Published online Jan 28, 2023. doi: 10.3748/wjg.v29.i4.758
Peer-review started: August 3, 2022
First decision: November 17, 2022
Revised: December 1, 2022
Accepted: January 3, 2023
Article in press: January 3, 2023
Published online: January 28, 2023
Processing time: 170 Days and 12.2 Hours
Corticosteroids and anti-tumor necrosis factor α mAbs are widely used to treat Crohn's disease (CD). However, one disadvantage of this treatment is impairment of normal immune function, leading to an increased risk of infection. Cryptococcus infection is an opportunistic infection that occurs mainly in immunocompromised patients and poses a significant diagnostic challenge in patients with CD.
Here, we report three cases of pulmonary cryptococcosis in patients with CD after receiving immunomodulatory treatment. The patients presented with no or mild respiratory symptoms. Chest computed tomography scans revealed pulmonary nodules in the unilateral or bilateral lobes. Diagnoses were made using path
The incidence of cryptococcus infection has increased along with immunomodulator use. Clinical vigilance is required for early identification and standardized treatment.
Core Tip: Corticosteroids and anti-tumor necrosis factor α mAbs are commonly used to treat Crohn's disease (CD). However, they may also contribute to an increased risk of opportunistic infections. In this article, we report three cases of pulmonary cryptococcosis in patients with CD after receiving immu-nomodulatory treatment. Pathogen identification mainly depends on pathological examination findings, but metagenomics can serve as an alternative tool. Patients with timely diagnosis generally have a good prognosis, but clinical alerts should be raised in those who are elderly and have comorbidities and dissemination phenotype.
- Citation: Fang YF, Cao XH, Yao LY, Cao Q. Pulmonary cryptococcosis after immunomodulator treatment in patients with Crohn’s disease: Three case reports. World J Gastroenterol 2023; 29(4): 758-765
- URL: https://www.wjgnet.com/1007-9327/full/v29/i4/758.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i4.758
Crohn's disease (CD), a chronic inflammatory disease that may involve any part of the digestive tract, is characterized by periodic clinical relapse and remission[1]. Treatment medications include mesalamine, corticosteroids, small-molecule immunosuppressants, and biologics such as mAbs[2]. However, these drugs also affect normal immune function and may contribute to an increased risk of opportunistic infections.
Pulmonary cryptococcosis is a type of subacute or chronic fungal infection caused by the genus Cryptococcus, and is found mostly in immunocompromised patients. It usually presents with isolated pulmonary granulomatous lesions but can also disseminate to other organ systems[3]. Here, we report three cases of pulmonary cryptococcosis in patients with CD who received immunomodulatory treatment, and review previously reported cases. Literature searches were conducted in PubMed, Web of Science and Embase databases using the keywords “Crohn's disease”, “pulmonary cryptococcosis”, and “cryptococcus”. The search was restricted to full-text journal articles and conference abstracts published in English between January 1980 and May 2022. The bibliographies of the included articles were manually reviewed.
Case 1: A 65-year-old man was admitted to a local hospital for recurrent abdominal distension and pain 10 years ago.
Case 2: A 20-year-old man was admitted to our hospital for perianal pain with fever 5 years ago.
Case 3: A 59-year-old man was admitted to a local hospital for recurrent abdominal pain and diarrhea 13 years ago.
Case 1: The patient was referred to our hospital and diagnosed with CD. Before treatment initiation, chest computed tomography (CT) showed small nodules in the bilateral upper lobes with a benign tendency, pulmonary sac in the right upper lobe, and fibrous foci in the right middle lobe and bilateral lower lobes. The patient received four doses of infliximab (IFX; 300 mg) and achieved clinical remission.
Case 2: The patient was diagnosed with CD and was treated with IFX for 2 years (22 doses; 300 mg), which was discontinued due to secondary loss of response. He complained of night sweats and right-sided chest pain during deep breathing.
Case 3: The patient was diagnosed with CD 5 years ago and had been treated with methylprednisolone (MP; 0.75 mg/kg) for 3 years. He complained of productive cough for 1 mo.
