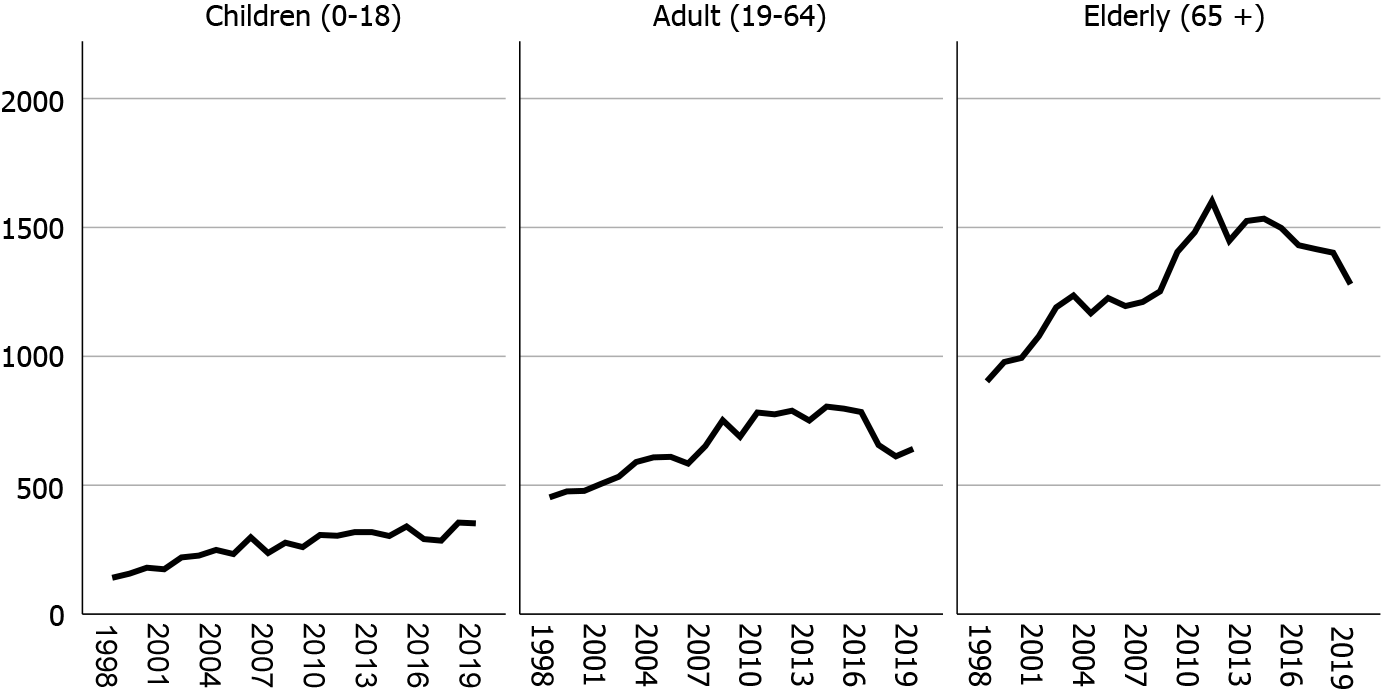
Children constituted 12.0% (n = 5828), adults 29.5% (n = 14340) and elderly 58.5% (n = 28483) of the cohort. In all three groups, the number of gastrostomies increased during the study period, from 6.1/100000 to 16.3/100000, from 7.1/100000 to 10.7/100000, and from 46.5/100000 to 62.5/100000, respectively. The total number of gastrostomies are demonstrated in Figure 1.
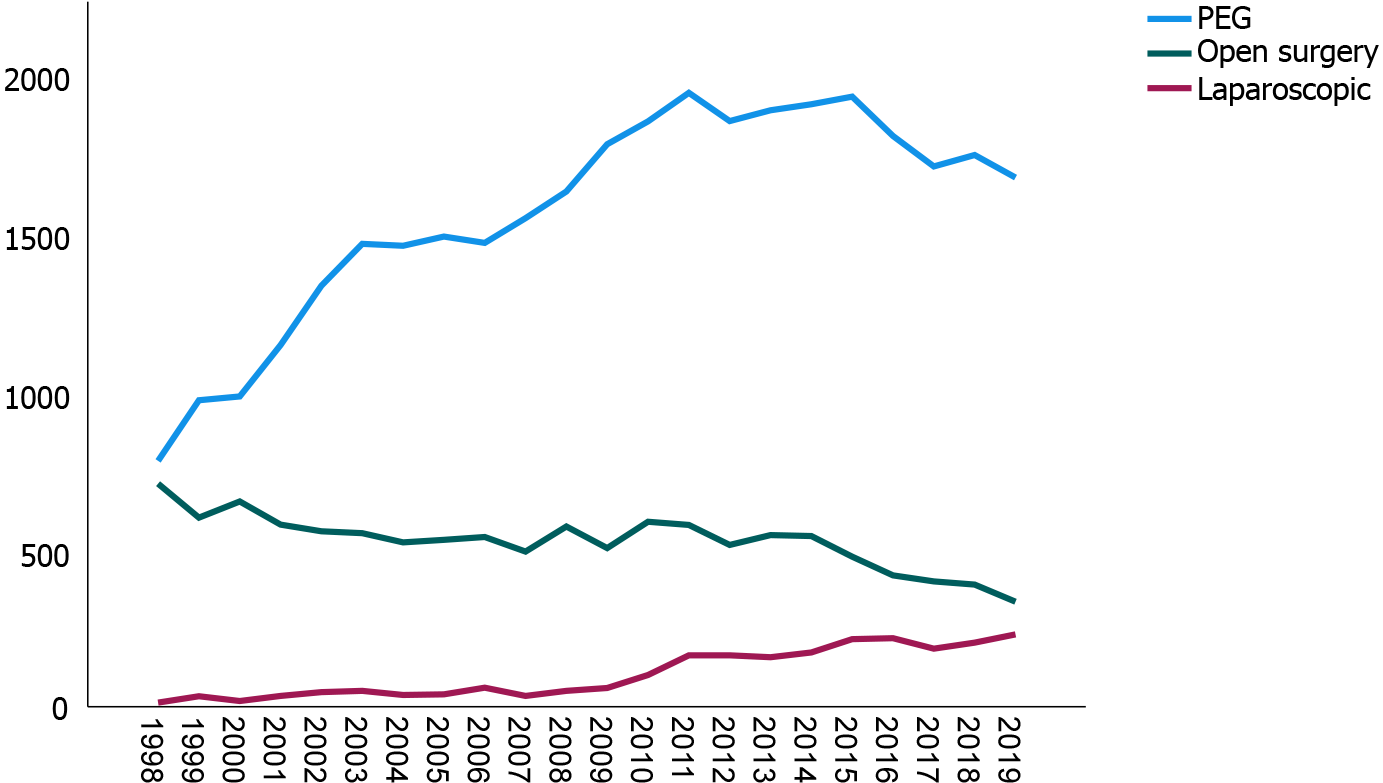
The technique used for placing the gastrostomy was PEG, open gastrostomy, and laparoscopic gastrostomy in 70.0% (n = 34060), 23.3% (n = 11336), and 4.9% (n = 2404), respectively. The remaining 