Published online Jan 7, 2024. doi: 10.3748/wjg.v30.i1.17
Peer-review started: November 4, 2023
First decision: November 30, 2023
Revised: December 7, 2023
Accepted: December 28, 2023
Article in press: December 28, 2023
Published online: January 7, 2024
Processing time: 63 Days and 5.1 Hours
Artificial intelligence is increasingly entering everyday healthcare. Large language model (LLM) systems such as Chat Generative Pre-trained Transformer (ChatGPT) have become potentially accessible to everyone, including patients with inflammatory bowel diseases (IBD). However, significant ethical issues and pitfalls exist in innovative LLM tools. The hype generated by such systems may lead to unweighted patient trust in these systems. Therefore, it is necessary to understand whether LLMs (trendy ones, such as ChatGPT) can produce plausible medical information (MI) for patients. This review examined ChatGPT’s potential to provide MI regarding questions commonly addressed by patients with IBD to their gastroenterologists. From the review of the outputs provided by ChatGPT, this tool showed some attractive potential while having significant limitations in updating and detailing information and providing inaccurate information in some cases. Further studies and refinement of the ChatGPT, possibly aligning the outputs with the leading medical evidence provided by reliable databases, are needed.
Core Tip: Patients with inflammatory bowel disease (IBD) increasingly access information resources online to receive information about disease management. Emerging artificial intelligence (AI) systems such as Chat Generative Pre-trained Transformer (ChatGPT) are taking hold in the daily reality of many patients with IBD. Through them, patients can potentially understand these systems as reliable or substitutes for medical consultation, especially for issues about reluctantly talking to their gastroenterologist. This review, examining ChatGPT’s outputs to common questions from patients with IBD, outlined how, while this AI system can provide some medical information, there are some limitations related to poor updating and the risk of inaccuracies that push for its cautious use.
- Citation: Gravina AG, Pellegrino R, Cipullo M, Palladino G, Imperio G, Ventura A, Auletta S, Ciamarra P, Federico A. May ChatGPT be a tool producing medical information for common inflammatory bowel disease patients’ questions? An evidence-controlled analysis. World J Gastroenterol 2024; 30(1): 17-33
- URL: https://www.wjgnet.com/1007-9327/full/v30/i1/17.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i1.17
The Chat Generative Pre-trained Transformer (ChatGPT) (www.chat.openai.com) is an artificial intelligence (AI)-based conversational large language model (LLM) chatbot system developed by OpenAI (San Francisco, CA, United States) and released in November 2022[1]. ChatGPT sparked a vigorous debate in the scientific community regarding the application of AI in the scientific literature (e.g., in the writing of scientific articles) by bringing the spotlight to bear on the scientific reliability and accuracy that such a system could offer[2,3].
ChatGPT has also been called upon as a possible bot to answer patients’ questions regarding their diseases, offering, in some cases, the potential for this purpose[4,5]. In gastroenterology, the possible application of ChatGPT is still highly pioneering, little explored, and far from being codified. There has been an interest in ChatGPT in the gastroenterology community, especially in the possibility of being able to answer clinical questions posed by patients and research questions. Concerning the latter, Lahat et al[6], for example, expressed some potential of LLMs in the genesis of research questions, although there is a great need to improve their novelty. Yeo et al[7], on the other hand, showed promising results of ChatGPT in answering clinical questions about liver cirrhosis. Similar results have recently been reported regarding colonoscopy-related medical information (MI)[8].
In inflammatory bowel disease (IBD), medical communication with the patient is crucial, as these diseases affect the patient to three hundred and sixty degrees by directly affecting their quality of life. IBDs are chronic, relapsing-remitting diseases with a particularly complex and multifactorial pathogenesis, mainly including Crohn’s disease (CD) and ulcerative colitis (UC). Therefore, patients must undergo periodic medical check-ups, diagnostic tests, and courses of treatment, often for a lifetime[9,10].
Consequently, in today’s context of widely available technology, patients often access information technology resources to obtain information for managing their IBD. The Internet is a prime tool for this purpose because it offers the patient a considerable window of resources, including social media[11,12] and ChatGPT. Patients often consult these resources independently to conduct targeted research for their concerns, but the physician is often integrated into this process through telehealth tools[13]. This analysis aimed to review the scientific validity of AI-generated outputs provided by ChatGPT regarding the genesis of MI regarding ten questions raised by patients with IBD.
ChatGPT is based on a natural language processing model developed by OpenAI, which allows the user to use it for various operations such as chatbots, dialogue systems, text formation, and question-answering[14]. Different versions of ChatGPT (i.e., GPT 1, 2, 3, and 4) have been developed over time, and it has been observed that it has grown from 117 million programming parameters (in GPT 1) to 300 billion parameters in GPT-3 with exponential improvement in various tasks (i.e., fine-tuning datasets, fine-tuning tasks, language understanding, text generation, and sentiment analysis)[14,15]. ChatGPT is based on a “training model” for reinforcement learning[14].
However, because ChatGPT is available to everyone, special care must be taken when such a platform is used by both healthcare professionals and patients to produce MI. ChatGPT has several limitations that have already been postulated. These include the lack of contextual understanding, the lack of common sense, the dependence of information on the need to provide the system with large amounts of data, and the lack of interpretability[14].
Ultimately, ChatGPT has limited knowledge because its operation (based on data-driven training processes) depends on the data on which it has been trained; thus, its merits do not include constant updating[16]. This is a significant limitation when approaching MI, as medical knowledge is highly changeable and is significantly affected by daily updates.
Because of these limitations, some authors have emphasised developing advanced LLMs to benefit patients with error-free MI[17]. In some medical contexts, however, ChatGPT has proven in early studies to perform better than other mainstream search engines (e.g., Google search)[18].
In contrast, the ChatGPT has several advantages. These include the availability of an always-on service with no downtime, a fast system with some efficiency, the ability to speak several languages (expanding the user base to include non-English-speaking people), and lastly, it is not operator-dependent as an AI[16].
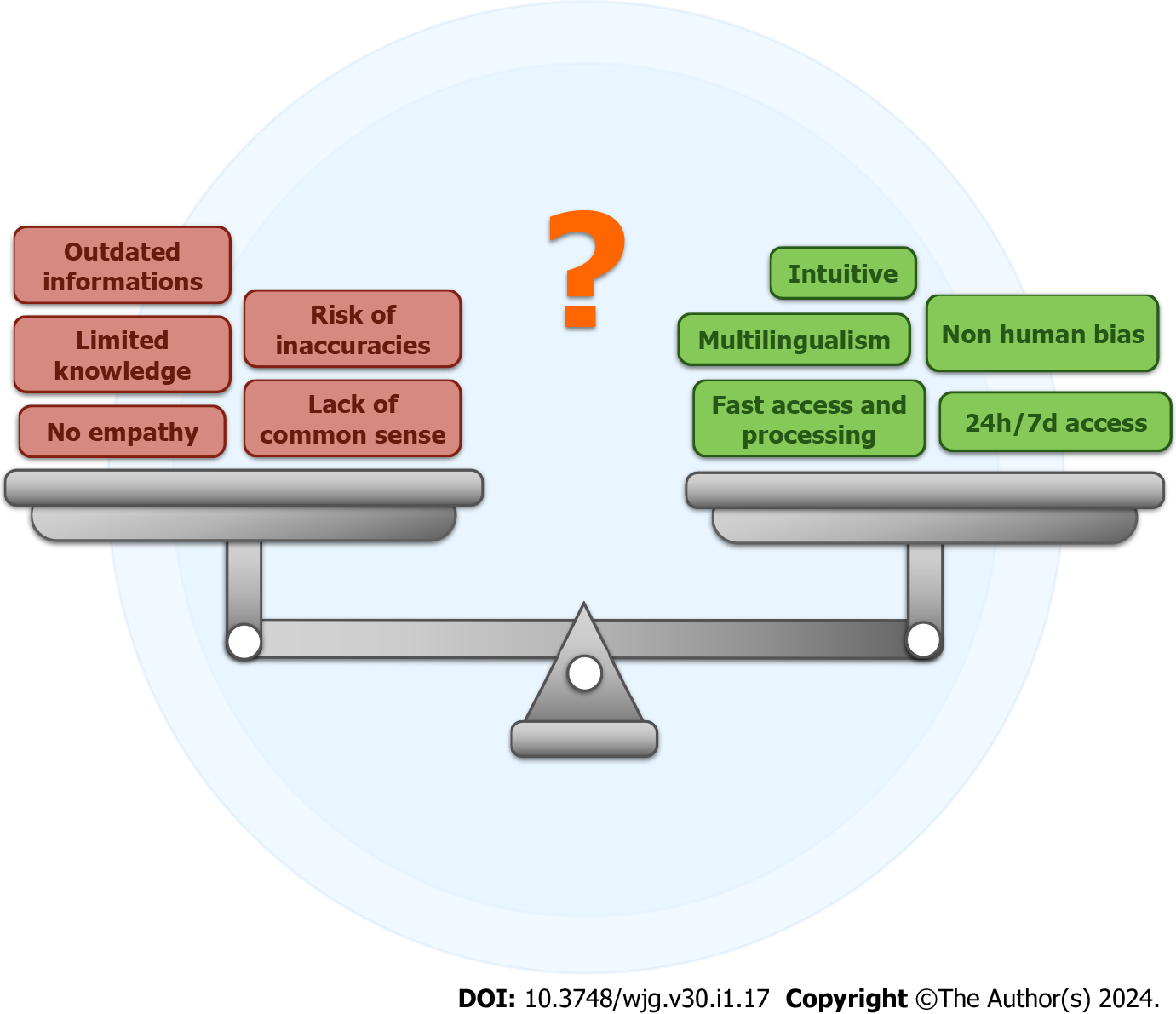
ChatGPT’s ability to produce human-like language led to the theorising that LLMs could represent an apparent revolution in healthcare[19]. The same applies to human-like problem-solving skills[20]. However, in a healthcare setting, especially a chronic one such as IBD, one of the biggest challenges is dealing with the empathy skills of the ChatGPT[5]. The empathy physicians can create with patients with IBD is crucial to the physician-patient relationship[21-24]. Patients with IBD are known to suffer from a high prevalence of anxiety-depressive disorders even in remission[25,26]. Figure 1 summarises some general advantages and disadvantages of using ChatGPT-generated AI.
A group of IBD-expert physicians retrieved a list of ten questions most frequently asked by patients with IBD (related to their IBD management) in their current clinical care practice. The ten with the highest frequency (Q1-10) were collected from the total number of questions. The people selecting inputs were not restricted in their choice of questions or given specific filters to adopt, but the only guideline provided was to select questions that patients asked most frequently in their current clinical practice. This mechanism was intended to sample real questions asked by IBD patients and not hypothesized/thought by physicians to avoid biased questions generated by a person with IBD scientific expertise. These questions were then input on ChatGPT on three different days (18th, 19th, and 20th August 2023), and each output generated by the chatbot was categorised as O1, O2, and O3, respectively. All research staff belonged to the Hepatogastroenterology Division of the University of Campania Luigi Vanvitelli, a regional Italian referral hospital for the management of IBD. All physicians involved in the study regularly contacted patients with IBD in their daily clinical practice.