Case 2: The carbohydrate antigen 125 (CA-125) level was 54.2 U/mL. The G test, galactomannan (GM) test, and sputum fungal test results were negative.
Case 3: Vitamin B12 and folic acid levels were normal. Hepatitis B virus surface, core and E antibodies, antinuclear antibodies, vasculitis antibodies, sputum acid-fast (AF) staining, bronchoscopic brush cytology, and bronchoalveolar lavage fluid (BALF) cytopathology showed negative findings.
Other laboratory examination results are summarized in Table 1.
| Case | 1 | 2 | 3 |
| WBC count (× 109/L) | 10.0 | 9.4 | 2.5 |
| Neutrophil count (× 109/L) | 8.13 | 8.0 | 1.6 |
| Platelet count (× 109/L) | 305 | 282 | 220 |
| Hemoglobin (g/L) | 120 | 139 | 97 |
| Albumin (g/L) | 34.3 | 42.8 | 12.0 |
| CRP (mg/L) | 23.3 | 17.4 | 34.9 |
| ESR (mm/hr) | 19 | 16 | 14 |
| Tumor markers | Negative | Negative | Negative |
| T-SPOT.TB | Negative | Negative | Weak positive |
| EBV IgM | Negative | Negative | - |
| Cytomegalovirus IgM | Negative | Negative | Negative |
| HIV | Negative | Negative | Negative |
| TPPA test | Negative | Negative | Negative |
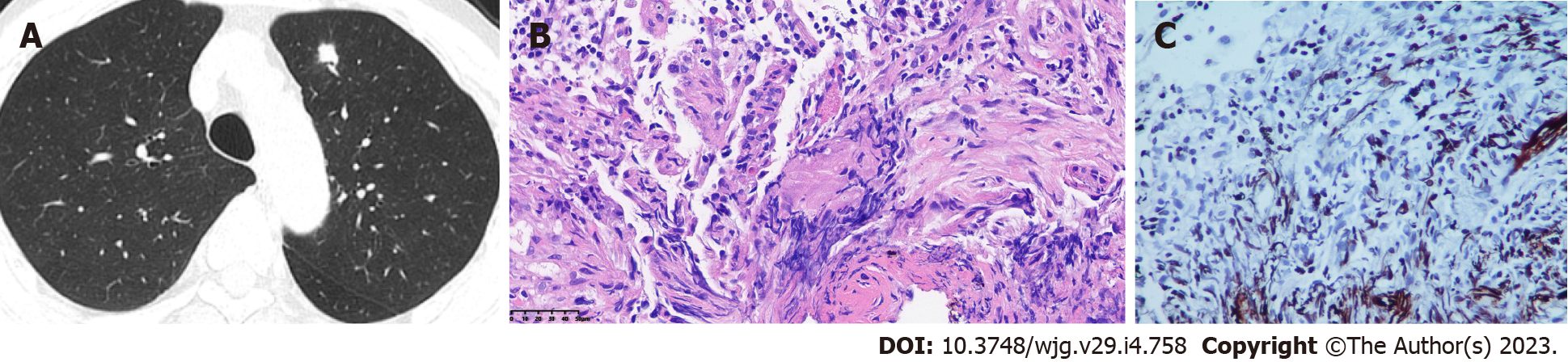