1.8% (n = 882) were not specified in the register. During the study period, the use of PEG more than doubled (about 800 to 1800/year), with a corresponding decrease in open gastrostomy (about 700 to 340/year). Laparoscopic gastrostomy increased more than 10-fold (about 20 to 240/year). All changes were statistically significant (P < 0.001) (Figure 2).
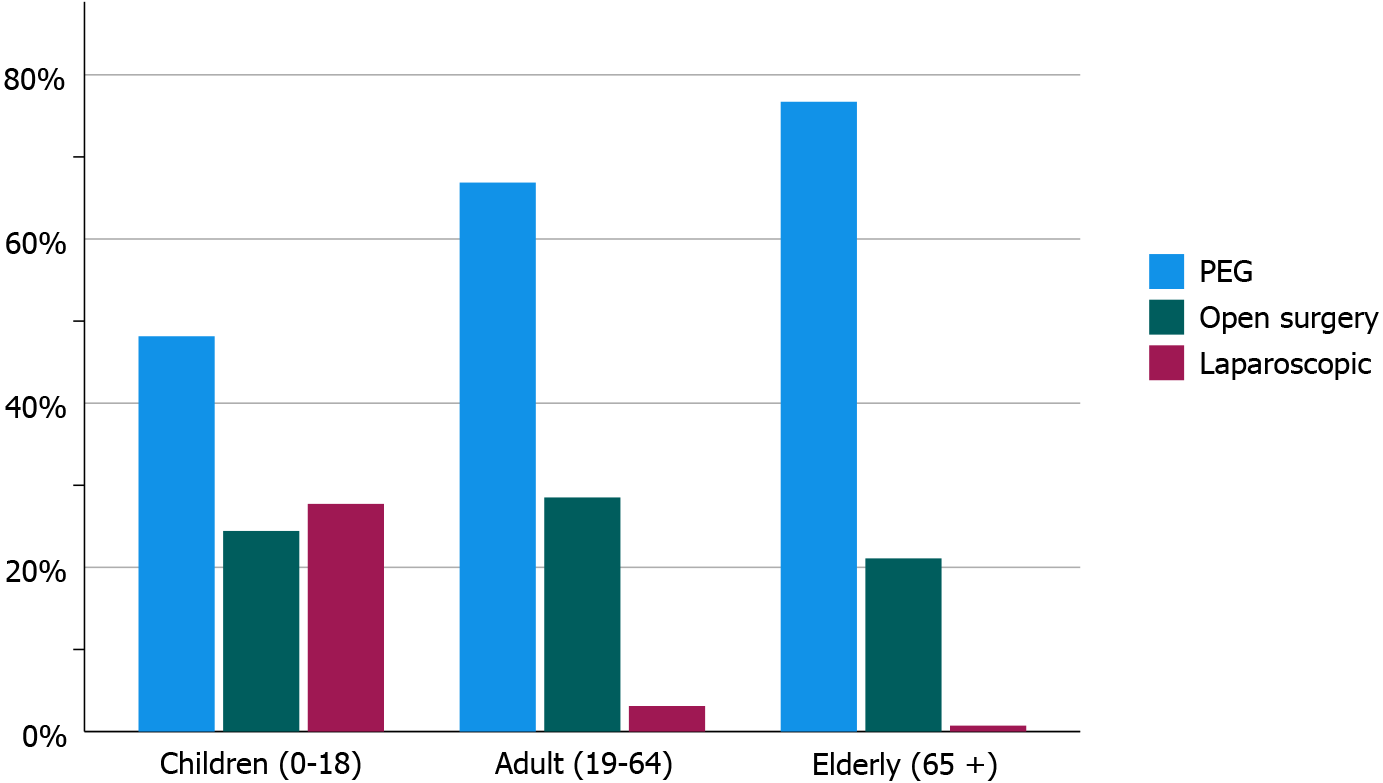
PEG was the most commonly used technique in all three age groups, followed by open surgery in adults and elderly. The gradual increase in laparoscopically-inserted gastrostomy made laparoscopic gastrostomy the second most common in children (Figure 3).