The same research team evaluated the AI-generated responses by ChatGPT for each question by objectively comparing them with the available evidence. The ten questions with the highest frequency provided by all gastroenterologists in the study are listed in Table 1, and the ChatGPT outputs are listed in Table 2.
| Question | Question text (ChatGPT input) |
| 1 | Is there a definitive cure for IBD? |
| 2 | What should I eat to manage my IBD well? |
| 3 | How many times, as an IBD patient, in my life will I have to have a colonoscopy? |
| 4 | Can I avoid doing enemas for the management of my UC? |
| 5 | Can I have a baby with my IBD? |
| 6 | Can I, as an IBD patient, have my biologic drug in tablet form, avoiding subcutaneous or intravenous administration? |
| 7 | How much do I risk colorectal cancer with my IBD? |
| 8 | Do I, as an IBD patient, risk infection or cancer by doing biological therapy? |
| 9 | Will my IBD be transmitted to my children? |
| 10 | Can I avoid biological therapy after my first CD surgery? |
| Question | ChatGPT O1 | ChatGPT O2 | ChatGPT O3 |
| Day: August 18, 2023 - default (GPT-3.5) | Day: August 19, 2023 - default (GPT-3.5) | Day: August 20, 2023 - default (GPT-3.5) | |
| Q1 | As of my last knowledge update in September 2021, there is no definitive cure for IBD, which is a group of chronic inflammatory conditions that primarily affect the digestive tract. The two main types of IBD are CD and UC. While there is no cure, there are various treatment options available to manage the symptoms and control the inflammation associated with IBD. These treatments include medications, lifestyle changes, dietary modifications, and in some cases, surgical interventions. The goal of treatment is to induce and maintain remission, improve quality of life, and prevent complications. It’s important to note that research and medical advancements are ongoing, so I recommend consulting with a healthcare professional or checking more recent sources for the latest information on IBD treatment options and potential developments | As of my last knowledge update in September 2021, there is still no definitive cure for IBD. IBD is a complex and chronic condition that includes conditions like CD and UC, which involve inflammation of the digestive tract. While there have been significant advancements in understanding and treating IBD, no treatment or intervention has been proven to completely eliminate the underlying causes of the disease. Current treatments aim to manage symptoms, reduce inflammation, and promote remission, but they do not offer a guaranteed cure. It’s important to stay updated with the latest medical research and consult with healthcare professionals for the most accurate and current information on IBD treatments and potential breakthroughs | As of my last update in September 2021, there is still no definitive cure for IBD, which includes conditions like CD and UC. IBD is a complex and chronic condition characterized by inflammation of the digestive tract. While there have been significant advancements in understanding and managing IBD, a true cure that eliminates the underlying causes of the disease has not been discovered. Current treatments focus on managing symptoms, reducing inflammation, and achieving periods of remission, but they do not provide a permanent cure. Research and medical advancements are ongoing, so it’s important to stay informed about the latest developments in IBD treatments. Always consult with healthcare professionals for the most up-to-date information and advice regarding IBD management and potential breakthroughs |
| Q2 | I am not a doctor, but I can offer some general dietary guidelines that are commonly recommended for managing IBD. It’s important to consult with a qualified healthcare professional or a registered dietitian who specializes in IBD for personalized advice tailored to your specific condition and needs. Here are some general tips: (1) Low-residue diet: This involves consuming foods that are easy to digest and produce less waste. It may include well-cooked and peeled fruits and vegetables, refined grains, lean protein sources, and well-cooked eggs; (2) FODMAP diet: This diet reduces intake of certain types of carbohydrates that can be poorly absorbed in the small intestine, leading to symptoms in some individuals. It may be helpful for managing symptoms such as gas, bloating, and diarrhea; (3) Anti-inflammatory foods: Incorporate foods rich in anti-inflammatory properties, such as fatty fish (like salmon and mackerel), walnuts, flaxseeds, chia seeds, turmeric, ginger, and leafy greens; (4) Lean protein: Choose lean sources of protein, such as skinless poultry, fish, eggs, tofu, and tempeh. Protein is important for tissue repair and immune function; (5) Good fats: Consume healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Drink plenty of fluids to stay hydrated, as diarrhea and other symptoms can lead to dehydration. Water, herbal teas, and clear broths are good options; (7) Avoid trigger foods: Identify and avoid foods that trigger your symptoms. Common triggers vary from person to person but may include dairy products, spicy foods, caffeine, and alcohol; (8) Small, frequent meals: Eating smaller, more frequent meals throughout the day can help ease the digestive process and prevent overwhelming your system; (9) Probiotics: Some people with IBD find that probiotics can help regulate gut flora and improve symptoms. Consult your healthcare provider before adding probiotics to your routine; (10) Monitor fiber intake: While fiber is generally beneficial for digestion, too much insoluble fiber can worsen symptoms for some individuals. Gradually introduce soluble fiber sources like oats, bananas, and cooked vegetables; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider trying lactose-free or plant-based dairy alternatives like almond milk, coconut milk, or lactose-free yogurt; and (12) Supplements: Some people with IBD may need supplements to address nutrient deficiencies. Consult your healthcare provider before taking any supplements. Remember, what works for one person may not work for another. Keep a food diary to track your symptoms and identify patterns, and work closely with a healthcare professional to develop a personalized dietary plan that suits your specific condition and needs | Managing IBD requires a personalized approach that considers your specific symptoms, triggers, and nutritional needs. While I can’t provide medical advice, I can offer some general dietary tips that may help you manage your condition better. However, it’s crucial to work closely with a healthcare professional or registered dietitian who specializes in IBD to develop a tailored eating plan. Here are some dietary principles to consider: (1) Low-residue diet: This diet focuses on consuming foods that are easily digestible and produce minimal waste. It may include well-cooked fruits and vegetables, refined grains, lean proteins, and limited high-fiber foods; (2) FODMAP diet: Some individuals with IBD find relief by following a low-FODMAP diet, which limits certain types of carbohydrates that can trigger digestive symptoms; (3) Anti-inflammatory foods: Include foods rich in anti-inflammatory properties, such as fatty fish (salmon, mackerel), walnuts, flaxseeds, turmeric, ginger, and leafy greens; (4) Lean protein: Opt for lean sources of protein like skinless poultry, fish, eggs, tofu, and tempeh. Protein is essential for healing and immune function; (5) Healthy fats: Incorporate healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Stay well-hydrated to prevent dehydration, which can worsen symptoms. Water, herbal teas, and clear broths are good choices; (7) Individual triggers: Identify and avoid specific trigger foods that exacerbate your symptoms. These triggers can vary widely from person to person; (8) Small, frequent meals: Eating smaller meals throughout the day can ease digestion and prevent overwhelming your digestive system; (9) Probiotics: Some individuals with IBD find that probiotics help balance gut bacteria and improve symptoms. Consult your healthcare provider before using probiotics; (10) Monitor fiber intake: Gradually introduce soluble fiber sources like oats, bananas, and cooked vegetables. Monitor your tolerance and adjust accordingly; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider lactose-free or plant-based alternatives like almond milk or coconut yogurt; (12) Supplements: Nutrient deficiencies are common in IBD. Discuss with your healthcare provider whether you need supplements to address any deficiencies; (13) Listen to your body: Pay attention to how your body responds to different foods. Keep a food diary to track symptoms and identify patterns; (14) Avoid rapid changes: Make dietary changes gradually to give your body time to adapt and monitor how each change affects you; and (15) Collaborate with professionals: Work closely with a healthcare provider and a registered dietitian who specializes in IBD to create a personalized eating plan that meets your nutritional needs and helps manage your symptoms. Remember that IBD is a complex condition, and what works for one person might not work for another. It’s important to develop an individualized approach that considers your unique situation and preferences | Managing IBD through diet can be complex and highly individualized, as the condition varies from person to person. It’s important to work closely with a healthcare provider or a registered dietitian who specializes in IBD to create a personalized eating plan tailored to your specific needs and symptoms. That being said, here are some general dietary guidelines that you might find helpful: (1) Low-residue diet: This type of diet focuses on consuming foods that are easy to digest and produce minimal waste. It may include well-cooked vegetables, lean protein sources, refined grains, and tender fruits; (2) FODMAP diet: Some individuals with IBD may benefit from a low-FODMAP diet, which limits certain types of carbohydrates that can trigger digestive symptoms. It’s important to work with a healthcare professional to properly implement this diet; (3) Anti-inflammatory foods: Incorporate foods with anti-inflammatory properties, such as fatty fish (salmon, mackerel), nuts, seeds, turmeric, ginger, and leafy greens; (4) Lean protein: Choose lean sources of protein like skinless poultry, fish, eggs, tofu, and tempeh. Protein is essential for healing and immune function; (5) Healthy fats: Include healthy fats from sources like olive oil, avocados, nuts, and seeds. These fats can help reduce inflammation; (6) Hydration: Drink plenty of fluids to prevent dehydration, which can worsen symptoms. Water, herbal teas, and clear broths are good options; (7) Individual triggers: Identify and avoid foods that trigger your symptoms. Common triggers include dairy products, spicy foods, caffeine, and alcohol; (8) Small, frequent meals: Eating smaller meals throughout the day can help ease digestion and prevent overwhelming your digestive system; (9) Probiotics: Some individuals with IBD find that probiotics help balance gut bacteria and improve symptoms. Consult your healthcare provider before using probiotics; (10) Monitor fiber intake: Gradually introduce soluble fiber sources like oats, bananas, and well-cooked vegetables. Monitor how fiber affects your symptoms and adjust as needed; (11) Dairy alternatives: If you’re lactose intolerant or sensitive to dairy, consider lactose-free or plant-based alternatives like almond milk or coconut yogurt; (12) Supplements: Nutrient deficiencies are common in IBD. Work with your healthcare provider to determine if you need supplements to address any deficiencies; (13) Listen to your body: Pay attention to how your body responds to different foods. Keep a food diary to track symptoms and identify patterns; and (14) Collaborate with professionals: Your healthcare provider and a registered dietitian experienced in IBD can help you create a personalized eating plan that considers your individual needs and goals. Remember, managing IBD involves ongoing experimentation to find what works best for you. It’s not uncommon for dietary needs to change over time, so staying in close communication with your healthcare team is crucial |
| Q3 | I am not a doctor, but I can provide you with some general information about colonoscopies for IBD. The frequency of colonoscopies for IBD patients can vary depending on several factors, including the type of IBD (CD or UC), the severity of the condition, your response to treatment, and your doctor’s recommendations. In general, people with IBD may need to undergo colonoscopies periodically to monitor the progression of the disease, assess the effectiveness of treatment, and detect any complications. Early detection and management of inflammation are important to prevent further damage to the digestive tract. It’s best to discuss the recommended frequency of colonoscopies with your gastroenterologist, as they can provide personalized guidance based on your specific condition and medical history. They will take into account factors such as your symptoms, disease activity, and overall health to determine the appropriate timing and frequency of colonoscopies for you | The number of colonoscopies a person with IBD may need during their lifetime can vary widely based on individual factors. These factors include the type of IBD (CD or UC), the severity of the disease, how well the disease responds to treatment, and the presence of any complications. Generally, individuals with IBD may have colonoscopies at various points in their lives: (1) Diagnosis: Colonoscopy is often used to diagnose IBD. If you are newly diagnosed, you might have had at least one colonoscopy for diagnostic purposes; (2) Monitoring disease activity: Depending on the severity and type of IBD, your doctor may recommend regular colonoscopies to monitor disease activity and assess the effectiveness of treatment. This could range from once a year to every few years; (3) Flares or symptoms: During periods of disease flares or if new symptoms develop, your doctor might recommend a colonoscopy to assess the current state of your digestive tract; (4) Surveillance: In some cases, individuals with long-standing UC may need regular colonoscopies to monitor for the development of dysplasia (abnormal cell changes that can lead to cancer). This is less common in CD; (5) Preventive measures: If you have a family history of colorectal cancer or other risk factors, your doctor might recommend more frequent colonoscopies as a preventive measure; and (6) Post-surgery: After certain surgeries for IBD, follow-up colonoscopies might be performed to assess healing and the overall condition of the intestine. It’s important to note that medical recommendations can change over time as new research and guidelines emerge. Your healthcare provider will create a personalized plan based on your specific circumstances and the most up-to-date medical knowledge. Regular communication with your gastroenterologist is crucial