Case 1: A repeat CT scan after the fourth dose of IFX revealed an increased number of bilateral nodules and a large nodule in the left upper lobe with possible inflammation (Fig. 1A). Electromagnetic navigation bronchoscopy revealed a clear trachea and no neoplasm in the principal and segmental bro
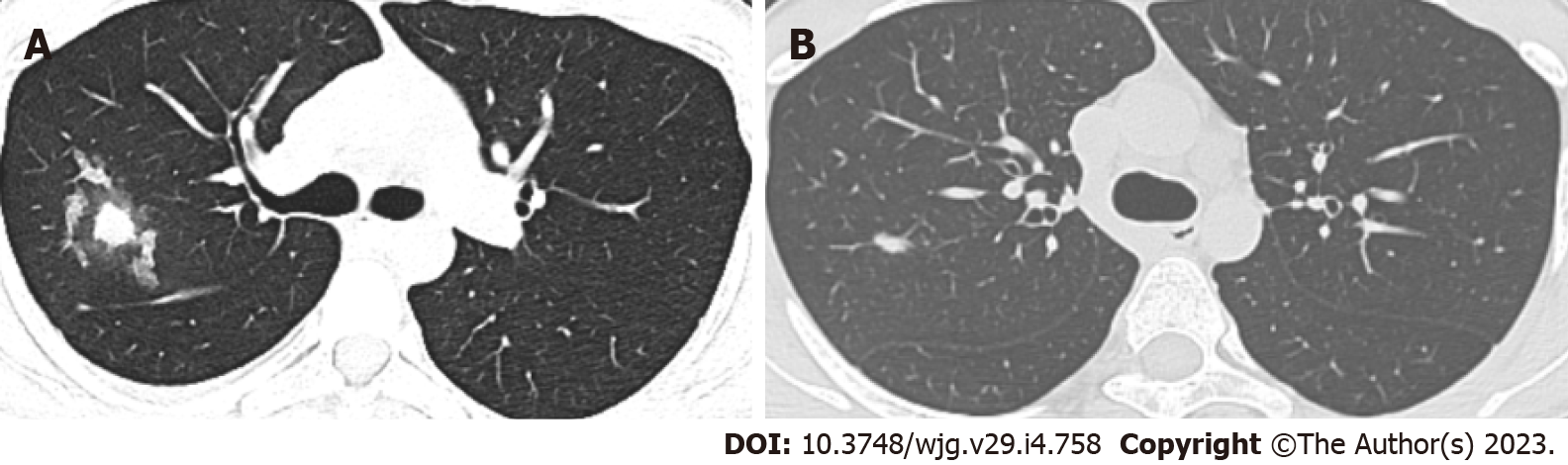
Case 2: Chest CT revealed patchy lesions in the right upper lobe and right interlobar fissure, and multiple bilateral nodules with inflammatory propensity (Figure 2A). Bronchoscopy revealed clear segmental bronchi with no apparent stenosis or neoplasm in the lumen. Fibrinobronchoscopy was performed, and the BALF Aspergillus GM level was 0.840 μg/L. AF staining, fungus, brush cytology, and culture results were negative. BALF was sent for metagenomic sequencing and Cryptococcus was detected.
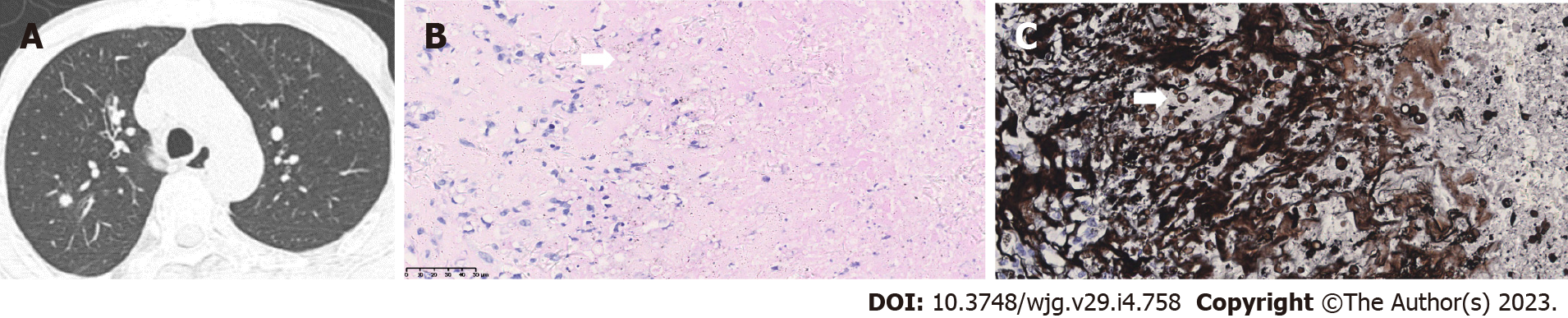
Case 3: Chest CT tomography revealed nodules in the posterior segment of the right upper lobe (Figure 3A). Tumor presence could not be ruled out. Bronchoscopy revealed no neoplasm in bilateral bronchi. Considering the difficulty of bronchoscopic biopsy, thoracoscopic lobectomy of the posterior segment of the right upper lobe was performed. Postoperative pathology revealed negative AF staining results but positive PAS and PASM staining results (Figure 3B and C). Tuberculosis- DNA (TB-DNA) test was negative.