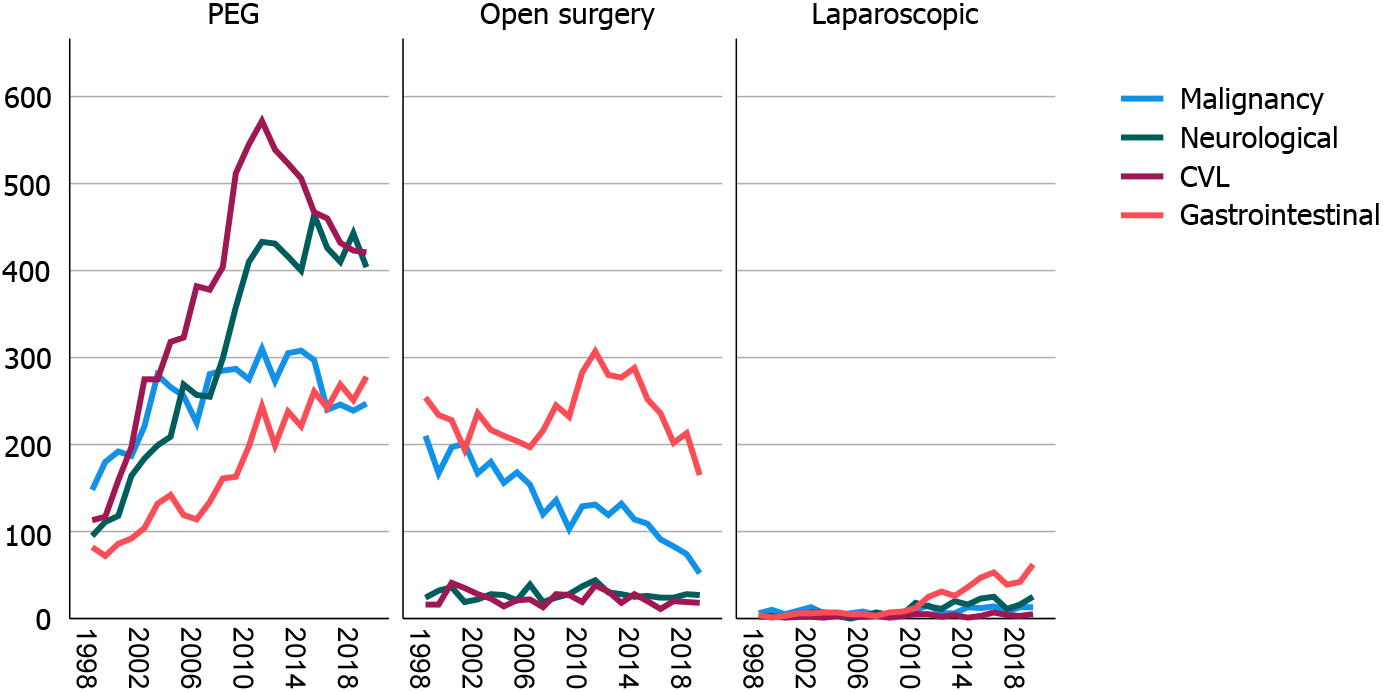
The most common indication for a gastrostomy was various non-malignant gastrointestinal conditions (19.7%), closely followed by CVL (18.9%), malignancies (18.7%), and neurological disorders (16.7%). The two most common individual diagnoses were stroke and neurodegenerative disorders, including amyotrophic lateral sclerosis (Table 1). As demonstrated in Figure 4, PEG dominated in CVL and neurological diseases, while the opposite was seen in non-malignant gastrointestinal conditions where open gastrostomy placement was predominantly used.
| Indication | Subgroup (ICD-10 codes) | n | % of total |
| Malignancy | 9103 | 18.7 | |
| Head and neck cancer (C00-C14) | 2670 | 5.5 | |
| Esophageal cancer (C15) | 1784 | 3.7 | |
| Other gastrointestinal malignancies (C16-C26) | 3539 | 7.3 | |
| Laryngeal cancer (C32-C33) | 469 | 1.0 | |
| Lung cancer (C34) | 384 | 0.8 | |
| Malignant brain tumors (C70-C72) | 257 | 0.5 | |
| Neurological diseases | 8129 | 16.7 | |
| Dementia (F00-F03) | 1251 | 2.6 | |
| Meningitis/encephalitis (G00-G07) | 147 | 0.3 | |
| Neurodegenerative disorders (G10-G37) | 3185 | 6.5 | |
| Amyotrophic lateral sclerosis (G12.2) | 2276 | 4.7 | |
| Neuromuscular disorders (G70-G73) | 349 | 0.7 | |
| Cerebral palsy (G80) | 921 | 0.9 | |
| Cerebrovascular lesions | 9196 | 18.9 | |
| Hemorrhagic or ischemic stroke (I60-I63) | 8263 | 17.0 | |
| Traumatic brain injury (S06) | 933 | 1.9 | |
| Non-malignant gastrointestinal conditions | 9588 | 19.7 | |
| Non-malignant diseases of the esophagus (K22) | 1318 | 2.7 | |
| Peptic ulcer with perforation (K25-K28) | 1560 | 3.2 | |
| Hiatal hernia (K44) | 596 | 1.2 | |
| Bowel obstruction (K56) | 1587 | 3.3 | |
| Other gastrointestinal diseases (e.g., bowel perforations, pancreatitis) | 4527 | 9.3 | |
| Other/missing | 12666 | 26.0 | |
| Total | 48682 | 100 | |
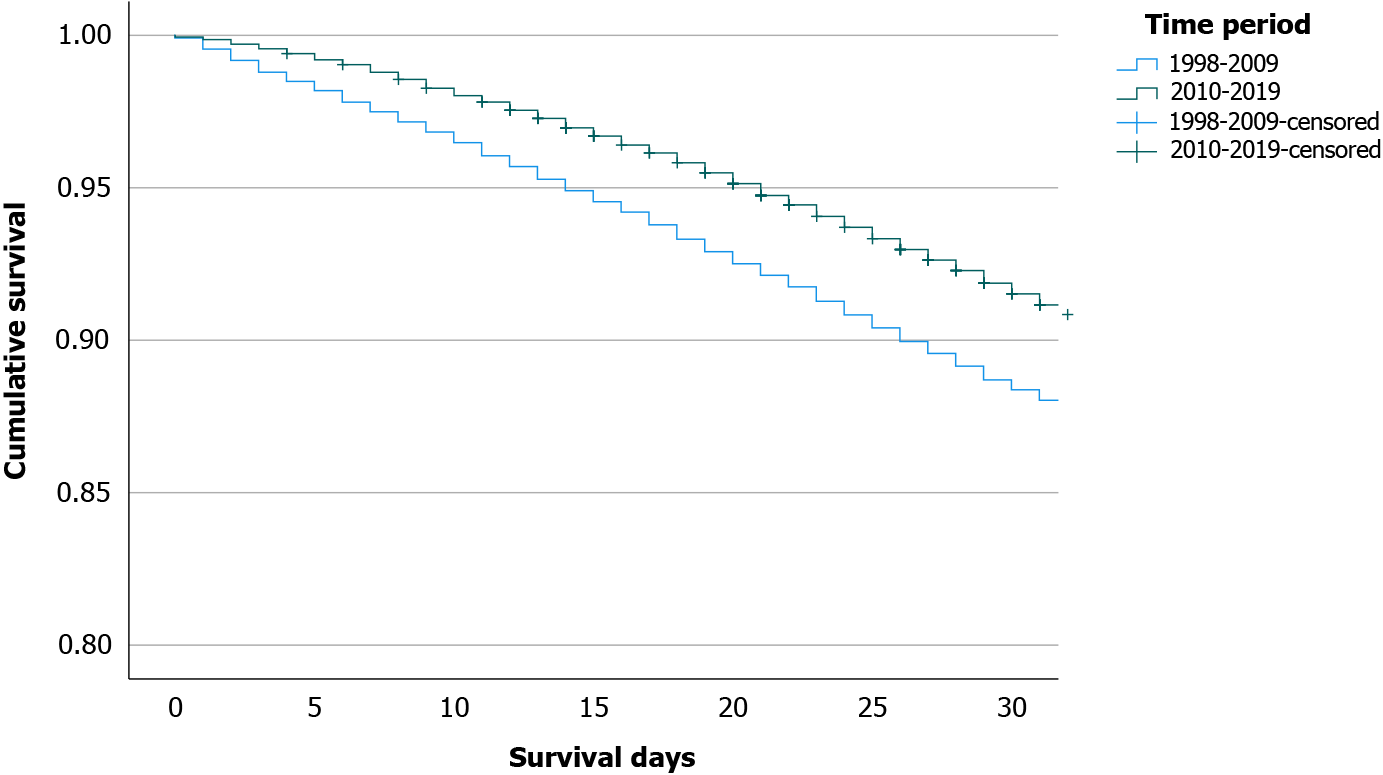