to determining the appropriate frequency of colonoscopies for your situation | The number of colonoscopies you’ll need as an individual with IBD can vary greatly depending on multiple factors. These factors include the type of IBD (CD or UC), the severity of your condition, your response to treatment, your overall health, and any complications that may arise. It’s important to understand that there is no fixed number of colonoscopies that applies to all IBD patients. The frequency and necessity of colonoscopies will be determined by your healthcare provider based on your specific situation. Here are some general guidelines: (1) Diagnosis: You will likely have at least one colonoscopy for diagnostic purposes when your IBD is first diagnosed; (2) Disease monitoring: Depending on the severity of your IBD and how well it responds to treatment, your doctor may recommend periodic colonoscopies to monitor disease activity and assess the condition of your intestines. This could range from once every year or two to less frequently; (3) Flares or symptoms: If you experience a flare-up of symptoms or new symptoms emerge, your doctor might recommend a colonoscopy to evaluate the extent of inflammation and identify any issues; (4) Long-term management: If your IBD is well controlled, the frequency of colonoscopies might decrease over time. However, your doctor will still periodically assess whether colonoscopies are necessary; (5) Complications or surgery: If you experience complications related to IBD or if you undergo surgery, you may need additional colonoscopies to monitor healing and overall intestinal health; and (6) Individualized care: Your doctor will create an individualized care plan that takes into account your specific medical history, disease progression, and treatment response. This plan will determine the frequency of colonoscopies you’ll need throughout your life. The best source of information regarding the number and timing of colonoscopies for your specific situation is your gastroenterologist. They will guide you based on the latest medical guidelines and your personal health profile. Regular communication with your healthcare provider is crucial to managing your IBD effectively and making informed decisions about your medical care |
| Q4 | I am not a doctor, but I can offer you some general information. The management of UC typically involves a combination of medications, lifestyle changes, and sometimes medical procedures. Enemas may be recommended by a healthcare professional as part of the treatment plan, but whether you can avoid doing enemas depends on various factors, including the severity of your condition and your individual response to treatment. It’s important to discuss your concerns and preferences with your healthcare provider | Whether you can avoid using enemas for the management of your UC depends on several factors, including the severity of your condition, your response to other treatments, and your doctor’s recommendations. Enemas are one of the treatment options used to deliver medications directly to the inflamed areas of the colon in order to reduce inflammation and manage symptoms. However, there are alternative treatments available for UC that you can discuss with your healthcare provider. These may include: (1) Oral medications: Depending on the severity of your condition, your doctor may prescribe oral medications such as aminosalicylates, corticosteroids, immunomodulators, or biologics. These medications can help reduce inflammation and manage symptoms without the need for enemas; (2) Suppositories: If you are uncomfortable with enemas, your doctor might recommend using rectal suppositories as an alternative. These medications work similarly to enemas but are inserted into the rectum; (3) Lifestyle modifications: Making certain changes to your diet and lifestyle can also help manage UC symptoms. This includes avoiding trigger foods, staying hydrated, managing stress, and getting regular exercise; and (4) Surgery: In more severe cases of UC that do not respond well to other treatments, surgery may be considered. Surgery can involve removing the affected portion of the colon and may offer long-term relief from symptoms. It’s important to have an open and honest discussion with your healthcare provider about your preferences, concerns, and treatment options. They can help tailor a treatment plan that aligns with your needs and goals while effectively managing your UC symptoms. Remember that self-management decisions should be made in consultation with your healthcare team, as they have the expertise to guide you toward the best treatment approach for your individual case | Yes, in some cases, it might be possible to avoid using enemas for the management of UC, depending on the severity of your condition, your response to other treatments, and your doctor’s recommendations. Enemas are one way to deliver medications directly to the inflamed areas of the colon, but there are alternative treatments available that might be suitable for you. It’s important to work closely with your healthcare provider to determine the best treatment plan for your specific situation. Here are some alternatives to enemas for managing UC: (1) Oral medications: Your doctor might prescribe oral medications such as aminosalicylates, corticosteroids, immunomodulators, or biologics to reduce inflammation and manage symptoms; (2) Rectal suppositories: If you’re uncomfortable with enemas, your doctor might recommend using rectal suppositories. These medications are inserted into the rectum and can be effective in treating inflammation in the lower part of the colon; (3) Lifestyle modifications: Making dietary and lifestyle changes can help manage UC symptoms. Avoiding trigger foods, staying hydrated, managing stress, and getting regular exercise can contribute to symptom relief; (4) Topical creams or foams: Some topical creams or foams containing corticosteroids can be used to treat inflammation in the rectum and lower colon; (5) Biologic injections: Biologic medications can be administered through injections or infusions, and they target specific parts of the immune system to reduce inflammation; and (6) Surgery: In severe cases where other treatments are not effective, surgery might be considered to remove the affected part of the colon. This can offer long-term relief from symptoms, but it’s typically considered when other options have been exhausted. Ultimately, the decision to avoid enemas and explore alternative treatments should be made in consultation with your healthcare provider. They will take into account your medical history, the severity of your condition, and your preferences to help you create a treatment plan that is both effective and manageable for you |
| Q5 | IBD refers to a group of chronic inflammatory conditions that affect the gastrointestinal tract. The two main types of IBD are CD and UC. These conditions can cause symptoms such as abdominal pain, diarrhea, fatigue, and weight loss. If you have IBD and are considering having a baby, it’s important to consult with your healthcare provider, such as a gastroenterologist and an obstetrician/gynecologist. While having IBD may present some challenges during pregnancy, many women with IBD can have successful pregnancies and healthy babies with proper medical care and management. Here are a few points to consider and discuss with your healthcare provider: (1) Pre-pregnancy planning: It’s a good idea to discuss your plans to conceive with your healthcare provider before getting pregnant. They can help you optimize your IBD management and make any necessary adjustments to your treatment plan to ensure your health is stable before conception; (2) Medication management: Many medications used to treat IBD have been studied for their safety during pregnancy. Your doctor will work with you to find the right balance between managing your disease and minimizing potential risks to the baby. In some cases, adjustments to medications might be needed during pregnancy; (3) Disease activity: Ideally, it’s best to conceive when your IBD is in remission or under good control. Active inflammation could potentially affect both your health and the health of the baby; (4) Nutrition and lifestyle: Maintaining a healthy lifestyle and nutrition plan can be crucial for managing IBD during pregnancy. Your doctor or a registered dietitian can provide guidance on foods that may help manage your symptoms; (5) Monitoring and follow-up: Regular prenatal care and monitoring are essential. Your healthcare team will monitor your IBD symptoms and adjust your treatment plan as needed throughout your pregnancy; and (6) Delivery and postpartum: The mode of delivery (vaginal or cesarean) may be influenced by your IBD status and any complications. Postpartum care should also be carefully managed to ensure your IBD remains well-controlled. Remember, every individual’s situation is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare team and following their guidance, you can make informed decisions to promote a healthy pregnancy and successful outcomes for both you and your baby | Yes, many individuals with IBD can have successful pregnancies and healthy babies with proper medical care and management. However, it’s important to approach pregnancy with careful planning and consultation with your healthcare providers, including a gastroenterologist and an obstetrician/gynecologist. Here are a few key points to keep in mind: (1) Pre-pregnancy planning: Before trying to conceive, it’s advisable to consult with your healthcare team. They can assess your overall health, the status of your IBD, and your current treatment plan. This will allow them to make any necessary adjustments to ensure you’re in the best possible condition for pregnancy; (2) Medication management: Your healthcare provider will review your medications to ensure they are safe for pregnancy. In some cases, modifications to your treatment plan might be necessary to balance managing your IBD symptoms while minimizing potential risks to the baby; (3) Disease activity: If possible, it’s generally recommended to conceive when your IBD is in remission or well-controlled. Active inflammation could potentially affect your health and the health of the baby; (4) Prenatal care: Regular prenatal care is crucial for monitoring both your IBD and the progress of your pregnancy. Your healthcare team will work together to ensure your health and the health of your baby are being adequately managed; (5) Delivery planning: Depending on the status of your IBD and any potential complications, your healthcare team will discuss the most appropriate mode of delivery for you, whether it’s vaginal or caesarean; and (6) Postpartum care: After giving birth, it’s important to continue managing your IBD with your healthcare team’s guidance. They will monitor your condition and make any necessary adjustments to your treatment plan. Remember that each person’s situation is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare providers and following their advice, you can increase the likelihood of a healthy pregnancy and successful outcomes for both you and your baby | Yes, it is possible to have a baby if you have IBD. Many individuals with IBD go on to have successful pregnancies and healthy babies. However, there are certain factors to consider and steps to take to ensure a safe and healthy pregnancy: (1) Consult your healthcare team: Before attempting to conceive, it’s important to consult with your healthcare providers, including your gastroenterologist and obstetrician/gynecologist. They can assess your current health, the severity of your IBD, and your medication regimen to determine if you are in a good condition for pregnancy; (2) Pre-pregnancy planning: Your healthcare team will work with you to optimize your IBD management before pregnancy. This might involve adjusting your medication, addressing any nutritional concerns, and ensuring your IBD is well-controlled; (3) Medication management: Many IBD medications have been studied for their safety during pregnancy. Your doctors will help you balance managing your IBD symptoms with the potential risks to the baby. In some cases, medication adjustments might be necessary; (4) Disease activity: If possible, it’s generally recommended to conceive when your IBD is in remission or well-controlled. Active inflammation could potentially affect both your health and the health of the baby; (5) Prenatal care: Regular prenatal check-ups are crucial to monitor both your IBD and the progress of your pregnancy. Your healthcare team will collaborate to ensure both your well-being and the baby’s health; (6) Delivery planning: Depending on the state of your IBD and any potential complications, your healthcare providers will help you decide on the best mode of delivery for you; and (7) Postpartum care: After giving birth, it’s important to continue managing your IBD with your healthcare team’s guidance. They will monitor your condition and make any necessary adjustments to your treatment plan. Remember that each person’s experience is unique, and the impact of IBD on pregnancy can vary. By working closely with your healthcare providers and following their guidance, you can increase the likelihood of a successful pregnancy and a healthy baby |
| Q6 | As of my last knowledge update in September 2021, most biologic drugs used for treating IBD are typically administered through subcutaneous injections or intravenous infusions. However, new developments and advancements in medical treatments may have occurred since then. Tablet or oral formulations of biologic drugs are an area of ongoing research and development. These formulations aim to provide a more convenient option for patients who prefer oral medications over injections or infusions. Oral administration of biologics could potentially improve patient compliance and quality of life. To get the most accurate and up-to-date information about the availability of tablet forms of biologic drugs for IBD treatment, I recommend discussing this with your gastroenterologist or healthcare provider. They will be able to provide you with information about the latest treatment options and whether any tablet formulations are currently available or under development for IBD management. Always consult with a medical professional for personalized advice regarding your specific condition and treatment options | As of my last update in September 2021, the majority of biologic drugs for IBD were administered through subcutaneous injections or intravenous infusions. However, there have been ongoing efforts to develop oral formulations of biologics for IBD treatment to offer patients a more convenient option. Since I don’t have access to real-time information beyond September 2021, I recommend checking with your healthcare provider or gastroenterologist for the latest updates on available treatment options. If any tablet forms of biologic drugs for IBD have been developed since then, your healthcare provider will be able to provide you with accurate and current information about whether this option is available for you and whether it’s suitable for your specific condition | As of my last knowledge update in September 2021, most biologic drugs for IBD were administered through subcutaneous injections or intravenous infusions. However, there were ongoing research and development efforts to create oral tablet forms of biologic medications for IBD to provide a more convenient option for patients. If you are interested in exploring the possibility of receiving your biologic drug in tablet form, I recommend discussing this with your healthcare provider or gastroenterologist. They will have the most up-to-date information about available treatment options and whether any tablet formulations have been approved or are in development for IBD treatment. Your healthcare provider will consider your individual medical history, disease severity, and treatment preferences to determine the best course of action for your specific situation. Always follow the guidance of your healthcare provider when making decisions about your treatment plan |