Case 1-3: A diagnosis of CD combined with pulmonary cryptococcosis was confirmed.
Case 1: IFX was discontinued, and the patient was administered fluconazole (FLCZ) 400 mg once daily for 6 mo.
Case 2: Medications for CD were discontinued. The patient was given FLCZ 400 mg once daily for 5 mo.
Case 3: MP was switched to pan-enteral nutrition therapy. The patient was administered FLCZ 400 mg once daily for 1 mo.
Case 1: A chest CT upon completion of anti-fungal therapy showed reduced size of the pulmonary nodule in the left upper lobe.
Case 2: During anti-fungal therapy, the patient was started on thalidomide for CD treatment and reported no apparent abdominal pain. One month after anti-fungal therapy, he achieved symptom resolution, and a repeat chest CT scan showed lesion absorption (Figure 2B).
Case 3: IFX was initiated 7 years later because of the progression of CD. Regular follow-ups have revealed no recurrence so far.
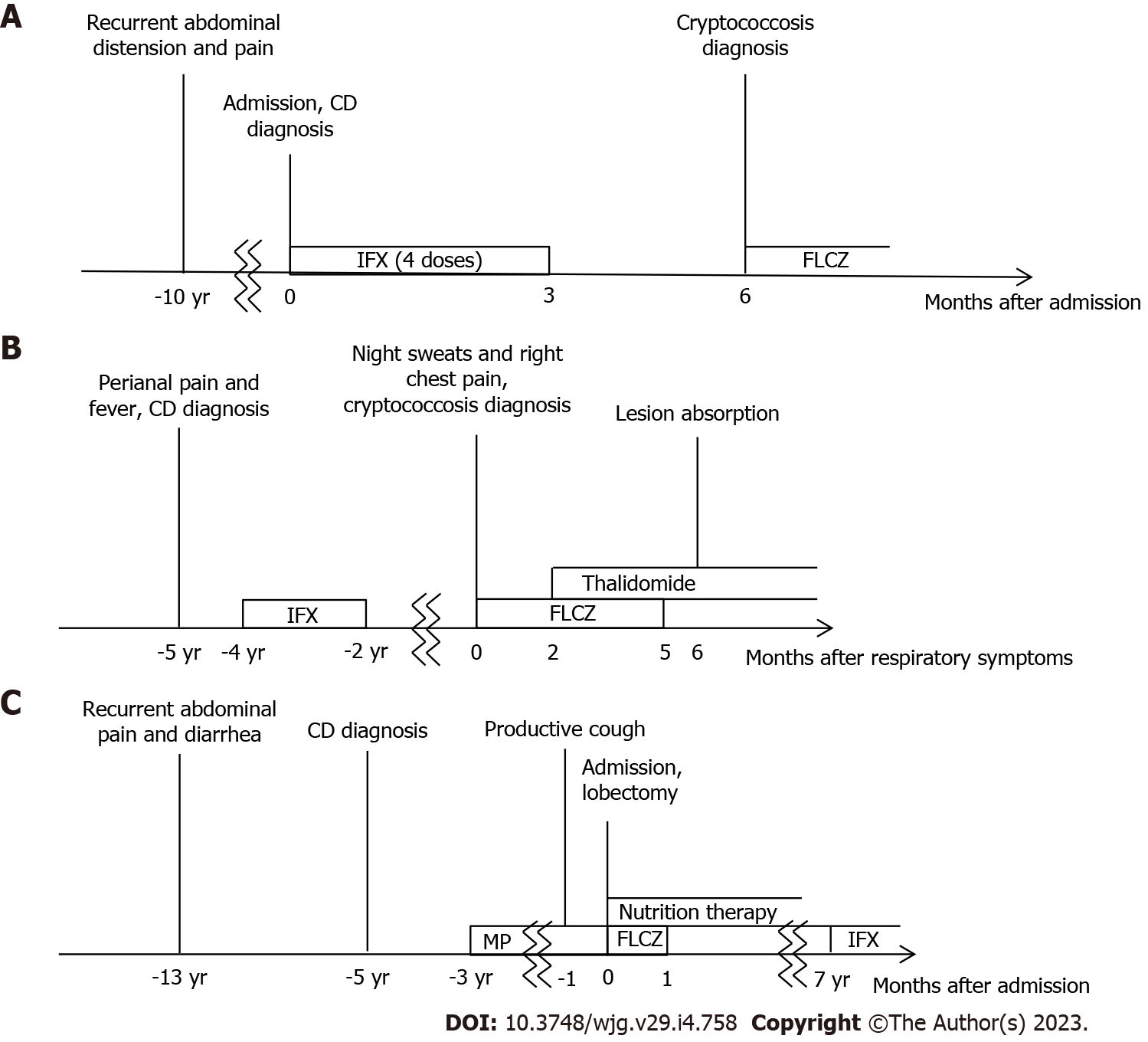
The clinical courses of the three cases are summarized in Figure 4.
Cryptococcus infection is an opportunistic fungal infection caused by Cryptococcus neoformans or Cryptococcus gattii. These pathogens are ubiquitously distributed, with the respiratory tract being the primary portal of entry. Cryptococcosis often occurs in immunocompromised individuals, such as human immunodeficiency virus-infected patients, organ transplant recipients, and those with indications for immunosuppressants[3]. However, it has also been reported in immunocompetent patients[4].
A total of 21 studies reporting CD cases complicated by Cryptococcus infection were identified (Table 2)[4-24]. Among them, one was a retrospective analysis[21] (197 males and 69 females) and another reported relapse of a previously reported case[13]. The remaining 19 patients comprised 13 males and 6 females; 9 of the cases were disseminated cryptococcosis[4,5,8,12,15-19]. Infection sites included lungs (15 cases), central nervous system (CNS; 5 cases), gastrointestinal tract (GI; 3 cases), skin (1 case), omentum (1 case), and pleural fluid and ascites (1 case).
| Ref. | Age/sex | Comorbidity | CD medication | Symptom | Infection site | Treatment | Outcome |
| Lerner et al[5], 1988 | 65/M | Ankylosing spondylitis | Prednisone | Calf ulcer | Lungs, skin | AmB, 5FC | Died |
| Hrnicek et al[6], 2003 | 51/M | None | IFX, prednisone, MTX, ciprofloxacin | Cough, fatigue, headache, fever, chills | Lungs | Surgery, FLCZ | Recovered |