30-d mortality: The overall 30-d mortality rate was 10.0% (n = 4863), ranging from 0.3% (n = 17) in children to 6.2% (n = 883) in adults and 13.9% (n = 3962) in elderly. For the three different types of gastrostomies, the 30-d mortality was 9.8%, 12.4%, and 1.7% for PEG, open gastrostomy, and laparoscopic gastrostomy, respectively. The 30-d mortality during the early period was higher than during the late period (11.6% vs 8.5%, P < 0.001) (Figure 5).
Adjusted analysis (Cox regression) of differences in sex, time period, age group, and type of gastrostomy, identified male sex (HR = 1.11, 95%CI: 1.05-1.18), early time period (HR = 1.33, 95%CI: 1.26-1.41), open gastrostomy (HR = 1.44, 95%CI: 1.35-1.53), and belonging to the adult group (HR = 20.9, 95%CI: 12.7-34.4) or elderly group (HR = 50.2, 95%CI: 30.7-82.3) as risk factors for 30-d mortality (Supplementary Table 1).
Procedure-related mortality: In 44 patients (16 PEG, 27 open, and 1 laparoscopic) the primary cause of death was coded as directly related to a complication of the procedure, giving an overall procedure-related mortality of 0.1% (PEG: 0.05%, open: 0.24%, laparoscopic: 0.04%). The most common procedure-related death was bowel perforation (n = 16), followed by acute cardiovascular event (n = 9), acute respiratory failure (including aspiration and overdose of sedative drugs, n = 8), and gastrointestinal bleeding (n = 1). In the remaining 10 cases septicemia was coded as the secondary cause of death.
In an additional 141 patients, a procedure-related complication was judged to have contributed to the cause of death within 30 d. Thus, in 185 patients (0.4%), a procedure-related complication was either the direct cause of death or a contributing factor. This was more common among those that had undergone an open gastrostomy (0.9%, n = 102) compared to PEG (0.2%, n = 74) and laparoscopic gastrostomy (0.2%, n = 6, P < 0.001).
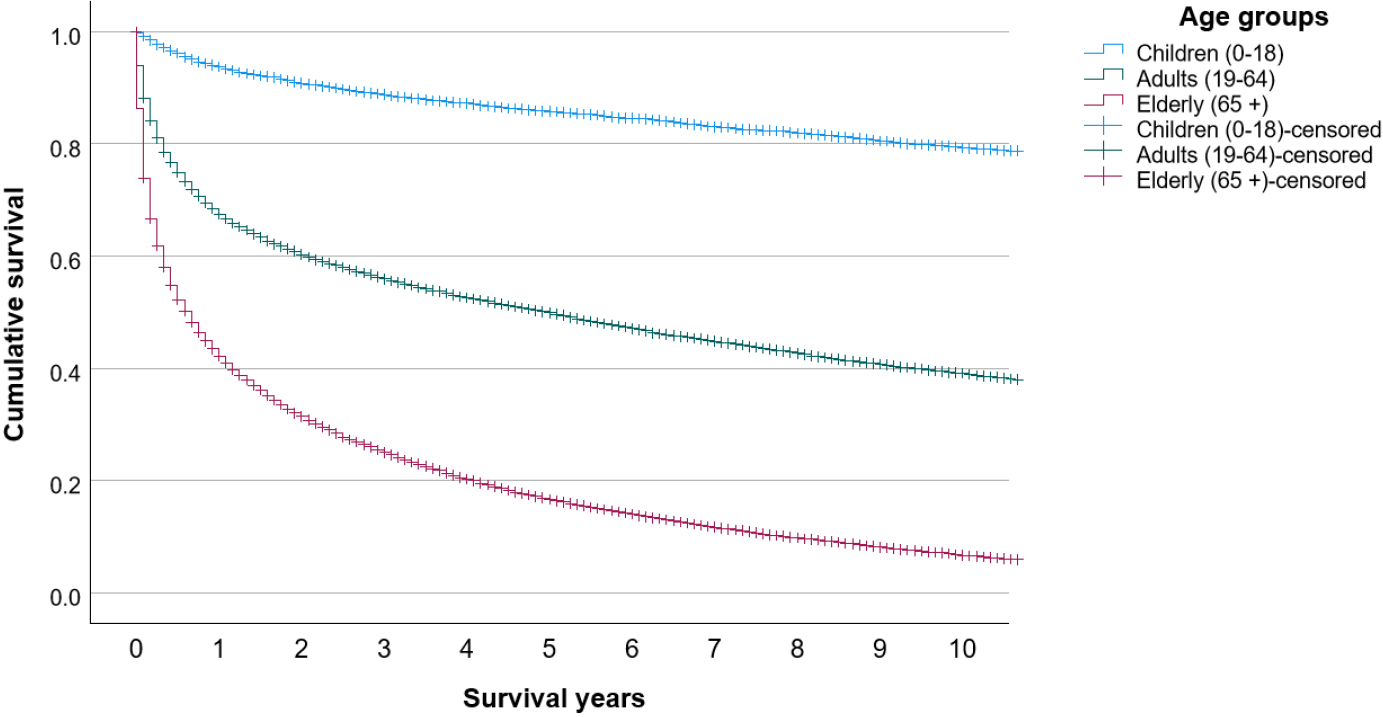
Long-term survival: During the mean observational time of 10.0 ± 6.1 years, 70% (n = 34055) of the patients had died after 21.9 ± 35.6 mo (on average) after receiving the gastrostomy. One-year and ten-year survival rates were 93.7%, 67.5%, and 42.1% and 79.9%, 39.2%, and 6.8% in children, adults, and elderly, respectively (Figure 6). The most common stated causes of death were malignancies (C00-D48, 24.4%), cardiovascular diseases (I00-I99, 23.1%), and respiratory conditions (J00-J99, 20.3%).
In this nationwide cohort study of 48682 individuals who received a gastrostomy from 1998-2019 in Sweden, an increased use of gastrostomies was seen, from 13.7/100000 to 22.3/100000 inhabitants. The increase was found in PEG and laparoscopically-inserted gastrostomy, while open gastrostomy was halved. We believe that this mirrors the international shift towards more minimally invasive procedures[17]. Very few studies have examined the number of gastrostomy placements in other countries, but the observed doubling of PEG is similar to the 2.5-fold increase observed in Poland from 2010-2020[18]. The United States experienced an exponential increase in PEG use from 1980-2000, resulting in more than 216000 annual PEGs[19]. Based on a population of about 280 million in 2000, this should correspond to 77/100000 inhabitants. However, the opposite trend has been described in Japan, where a decreased use of PEG has been observed since 2011[20], especially in patients aged 80 years and over. This has resulted in an increased use of total parenteral nutrition in home care. Stated reasons include changes in the health insurance system, reimbursement-related factors, and emotional and ethical barriers.
The most common indication for gastrostomy in the present study was various non-malignant gastrointestinal conditions (19.7%), closely followed by CVL (18.9%), malignancies (18.7%), and neurological disorders (16.7%). Neurological dysphagia is one of the most common indications for PEG tube insertion, and the incidence among stroke patients has been reported to be as high as 78%[21]. In our study, stroke (ischemic or hemorrhagic) was the most common subgroup (17%). In a prospectively collected case series of 1041 PEG patients in Germany, the most common indication was neurogenic dysphagia (43%), followed by cancer (37%)[22]. In the previously mentioned Polish PEG study[18], where indication was also based on ICD-10 codes, the most common indication was dysphagia and malnutrition (37.2%), which as the author states might have been a consequence of other diseases. The high proportion of non-malignant gas
Although gastrostomy tube placement, especially PEG, is considered a relatively safe surgical procedure, complications are common, which is likely due to greater frailty given an elderly population with multiple comorbidities. About one-third of PEG insertions result in minor complications, such as local wound infection, tube dislodgement, or peristomal leakage. Major complications, such as bowel or liver injuries, aspiration pneumonia, or major bleedings, are rare, affecting 2%-4% of the patients[23-26]. In this registry-based study, it was unfortunately not possible to explore the incidence of specific complications. However, in 0.1% (PEG: 0.05%, open: 0.24%, laparoscopic: 0.04%) a procedure-related complication was stated as the primary cause of death, and in 0.4% (PEG: 0.2%, open: 0.9%, laparoscopic: 0.2%) of the patients, a procedure-related complication was stated as a contributing factor to death within 30 d. Our large number of patients allowed for the detection of this rare event, which is often reported to be zero in smaller studies[22,26-28]. The fact that the majority of the procedure-related deaths occurred after an open gastrostomy is no surprise and likely explained by other concomitant surgical procedures as previously mentioned.
The 30-d mortality rates are difficult to compare between studies because of differences in indication, age, comorbidities, etc. Previous PEG studies reported a 30-d mortality of 3.3% (n = 302, Taiwan)[28], 3.9% (n = 388, Japan)[29], 6.5% (n = 168, Brazil and n = 787, Germany)[26,30], 13.0% (n = 277, Canada)[27], and 23.5% (n = 272, Israel)[31]. Our 30-d mortality rate of 9.8% in PEG patients was similar to these studies. Interestingly, the overall 30-d mortality decreased from 11.6% in the early time period (1998-2009) to 8.5% in the late time period (2010-2019). We hypothesize that the main driving factor was the shift towards the more minimally invasive techniques, PEG and laparoscopic gastrostomy. In addition to time period and open gastrostomy, older age and male sex was associated with an increased 30-d mortality. Due to the registry-based design, we were not able to verify other predictive factors, such as elevated C-reactive protein, anemia, previous intensive care admission, low albumin, high creatinine levels, malignancy, diabetes, heart failure, and low body mass index, found in other studies[23,26,27,29,30].
One of the first publications on laparoscopic gastrostomy in children was published in 1997[32], and the technique has since then been modified by Backman et al[33]. In a meta-analysis from 2018[6], it was found that PEG was associated with a significantly higher risk of major complications (odds ratio = 3.86, 95%CI: 1.90-7.81) compared to laparoscopic gastrostomy in a pediatric population. Therefore, it was stated that laparoscopic gastrostomy should be the preferred method in children. The adoption of the new modified technique for laparoscopic gastrostomy is mirrored in this study, where a clear increase was observed from 2010 on. Likely, it explains the 10-fold increase in laparoscopic gastrostomy procedures in Sweden during the study period.
Although procedure-related mortality was a rare event (0.1% overall), an observed 30-d mortality of 10% cannot be ignored. In the cases of patient deaths within 30 d of placement, the gastrostomy hardly benefited the patient. We believe these numbers are important to consider in the risk-benefit analysis when consulting patients before gastrostomy placement, especially in frail patients. However, we acknowledge the difficulties in deciding which patients will benefit from a gastrostomy. Indication, timing of the intervention, and ethical aspects are of importance. A recent Cochrane review found no evidence that enteral tube feeding improved survival or quality of life in patients with dementia[13]. However, in patients with amyotrophic lateral sclerosis, PEG placement was found to prolong survival if performed before the disease had become too advanced[34]. The present 42.1% 1-year survival in the elderly is very similar to the 38% reported from a systematic review of patients (> 65 years) receiving a PEG[35]. Thus, on a national level, our patient selection seems acceptable. In children, however, the situation is completely different, as almost 80% were alive at 10 years in this study.
The cause of death is often related to the underlying diseases[23], which we could confirm when comparing indication for gastrostomy and cause of death, e.g., malignancies (18.7% vs 24.4%) and cardiovascular diseases (17.0% stroke vs 23.1% overall cardiovascular death). Respiratory conditions were the third most common cause of death (20.3% of the overall mortality), likely because dysphagia (with the concomitant risk of aspiration pneumonia) was one of the main indications for gastrostomy.
The registry-based nature of this study was both a strength and a limiting factor. The registries made it possible to include all gastrostomies in Sweden with a 100% follow-up on survival time and cause of death since it is mandatory for physicians to register these data in the Swedish Death Register. However, the major limiting factor of this study was the impossibility of determining the indication for the gastrostomy since it was based on ICD-10 codes. Many patients had symptomatic diagnoses such as dysphagia (R13) as the principal diagnosis or a principal diagnosis was missing at the index occasion of gastrostomy. Despite efforts to find the indication among secondary diagnosis or at the occasion before gastrostomy, it was not possible to categorize 26% of the patients into one of the four main categories.
During the last two decades in Sweden, there has been a significant increase in the number of PEG and laparoscopically-inserted gastrostomies, while open gastrostomy has become less common. Although, procedure-related death was rare, the overall 30-d mortality rate was high (10%). One-year and ten-year survival rates were 93.7%, 67.5%, and 42.1% and 79.9%, 39.2%, and 6.8% in children, adults, and elderly, respectively. This study contributes robust survival data that can assist physicians in a risk-benefit assessment before gastrostomy placement, and we predict that the 30-d mortality should be lowered by selecting patients who actually benefit from a gastrostomy.
Placing a gastrostomy in patients requiring long-term nutritional support is standard care. Since the introduction of percutaneous endoscopic gastrostomy (PEG), there has been a continuous shift towards minimally invasive procedures. However, nationwide population-based data on the use of different techniques and overall outcomes is scarce.
As many patients are frail, the balance between risk and benefit is of particular importance. In the present nationwide population-based cohort, we could evaluate indication, choice of gastrostomy technique, complications, mortality, and time trends over two decades. The dissemination of such findings can lead to improved care.
To study the use of gastrostomies in clinical praxis concerning number and type of procedures (PEG, open gastrostomy, and laparoscopic gastrostomy) as well as indication (malignancy, neurological diseases, cerebrovascular lesions, and non-malignant gastrointestinal conditions). To analyze time trends concerning any shift between the three different methods, procedure-related mortality, and short-term mortality (within 30 d). To explore long-term survival up until 10 years after gastrostomy placement.
Data on 48682 individuals who had a gastrostomy between 1998-2019 in Sweden were collected from the mandatory National Patient Register. Indication, type of gastrostomy, and complications were based on registered International Statistical Classification of Diseases and Related Health Problems-diagnoses. Date and cause of death were retrieved by cross-matched data from the Death Register. The cohort was divided into three age groups: Children (0-18 years); adults (19-64 years); and elderly (≥ 65 years). The cohort was also divided by type of gastrostomy: PEG; open gastrostomy; and laparoscopic gastrostomy.
The annual use of gastrostomies in Sweden increased during the study period, from 13.7/100000 to 22.3/100000 individuals. PEG more than doubled, while a 10-fold increase was seen in laparoscopic gastrostomies. Although the procedure-related mortality was low (0.1%), a 10%-overall 30-d mortality was seen. The latter, however, decreased over time. One-year and ten-year survival rates for children, adults, and elderly were 93.7%, 67.5%, and 42.1% and 79.9%, 39.2%, and 6.8%, respectively. The most common causes of death were malignancies, cardiovascular conditions, and respiratory diseases.
More and more gastrostomies were placed in Sweden. The increase was due to the number of PEG procedures doubling. Although the 30-d mortality rate decreased during the study period, it was still high (10%). The most common causes of death were consistent with the gastrostomy indication, and as expected long-term survival was mainly dependent on patient age.
The present nationwide population-based results can be used as a reference in future trials and in quality controls at various levels.
| 1. | Park RH, Allison MC, Lang J, Spence E, Morris AJ, Danesh BJ, Russell RI, Mills PR. Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ. 1992;304:1406-1409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 258] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | Dietrich CG, Schoppmeyer K. Percutaneous endoscopic gastrostomy - Too often? World J Gastroenterol. 2020;26:2464-2471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (9)] |
| 3. | Kawata N, Kakushima N, Tanaka M, Sawai H, Imai K, Hagiwara T, Takao T, Hotta K, Yamaguchi Y, Takizawa K, Matsubayashi H, Ono H. Percutaneous endoscopic gastrostomy for decompression of malignant bowel obstruction. Dig Endosc. 2014;26:208-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1408] [Cited by in RCA: 1311] [Article Influence: 28.5] [Reference Citation Analysis (1)] |
| 5. | Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20:7739-7751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 416] [Cited by in RCA: 354] [Article Influence: 29.5] [Reference Citation Analysis (9)] |
| 6. | Sandberg F, Viktorsdóttir MB, Salö M, Stenström P, Arnbjörnsson E. Comparison of major complications in children after laparoscopy-assisted gastrostomy and percutaneous endoscopic gastrostomy placement: a meta-analysis. Pediatr Surg Int. 2018;34:1321-1327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Baker L, Beres AL, Baird R. A systematic review and meta-analysis of gastrostomy insertion techniques in children. J Pediatr Surg. 2015;50:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Rutter CE, Yovino S, Taylor R, Wolf J, Cullen KJ, Ord R, Athas M, Zimrin A, Strome S, Suntharalingam M. Impact of early percutaneous endoscopic gastrostomy tube placement on nutritional status and hospitalization in patients with head and neck cancer receiving definitive chemoradiation therapy. Head Neck. 2011;33:1441-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Klose J, Heldwein W, Rafferzeder M, Sernetz F, Gross M, Loeschke K. Nutritional status and quality of life in patients with percutaneous endoscopic gastrostomy (PEG) in practice: prospective one-year follow-up. Dig Dis Sci. 2003;48:2057-2063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Gavazzi C, Colatruglio S, Valoriani F, Mazzaferro V, Sabbatini A, Biffi R, Mariani L, Miceli R. Impact of home enteral nutrition in malnourished patients with upper gastrointestinal cancer: A multicentre randomised clinical trial. Eur J Cancer. 2016;64:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 11. | Dorst J, Dupuis L, Petri S, Kollewe K, Abdulla S, Wolf J, Weber M, Czell D, Burkhardt C, Hanisch F, Vielhaber S, Meyer T, Frisch G, Kettemann D, Grehl T, Schrank B, Ludolph AC. Percutaneous endoscopic gastrostomy in amyotrophic lateral sclerosis: a prospective observational study. J Neurol. 2015;262:849-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Suzuki Y, Urashima M, Izumi M, Ito Y, Uchida N, Okada S, Ono H, Orimo S, Kohri T, Shigoka H, Shintani S, Tanaka Y, Yoshida A, Ijima M, Ito T, Endo T, Okano H, Maruyama M, Iwase T, Kikuchi T, Kudo M, Takahashi M, Goshi S, Mikami T, Yamashita S, Akiyama K, Ogawa T, Ono S, Onozawa S, Kobayashi J, Matsumoto M, Matsumoto T, Jomoto K, Mizuhara A, Nishiguchi Y, Nishiwaki S, Aoki M, Ishizuka I, Kura T, Murakami M, Murakami A, Ohta T, Onishi K, Nakahori M, Tsuji T, Tahara K, Tanaka I, Kitagawa K, Shimazaki M, Fujiki T, Kusakabe T, Iiri T, Kitahara S, Horiuchi A, Suenaga H, Washizawa N, Suzuki M. The Effects of Percutaneous Endoscopic Gastrostomy on Quality of Life in Patients With Dementia. Gastroenterology Res. 2012;5:10-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Davies N, Barrado-Martín Y, Vickerstaff V, Rait G, Fukui A, Candy B, Smith CH, Manthorpe J, Moore KJ, Sampson EL. Enteral tube feeding for people with severe dementia. Cochrane Database Syst Rev. 2021;8:CD013503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Berg L. NOMESCO Classification of Surgical Procedures. [cited 11 November 2023]. Available from: https://norden.diva-portal.org/smash/get/diva2:970547/FULLTEXT01.pdf. |
| 15. | World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2019. [cited 11 November 2023]. Available from: https://icd.who.int/browse10/2019/en#!. |
| 16. | Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3938] [Cited by in RCA: 4219] [Article Influence: 281.3] [Reference Citation Analysis (0)] |
| 17. | Arvanitakis M, Gkolfakis P, Despott EJ, Ballarin A, Beyna T, Boeykens K, Elbe P, Gisbertz I, Hoyois A, Mosteanu O, Sanders DS, Schmidt PT, Schneider SM, van Hooft JE. Endoscopic management of enteral tubes in adult patients - Part 1: Definitions and indications. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53:81-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 18. | Folwarski M, Klek S, Brzeziński M, Szlagatys-Sidorkiewicz A, Wyszomirski A, Meyer-Szary J, Skonieczna-Żydecka K. Prevalence and Trends in Percutaneous Endoscopic Gastrostomy Placement: Results From a 10-Year, Nationwide Analysis. Front Nutr. 2022;9:906409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 19. | Gauderer MW. Percutaneous endoscopic gastrostomy-20 years later: a historical perspective. J Pediatr Surg. 2001;36:217-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 79] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Komiya K, Usagawa Y, Kadota JI, Ikegami N. Decreasing Use of Percutaneous Endoscopic Gastrostomy Tube Feeding in Japan. J Am Geriatr Soc. 2018;66:1388-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756-2763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1142] [Cited by in RCA: 1337] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 22. | Richter-Schrag HJ, Richter S, Ruthmann O, Olschewski M, Hopt UT, Fischer A. Risk factors and complications following percutaneous endoscopic gastrostomy: a case series of 1041 patients. Can J Gastroenterol. 2011;25:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (2)] |
| 23. | Stenberg K, Eriksson A, Odensten C, Darehed D. Mortality and complications after percutaneous endoscopic gastrostomy: a retrospective multicentre study. BMC Gastroenterol. 2022;22:361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 24. | Blomberg J, Lagergren J, Martin L, Mattsson F, Lagergren P. Complications after percutaneous endoscopic gastrostomy in a prospective study. Scand J Gastroenterol. 2012;47:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Vujasinovic M, Ingre C, Baldaque Silva F, Frederiksen F, Yu J, Elbe P. Complications and outcome of percutaneous endoscopic gastrostomy in a high-volume centre. Scand J Gastroenterol. 2019;54:513-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Figueiredo FA, da Costa MC, Pelosi AD, Martins RN, Machado L, Francioni E. Predicting outcomes and complications of percutaneous endoscopic gastrostomy. Endoscopy. 2007;39:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 27. | Lima DL, Miranda LEC, da Penha MRC, Lima RNCL, Dos Santos DC, Eufrânio MS, Miranda ACG, Pereira LMMB. Factors Associated with 30-Day Mortality in Patients after Percutaneous Endoscopic Gastrostomy. JSLS. 2021;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Lee TH, Shih LN, Lin JT. Clinical experience of percutaneous endoscopic gastrostomy in Taiwanese patients--310 cases in 8 years. J Formos Med Assoc. 2007;106:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Limpias Kamiya KJL, Hosoe N, Takabayashi K, Hayashi Y, Fukuhara S, Mutaguchi M, Nakamura R, Kawakubo H, Kitagawa Y, Ogata H, Kanai T. Factors predicting major complications, mortality, and recovery in percutaneous endoscopic gastrostomy. JGH Open. 2021;5:590-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Zopf Y, Maiss J, Konturek P, Rabe C, Hahn EG, Schwab D. Predictive factors of mortality after PEG insertion: guidance for clinical practice. JPEN J Parenter Enteral Nutr. 2011;35:50-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Sbeit W, Kadah A, Mari A, Mahamid M, Khoury T. Simple Bedside Predictors of Survival after Percutaneous Gastrostomy Tube Insertion. Can J Gastroenterol Hepatol. 2019;2019:1532918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Andersson L, Mikaelsson C, Arnbjörnsson E, Larsson LT. Laparoscopy aided gastrostomy in children. Ann Chir Gynaecol. 1997;86:19-22. [PubMed] |
| 33. | Backman T, Sjövie H, Kullendorff CM, Arnbjörnsson E. Continuous double U-stitch gastrostomy in children. Eur J Pediatr Surg. 2010;20:14-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Castanheira A, Swash M, De Carvalho M. Percutaneous gastrostomy in amyotrophic lateral sclerosis: a review. Amyotroph Lateral Scler Frontotemporal Degener. 2022;23:176-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Mitchell SL, Tetroe JM. Survival after percutaneous endoscopic gastrostomy placement in older persons. J Gerontol A Biol Sci Med Sci. 2000;55:M735-M739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Swedish Surgical Society.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Sweden
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Jadallah KA, Jordan; Osatakul S, Thailand S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Yuan YY