| Q7 | People with IBD, which includes conditions like CD and UC, do have an increased risk of developing colorectal cancer compared to the general population. However, the exact level of risk can vary based on factors such as the type and duration of IBD, the extent of inflammation, and individual characteristics. Here are some general points to consider: (1) Type of IBD: Patients with UC, especially if it involves a larger portion of the colon and has been present for a longer time, tend to have a higher risk of colorectal cancer compared to those with CD; (2) Duration of disease: The longer you have had IBD, the higher your risk of developing colorectal cancer. The risk generally increases after about 8-10 yr of having the disease; (3) Severity of inflammation: Those who experience more severe and widespread inflammation in the colon are at a higher risk of colorectal cancer; (4) Family history: If you have a family history of colorectal cancer or other risk factors, your overall risk may be higher; (5) Regular monitoring: Regular surveillance colonoscopies are often recommended for individuals with IBD to detect precancerous changes or early-stage cancer. The frequency of these screenings depends on individual risk factors and your doctor’s recommendations; (6) Management and treatment: Proper management of IBD, including medication and lifestyle changes, can help reduce the risk of colorectal cancer. Working closely with a healthcare provider is essential; and (7) Advancements in treatment: With advancements in IBD treatment and management, the risk of colorectal cancer in IBD patients has been decreasing over time. It’s important to have open and regular discussions with your healthcare provider about your specific risk profile and the steps you can take to minimize your risk. They can provide personalized guidance based on your medical history, current condition, and any other relevant factors | I’m not a doctor, but I can provide some general information based on existing knowledge. People with IBD, such as CD or UC, do have an increased risk of colorectal cancer compared to the general population. The exact level of risk can vary widely based on several factors, including the type of IBD, the extent and severity of inflammation, the duration of the disease, family history, and other individual characteristics. As a rough estimate, it’s been suggested that individuals with extensive and long-standing UC may have a colorectal cancer risk that is several times higher than that of the general population. However, advancements in treatment and monitoring have helped reduce this risk over the years. It’s important to work closely with your healthcare provider who can assess your specific risk factors and recommend appropriate monitoring and management strategies. Regular colonoscopies and other surveillance measures are often recommended for individuals with IBD to detect any potential precancerous changes or early signs of cancer. Remember that your healthcare provider is the best source of information regarding your personal health and risk factors | I understand your concern, but it’s important to note that I am not able to provide personalized medical advice or predict individual outcomes. The risk of colorectal cancer associated with IBD can vary significantly from person to person. It depends on factors such as the type of IBD (CD or UC), the duration and severity of the inflammation, your family history, and other individual factors. Generally, individuals with long-standing and extensive UC have a higher risk of developing colorectal cancer compared to those with CD or those with milder forms of IBD. However, advancements in medical management and surveillance have helped reduce the overall risk over the years. To get accurate and personalized information about your risk of colorectal cancer with your specific inflammatory bowel disease, it’s best to consult with your healthcare provider. They can assess your medical history, current condition, and other relevant factors to provide you with the most appropriate guidance and recommendations. Regular monitoring and open communication with your healthcare team are key to managing your health effectively |
| Q8 | I am not a doctor, but I can provide you with some general information based on what is known up to my knowledge cutoff date in September 2021. Biological therapies, also known as biologics, are a type of treatment often used for IBD such as CD and UC. These therapies target specific components of the immune system to help reduce inflammation and control symptoms of IBD. Biologics can be effective in managing IBD symptoms and inducing and maintaining remission. However, like any medical treatment, biological therapies do carry potential risks and side effects. Some of these risks include: (1) Infections: Biologics suppress certain aspects of the immune system, which can increase the risk of infections. While on biologics, you may be more susceptible to certain types of infections. It’s important to discuss your individual risk factors and ways to mitigate infection risks with your healthcare provider; (2) Cancer: Some studies have suggested a possible increased risk of certain types of cancers, particularly lymphomas and skin cancers, in individuals using biologics. However, the overall risk appears to be relatively low, and the benefits of controlling inflammation and maintaining remission may outweigh the potential risks. Regular monitoring and communication with your healthcare provider are essential; (3) Allergic reactions: While uncommon, some people may experience allergic reactions to biologics; (4) Other side effects: Biologics can also have other side effects, such as injection site reactions, fatigue, headaches, and more. Your healthcare provider will monitor you closely and help manage any side effects. It’s important to note that the risks and benefits of biological therapy can vary depending on the specific type of biologic, your individual health status, and other factors. Your healthcare provider will carefully evaluate your situation and help you make an informed decision about whether biologic therapy is the right choice for you. Always consult your healthcare provider for personalized advice and recommendations based on your specific medical history, current health status, and the latest available medical knowledge. They can provide you with the most up-to-date information and help you weigh the potential benefits and risks of any treatment option | As of my last knowledge update in September 2021, I can provide you with some general information about the potential risks associated with biological therapy for IBD. However, please keep in mind that medical knowledge and research can evolve, so it’s important to consult with your healthcare provider for the most up-to-date and personalized information: (1) Infection risk: Biological therapies work by targeting specific components of the immune system. While they can help control inflammation and manage IBD symptoms, they can also suppress the immune response, which may increase the risk of infections. Infections could range from common ones like respiratory infections to potentially more serious ones. It’s important to discuss your risk factors and preventive measures with your healthcare provider. They will likely monitor you closely for any signs of infection while you are on biological therapy; (2) Cancer risk: There have been concerns about a potential increased risk of certain types of cancers in individuals using biological therapies for IBD. The risk seems to be relatively low, and it’s important to weigh this risk against the potential benefits of managing your IBD symptoms. Some studies have suggested a slightly elevated risk of lymphomas and skin cancers. However, the overall risk increase is considered small, and many patients benefit greatly from biologic therapies. Regular monitoring and communication with your healthcare provider are key to managing any potential risks; and (3) Individual factors: Your specific risk factors for infections and cancer will depend on various factors, including the specific type of biological therapy you are considering, your medical history, your overall health, and any other treatments you might be undergoing. Your healthcare provider will assess these factors to help you make an informed decision about the best treatment approach for you. It’s important to have an open and thorough discussion with your healthcare provider before starting any new treatment, including biological therapies. They will be able to provide you with the most relevant and up-to-date information based on your individual circumstances. Additionally, they can help you understand the potential benefits and risks of the treatment and work with you to develop a plan that maximizes the benefits while minimizing potential risks | Yes, individuals with IBD who undergo biological therapy do carry a certain level of risk for infections and potentially some types of cancers. However, the actual risk varies depending on several factors including the specific type of biological therapy, your medical history, and other individual factors: (1) Infection risk: Biological therapies can suppress the immune system’s response to inflammation, which can increase the risk of infections. While the risk is generally higher compared to individuals not on these medications, the extent of the risk can vary depending on the specific drug, your overall health, and how closely you’re monitored. It’s important to work with your healthcare provider to minimize this risk and to promptly address any signs of infection; and (2) Cancer risk: Some studies have suggested a slightly elevated risk of certain cancers, particularly lymphomas and skin cancers, in individuals using certain types of biological therapies. However, the overall risk increase is generally considered to be low. Again, the specific risk varies based on the type of medication and other individual factors. Regular monitoring and open communication with your healthcare provider are crucial to manage this risk. Ultimately, the decision to undergo biological therapy should be made in consultation with your healthcare provider, taking into consideration your overall health, disease severity, treatment alternatives, and potential benefits and risks. Your healthcare provider will be able to guide you through the decision-making process, help you understand the potential risks, and monitor your health closely throughout the course of treatment |
| Q9 | IBD, which includes conditions like CD and UC, has a complex and multifactorial etiology involving both genetic and environmental factors. While there is a genetic component to IBD, it is not solely determined by genetics, and the risk of passing the disease on to your children is not absolute. Here are a few points to consider: (1) Genetics: IBD does have a genetic component, meaning that if you have IBD, there is a slightly increased risk that your children may also develop the condition. However, the exact genetic contribution is not fully understood, and having a family member with IBD doesn’t guarantee that your children will develop it; (2) Environmental factors: Environmental factors, such as diet, lifestyle, and exposure to certain triggers, also play a significant role in the development of IBD. It’s not only about genetics. Your children’s risk could be influenced by a combination of genetic susceptibility and environmental factors; (3) Complex inheritance: IBD is considered a complex genetic disorder, meaning that it is influenced by multiple genes rather than being caused by a single gene. This complexity makes it challenging to predict the likelihood of transmission to your children; (4) Risk factors: If one parent has IBD, the risk of their children developing the disease is slightly higher compared to the general population, but it is still relatively low. If both parents have IBD, the risk may be higher than if only one parent is affected; and (5) Genetic counseling: If you are concerned about the potential transmission of IBD to your children, it’s a good idea to consult with a genetic counselor or a medical professional who specializes in this area. They can provide personalized information based on your medical history, family history, and current understanding of the genetic factors involved. Remember that genetics is just one piece of the puzzle, and many other factors contribute to the development of IBD. If you have concerns about IBD and its potential impact on your children, it’s best to have an open and thorough discussion with a healthcare provider who can provide guidance and address your specific situation | The transmission of IBD to children is not a straightforward process and can be influenced by a combination of genetic and environmental factors. While there is a genetic component to IBD, it doesn’t guarantee that your children will definitely inherit the condition. Here’s what you should consider: (1) Genetic predisposition: There is a genetic predisposition to IBD, which means that having a family member with the condition increases the risk of developing it. However, the genetics of IBD are complex and involve the interaction of multiple genes. It’s not a simple case of one gene causing the disease. This makes it difficult to predict with certainty whether your children will inherit IBD; (2) Environmental factors: Environmental factors play a significant role in the development of IBD. Factors such as diet, lifestyle, exposure to certain triggers, and the overall environment can contribute to the onset and severity of the disease. Even if your children have a genetic predisposition, environmental factors could influence whether or not they actually develop IBD; (3) Relative risk: Having a parent with IBD does increase the risk for children, but the actual risk remains relatively low. If one parent has IBD, the risk for their children is higher compared to the general population but is still not a certainty. If both parents have IBD, the risk may be slightly higher; (4) Genetic counseling: If you are concerned about the potential transmission of IBD to your children, it’s advisable to consult with a genetic counselor or a healthcare professional who specializes in this area. They can assess your specific situation, provide information about the genetic factors involved, and offer guidance on potential risks; and (5) Advancements in research: Medical knowledge and research are continuously advancing. There might be new insights and discoveries about the genetics and inheritance of IBD in the future that could provide a clearer understanding of the risks involved. Ultimately, while there is a genetic component to IBD, it is not the sole determinant of whether your children will develop the condition. Genetic predisposition combined with environmental factors contribute to the overall risk. If you have concerns about passing on IBD to your children, seeking guidance from medical professionals with expertise in this area is recommended | I understand your concern, but I’m not able to provide personalized medical predictions. The risk of transmitting IBD to your children depends on a combination of genetic and environmental factors. While there is a genetic predisposition to IBD, it’s not a guarantee that your children will inherit the condition. IBD is influenced by multiple genes, and the interplay between these genes and environmental factors makes it challenging to predict the exact likelihood of passing the disease on to your children. Genetic factors do increase the risk, especially if you or your partner have IBD, but many individuals with a family history of IBD do not develop the disease. If you are concerned about the potential transmission of IBD to your children, I recommend consulting a healthcare professional or a genetic counselor. They can provide more personalized information based on your medical history, family history, and current understanding of the genetics of IBD |