| Rehman et al[7], 2008 | 61/M | None | IFX, prednisone, budesonide, AZA | None | Lungs | AmB, 5FC → FLCZ | Recovered |
| Osawa et al, 2010[8] | 53/M | Silicosis | IFX, prednisone, AZA | Abdominal pain, diarrhea, fever, night sweats, headache | Lungs, GI, CNS | AmB → LAmB, 5FC → FLCZ | Recovered |
| Sciaudone et al[4], 2011 | 26/F | None | None | Diarrhea, abdominal pain, weight-loss, headache, cough | Lungs, GI | Surgery, LAmB → FLCZ | Recovered |
| Hirai et al[9], 2011 | 39/M | None | IFX | None | Lungs | Surgery | Recovered |
| Takazono et al[10], 2012 | 35/M | None | IFX, prednisolone, mesalazine | Fever | Lungs | FLCZ | Recovered |
| Fraison et al[11], 2013 | 54/M | Ankylosing spondylitis | ADM, AZA | Fever, anorexia, cough, chest pain, dyspnea, arthralgia, myalgia | Lungs | LAmB, 5FC → FLCZ | Recovered |
| Wysocki et al[12], 2015 | 46/M | None | IFX, AZA →ADM →CZP | Abdominal and back pain, fever, headache | Omentum, CNS | LAmB, 5FC | Recovered |
| Takazono et al[13], 2016 | 35/M | None | IFX, prednisolone | Fever, fatigue, night sweats | Lungs | FLCZ → ITCZ | Recovered |
| Zhou et al[14], 2016 | 66/M | Cryptogenic organizing pneumonia | Prednisone | Dyspnea, cough | Lungs | FLCZ | Recovered |
| Saad et al[15], 2016 | 71/M | None | IFX, AZA | Meningitis | CNS | - | - |
| Vasant et al[16], 2016 | 74/F | Posterior reversible encephalopathy syndrome | IFX, prednisolone | Headache, confusion, fever, rigor, body ache | CNS | LAmB, 5FC → VRCZ | Died |
| Lee et al[17], 2017 | 70/F | Klebsiella pneumoniae and Pneumocystis jiroveci infections | IFX | Pyrexia | CNS | AmB → VRCZ | Died |
| Chavapradit et al[18], 2018 | 64/F | None | Prednisolone, AZA, mesalazine | Abdominal pain, diarrhea | Lungs, GI | AmB → FLCZ | Recovered |
| Maleb et al[19], 2019 | 45/M | None | Steroid, AZA | Shock, abundance of ascites, fever | Pleural fluid, ascites | FLCZ | Died |
| Santo et al[20], 2019 | 23/M | Tuberculosis | IFX, AZA | Fever, headache | Lungs | FLCZ | Recovered |
| Yeh et al[22], 2021 | 57/F | Systemic lupus erythematosus | ADM, prednisolone, mesalazine | Pneumonia | Lungs | AmB, 5FC | Recovered |
| Hussein et al[23], 2021 | 54/M | None | IFX, prednisolone, MTX | Fever, fatigue, cough | Lungs | FLCZ | Recovered |
| Yeoh et al[24], 2022 | 52/F | Autoimmune hepatitis | Prednisolone | Dyspnea, chest pain, cough, lethargy | Lungs | Surgery | Recovered |