| Q10 | I am not a doctor, but I can provide you with some general information. The decision about whether to use biological therapy after a CD surgery depends on various factors, including the severity of your condition, the extent of the surgery, your overall health, and your doctor’s recommendations. Biological therapies, such as anti-TNF drugs (e.g., infliximab, adalimumab), are often used to treat CD because they can help reduce inflammation and manage symptoms. They may be recommended to help prevent flare-ups or recurrence of the disease after surgery. It’s important to have an open and thorough discussion with your gastroenterologist or healthcare provider about your treatment options. They can provide personalized advice based on your medical history, current condition, and specific circumstances. If you have concerns about biological therapy, make sure to express them to your doctor so they can address them and work with you to find the most appropriate treatment plan. Remember, the decision to use or avoid biological therapy should be made in consultation with a qualified healthcare professional who has a complete understanding of your individual situation | Whether or not you can avoid biological therapy after your first CD surgery depends on several factors, and it’s a decision that should be made in consultation with your healthcare provider. Here are a few points to consider: (1) Severity of CD: If your CD is severe and has a high likelihood of recurrence after surgery, your doctor might recommend starting or continuing biological therapy to help prevent flare-ups; (2) Extent of surgery: The type of surgery you underwent and the amount of affected intestine that was removed can influence the risk of recurrence. More extensive surgeries may be associated with a higher risk of disease recurrence; (3) Medical history: Your medical history, including how well you responded to previous treatments, any complications you’ve experienced, and your overall health, will play a role in determining your post-surgery treatment plan; (4) Risks and benefits: Your doctor will weigh the potential benefits of biological therapy in preventing disease recurrence against the risks and side effects associated with these medications; (5) Patient preference: Your preferences and comfort with different treatment options are important. If you have concerns about biological therapy, make sure to discuss them with your doctor; (6) Alternative treatments: There are various treatments available for CD beyond biological therapies. Your doctor might consider other medications, dietary changes, and lifestyle modifications based on your specific situation; and (7) Regular monitoring: Even if you don’t start biological therapy immediately after surgery, your doctor will likely recommend regular follow-up appointments and monitoring to detect any signs of disease recurrence early. Ultimately, the decision about post-surgery treatment should be a collaborative one between you and your healthcare provider. They can provide you with the most up-to-date information about treatment options, potential benefits, risks, and expected outcomes based on your unique medical history and current condition. It’s important to have an open and honest conversation with your doctor to ensure you make the best decision for your health | Yes, it is possible to avoid biological therapy after your first CD surgery, but the decision will depend on several factors, including the recommendations of your healthcare provider, the severity of your condition, and your individual circumstances. Here are a few things to consider: (1) Doctor’s recommendation: Your healthcare provider will assess your medical history, the extent of your surgery, the severity of your CD, and your risk of recurrence. Based on these factors, they will recommend a treatment plan, which may or may not include biological therapy; (2) Disease severity: If your CD is relatively mild and your surgery was successful in removing the affected area, your doctor might consider alternatives to biological therapy, such as traditional medications or lifestyle changes; (3) Risk of recurrence: CD has a tendency to recur even after surgery. If your doctor believes that your risk of disease recurrence is high, they may recommend starting or continuing with biological therapy to help prevent flare-ups; (4) Personal preference: Your preferences and comfort with different treatment options are important. If you have concerns about biological therapy, make sure to express them to your doctor. They can discuss the pros and cons of various treatments with you; (5) Alternative treatments: There are other treatments available for CD, such as immunosuppressive medications, corticosteroids, and lifestyle modifications. Your doctor may explore these options based on your specific situation; and (6) Regular monitoring: Regardless of the treatment plan, it’s likely that your doctor will recommend regular follow-up appointments and monitoring to track your disease progression and adjust your treatment if necessary. It’s crucial to have an open and thorough discussion with your healthcare provider about your treatment options. They can provide you with the information you need to make an informed decision about whether to pursue biological therapy or explore alternative treatments. Remember that your doctor’s expertise and understanding of your condition are essential in guiding your treatment journey |
The first input (Q1) concerned the potential existence of a definitive therapy for IBD. Q1 ChatGPT outputs (O1-3) correctly defined IBD, expressing their chronicity, the main phenotypes (i.e., CD and UC), and the target of their inflammatory action (i.e., the gastrointestinal tract)[27]. The outputs correctly expressed the absence of definitive therapy for IBD, and Q1 O1 outlined the macro categories of treatments currently available for IBD (i.e., medical and surgical treatments)[28-31].
In addition, the goals toward which specific IBD therapy should strive provided by the outputs (i.e., induction/maintenance of remission, prevention of complications, and improvement of quality of life) are the focus of the European Crohn’s and Colitis Organisation guidelines[28-31], as of the current consensus on selecting therapeutic targets in IBD[32]. The final aspect of Q1 O1 is how optimal nutrition also affects the therapeutic management of IBD[33]. Q1 O2,3 did not address this aspect. In all outputs, ChatGPT set out the need to keep up to date with the pace of research and consult a health professional out of necessity.
Approaching this subject in the case of UC is particularly difficult. Surgical treatment of UC with definitive techniques (e.g., restorative proctocolectomy without ileostomy) does not always guarantee the absence of short- and long-term complications[31]. For example, packing the ileal pouch can lead to the emergence of acute and chronic forms of pouchitis[34]. In contrast, in CD, surgery does not exclude the reactivation of the disease at the perianastomotic site or its emergence at other gastrointestinal sites[35].
Q1 O1-3, therefore, failed to make a clear distinction between CD and UC in terms of the power to control the inflammatory burden of IBD by not expressing the different possibilities that surgery can offer between CD and UC. In other words, in conclusion, Q1 O1-3 have not been able to fully filter the nuances that exist between healing and cure, adapt these concepts to the IBD phenotype, and grade the therapeutic approach to the curative degree it can provide (especially in conditions such as UC where surgery drastically adjusts the course of the disease and its natural history by healing the underlying disease).
Q2 focused on the kind of nutrition the IBD patient should follow to correctly manage his or her disease. In the case of Q2, ChatGPT provided, in all outputs, a list of dietary advice; however, considering it as a prerequisite for such advice, the need for patient to seek professional advice. The proposed dietary advice included a low-residue diet, low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) diet, anti-inflammatory foods, lean protein, good fats, hydration, avoidance of trigger foods, small and frequent meals, probiotics, monitoring fiber intake, dairy alternatives, and supplements.
Q2, O2, and O3 also advised personalising the diet to identify trigger foods (i.e., “listen to your body”) and working with professionals. O2 also advised avoiding dietary changes too quickly. Comprehensive nutrition analysis in IBD is particularly complex because no specific diet can be specifically recommended to induce remission in patients with active disease, as stated by the European Society for Clinical Nutrition and Metabolism (i.e., ESPEN) guidelines[33]. The outputs’ premise differed in that O1 defined the provided list of nutritional recommendations as “commonly recommended for managing IBD” while still advising to counsel with a professional. In contrast, Q2 O2-3 were more reluctant to define specific recommendations. However, the list of dietary advice provided seems to appear as “generally deemed” dietary advice. The evidence underlying such advice from the perspective of the “safety/efficacy” profile is, as written, particularly poor[33].
In Q2, as in Q1, ChatGPT failed to detail some aspects of IBD nutrition. For example, IBD nutrition can be resent from watersheds, especially in patients who are already undergoing surgery. In addition, although a low-fiber diet is recommended in Q2 O1-O3, such a regimen is not always valid for all patients with IBD, but it can be considered in cases such as patients with CD with a stricturing phenotype[36]. In addition, it is still complex to isolate which specific dietary components (e.g., cereals, sugar, fat, protein, and dietary fiber) may be associated with relapse or worsening of pre-existing clinical manifestations in IBD[36].
Indeed, stepping outside the realm of specific guideline recommendations, the low-FODMAP diet, while giving good results on symptomatology control in several IBD-focused studies, has not yet been firmly proven to reduce gut inflammation and, indeed, in some settings, has reduced several favourable bacterial species (i.e., F. prausnitzii, C. cluster IV)[37].
Finally, ChatGPT correctly instructed the patients to hear from their professional caregivers before taking supplements or probiotics. This is because of the often disproportionate and misguided use of supplements in patients with IBD[38] and the poorly defined evidence on the benefits of consuming specific probiotics[39-41].
One of the most severe issues for IBD patients is undoubtedly the need to undergo repeated endoscopic examinations to manage their disease, especially when performed under conditions of clinical remission (e.g., colorectal cancer surveillance)[42]. ChatGPT has adopted a particularly weighted approach to answer this question. In Q3, O1 differed significantly from O2,3. O1 deferred the discussion to the gastroenterology specialist, expressing an extreme variety of factors determining the frequency of endoscopic examinations. O2,3, on the other hand, also explicitly listed several cases in which colonoscopy can be performed or repeated to manage IBD. Such cases include initial diagnosis, disease activity monitoring, flare-up, surveillance (i.e., long-standing UC), and after surgery. All possible indications of performing/repeating lower gastrointestinal endoscopic examinations proposed by ChatGPT are scientifically supportable[43,44]. Even in Q3, in each output, ChatGPT expressed the need for the patient to refer to their specialist and did not launch improper definitions of colonoscopy repeat frequency (since Q3 was a direct question about the number of times to repeat colonoscopy).
Traditional therapies still play a crucial role in UC management. Central to the latter is 5-aminosalicylic acid (5-ASA), which can be administered in oral formulations (with different delivery techniques based on Eudragit or MMX) and topically. Topical formulations allow the direct attack of proctitis-type (i.e., E1) or distal UC (i.e., E2) forms of UC according to the Montreal classification[29].
Recent meta-analytic evidence showed that combination therapy with topical and oral 5-ASA had the highest performance for induction of clinical remission (P-score 0.91), prevention of recurrence (P-score 0.91), and induction of endoscopic remission (P-score 0.9) while showing an optimal safety profile[45]. Nevertheless, 5-ASA also has the ability (with a minimum dosage of 1.2 g daily) to possess a chemopreventive effect against colorectal cancer (odds ratio = 0.46)[46]. These premises make the choice of modifying and/or removing topical therapy in UC difficult, considering the short- and long-term benefits it can provide in both the inductive and maintenance phases of remission. Conversely, the patient does not always easily tolerate topical therapy, which can provide discomfort[47-50].
In Q4, the input asked ChatGPT about the possibility of not performing topical therapy for UC. Q4 O1 correctly explained that the use of enemas is part of the therapeutic possibilities of UC and that it depends on disease activity and declined the choice of the removal of enemas to the healthcare professional[29,36]. Q4 O2,3 also expressed the alternatives to enemas that the patient can discuss with their specialist (i.e., oral therapy, suppositories, lifestyle modifications, surgery) and in the case of O3 biological therapy or topical foams/creams.
Q2 O2,3, however, in listing alternatives to enemas, ignored the aspects already written in the introduction to this paragraph, namely the evidence that topical 5-ASA therapy (especially when combined with oral therapy) is still highly relevant. Q2 O1-3 also ignored how enemas were administered and the importance of correctly delivering them. It would have been helpful (while advising referral to the physician) to provide a list of tips on how to perform enemas properly, the possibility of adjusting the volume of enemas according to individual tolerability, and advice on how to avoid local soreness or early evacuation of the enema. In other words, Q4 O1-3 may have too high a deterrent load toward enemas, prompting the patient not to do so.
In addition, Q4 O2 also provided inaccuracy in terms of oral therapy (i.e., “These drugs can help reduce inflammation and manage symptoms without the need for enemas”). This assertion contradicts the available evidence[29,45]. In addition, in the same output, ChatGPT asserts “These medications work similarly to enemas but are inserted into the rectum”, referring to suppositories. This is further evidence of inaccuracy[36]. Q4 O2-3 cannot be provided to the patient and should be subjected to a physician’s preliminary filter.
IBD affecting female patients of reproductive age can collide with pregnancies that such patients may develop. However, for this reason, there are concerns that patients manifest as many IBD-related as not[51-53].
In this sense, Q5 obtained outputs expressing the need to work side-by-side with specialists in the field (e.g., obstetricians/gynaecologists and gastroenterologists). The outputs also expressed some factors to consider when planning a pregnancy affected by IBD. ChatGPT correctly listed some essential factors in the pregnancy pathway in the context of IBD. In detail, they include pre-conception counselling, the preferability of having a pregnancy with well-controlled disease activity, and the need to tailor IBD therapy to safety for the foetus in prenatal care[54].
Another positive aspect is that ChatGPT, in all outputs related to Q5, expressly specified that the mode of delivery (vaginal or caesarean) is affected by IBD. It is well known that the non-vaginal mode of delivery should be preferred in patients with active perinatal disease, after restorative proctocolectomy, or with rectovaginal fistula[54].
In Q6, the question was asked about the possibility of receiving biologic drug administration for IBD treatment in the oral vs the parenteral form (i.e., intravenous or subcutaneous). ChatGPT responses (updated until September 2021) were far from the current reality, where oral formulations for IBD, particularly approved for UC, are also available in guideline-recommended indications (e.g., tofacitinib, filgotinib, ozanimod, upadacitinib)[29,55,56].
Q7 receives slightly different outputs. O1 was the most in-depth and listed some factors that influence the increased risk of colorectal cancer in IBD (especially in UC), such as, by way of example, duration of disease and severity of inflammation and family history, as well as how it is necessary to undergo regular surveillance colonoscopy and IBD therapy because of the action of some therapies for IBD in colorectal cancer management. Q7 O2 and O3 expounded these concepts more succinctly than O1 did. ChatGPT answers are scientifically plausible because, to date, European guidelines recommend risk stratification into three risk categories (i.e., lower, intermediate, and high) based on several parameters (e.g., extent of disease, familiarity, presence of stenosis/dysplasia, and extra-intestinal manifestations such as primary sclerosing cholangitis) and, based on these, determine the frequency with which patients with IBD should undergo surveillance colonoscopy[57].
The prevalence of colorectal cancer or colic dysplasia in IBD is far from insignificant and is responsible for 10%-15% of deaths in patients with IBD[58]. The risk is especially high in UC patients with extensive disease after 8-10 years of diagnosis[57]. In addition, undergoing some biological therapies may increase the risk of infectious events[59].
Regarding the risk of biologics-related cancer, ChatGPT outputs were cautious, expressing that risk was generally low, stigmatizing the need for this risk to be weighed individually for the risk-benefit ratio by the health care specialist[60-63]. Regarding infectious risk, outputs have correctly expressed how it may be increased during biological therapy[59].
Q9 O1-3 correctly included genetics as one of many components that can determine the pathogenesis of IBD[27] and did not guarantee the patient a heritability of IBD to offspring as a canonical genetically transmitted disease[64]. In addition, ChatGPT, in its outputs, also added how family history, a well-known risk factor for IBD, plays a role in determining the heritability of IBD[65,66]. As in all outputs related to all questions, in the case of Q9, ChatGPT referred the patient to a specialist in the field. In this specific question, it avowed the role of the geneticist.
The last question (i.e., Q10) exposed the possibility of avoiding the biological therapy set for prophylaxis of postoperative recurrence in CD. Q10 O1 did not comment and referred the discussion to the physician. Q10 O2,3, on the other hand, correctly exhibited some of the factors based on which one may decide to avoid biological therapy after initial CD surgery (e.g., extent of surgery, risks and benefits, patient preference)[35].
To the best of our knowledge, this review was the first of its kind to weigh the ability of ChatGPT, an LLM system, to provide AI-generated reliable MI for IBD-related questions. A comparison of the outputs provided by ChatGPT showed that such AI-generated MI shows some scientific reliability. However, our analysis shows that this judgment is not always valid and expected in that some outputs (e.g., those related to Q4 or Q6) were not scientifically correct or poorly updated (i.e., until September 2021).
The use of LLM and AI-generated MI is, at present, the subject of intense controversy in the scientific community in a dichotomy between revolution in medical education, research and patient communication until concerns related to a new potential infodemic[1-3,67-69]. This review expresses the need for further refinements of ChatGPT before it can be implemented as a complementary response mechanism to patient concerns.
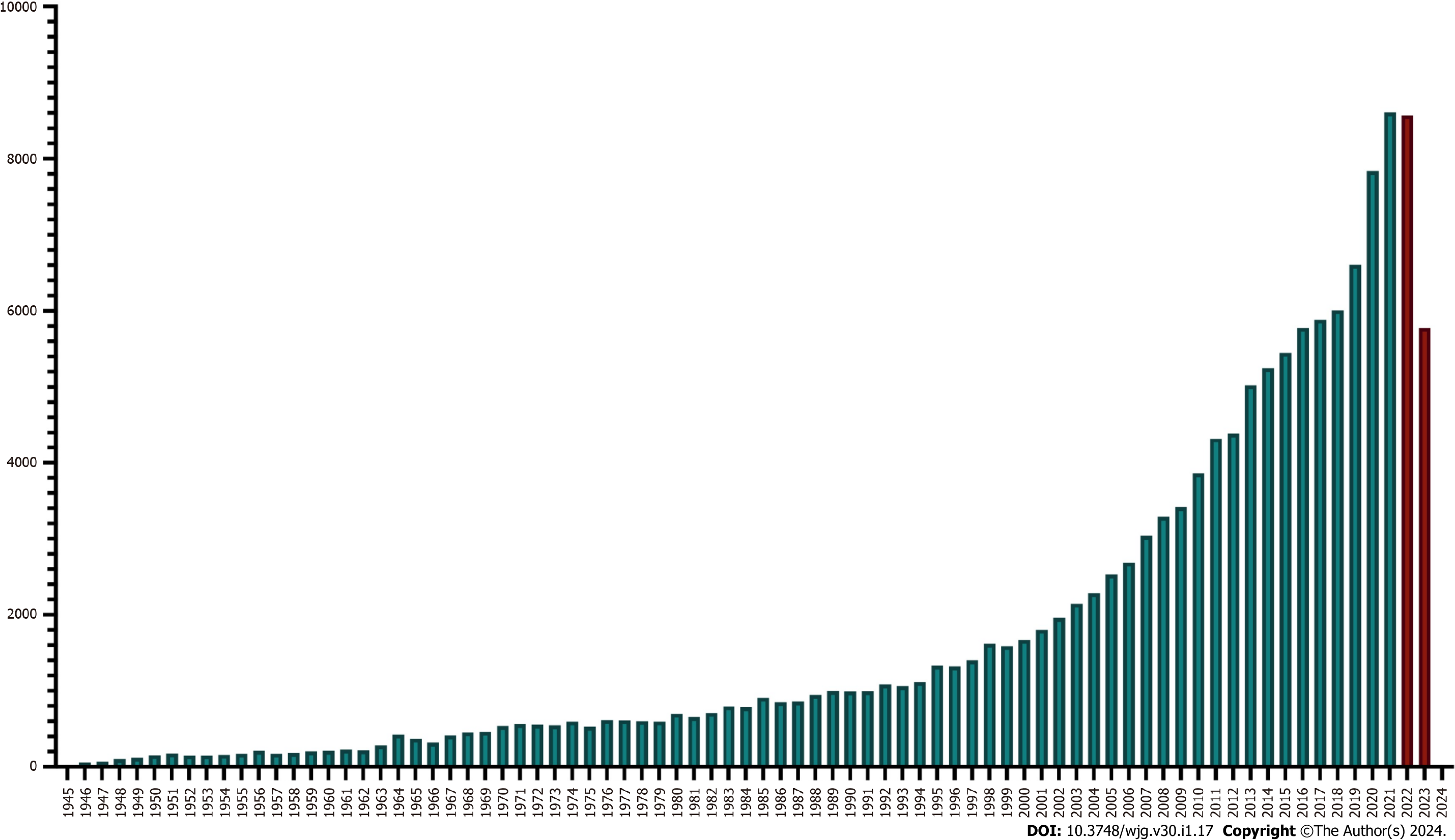
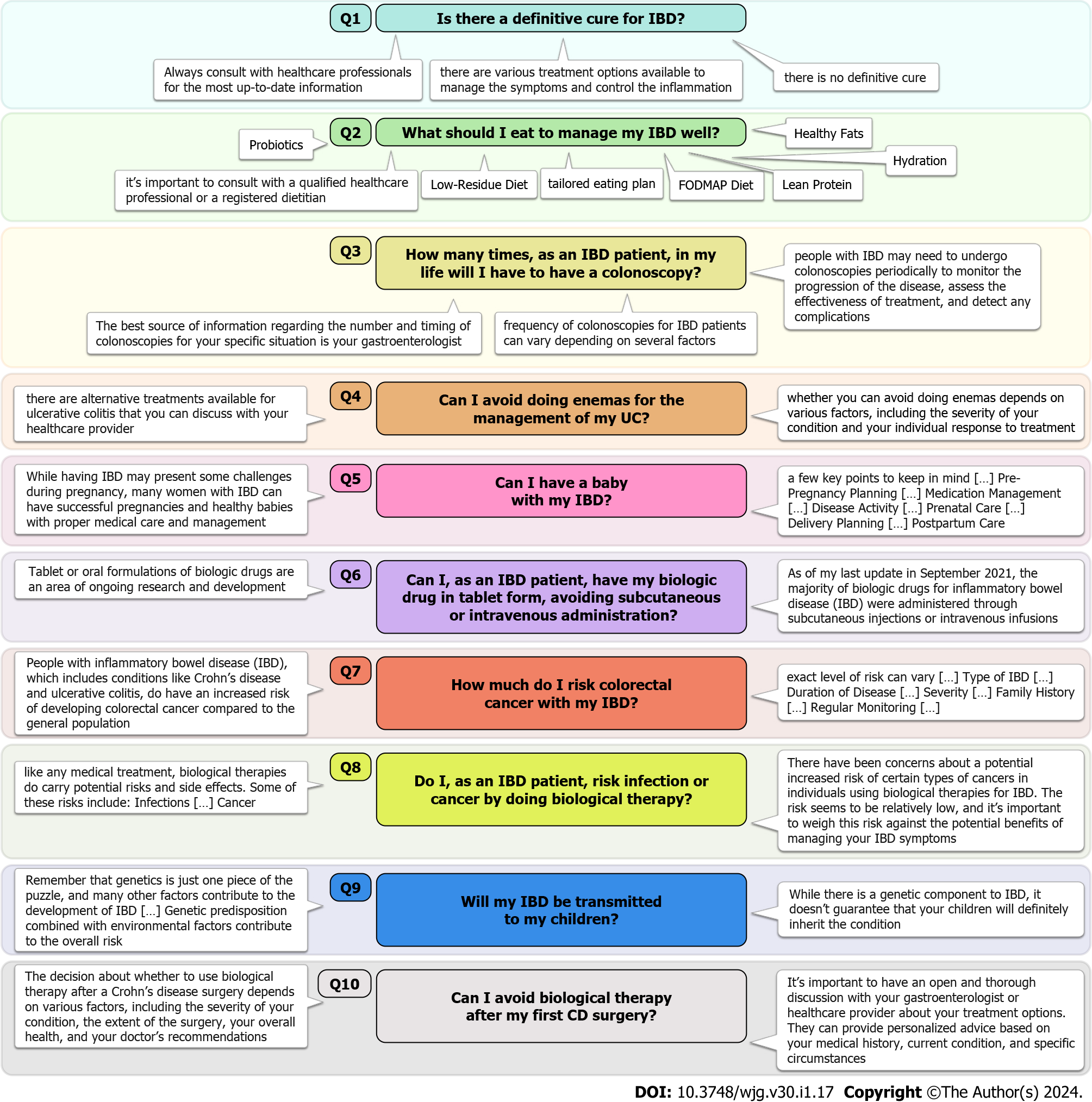
In addition, it should be made sure that ChatGPT is trained on papers provided by databases commonly considered valid in the scientific community (e.g., Scopus, Web of Science, MEDLINE). Another essential pitfall is the lack of updating that ChatGPT detects in almost all its outputs referred to until September 2021 (Figure 2). In addition, ChatGPT did not provide evidence levels for the sources employed to generate the outputs, thus removing the reader’s ability to discern different degrees of quality for the same. Finally, it is also necessary to explore the capability of ChatGPT in so many other aspects related to IBD not already covered in this review (the latter, moreover, schematized in Figure 3).