Infected patients had been treated with different combinations of CD drugs, including anti-tumor necrosis factor α (TNF-α) agents, such as IFX, adalimumab and certolizumab pegol, corticosteroids, and other immunosuppressants. Symptoms ranged from asymptomatic lung granulomas to severe pneumonia. Patients with disseminated cryptococcosis may also present with symptoms of other organ systems, such as colitis[8], meningitis[12], or skin ulcers[5]. Chest imaging typically revealed single or multiple pulmonary nodules. Diagnosis mainly relies on pathological examination, with accessory methods including fungal culture and the cryptococcal polysaccharide capsular antigen test. The most commonly used anti-fungal medications are amphotericin B (AmB), liposomal AmB (LAmB), 5-flucytosine (5FC), FLCZ, itraconazole, and voriconazole. Patients with mild symptoms generally recovered after treatment with triazole, while AmB and 5FC were intended for deep fungal infections; however, AmB and LAmB may cause serious adverse events[4,8]. Patients with disseminated cryptococcosis have a relatively poor prognosis, particularly when the CNS is involved.
Anti-TNF-α antibodies have been widely administered among CD patients with high efficacy, but concerns remain regarding their immunogenicity, skin toxicity, and increased risk of infection, such as the possible activation of latent TB. Therefore, current guidelines suggest that TB screening should be conducted before medication infusion[25]. TNF-α also plays a role in clearing pulmonary Cryptococcus infections by inducing interleukin-12 and interferon γ to promote a T1-cell-mediated immune response[26]. Anti-TNF-α agents, among other immunomodulators, may interfere with this process and increase the risk of Cryptococcus infection.
In this paper, we report three male patients diagnosed with CD, aged 20–65 years, who developed pulmonary cryptococcosis after being treated with anti-TNF-α agents or corticosteroids. The patients presented with asymptomatic or mild pneumonia with pulmonary nodules. One patient (case 2) showed elevated CA-125 level, which might be due to intestinal inflammation. G test and GM test were both negative, possibly because of low sensitivity of the tests for Cryptococcus. One patient (case 3) underwent surgery because of difficulty in biopsy. Diagnosis depended on postoperative pathological examinations since BALF might fail to detect Cryptococcus. All patients achieved symptom resolution after FLCZ treatment, consistent with other studies[6,10,23].
CD complicated with pulmonary cryptococcosis is relatively rare, but its incidence has increased in recent years with the use of various immunomodulators, particularly biologics, in CD management. Diagnosis is challenging because clinical symptoms and chest imaging both lack specificity, and GI manifestations can resemble CD progression, leading to misdiagnosis. Therefore, high clinical vigilance is required for early identification of infection, discontinuation of immunomodulators, and standardized treatment.
Our three case reports and literature review suggest that patients with timely diagnosis generally have a good prognosis. However, comorbidities, advanced age, and dissemination phenotype should raise clinical alerts. Metagenomic sequencing can be an alternative approach for pathogen diagnosis when biopsy is unfeasible.
| 1. | Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG Clinical Guideline: Management of Crohn's Disease in Adults. Am J Gastroenterol. 2018;113:481-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 1021] [Article Influence: 127.6] [Reference Citation Analysis (0)] |
| 2. | Adamina M, Bonovas S, Raine T, Spinelli A, Warusavitarne J, Armuzzi A, Bachmann O, Bager P, Biancone L, Bokemeyer B, Bossuyt P, Burisch J, Collins P, Doherty G, El-Hussuna A, Ellul P, Fiorino G, Frei-Lanter C, Furfaro F, Gingert C, Gionchetti P, Gisbert JP, Gomollon F, González Lorenzo M, Gordon H, Hlavaty T, Juillerat P, Katsanos K, Kopylov U, Krustins E, Kucharzik T, Lytras T, Maaser C, Magro F, Marshall JK, Myrelid P, Pellino G, Rosa I, Sabino J, Savarino E, Stassen L, Torres J, Uzzan M, Vavricka S, Verstockt B, Zmora O. ECCO Guidelines on Therapeutics in Crohn's Disease: Surgical Treatment. J Crohns Colitis. 2020;14:155-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 385] [Article Influence: 64.2] [Reference Citation Analysis (0)] |
| 3. | Maziarz EK, Perfect JR. Cryptococcosis. Infect Dis Clin North Am. 2016;30:179-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 492] [Article Influence: 49.2] [Reference Citation Analysis (0)] |
| 4. | Sciaudone G, Pellino G, Guadagni I, Somma A, D'Armiento FP, Selvaggi F. Disseminated Cryptococcus neoformans infection and Crohn's disease in an immunocompetent patient. J Crohns Colitis. 2011;5:60-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Lerner EA, Kibbi AG, Haas A. Calf ulcer in an immunocompromised host. Cryptococcosis. Arch Dermatol. 1988;124:430-431, 433. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Hrnicek M J, Young R L. Immunomodulatory therapy in Crohn's disease as a cause of Cryptococcus neoformans pneumonia. Am J Gastroenterol. 2003;98:S162. [DOI] [Full Text] |
| 7. | Rehman T, Ali J, Lopez FA. A 61-year-old man with asymptomatic, bilateral lung masses. J La State Med Soc. 2008;160:309-349. [PubMed] |
| 8. | Osawa R, Singh N. Colitis as a manifestation of infliximab-associated disseminated cryptococcosis. Int J Infect Dis. 2010;14:e436-e440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Hirai F, Matsui T, Ishibashi Y, Higashi D, Futami K, Haraoka S, Iwashita A. Asymptomatic pulmonary cryptococcosis in a patient with Crohn's disease on infliximab: case report. Inflamm Bowel Dis. 2011;17:1637-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Takazono T, Izumikawa K, Yoshioka S, Matsuo N, Yamakawa M, Suyama N, Kohno S. Possible pulmonary cryptococcosis in a patient with Crohn's disease during anti-tumor necrosis factor-alpha treatment: a case report and literature review. Jpn J Infect Dis. 2012;65:461-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Fraison JB, Guilpain P, Schiffmann A, Veyrac M, Le Moing V, Rispail P, Le Quellec A. Pulmonary cryptococcosis in a patient with Crohn's disease treated with prednisone, azathioprine and adalimumab: exposure to chicken manure as a source of contamination. J Crohns Colitis. 2013;7:e11-e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Wysocki JD, Said SM, Papadakis KA. An uncommon cause of abdominal pain and fever in a patient with Crohn's disease. Gastroenterology. 2015;148:e12-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Takazono T, Sawai T, Tashiro M, Saijo T, Yamamoto K, Imamura Y, Miyazaki T, Suyama N, Izumikawa K, Kakeya H, Yanagihara K, Mukae H, Kohno S. Relapsed Pulmonary Cryptococcosis during Tumor Necrosis Factor α Inhibitor Treatment. Intern Med. 2016;55:2877-2880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Zhou L, Ouyang R, Peng Y. Cryptogenic organizing pneumonia and asymptomatic pulmonary cryptococosis coexisting in a patient with crohn's disease. Chest. 2016;149:A189. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Saad AM, Czul F, Sakuraba A, Rubin DT, Cohen RD. Age of Diagnosis is Associated with Disease Presentation and Therapeutic Complications in Patients with Crohn's Disease. Inflamm Bowel Dis. 2016;22:1027-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Vasant DH, Limdi JK, Borg-Bartolo SP, Bonington A, George R. Posterior Reversible Encephalopathy Syndrome and Fatal Cryptococcal Meningitis After Immunosuppression in a Patient With Elderly Onset Inflammatory Bowel Disease. ACG Case Rep J. 2016;3:e98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lee WS, Azmi N, Ng RT, Ong SY, Ponnampalavanar SS, Mahadeva S, Hilmi I. Fatal infections in older patients with inflammatory bowel disease on anti-tumor necrosis factor therapy. Intest Res. 2017;15:524-528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Chavapradit N, Angkasekwinai N. Disseminated cryptococcosis in Crohn's disease: a case report. BMC Infect Dis. 2018;18:620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Maleb A, Hami A, Lahlou Y B, Lamrabat S, Rifai S, Rahmani N, Bensalah M, Frikh M, Lemnouer A, Elouennass M. Disseminated Cryptococcosis Incorrectly Managed: a Case Report. Journal of Mycology and Infection. 2019;24:28-31. [DOI] [Full Text] |
| 20. | Santo P, Zaltman C, Santos P, Valente F, Costa M, Silveira M, Barroso P. Association of Cryptococcosis and Tuberculosis in a Patient With Crohn's Disease - A Challenging Diagnosis. Am J Gastroenterol. 2019;1141:S29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Mushtaq K, Khan Z, Aziz M, Alyousif ZA, Siddiqui N, Khan MA, Nawras A. Trends and outcomes of fungal infections in hospitalized patients of inflammatory bowel disease: a nationwide analysis. Transl Gastroenterol Hepatol. 2020;5:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Yeh H, Wu RC, Tsai WS, Kuo CJ, Su MY, Chiu CT, Le PH. Systemic lupus erythematosus complicated by Crohn's disease with rectovaginal fistula. BMC Gastroenterol. 2021;21:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 23. | Hussein M, Haq IU, Hameed M, Alabbas A, Hadi HA, Elarabi A, Al-Bozom I. Isolated pulmonary cryptococcosis in a patient with Crohn's disease treated with infliximab: A case report and literature review. Respir Med Case Rep. 2021;33:101459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Yeoh K, McGregor A. Persistent Dyspnea in a Patient with Altered Immune Status. Infectious Diseases in Clinical Practic. 30. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | D'Haens GR, van Deventer S. 25 years of anti-TNF treatment for inflammatory bowel disease: lessons from the past and a look to the future. Gut. 2021;70:1396-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 26. | Herring AC, Lee J, McDonald RA, Toews GB, Huffnagle GB. Induction of interleukin-12 and gamma interferon requires tumor necrosis factor alpha for protective T1-cell-mediated immunity to pulmonary Cryptococcus neoformans infection. Infect Immun. 2002;70:2959-2964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 109] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Said ZNA, Egypt; Wang P, China S-Editor: Liu GL L-Editor: A P-Editor: Liu GL