| 1. | Sallam M. ChatGPT Utility in Healthcare Education, Research, and Practice: Systematic Review on the Promising Perspectives and Valid Concerns. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1517] [Cited by in RCA: 1069] [Article Influence: 356.3] [Reference Citation Analysis (96)] |
| 2. | Thorp HH. ChatGPT is fun, but not an author. Science. 2023;379:313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 358] [Reference Citation Analysis (0)] |
| 3. | The Lancet Digital Health. ChatGPT: friend or foe? Lancet Digit Health. 2023;5:e102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 145] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 4. | Potapenko I, Boberg-Ans LC, Stormly Hansen M, Klefter ON, van Dijk EHC, Subhi Y. Artificial intelligence-based chatbot patient information on common retinal diseases using ChatGPT. Acta Ophthalmol. 2023;101:829-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 111] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 5. | Ayers JW, Poliak A, Dredze M, Leas EC, Zhu Z, Kelley JB, Faix DJ, Goodman AM, Longhurst CA, Hogarth M, Smith DM. Comparing Physician and Artificial Intelligence Chatbot Responses to Patient Questions Posted to a Public Social Media Forum. JAMA Intern Med. 2023;183:589-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 767] [Cited by in RCA: 1208] [Article Influence: 402.7] [Reference Citation Analysis (0)] |
| 6. | Lahat A, Shachar E, Avidan B, Shatz Z, Glicksberg BS, Klang E. Evaluating the use of large language model in identifying top research questions in gastroenterology. Sci Rep. 2023;13:4164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 54] [Reference Citation Analysis (0)] |
| 7. | Yeo YH, Samaan JS, Ng WH, Ting PS, Trivedi H, Vipani A, Ayoub W, Yang JD, Liran O, Spiegel B, Kuo A. Assessing the performance of ChatGPT in answering questions regarding cirrhosis and hepatocellular carcinoma. Clin Mol Hepatol. 2023;29:721-732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 389] [Article Influence: 129.7] [Reference Citation Analysis (0)] |
| 8. | Lee TC, Staller K, Botoman V, Pathipati MP, Varma S, Kuo B. ChatGPT Answers Common Patient Questions About Colonoscopy. Gastroenterology. 2023;165:509-511.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 106] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 9. | Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life. 2019;12:113-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 210] [Cited by in RCA: 465] [Article Influence: 66.4] [Reference Citation Analysis (113)] |
| 10. | Zhang YZ, Li YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014;20:91-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 751] [Cited by in RCA: 1132] [Article Influence: 94.3] [Reference Citation Analysis (31)] |
| 11. | Fortinsky KJ, Fournier MR, Benchimol EI. Internet and electronic resources for inflammatory bowel disease: a primer for providers and patients. Inflamm Bowel Dis. 2012;18:1156-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Ahmed W, Taft TH, Charabaty A. Social media in inflammatory bowel disease: the patient and physician perspective. Curr Opin Gastroenterol. 2021;37:328-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Pang L, Liu H, Liu Z, Tan J, Zhou LY, Qiu Y, Lin X, He J, Li X, Lin S, Ghosh S, Mao R, Chen M. Role of Telemedicine in Inflammatory Bowel Disease: Systematic Review and Meta-analysis of Randomized Controlled Trials. J Med Internet Res. 2022;24:e28978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 14. | Alawida M, Mejri S, Mehmood A, Chikhaoui B, Isaac Abiodun O. A Comprehensive Study of ChatGPT: Advancements, Limitations, and Ethical Considerations in Natural Language Processing and Cybersecurity. Information. 2023;14:462. [DOI] [Full Text] |
| 15. | Goyal T, Li JJ, Durrett G. News Summarization and Evaluation in the Era of GPT-3. 2022 Preprint. Available from: arXiv:2209.12356. [DOI] [Full Text] |
| 16. | Thakkar KY, Jagdishbhai N. Exploring the capabilities and limitations of GPT and Chat GPT in natural language processing. JMRA. 2023;10:18-20. [DOI] [Full Text] |
| 17. | Chakraborty C, Bhattacharya M, Lee SS. Need an AI-Enabled, Next-Generation, Advanced ChatGPT or Large Language Models (LLMs) for Error-Free and Accurate Medical Information. Ann Biomed Eng. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Ayoub NF, Lee YJ, Grimm D, Divi V. Head-to-Head Comparison of ChatGPT Versus Google Search for Medical Knowledge Acquisition. Otolaryngol Head Neck Surg. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 53] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 19. | Will ChatGPT transform healthcare? Nat Med. 2023;29:505-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 131] [Reference Citation Analysis (0)] |
| 20. | Orrù G, Piarulli A, Conversano C, Gemignani A. Human-like problem-solving abilities in large language models using ChatGPT. Front Artif Intell. 2023;6:1199350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 21. | Chiapponi C, Witt M, Dlugosch GE, Gülberg V, Siebeck M. The Perception of Physician Empathy by Patients with Inflammatory Bowel Disease. PLoS One. 2016;11:e0167113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Wagoner ST, Kavookjian J. The Influence of Motivational Interviewing on Patients With Inflammatory Bowel Disease: A Systematic Review of the Literature. J Clin Med Res. 2017;9:659-666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Mocciaro F, Di Mitri R, Russo G, Leone S, Quercia V. Motivational interviewing in inflammatory bowel disease patients: a useful tool for outpatient counselling. Dig Liver Dis. 2014;46:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Gargallo-Puyuelo CJ, García-Mateo S, Martinez-Domínguez SJ, Gomollón F. Is the gender or age of the physician key to a good physician-patient with inflammatory bowel disease relationship? Gastroenterol Hepatol. 2023;46:261-265. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 479] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 26. | Spina A, Mazzarella C, Dallio M, Romeo M, Pellegrino R, Durante T, Romano M, Loguercio C, Di Mauro M, Federico A, Gravina AG. The Lesson from the First Italian Lockdown: Impacts on Anxiety and Depressive Symptoms and Sleep Quality in Patients with Remission of Inflammatory Bowel Disease. Rev Recent Clin Trials. 2022;17:109-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (2)] |
| 27. | Chang JT. Pathophysiology of Inflammatory Bowel Diseases. N Engl J Med. 2020;383:2652-2664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 891] [Article Influence: 148.5] [Reference Citation Analysis (0)] |
| 28. | Adamina M, Bonovas S, Raine T, Spinelli A, Warusavitarne J, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, Doherty G, El-Hussuna A, Ellul P, Fiorino G, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gisbert JP, Gomollon F, González Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Kucharzik T, Lytras T, Maaser C, Magro F, Marshall JK, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Stassen L, Torres J, Uzzan M, Vavricka S, Verstockt B, Zmora O. ECCO Guidelines on Therapeutics in Crohn's Disease: Surgical Treatment. J Crohns Colitis. 2020;14:155-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 388] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 29. | Raine T, Bonovas S, Burisch J, Kucharzik T, Adamina M, Annese V, Bachmann O, Bettenworth D, Chaparro M, Czuber-Dochan W, Eder P, Ellul P, Fidalgo C, Fiorino G, Gionchetti P, Gisbert JP, Gordon H, Hedin C, Holubar S, Iacucci M, Karmiris K, Katsanos K, Kopylov U, Lakatos PL, Lytras T, Lyutakov I, Noor N, Pellino G, Piovani D, Savarino E, Selvaggi F, Verstockt B, Spinelli A, Panis Y, Doherty G. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Medical Treatment. J Crohns Colitis. 2022;16:2-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 667] [Article Influence: 166.8] [Reference Citation Analysis (1)] |
| 30. | Torres J, Bonovas S, Doherty G, Kucharzik T, Gisbert JP, Raine T, Adamina M, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, El-Hussuna A, Ellul P, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gomollon F, González-Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Lytras T, Maaser C, Magro F, Marshall JK, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Spinelli A, Stassen L, Uzzan M, Vavricka S, Verstockt B, Warusavitarne J, Zmora O, Fiorino G. ECCO Guidelines on Therapeutics in Crohn's Disease: Medical Treatment. J Crohns Colitis. 2020;14:4-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 991] [Cited by in RCA: 978] [Article Influence: 163.0] [Reference Citation Analysis (2)] |
| 31. | Spinelli A, Bonovas S, Burisch J, Kucharzik T, Adamina M, Annese V, Bachmann O, Bettenworth D, Chaparro M, Czuber-Dochan W, Eder P, Ellul P, Fidalgo C, Fiorino G, Gionchetti P, Gisbert JP, Gordon H, Hedin C, Holubar S, Iacucci M, Karmiris K, Katsanos K, Kopylov U, Lakatos PL, Lytras T, Lyutakov I, Noor N, Pellino G, Piovani D, Savarino E, Selvaggi F, Verstockt B, Doherty G, Raine T, Panis Y. ECCO Guidelines on Therapeutics in Ulcerative Colitis: Surgical Treatment. J Crohns Colitis. 2022;16:179-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 190] [Article Influence: 47.5] [Reference Citation Analysis (1)] |
| 32. | Turner D, Ricciuto A, Lewis A, D'Amico F, Dhaliwal J, Griffiths AM, Bettenworth D, Sandborn WJ, Sands BE, Reinisch W, Schölmerich J, Bemelman W, Danese S, Mary JY, Rubin D, Colombel JF, Peyrin-Biroulet L, Dotan I, Abreu MT, Dignass A; International Organization for the Study of IBD. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology. 2021;160:1570-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 473] [Cited by in RCA: 1950] [Article Influence: 390.0] [Reference Citation Analysis (1)] |
| 33. | Bischoff SC, Bager P, Escher J, Forbes A, Hébuterne X, Hvas CL, Joly F, Klek S, Krznaric Z, Ockenga J, Schneider S, Shamir R, Stardelova K, Bender DV, Wierdsma N, Weimann A. ESPEN guideline on Clinical Nutrition in inflammatory bowel disease. Clin Nutr. 2023;42:352-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 184] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 34. | Shah H, Zezos P. Pouchitis: diagnosis and management. Curr Opin Gastroenterol. 2020;36:41-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | Lee KE, Cantrell S, Shen B, Faye AS. Post-operative prevention and monitoring of Crohn's disease recurrence. Gastroenterol Rep (Oxf). 2022;10:goac070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 36. | Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, Barrett KJ, Davies RJ, Bennett C, Gittens S, Dunlop MG, Faiz O, Fraser A, Garrick V, Johnston PD, Parkes M, Sanderson J, Terry H; IBD guidelines eDelphi consensus group, Gaya DR, Iqbal TH, Taylor SA, Smith M, Brookes M, Hansen R, Hawthorne AB. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1-s106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1929] [Cited by in RCA: 1718] [Article Influence: 245.4] [Reference Citation Analysis (0)] |
| 37. | Lewis JD, Abreu MT. Diet as a Trigger or Therapy for Inflammatory Bowel Diseases. Gastroenterology. 2017;152:398-414.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 276] [Article Influence: 30.7] [Reference Citation Analysis (1)] |
| 38. | Ghishan FK, Kiela PR. Vitamins and Minerals in Inflammatory Bowel Disease. Gastroenterol Clin North Am. 2017;46:797-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 39. | Limketkai BN, Akobeng AK, Gordon M, Adepoju AA. Probiotics for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2020;7:CD006634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (1)] |
| 40. | Parker EA, Roy T, D'Adamo CR, Wieland LS. Probiotics and gastrointestinal conditions: An overview of evidence from the Cochrane Collaboration. Nutrition. 2018;45:125-134.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 41. | Derwa Y, Gracie DJ, Hamlin PJ, Ford AC. Systematic review with meta-analysis: the efficacy of probiotics in inflammatory bowel disease. Aliment Pharmacol Ther. 2017;46:389-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 268] [Article Influence: 29.8] [Reference Citation Analysis (1)] |
| 42. | Braithwaite E, Carbonell J, Kane JS, Gracie D, Selinger CP. Patients' perception of colonoscopy and acceptance of colonoscopy based IBD related colorectal cancer surveillance. Expert Rev Gastroenterol Hepatol. 2021;15:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 43. | Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, Calabrese E, Baumgart DC, Bettenworth D, Borralho Nunes P, Burisch J, Castiglione F, Eliakim R, Ellul P, González-Lama Y, Gordon H, Halligan S, Katsanos K, Kopylov U, Kotze PG, Krustinš E, Laghi A, Limdi JK, Rieder F, Rimola J, Taylor SA, Tolan D, van Rheenen P, Verstockt B, Stoker J; European Crohn’s and Colitis Organisation [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR]. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1242] [Cited by in RCA: 1317] [Article Influence: 188.1] [Reference Citation Analysis (2)] |
| 44. | Sturm A, Maaser C, Calabrese E, Annese V, Fiorino G, Kucharzik T, Vavricka SR, Verstockt B, van Rheenen P, Tolan D, Taylor SA, Rimola J, Rieder F, Limdi JK, Laghi A, Krustiņš E, Kotze PG, Kopylov U, Katsanos K, Halligan S, Gordon H, González Lama Y, Ellul P, Eliakim R, Castiglione F, Burisch J, Borralho Nunes P, Bettenworth D, Baumgart DC, Stoker J; European Crohn’s and Colitis Organisation [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR]. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD scores and general principles and technical aspects. J Crohns Colitis. 2019;13:273-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 331] [Article Influence: 47.3] [Reference Citation Analysis (1)] |
| 45. | Barberio B, Segal JP, Quraishi MN, Black CJ, Savarino EV, Ford AC. Efficacy of Oral, Topical, or Combined Oral and Topical 5-Aminosalicylates, in Ulcerative Colitis: Systematic Review and Network Meta-analysis. J Crohns Colitis. 2021;15:1184-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 46. | Qiu X, Ma J, Wang K, Zhang H. Chemopreventive effects of 5-aminosalicylic acid on inflammatory bowel disease-associated colorectal cancer and dysplasia: a systematic review with meta-analysis. Oncotarget. 2017;8:1031-1045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 47. | Baehler C, Brüngger B, Blozik E, Vavricka SR, Schoepfer AM. Real-World Data on Topical Therapies and Annual Health Resource Utilization in Hospitalized Swiss Patients with Ulcerative Colitis. Inflamm Intest Dis. 2019;4:144-153. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Yanai S, Toya Y, Nakamura S, Matsumoto T. Patients' Preference of Topical Therapy for Ulcerative Colitis in Japan: A Web-based 3T Survey. Crohns Colitis 360. 2020;2:otaa030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 49. | Loew BJ, Siegel CA. Foam preparations for the treatment of ulcerative colitis. Curr Drug Deliv. 2012;9:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 50. | Ingram JR, Rhodes J, Evans BK, Newcombe RG, Thomas GA. Comparative study of enema retention and preference in ulcerative colitis. Postgrad Med J. 2005;81:594-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 51. | Foulon A, Chevreau J, Yzet C, Gondry J, Fumery M. IBD and pregnancy: From conception to birth. Gynecol Obstet Fertil Senol. 2020;48:514-519. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 52. | Gaidos JK, Kane SV. Managing IBD Therapies in Pregnancy. Curr Treat Options Gastroenterol. 2017;15:71-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Gawron LM, Goldberger AR, Gawron AJ, Hammond C, Keefer L. Disease-related pregnancy concerns and reproductive planning in women with inflammatory bowel diseases. J Fam Plann Reprod Health Care. 2015;41:272-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 54. | Torres J, Chaparro M, Julsgaard M, Katsanos K, Zelinkova Z, Agrawal M, Ardizzone S, Campmans-Kuijpers M, Dragoni G, Ferrante M, Fiorino G, Flanagan E, Gomes CF, Hart A, Hedin CR, Juillerat P, Mulders A, Myrelid P, O'Toole A, Rivière P, Scharl M, Selinger CP, Sonnenberg E, Toruner M, Wieringa J, Van der Woude CJ. European Crohn's and Colitis Guidelines on Sexuality, Fertility, Pregnancy, and Lactation. J Crohns Colitis. 2023;17:1-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 173] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 55. | Higashiyama M, Hokaria R. New and Emerging Treatments for Inflammatory Bowel Disease. Digestion. 2023;104:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 83] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 56. | Núñez P, Quera R, Yarur AJ. Safety of Janus Kinase Inhibitors in Inflammatory Bowel Diseases. Drugs. 2023;83:299-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 65] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 57. | Gordon H, Biancone L, Fiorino G, Katsanos KH, Kopylov U, Al Sulais E, Axelrad JE, Balendran K, Burisch J, de Ridder L, Derikx L, Ellul P, Greuter T, Iacucci M, Di Jiang C, Kapizioni C, Karmiris K, Kirchgesner J, Laharie D, Lobatón T, Molnár T, Noor NM, Rao R, Saibeni S, Scharl M, Vavricka SR, Raine T. ECCO Guidelines on Inflammatory Bowel Disease and Malignancies. J Crohns Colitis. 2023;17:827-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 204] [Reference Citation Analysis (0)] |
| 58. | Keller DS, Windsor A, Cohen R, Chand M. Colorectal cancer in inflammatory bowel disease: review of the evidence. Tech Coloproctol. 2019;23:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 59. | Kucharzik T, Ellul P, Greuter T, Rahier JF, Verstockt B, Abreu C, Albuquerque A, Allocca M, Esteve M, Farraye FA, Gordon H, Karmiris K, Kopylov U, Kirchgesner J, MacMahon E, Magro F, Maaser C, de Ridder L, Taxonera C, Toruner M, Tremblay L, Scharl M, Viget N, Zabana Y, Vavricka S. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J Crohns Colitis. 2021;15:879-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 315] [Article Influence: 63.0] [Reference Citation Analysis (32)] |
| 60. | Honap S, Netter P, Danese S, Peyrin-Biroulet L. An update on the safety of long-term vedolizumab use in inflammatory bowel disease. Expert Opin Drug Saf. 2023;22:767-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 61. | Massano A, Bertin L, Zingone F, Buda A, Visaggi P, Bertani L, de Bortoli N, Fassan M, Scarpa M, Ruffolo C, Angriman I, Bezzio C, Casini V, Ribaldone DG, Savarino EV, Barberio B. Extraintestinal Cancers in Inflammatory Bowel Disease: A Literature Review. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 62. | Russell MD, Stovin C, Alveyn E, Adeyemi O, Chan CKD, Patel V, Adas MA, Atzeni F, Ng KKH, Rutherford AI, Norton S, Cope AP, Galloway JB. JAK inhibitors and the risk of malignancy: a meta-analysis across disease indications. Ann Rheum Dis. 2023;82:1059-1067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 93] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 63. | Poullenot F, Laharie D. Management of Inflammatory Bowel Disease in Patients with Current or Past Malignancy. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 64. | Turpin W, Goethel A, Bedrani L, Croitoru Mdcm K. Determinants of IBD Heritability: Genes, Bugs, and More. Inflamm Bowel Dis. 2018;24:1133-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 127] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 65. | Gearry RB. IBD and Environment: Are There Differences between East and West. Dig Dis. 2016;34:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 66. | Torres J, Gomes C, Jensen CB, Agrawal M, Ribeiro-Mourão F, Jess T, Colombel JF, Allin KH, Burisch J. Risk Factors for Developing Inflammatory Bowel Disease Within and Across Families with a Family History of IBD. J Crohns Colitis. 2023;17:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 67. | Mesko B. The ChatGPT (Generative Artificial Intelligence) Revolution Has Made Artificial Intelligence Approachable for Medical Professionals. J Med Internet Res. 2023;25:e48392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 66] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 68. | De Angelis L, Baglivo F, Arzilli G, Privitera GP, Ferragina P, Tozzi AE, Rizzo C. ChatGPT and the rise of large language models: the new AI-driven infodemic threat in public health. Front Public Health. 2023;11:1166120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 246] [Article Influence: 82.0] [Reference Citation Analysis (0)] |
| 69. | Aubignat M, Diab E. Artificial intelligence and ChatGPT between worst enemy and best friend: The two faces of a revolution and its impact on science and medical schools. Rev Neurol (Paris). 2023;179:520-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: United European Gastroenterology; Società Italiana Di Gastroenterologia Ed Endoscopia Digestiva.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tu JY, China; Zhu L, China S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY