Published online Jun 7, 2023. doi: 10.3748/wjg.v29.i21.3341
Peer-review started: January 1, 2023
First decision: January 10, 2023
Revised: February 1, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: June 7, 2023
Processing time: 153 Days and 23.5 Hours
The introduction of lumen-apposing metal stents (LAMS) for endoscopic ultrasound (EUS)-guided drainages has marked a turning point in the field of interventional ultrasound and it is gathering worldwide diffusion in different clinical settings. Nevertheless, the procedure may conceal unexpected pitfalls. LAMS misdeployment is the most frequent cause of technical failure and it can be considered a procedure-related adverse event when it hampers the conclusion of the planned procedure or results in significant clinical consequences. Stent misdeployment can be managed successfully by endoscopic rescue maneuvers to allow the completion of the procedure. To date, no standardized indication is available to guide an appropriate rescue strategy depending on the type of procedure or of misdeployment.
To evaluate the incidence of LAMS misdeployment during EUS-guided choledo
We conducted a systematic review of the literature on PubMed by searching for studies published up to October 2022. The search was carried out using the exploded medical subject heading terms “lumen apposing metal stent”, “LAMS”, “endoscopic ultrasound” and “choledochoduodenostomy” or “gallbladder” or “pancreatic fluid collections”. We included in the review on-label EUS-guided procedures namely EUS-CDS, EUS-GBD and EUS-PFC. Only those publications reporting EUS-guided LAMS positioning were considered. The studies reporting a technical success rate of 100% and other procedure-related adverse events were considered to calculate the overall rate of LAMS misdeployment, while studies not reporting the causes of technical failure were excluded. Case reports were considered only for the extraction of data regarding the issues of misdeployment and rescue techniques. The following data were collected from each study: Author, year of publication, study design, study population, clinical indication, technical success, reported number of misdeployment, stent type and size, flange misdeployed and type of rescue strategy.
The overall technical success rate of EUS-CDS, EUS-GBD and EUS-PFC was 93.7%, 96.1%, and 98.1% respectively. Significant rates of LAMS misdeployment have been reported for EUS-CDS, EUS-GBD and EUS-PFC drainage, respectively 5.8%, 3.4%, and 2.0%. Endoscopic rescue treatment was feasible in 86.8%, 80%, and 96.8% of cases. Non endoscopic rescue strategies were required only in 10.3%, 16% and 3.2% for EUS-CDS, EUS-GBD, and EUS-PFC. The endoscopic rescue techniques described were over-the-wire deployment of a new stent through the created fistula tract in 44.1%, 8% and 64.5% and stent-in-stent in 23.5%, 60%, and 12.9%, respectively for EUS-CDS, EUS-GBD, and EUS-PFC. Further therapeutic option were endoscopic rendezvous in 11.8% of EUS-CDS and repeated procedure of EUS-guided drainage in 16.1% of EUS-PFC.
LAMS misdeployment is a relatively common adverse event in EUS-guided drainages. There is no consensus on the best rescue approach in these cases and the choice is often made by the endoscopist relying upon the clinical scenario, anatomical characteristics, and local expertise. In this review, we investigated the misdeployment of LAMS for each of the on-label indications focusing on the rescue therapies used, with the aim of providing useful data for endoscopists and to improve patient outcomes.
Core Tip: Scant data are available about rescue techniques in cases of lumen-apposing metal stents (LAMS) misdeployment which is the main cause of technical failure in endoscopic ultrasound-guided drainage procedures. We performed a systematic review of the literature about LAMS misdeployment and rescue techniques in the biliopancreatic setting, focusing on technical aspects and success rate of endoscopic maneuvers. In accordance with our results endoscopic rescue techniques are feasible in most cases (up to 96.8%). Three endoscopic rescue strategies have been identified. The choice of the endoscopic rescue maneuver is based on the clinical scenario, type of misdeployment and expertise of the endoscopic team.
- Citation: Armellini E, Metelli F, Anderloni A, Cominardi A, Aragona G, Marini M, Pace F. Lumen-apposing-metal stent misdeployment in endoscopic ultrasound-guided drainages: A systematic review focusing on issues and rescue management. World J Gastroenterol 2023; 29(21): 3341-3361
- URL: https://www.wjgnet.com/1007-9327/full/v29/i21/3341.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i21.3341
The progress in interventional endoscopy, particularly in the field of endoscopic ultrasound (EUS), has changed the treatment algorithms for digestive and pancreaticobiliary diseases. The evolution of devices combined with improvements in endoscopic techniques, have allowed access to mini-invasive therapeutic solutions for complex diseases that affect areas beyond the gastrointestinal tract.
Nowadays, interventional EUS can manage local complications of acute pancreatitis[1], drain the biliary tree and gallbladder[2], establish gastrointestinal anastomoses[3], and treat tumors by radiofrequency ablation or injection of substances[4,5]. A paradigmatic example of this evolution is the approach to biliopancreatic drainage. The first EUS-guided transluminal drainage of the biliary tree was performed in 2001. Giovannini et al[6] used a 10-Fr plastic stent to achieve trans-duodenal biliary drainage (BD) under EUS guidance in a patient with a pancreatic head mass after failed endoscopic retrograde cholangiopancreatography (ERCP). Since then, the evolution of EUS-guided drainage has led to the continuous improvement of available devices and of endoscopic techniques. The introduction of self-expanding metal stents (SEMS) and lumen-apposing metal stents (LAMS) for EUS-guided drainage is a turning point in the field of endoscopic drainage. The first transluminal stenting between two nonadherent lumens of the digestive tract using a bi-flanged covered metal stent with lumen-to-lumen apposition property was described by Binmoeller and Shah[7] in an ex vivo model. Itoi et al[8] reported the first use of LAMS in humans, describing the successful treatment of 15 symptomatic pancreatic pseudocysts and five acute cholecystitis cases in patients unfit for surgery.
Itoi and Binmoeller[9] successfully performed the first EUS-guided choledochoduodenostomy (EUS-CDS) with LAMS in a patient with unresectable pancreatic cancer and obstructive jaundice. Prior to that, the technique of LAMS deployment was the same as that of tubular stents (plastic or metal stents), which is a multi-step procedure with device exchanges that are exposed to the risk of adverse events (i.e., loss of the wire and/or scope position, biliary leak). To address this issue, a new LAMS delivery system with an electrocautery tip [electrocautery-enhanced (EC)-LAMS-Hot-Axios, Boston Scientific Corp., Marlborough, Massachusetts, United States] was developed, giving rise to a single-stage technique[10,11]. Presently, two LAMS in different diameters and lengths are commercially available: The Hot Axios stent (Boston Scientific, Marlborough, Mass, United States) and the Hot Spaxus stent (Taewoong Medical Co. Gimpo, Korea), and new LAMS types are on the way. Other fully covered (FC) metal stents are available for similar indications: Aixstent (Leufen Medical, Aachen, Germany), Hanarostent (Mi-TECH-Medical Co, Seoul, South Korea), and NAGI stents (Taewoong Medical Co., Ltd., Ilsan, Korea)[11,12]. These stents are non-cautery and require a multi-step procedure for their insertion. Anyway, LAMS loaded on an EC delivery system require precise execution of some sequential steps (puncture of the target lumen, opening and retraction of the distal flange to the adjacent cavity wall, deployment, and release of the proximal flange) to achieve technical success, which is defined as the correct placement of the stent across the newly created tract.
There are various issues that may occur during LAMS deployment, resulting in stent misdeployment. Unfavorable conditions range from unfamiliarity with the stent to patient movement, angled scope tip or confined space within the gastrointestinal cavity, small diameter of the target lumen[13], and target structure located at a distance of more than 15-20 mm[14]. Stent misdeployment usually results in a full-thickness defect of the gastrointestinal wall, possibly associated with the perforation of the target organ. Prompt identification of this complication is crucial to managing the perforation, possibly completing the procedure, and avoiding major consequences. This paper reviews EUS-guided drainage procedures using LAMS, with a focus on misdeployment and endoscopic rescue therapies.
This systematic review was performed in agreement with PRISMA guidelines. Two independent investigators (Cominardi A and Metelli F) performed a review on PubMed by searching for studies published up to October 2022. The search was limited to English-language articles and human studies, and it was carried out using the exploded medical subject heading terms “lumen apposing metal stent”, “LAMS”, “endoscopic ultrasound” and “choledochoduodenostomy” or “gallbladder” or “pancreatic fluid collections”. We included in the review on-label EUS-guided procedures namely EUS-CDS, EUS-guided gallbladder drainage (EUS-GBD) and EUS-guided pancreatic fluid collections drainage (EUS-PFC). Boolean operators (NOT, AND, OR) were also used in succession to narrow and widen the search.
Both investigators used a standardized data collection form to increase uniformity and reduce bias in reporting. In the case of discrepancy, the investigators resolved the disagreement by discussion with a senior investigator (Armellini E). Only publications on EUS-guided LAMS positioning were considered, whereas studies on drainage with other metallic or plastic stents were excluded. Meta-analysis, review and drainage performed in non-human models were also excluded.
The studies reporting a technical success rate of 100% and other procedure-related adverse events were considered to calculate the overall rate of LAMS misdeployment, while studies not reporting the causes of technical failure were excluded. Case reports were considered only for the extraction of data regarding the issues of misdeployment and rescue techniques.
The full paper of each identified article was retrieved, and references were evaluated to search for potentially missed articles. Data were extracted independently and entered standardized Excel spreadsheet (Microsoft Inc. Redmond, Washington, United States). For EUS-CDS and EUS-PFC drainage the following data were extracted from each study: Year of publication, study design, study population, clinical indication, technical success, reported number of misdeployment, LAMS type and size, flange misdeployed, and type of rescue strategy. For EUS-GBD the following data were collected from each study: Author, year of publication, study design, study population, clinical indication, access to GB (stomach or duodenum), technical success, reported number of misdeployment, LAMS type and size, flange misdeployed, and type of rescue strategy.
Baseline characteristics of study population, EUS-guided procedures, technical details, and procedure outcomes were summarized as means (SD) or medians (with interquartile range and range) for continuous data, and as frequencies and proportions for categorical data. Data were analyzed using the Statistical Package for Social Sciences (SPSS software v. 15.0, Chicago, Illinois, United States) for Windows.
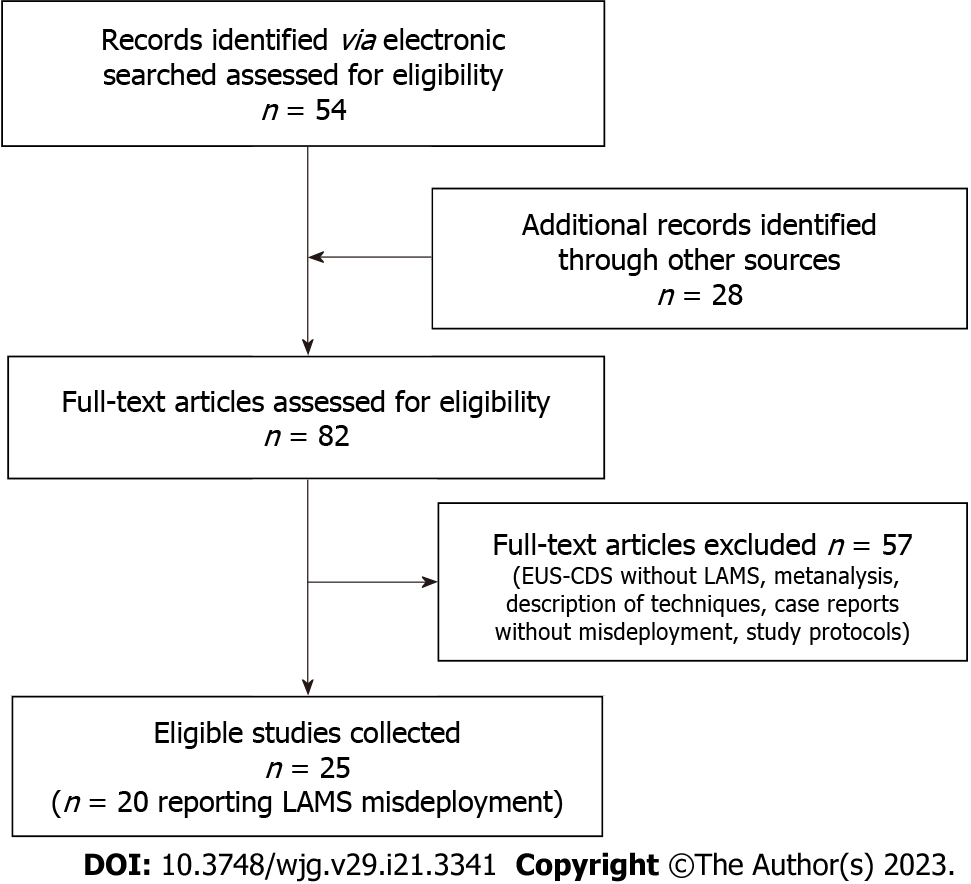
Literature research identified 82 studies that were fully assessed for eligibility in this review. We excluded 57 studies since they did not meet our inclusion criteria. A total of 25 studies were included in our review[15-39]; in 20 studies LAMS misdeployment occurred[20-39] (study flow chart was shown in Figure 1).
A total of 1081 patients underwent EUS-CDS for malignant biliary obstruction (MBO), almost all after failed ERCP. The overall technical success rate of EUS-CDS was 93.7%. Excluding 5 case reports, a total of 63 LAMS misdeployments were reported, with a rate of 5.8%; the study detailed characteristics were summarized in Table 1. Including case reports, an Axios stent was employed in 61 (89.7%) cases of EUS-CDS. Spaxus stent was used in 3 (4.4%) cases. In 4 cases (5.9%) type of stent was not declared. The procedures were performed with a pre-loaded guidewire in 23 (33.8%) cases, without a pre-loaded guidewire in 12 (17.6%) cases, whereas this data was not available in most of cases (48.6%).
| Ref. | Study design | Study population | Clinical indication | Technical success (%) | LAMS misdeployment | LAMS type | Size of LAMS (mm) | Use of guidewire | LAMS flange misdeployed | Rescue therapy |
| Anderloni et al[20], 2019 | Retrospective single center | 46 | MBO | 93.5 | 3 | Hot Axios | - | No | Distal (1/3), not specified (2/3) | Rendezvous technique with transpapillary placement of 10 mm × 40 mm FCSEMS after advancing a guidewire through the existing fistula into the bile duct and then across the papilla (1/3); 10 mm × 10 mm LAMS placement through the existing fistula (1/3); double-pigtail plastic stent placement across the LAMS (1/3) |
| Di Mitri R et al[21], 2022 | Retrospective single center | 31 | MBO | 80.6 | 7 | Hot Axios | 8 mm × 8 mm (6/7) 10 mm × 10 mm (1/7) | Yes | Distal | Over-the-wire FCSEMS placement (5/7); transpapillary percutaneous-transhepatic-endoscopic rendezvous (1/7); transpapillary laparoscopic-endoscopic rendezvous (1/7) |
| Rajadurai et al[22], 2022 | Retrospective multicenter | 66 | MBO | 90.9 | 6 | Hot Axios | - | No (4/6). Yes (2/6) | Distal | Over-the-wire FCSEMS placement (2/6); laparotomy (2/6); EUS-GBD (1/6); palliation due to rapid deterioration (1/6) |
| Jacques et al[23], 2019 | Retrospective multicenter | 52 | MBO | 88.5 | 4 | Hot Axios | - | - | Distal (1/4), proximal (1/4 intraperitoneal, 2/4 intraparietal) | Stent-in-stent strategy with SEMS (1/4); ERCP rendezvous (1/4); repeat classic EUS-CDS with SEMS (2/4) |
| Jacques et al[24], 2020 | Retrospective multicenter | 70 | MBO | 98.6 | 1 | Hot Axios | - | - | No evidence of bile flow even if stent was correctly in situ | Stent-in-stent strategy |
| El Chafic et al[25], 2019 | Retrospective multicenter | 67 | MBO | 95.5 | 2 | Hot Axios | - | Yes | - | Over the same guidewire FCSEMS placement (all) |
| Fugazza et al[26], 2022 | Retrospective multicenter | 256 | MBO | 93.3 | 17 | Hot Axios | - | - | - | Over the guidewire SEMS placement (10/17); deployment of a second LAMS (4/17); EUS-guided rendezvous with subsequent placement of a transpapillary stent (3/17) |
| Hindryckx and Degroote[27], 2021 | Retrospective single center | 13 | - | 92.3 | 1 | Hot Axios | 8 mm × 6 mm | Yes | Distal | Clip closure of duodenal defect and new EUS-CDS with 8 mm × 6 mm LAMS |
| Armellini et al[28], 2023 | Case report | 1 | Difficult biliary lithiasis | - | 1 | Hot Axios | 8 mm × 8 mm | Yes | Distal | Rendezvous technique with transpapillary placement of FCSEMS after advancing a guidewire directly through the LAMS and choledochal breach into the bile duct and then across the papilla |
| Teoh et al[29], 2021 | Prospective multicenter | 26 | MBO | 88.5 | 3 | Cold spaxus | - | Yes | Entirely into the bile duct | Over the guidewire SEMS placement |
| Fugazza et al[30], 2020 | Case report | 1 | Pancreatic adenocarcinoma | - | 1 | Axios | 6 mm × 8 mm | Yes | Proximal | Stent-in-stent strategy using SEMS |
| Brückner et al[31], 2015 | Case series | 5 | MBO | 80 | 1 | Cold Axios | 6 mm × 8 mm | Yes | Distal | Over the guidewire stent placement |
| Vanella et al[32], 2023 | Retrospective study of prospectively maintained databases | 93 | MBO | 97.8 | 4 | Hot Axios | - | No | Distal (2/4); misdeployments after both flanges release (2/4) | Repeat EUS-CDS (1/4); inserting a guidewire through the LAMS catheter followed by over the guidewire LAMS placement (1/4) (the effective rescue therapies were counted as technical success); PTBD (2/4) |
| de Benito Sanz et al[33], 2021 | Retrospective single center | 37 | MBO | 100 | 4 | - | - | - | Distal (2/4); not specified (2/4) | Stent-in-stent strategy (the effective rescue therapies were counted as technical success) |
| Garcia-Sumalla et al[34], 2021 | Retrospective multicenter | 41 | MBO | 95.1 | 2 | Hot Axios | - | - | No evidence of bile flow even if stent was correctly in situ; distal flange | Stent-in-stent strategy using SEMS; rendezvous technique with placement of a transpapillary FCSEMS |
| Sanchez-Ocana et al[35], 2022 | Case report | 1 | Pancreatic adenocarcinoma | - | 1 | Axios | 8 mm × 8 mm | Yes | Distal | EUS-guided gallbladder drainage as a portal for antegrade transcystic guidewire passage, followed by rendezvous ERCP with placement of a biliary metal stent and clips to seal the perforation |
| Graves et al[36], 2021 | Case report | 1 | Pancreatic metastasis of renal cell carcinoma | - | 1 | Axios | 10 mm × 10 mm | No | Distal | A bridging 10 mm × 8 mm FCSEMS was deployed over the guidewire and through theccessing LAMS |
| Chin et al[37], 2020 | Retrospective analysis of a prospectively maintained database | 56 | MBO | 100 | 1 | Axios | - | - | - | Over the guidewire tubular biliary stent placement (the effective rescue therapy was counted as technical success) |
| On et al[38], 2022 | Retrospective multicenter | 120 | MBO | 90.8 | 7 | Hot Axios | - | No (4/7). Yes (3/7) | - | Bridging stents (5/7), PTBD (1/7), conservative management (1/7) |
| Ligresti et al[39], 2018 | Case report | 1 | Pancreatic adenocarcinoma | - | 1 | Axios | 8 mm × 8 mm | Yes | Distal | Reinsertion of the delivery system over the guide wire and second deployment of distal flange into common bile duct under EUS guidance |
In 28 (41.2%) cases the misdeployment of the distal flange was reported, in 4 (5.9%) cases the misdeployment involved the proximal flange, in 3 (4.7%) EUS-CDS LAMS was entirely misdeployed inside the common bile duct (CBD) and in 2 (2.9%) patients no bile flow was observed after LAMS deployment despite no evidence of LAMS misdeployment. The type of misdeployment was not properly described in 31 (45.6%) EUS-CDS. Seven other causes of technical failure were reported in four studies[15,22,24,38]: 1 massive bleeding, 1 inability to puncture the bile duct, 2 duodenal perforations, 1 failure of fistula creation, 1 mechanical failure and 1 patient intolerance. In three studies[31,33,37], the effective rescue therapy after LAMS misdeployment was considered a technical success by the authors and in one study[15] duodenal perforation during dilation of the fistulous tract was the cause of technical failure.
LAMS misdeployment was managed by endoscopy in 86.8% (n = 59/68) cases, while 4.4% (n = 3/68) misdeployment cases were treated by percutaneous transhepatic BD (PTBD), 2.9% (n = 2/68) by rendezvous via PTBD and during surgery, and 2.9% (n = 2/68) by surgery. In 2 cases the procedure was abandoned in favor of supportive therapy. In 44.1% (n = 30/68) cases of LAMS misdeployment, the rescue strategy was LAMS removal followed by over-the-wire deployment of a new stent; in 7 (23.3%) cases a new LAMS was deployed and in 23 (76.7%) cases a SEMS was used.
The stent-in-stent technique was the treatment of choice in 16 (23.5%) cases of misdeployment; in 7 (43.7%) cases SEMS was used, in 1 (6.3%) a plastic stent and in 8 (50%) the stent type was not specified. In 8 (11.8%) cases rendezvous procedure was performed by EUS/endoscopic technique. EUS-CDS was repeated in 4 (5.9%) cases. In 1 (1.5%) case EUS-GBD was used as a rescue strategy (see Table 2).
| EUS-CDS | |
| Deployment of a new stent through the created fistula tract | 44.1% |
| Stent-in-stent strategy | 23.5% |
| Endoscopic rendezvous | 11.8% |
| Non-endoscopic rescue strategies | 10.3% |
| EUS-GBD | |
| Stent-in-stent strategy | 60% |
| Clip closure of gastrointestinal wall defect | 13% |
| Deployment of a new stent through the created fistula tract | 8% |
| Non-endoscopic rescue strategies | 16% |
| EUS-PFC | |
| Deployment of a new stent through the created fistula tract | 64.5% |
| Repeated EUS-guided drainage | 16.1% |
| Stent-in-stent strategy | 12.9% |
| Non-endoscopic rescue strategies | 3.2% |
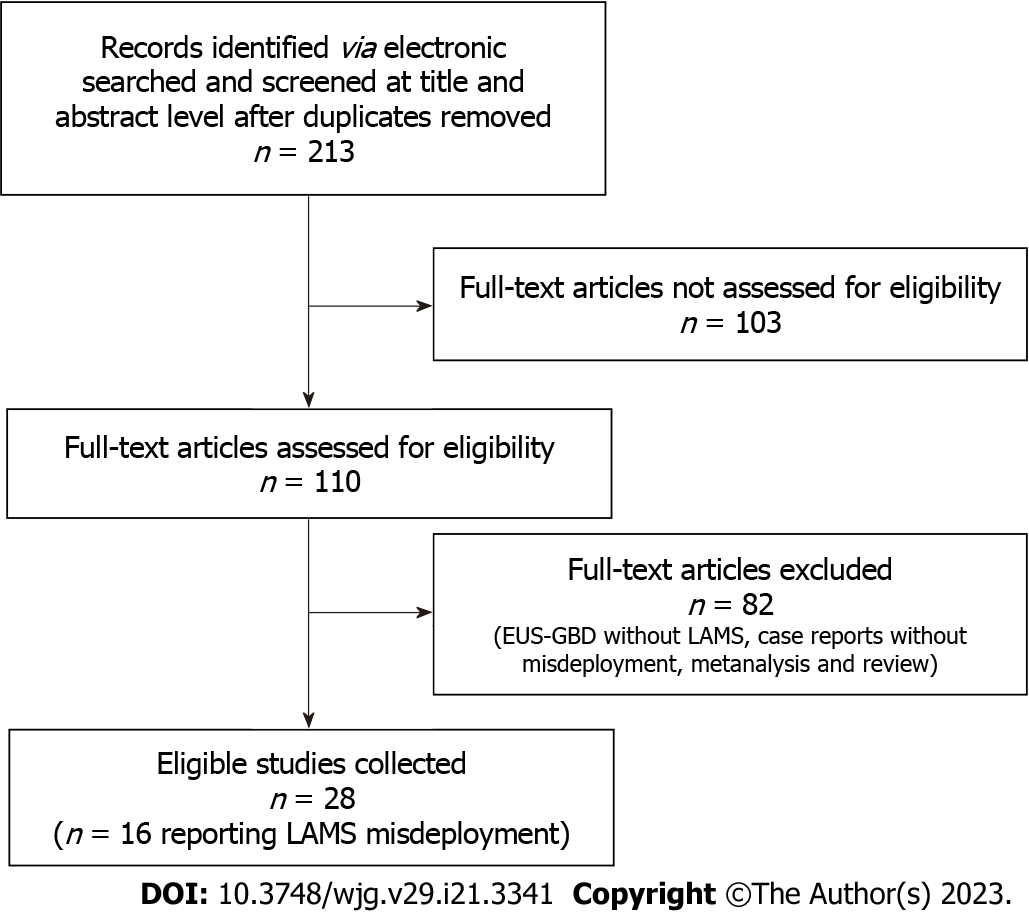
We identified 213 studies using our search strategy; 185 studies were excluded since they did not meet inclusion criteria. A total of 28 studies reported cases of EUS-GBD[8,22,29,37,40-63] including 16 studies in which LAMS misdeployment occurred[22,29,50-63]. The study flow chart is shown in Figure 2.
A total of 667 patients underwent EUS-GBD for acute cholecystitis since they were unfit for surgery. Only in one study patients were treated by EUS-GBD for unsuccessful BD with ERCP[60]. Studies characteristics are summarized in Table 3. The overall technical success of EUS-GBD was 96.1%. Excluding two case reports, we identified 23 LAMS misdeployments among patients who underwent EUS-GBD, with a rate of 3.4%. In 19/25 (76%) cases an Axios stent was employed for EUS-GBD, while a Spaxus stent was used in the remaining 6/25 (24%) cases.
| Ref. | Study design | Study population | Clinical indication | Access to GB | Technical success (%) | LAMS maldeployment | LAMS type | Size of LAMS (mm) | LAMS flange misdeployed | Rescue therapy |
| Ngamruengphong et al[50], 2015 | Case report | 1 | Cholecysto-choledocal lithiasis | Duodenum | - | 1 | Hot Axios | - | Proximal | Stent-in-stent strategy using SEMS |
| Rajadurai et al[22], 2022 | Retrospective multicenter | 49 | - | Duodenum | 95.7 | 2 | Hot Axios | 10 mm × 10 mm; 15 mm × 10 mm | Distal | Closure of the defect with clip; palliation (no further endoscopic treatment) |
| Cho et al[51], 2019 | Prospective single center | 22 | Acute cholecystitis unfit for surgery | - | 95.5 | 1 | Spaxus | 10 mm × 20 mm | Proximal | Stent-in-stent strategy using SEMS |
| Walter et al[52], 2016 | Prospective multicenter | 30 | Acute cholecystitis unfit for surgery | Stomach | 90 | 3 | Hot Axios | Stent-in-stent strategy using SEMS | ||
| Irani et al[53], 2015 | Retrospective multicenter | 15 | Acute cholecystitis unfit for surgery | Duodenum | 93 | 1 | Axios | 10 mm × 10 mm | Distal | Stent-in-stent strategy using SEMS |
| de la Serna-Higuera et al[54], 2013 | Prospective single center | 13 | Acute cholecystitis unfit for surgery | Stomach | 84.6 | 1 | Axios | 10 mm × 10 mm | Distal | Closure of the defect with clip (no further endoscopic treatment) |
| Dollhopf et al[55], 2017 | Retrospective multicenter | 75 | Acute cholecystitis unfit for surgery | Stomach | 98.7 | 1 | Hot-Axios | 10 mm × 10 mm | Proximal | Surgery |
| Teoh et al[56], 2017 | Retrospective multicenter | 59 | Acute cholecystitis unfit for surgery | - | 96.6 | 1 | Axios | 10 mm × 10 mm | Distal | Surgery |
| Mangiavillano et al[57], 2021 | Retrospective multicenter | 18 | Acute cholecystitis unfit for surgery | - | 83.3 | 1 | Spaxus | Distal | Closure of the defect with clip followed by transpapillary stent placment | |
| Teoh et al[29], 2021 | Retrospective multicenter | 27 | Acute cholecystitis unfit for surgery | - | 88.9 | 2 | Spaxus | 10 mm × 10 mm; 16 | Proximal | Stent-in-stent strategy using SEMS |
| Higa et al[58], 2019 | Retrospective single center | 40 | Acute cholecystitis unfit for surgery | - | 97.5 | 2 | Hot Axios | 10 mm × 10 mm; 15 mm × 10 mm | Distal | Redeployment of a new LAMS |
| Garg et al[59], 2018 | Case report | 1 | Acute cholecystitis unfit for surgery | Stomach | - | 1 | Hot Axios | 10 mm × 10 mm | Distal | Stent-in-stent strategy using SEMS |
| Torres Yuste et al[60], 2020 | Retrospective single center | 34 | Acute cholecystitis unfit for surgery | - | 97.1 | 3 | Axios | 10 mm × 10 mm; 15 mm × 10 mm | Distal | Stent-in-stent strategy using SEMS (2/3); double pig-tail plastic stent in LAMS (1/3) |
| 37 | - | 97.3 | 1 | Axios | 10 mm × 10 mm; 15 mm × 10 mm | Proximal | Stent-in-stent strategy using SEMS | |||
| James et al[61], 2019 | Retrospective multicenter | 15 | Acute cholecystitis unfit for surgery | Stomach | 93.3 | 1 | Axios | 10 mm × 10 mm; 15 mm × 10 mm | Proximal | Surgery |
| Irani et al[62],2017 | Retrospective multicenter | 45 | Acute cholecystitis unfit for surgery | - | 97.8 | 1 | Axios | - | Distal | Stent-in-stent strategy using SEMS |
| Cho et al[63], 2020 | Retrospective multicenter | 36 | Acute cholecystitis, advanced malignancy unfit for surgery | - | 94.4 | 2 | Spaxus | - | Proximal | Stent-in-stent strategy using SEMS, emergent PTC |
Only 8 studies reported if the GB was accessed from the stomach (n = 7/11, 63.6%) or duodenum (n = 4/11, 36.4%)[22,51-55,59,61]. The misdeployment of the proximal flange occurred in 9/25 (36%) cases, while the distal flange was misdeployed in 16/25 (64%) cases. The use of a guidewire was reported in 16/25 (64%) cases of misdeployment. Endoscopic management was the treatment of choice in 21/25 (84%) cases of LAMS misdeployment during EUS-CDS. In 15 of these 25 (60%) complicated EUS-GBD collected in our study, the initial failed LAMS deployment was overcome by reinsertion of a FC-SEMS through the LAMS lumen, the so-called “stent-in-stent” strategy; only in 1/15 a double pigtail stent was inserted. In 2/25 (8%) cases, the misdeployed stent was removed and a new LAMS was re-deployed over the guidewire across the fistula created during the first attempt for EUS-GBD.
In 3/25 (12%) cases, the LAMS was endoscopically removed, and the gastrointestinal wall perforation was closed by endoscopic clipping followed by transpapillary stent placement in 1 case. No further endoscopic maneuvers were attempted in the remaining 2 cases in favour of supportive care. Surgical management was the therapeutic option in 3/25 (12%) cases of misdeployment. In 1 (4%) case, emergent percutaneous cholecystostomy was performed after unsuccessful stent-in-stent placement attempt. In 1 (4%) case, palliation was the preferred strategy (see Table 2).
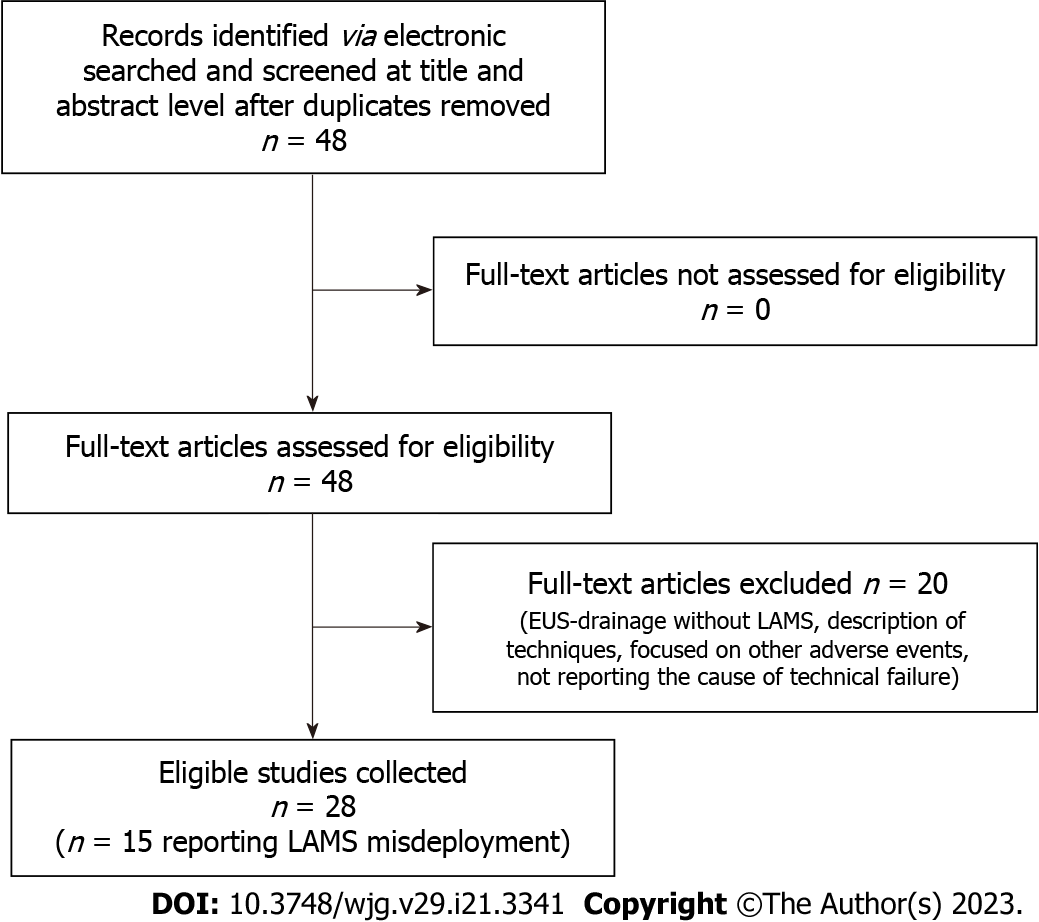
We collected 48 studies from the literature that were fully assessed for eligibility in this review; 20 studies were excluded since they did not meet our inclusion criteria. A total of 28 studies were included in our review[10,12,57,64-88] including 15 studies in which LAMS misdeployment occurred[10,12,70,77-88] (Figure 3). The overall technical success of EUS-PFC drainage was 98.1%. The cause of technical failure corresponded to LAMS misdeployment in all the studies except in one reporting two cases of technical failure due to a difficult scope position that prevented the advancement of the EC-LAMS device outside the operative channel of the echoendoscope[57]. In 3 cases, the effective rescue therapy by re-insertion of the same LAMS after misdeployment was considered a technical success by the authors[78,79].
Excluding two case reports, we collected 1684 patients who underwent EUS-PFC drainage in which 34 LAMS misdeployments occurred, with a rate of 2.0%. All study characteristics were reported in Table 4. In 13 (36.1%) cases misdeployment of the distal flange occurred, in 2 (5.5%) cases the proximal flange was deployed and then migrated entirely into the PFC. In most cases included in our study (20/36; 55.5%), the issue of misdeployment was not clearly described. A case report described the misdeployment of the stent in a non-target organ. In 4 cases data regarding rescue strategy were not available and the procedure was abandoned in one case.
| Ref. | Study design | Study population | Clinical indication | Technical success (%) | LAMS misdeployment | LAMS type | Size of LAMS (mm) | Use of guidewire | LAMS flange misdeployed | Rescue therapy |
| Venkatachalapathy et al[77], 2018 | Retrospective multicenter | 116 | WON, PFC | 99 | 1 | Hot Axios | - | No | Distal | LAMS removal followed by over-the-wire deployment of a new LAMS |
| Khan et al[78], 2021 | Retrospective multicenter | 208 | PFC | 97.1 | 7 | - | - | - | Distal | LAMS re-insertion (not counted as technical failure) (1/7); immediate repeat drainage (5/7); procedure abandoned (1/7) |
| Law et al[79], 2018 | Retrospective single center | 46 | WON | 93.5 | 5 | Cold Axios/hot Axios | - | - | - | LAMS removal followed by over-the-wire deployment of a new LAMS (4/5; 2 LAMS re-insertion, not counted as technical failure) and of a FCSEMS 10 × 60 mm (1/5) |
| Walter et al[10], 2015 | Prospective multicenter | 61 | PFC | 98 | 1 | Axios | - | Yes | Entirely inside the PFC | Placement of double pigtail stents |
| Siddiqui et al[80], 2016 | Retrospective multicenter | 82 | PFC | 97.5 | 2 | Cold Axios | - | Yes | Distal | LAMS removal followed by over-the-wire deployment of a SEMS; surgical cystogastrostomy (difficulty to re-advance the guidewire into the PFC to perform an endoscopic rescue therapy) |
| Mendoza et al[81], 2020 | Retrospective single center | 21 | WON | 95 | 1 | Hot Axios | - | Yes | Entirely inside the PFC | LAMS misdeployed was left inside the collection and a new one was then successfully placed through the original puncture site (both stents were removed 4 wk later) |
| Shah et al[82], 2015 | Prospective multicenter | 33 | PFC | 91 | 3 | Cold Axios | - | Yes | - | Placement of double pigtail stents |
| Despott et al[83], 2020 | Case report | 1 | WON | - | 1 | Hot Axios | 20x10 | - | Deployment in a non-target organ (colon) | LAMS removal and closure of both colonic and gastric defects with over-the-scope-clips |
| Rinninella et al[84], 2015 | Retrospective multicenter | 93 | PFC | 98.9 | 1 | Hot Axios | - | Yes | Distal | Placement of double pigtail stents |
| Song et al[85], 2019 | Prospective multicenter | 34 | PFC | 97.1 | 1 | Hot spaxus | - | Yes | Distal | LAMS in LAMS technique |
| Fugazza et al[86], 2020 | Retrospective multicenter | 328 | PFC, WON | 97.9 | 7 | Hot Axios | - | - | - | New LAMS placement (4/7); placement of plastic stents (3/7) |
| Zhang et al[12], 2022 | Retrospective multicenter | 35 | PFC | 97 | 1 | Hot Axios | 15 mm × 15 mm | Yes | - | SEMS in LAMS technique |
| Yang et al[87], 2019 | Retrospective multicenter | 80 | PFC | 97.5 | 3 | Cold Axios/hot Axios | - | - | - | - |
| Adler et al[70], 2018 | Retrospective multicenter | 80 | WON | 98.7 | 1 | Cold Axios | - | - | - | - |
| Curieses Luengo et al[88], 2019 | Case report | 1 | WON | - | 1 | Hot Axios | 10 mm × 10 mm | - | Distal | LAMS in LAMS technique |
The LAMS misdeployment in EUS-PFC drainage was managed as following: In 20/31 (64.5%) cases an over-the-wire deployment of a new stent was performed (10/20 with LAMS, 2/20 with SEMS, 8/20 with plastic stents), in 5/31 (16.1%) cases the EUS-PFC drainage was repeated, in 1/31 (3.2%) case surgical drainage was performed. The stent-in-stent strategy was the rescue treatment in 4/31 (12.9%) cases of LAMS misdeployment; in 3 (75%) cases a LAMS-in-LAMS technique was performed and in 1 (25%) case a SEMS was deployed inside the misdeployed LAMS (see Table 2).
Technical success of EUS-drainage is defined as the correct deployment of the stent between the gastrointestinal wall and target organ with evidence of bile flow in patients who underwent EUS-BD[24,25,32] or content flow/established access to the cavity in EUS-PFC or EUS-GBD cases[52,57].
Actually, stent misdeployment emerges as the primary cause of technical failure in the procedure of EUS-guided drainage. Among the studies we collected, different terms were used to define this complication, including misdeployment, dislodgement, and flange migration. We adopted the term ‘misdeployment’, as reported in the European Society of Gastrointestinal Endoscopy guidelines for therapeutic EUS[14].
According to the American Society for Gastrointestinal Endoscopy lexicon for endoscopic adverse events, LAMS misdeployment can be considered a procedure-related adverse event when it hampers the completion of the planned procedure and/or results in significant clinical consequences (i.e., prolongation of existing hospital stay and elicitation of the need for another procedure)[89]. Misdeployment can be defined as an incident if it does not interfere with the completion of the planned procedure or change the plan of care. Therefore, stent misdeployment can be managed successfully by endoscopic rescue maneuvers to allow the completion of the procedure; however, complications with different levels of severity can occur in some cases. In EUS-BD, stent misdeployment may be associated with spillage of bile and secretions into the peritoneal cavity or retroperitoneal space, resulting in peritonitis and pneumoretroperitoneum[90]. Recently Fabbri et al[91] proposed a classification of misdeployment types during EUS-guided gastroenterostomy as follows: Proximal flange misdeployment, distal flange misdeployment, stent misdeployment perforating other organs, and stent misdeployment into the peritoneum. This model considers which flange is misdeployed and the anatomical localization of the stent after misdeployment and can be supposedly adopted for all EUS-guided procedures involving the use of LAMS.
The rate of ERCP failure is 2%-10% and it is due to surgically altered anatomy, gastric outlet obstruction, duodenal and/or bile duct tumor infiltration, indwelling enteral stent, periampullary diverticula, impacted stones, and technical difficulties[92]. European guidelines suggest EUS-BD as the second-line treatment for patients with MBO. The optimal drainage strategy depends on the underlying disease (benign/malignant) and location of the obstruction (distal/hilar)[15].
EUS-BD proved to be equally effective with fewer adverse events and re-intervention compared to PTBD especially in gastric outlet obstructions[93]. In addition, EUS-BD is less invasive, leads to better nutrition, prevents electrolyte imbalances, and provides better quality of life[94]. As experience in EUS-BD continues to grow, comparative studies of EUS-CDS and ERCP have reported encouraging data in support of EUS-CDS as the primary treatment for distal MBO, challenging the role of ERCP[95].
In a meta-analysis, the technical and clinical success rates of EUS-CDS using LAMS were 93.6% and 94.8%, respectively, with pooled rate of overall adverse events of 17.1% and procedure-related adverse events of 6.2%[96]. In our research, LAMS misdeployment rate was 5.8%, and LAMS misdeployment represented the main cause of technical failure in EUS-CDS. Notably, technical failure was due to other causes in only seven cases (0.6%). In up to 86.8% of cases, the endoscopist managed LAMS misde
The most common endoscopic rescue technique involved misdeployed LAMS removal and over-the-wire deployment of a new stent through the same fistula tract (44.1%). SEMS were employed in most cases (76.7%). Other rescue strategies used include stent-in-stent (23.5%), EUS-guided/endoscopic rendezvous with transpapillary placement of a biliary SEMS (11.8%), and repeated EUS-drainage procedure (5.9%).
As reported in literature, the most common causes of LAMS misdeployment are related to difficult scope position[17,28,39] and small CBD diameter (< 15 mm)[21,27,34]. In a retrospective analysis by Jacques et al[23] involving 52 patients who underwent LAMS placement using various techniques, the technical and clinical success rates were 88.5% and 100%, respectively. In univariate analysis, CBD diameter > 15 mm, use of a 6-mm LAMS, and use of a one-step technique (direct puncture using the electrocautery system without needle puncture) were predictors of technical success in EUS-CDS. In another study, the authors performed EUS-CDS using a one-step technique in 97.1% (n = 68/70) of patients and achieved 98.6% of technical success[24]. The more frequent use of a pre-loaded guidewire in the group of patients with CBD < 15 mm compared to those with CBD ≥ 15 mm (33% vs 3.6%, P = 0.036) might have contributed to the comparable technical success, clinical success, and adverse event rates between the two groups. On the other hand, Di Mitri et al[21] reported seven cases of LAMS misdeployment in 31 patients with distal MBO who underwent EUS-CDS. CBD was ≤ 15 mm in six of the seven patients. In five cases, rescue therapies involved placing a fully covered self-expanding metal stent (FCSEMS) over the previously inserted guidewire, restoring the connection through the iatrogenic fistulous tract. In the remaining two cases, bile duct decompression after the puncture prevented the correct visualization of the CBD on EUS imaging and the possibility of approaching the CBD again; these cases were managed successfully by percutaneous- and laparoscopic-endoscopic rendezvous techniques. The authors assumed that the small caliber of the CBD forced the tip of the LAMS delivery catheter to be too close to the facing wall of the CBD and in an oblique direction, increasing the risk of misdeployment, even with the use of a small-size LAMS. In the largest study (256 patients enrolled) included in our review, Fugazza et al[26] reported that significantly higher technical success was achieved in patients with a larger CBD diameter compared to those with a smaller CBD diameter. The authors demonstrated that larger CBD size, use of a needle with a guidewire, fluoroscopy guidance, and LAMS placement in the proximal CBD were more likely in the non-expert group than in the expert group; however, technical [101 (94.4%) vs 138 (92.6%); P = 0.574] and clinical success [96 (95.0%) vs 134 (97.1%); P = 0.415] did not statistically differ between these two groups.
The use of a delivery system pre-loaded with a guidewire in complex cases (i.e., endoscope instability in the duodenal bulb or smaller CBD diameter) was emphasized by Anderloni et al[97] because it allowed rescue using an over-the-wire stent placement in cases of LAMS misdeployment, and the single-step technique was preferred in cases of dilated CBD > 15 mm.
Wire access into the CBD could be regained in some cases, allowing endoscopic rescue maneuvers to be performed, even in cases of non-identifiable CBD on EUS imaging[28,35]. Our data show that over-the-wire deployment of a tubular stent, particularly a biliary SEMS, was the preferred rescue procedure for LAMS misdeployment during EUS-CDS (44.1%). We suppose that this technique was preferred since EUS-BD with SEMS has long been a consolidated technique for BD and that SEMS placement can be performed without EUS guidance, which may be lost in these circumstances.
Laparoscopic cholecystectomy is the standard approach for acute calculus cholecystitis. In cases of severe inflammation, adhesive disease, bleeding in the surgical area, or suspected bile duct injury, open cholecystectomy may be required to achieve safe dissection and gallbladder resection. In recent years, EUS-GBD has emerged as the preferred alternative to surgical treatment over percutaneous GBD (PGBD) or endoscopic transpapillary GBD (ETP-GBD) and is included in the international guidelines for grade II cholecystitis and recommended for grade 3 cholecystitis in patients with American Society of Anesthesiologists scores ≥ 3 or Charlson Comorbidity Index ≥ 6[98,99]. It has a technical and clinical success rate of 94.65% [95% confidence interval (CI): 91.54-96.67; I2 = 0.00] and 92.06% (95%CI: 88.65-94.51; I2 = 0.00), respectively. The rates of adverse events associated with EUS-GBD, including perforations, misdeployment, bile leakage, stent migration into the gallbladder or peritoneum, bleeding, gastroduodenal perforation, pneumoperitoneum, and recurrent acute cholecystitis due to stent occlusion, varies between 8% and 17%[100-102]. EUS-GBD showed higher technical and clinical success rates and lower recurrence rates than those of ETP-GBD[103].
Moreover, several studies have compared EUS-GBD with PGBD, demonstrating similar technical and clinical success rates for both procedures[43,104-106]; however, EUS-GBD was associated with signi
Although studies comparing gastric and duodenal LAMS access for EUS-GBD did not find any significant differences in technical or clinical success or adverse event rates[107], the duodenum is a less mobile organ and is closer to the gallbladder than the stomach. Therefore, there is a lower risk of LAMS migration when gallbladder access is via the duodenum.
In 68% of cases, LAMS misdeployment involved the distal flange. This suggests that a careful choice of the position and proper advancement of the LAMS inside the GB are critical to avoiding misdeployment. The use of guidewire, reported in 68% of cases of misdeployment, helped to maintain secure access to the newly created fistula between the gastrointestinal system and GB. The most frequently performed rescue maneuver was the placement of LAMS or a longer SEMS through the lumen of the misdeployed stent (stent-in-stent strategy). The stent-in-LAMS was particularly the rescue strategy of choice in up to 60% of LAMS misdeployment cases.
Surgery or PTBD after endoscopic closure of the luminal perforation was required after the failure of endoscopic therapies[55,56,61]. LAMS removal and clip closure of digestive tract wall defect was the treatment of choice in 3 patients (one of them was treated by ETP-GBD while no further endoscopic maneuver was performed in the remaining two patients). This strategy allows a second drainage attempt during the index procedure or later in selected patients. According to our data, two patients died after LAMS misdeployment, one for surgical complications and one left to supportive care[22,56].
EUS-guided transmural drainage is considered the first-line treatment option for PFC, including walled-off necrosis (WON) and pancreatic pseudocysts[108]. Transluminal drainage in the “before-LAMS age” was achieved by the placement of double-pigtail plastic stents and afterward, by biliary/esophageal FC SEMS, which were associated with risks of migration, leakage, ulceration, and bleeding[109]. The LAMS design has the advantage of supporting drainage, preventing migration, and allowing direct access inside the WON cavity for endoscopic necrosectomy because it has a larger diameter, shorter length, and stent-anchoring flanges[110].
In our study, LAMS misdeployment during EUS-guided PFC drainage occurred in 34/1684 (2.0%) patients. This result is in accordance with the high technical success rate of these procedures reported in the literature (97.6%)[111]. Distal flange misdeployment in the peritoneal cavity, external to the cystic wall, was reported in up to 36.1% of cases[77,78,80,81,85]. Over-the-wire placement of a new stent (LAMS, SEMS, or double pigtail stents/plastic) through the novel fistula tract was the rescue therapy of choice in 64.5% of misdeployments. In 50% of cases, LAMS were deployed over the guidewire to complete the procedure as initially planned. The re-insertion of the same LAMS was performed in 15% of cases[78,79], resulting in a lower cost; these cases were counted as technical successes. In a study by Khan et al[78] involving 208 patients who underwent EUS-PFC drainage, 5/7 cases of LAMS misdeployment were managed by repeated EUS-guided drainage during index endoscopy.
There were two cases (5.5%) of complete LAMS misdeployment inside the PFC. In such cases, Mendoza Ladd et al[81] decided to leave the LAMS inside the PFC, and they deployed a new one through the fistula. After LAMS dilation, direct endoscopic necrosectomy was performed. Both stents were successfully removed four weeks later. The deployment of LAMS into an adjacent organ (the splenic flexure of the colon), described as WON, was reported by Despott et al[83], who identified the misdeployment only at the post-procedure scan (computerized tomography). After bowel preparation through a naso-jejunal tube to bypass the gastrocolic fistula, simultaneous upper and lower gastrointestinal endoscopies were performed, and the LAMS was removed. Both the colonic and gastric perforations were closed using over-the-scope clips. Although data regarding predictive factors related to LAMS misdeployment were lacking in the studies included in our review, Curieses Luengo et al[88] identified excessive flexion of the echoendoscope tip due to severe inflammatory duodenal stenosis as an unfavorable condition for correct LAMS deployment.
The use of LAMS has been demonstrated to have high technical and clinical success rates in EUS-CDS, EUS-GBD and EUS-PFC drainage, however significant rates of LAMS misdeployment are reported in 5.8%, 3.4%, and 2.0% of procedures, respectively. In a relevant rate of LAMS misdeployment, endoscopic rescue management has been shown to be technically feasible and effective in completing the procedure and avoiding major clinical consequences.
Although no algorithm is available to guide the appropriate rescue strategy for each case, three endoscopic techniques have been identified: (1) Gaining wire access to the target through the newly created tract and completing the procedure; (2) “Stent-in-stent” over the wire; and (3) Repeated procedures (ex novo or rendezvous). When endoscopic rescue procedures are not feasible, non-endoscopic options include percutaneous drainage or surgery.
In our analysis, the preferred strategy for LAMS misdeployment in EUS-CDS was LAMS removal and over-the-wire deployment of a new stent (44.1%), frequently SEMS (76.7% of cases), followed by stent-in-stent strategy (23.5%) and endoscopic rendezvous (11.8%). In EUS-GBD, the preferred technique was the stent-in-stent strategy (60%) using a SEMS in 93.3% of cases.
In EUS-PFC, the procedure of choice was LAMS removal followed by over-the-wire deployment of a new stent (64.5%), which was a LAMS or a plastic stent, in 50% and 40% of cases respectively. In conclusion, LAMS misdeployment is a relatively common adverse event, especially in EUS-BD. Endoscopic rescue strategies are feasible, and they vary depending on type of procedure, endoscopic technique used, and experience of the operators.
Scant data are available about rescue techniques in cases of lumen-apposing metal stents (LAMS) misdeployment which is the main cause of technical failure in endoscopic ultrasound (EUS)-guided drainage procedures. We performed a systematic review of the literature about LAMS misdeployment and rescue techniques in the biliopancreatic setting, focusing on technical aspects and success rate of endoscopic maneuvers.
LAMS misdeployment is a relatively common adverse event in EUS-guided drainages. There is no consensus on the best rescue approach in these cases and the choice is often made by the endoscopist relying upon the clinical scenario, anatomical characteristics, and local expertise.
The overall technical success rate of EUS-guided choledochoduodenostomy (EUS-CDS), gallbladder drainage (EUS-GBD) and pancreatic fluid collections drainage (EUS-PFC) was 93.7%, 96.1%, and 98.1% respectively. Significant rates of LAMS misdeployment have been reported for EUS-CDS, EUS-GBD and EUS-PFC drainage, respectively 5.8%, 3.4%, and 2.0%. Endoscopic rescue treatment was feasible in 86.8%, 80%, and 96.8% of cases. Non endoscopic rescue strategies were required only in 10.3%, 16% and 3.2% for EUS-CDS, EUS-GBD, and EUS-PFC.
We conducted a systematic review of the literature on PubMed searching for studies published up to October 2022 about on-label EUS-guided procedures namely EUS-CDS, EUS-GBD and EUS-PFC. The search was carried out using the exploded medical subject heading terms ‘lumen apposing metal stent’, ‘LAMS’, ‘endoscopic ultrasound’ and “choledochoduodenostomy” or “gallbladder” or “pancreatic fluid collections”.
The overall technical success rate of EUS-CDS, EUS-GBD and EUS-PFC was 93.7%, 96.1%, and 98.1% respectively. Significant rates of LAMS misdeployment have been reported for EUS-CDS, EUS-GBD and EUS-PFC drainage, 5.8%, 3.4%, and 2.0%, respectively. Endoscopic rescue treatment was feasible in 86.8%, 80%, and 96.8% of cases. Non endoscopic rescue strategies were required only in 10.3%, 16% and 3.2% for EUS-CDS, EUS-GBD, and EUS-PFC. The endoscopic rescue techniques described were over-the-wire deployment of a new stent through the created fistula tract in 44.1%, 8% and 64.5% and stent-in-stent in 23.5%, 60%, and 12.9%, respectively for EUS-CDS, EUS-GBD, and EUS-PFC. Further therapeutic option were endoscopic rendezvous in 11.8% of EUS-CDS and repeated procedure of EUS-guided drainage in 16.1% of EUS-PFC.
Stent misdeployment can be managed successfully by endoscopic rescue maneuvers to allow the completion of the procedure. In accordance with our results endoscopic rescue techniques are feasible in most cases (up to 96.8%). Three endoscopic rescue strategies have been identified: Gaining wire access to the target through the created fistula and completing the procedure; placement of a new stent through the misdeployed LAMS to the target (“stent-in-stent”) and repeated drainage procedures (ex novo or rendezvous).
LAMS misdeployment is the main cause of technical failure of EUS-drainages and it is potentially harmful to the patient. Knowledge of risk factors, classification of misdeployment and of endoscopic rescue techniques is useful to improve patient outcome and the safety of the procedure. Further prospective studies describing these issues are expected.
| 1. | Yasuda I, Takahashi K. Endoscopic management of walled-off pancreatic necrosis. Dig Endosc. 2021;33:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Dhindsa BS, Mashiana HS, Dhaliwal A, Mohan BP, Jayaraj M, Sayles H, Singh S, Ohning G, Bhat I, Adler DG. EUS-guided biliary drainage: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:101-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 3. | Vanella G, Bronswijk M, Arcidiacono PG, Larghi A, Wanrooij RLJV, de Boer YS, Rimbas M, Khashab M, van der Merwe SW. Current landscape of therapeutic EUS: Changing paradigms in gastroenterology practice. Endosc Ultrasound. 2023;12:16-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Armellini E, Crinò SF, Ballarè M, Occhipinti P. Endoscopic ultrasound-guided radiofrequency ablation of a pancreatic neuroendocrine tumor. Endoscopy. 2015;47 Suppl 1 UCTN:E600-E601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Melita G, Pallio S, Tortora A, Crinò SF, Macrì A, Dionigi G. Diagnostic and Interventional Role of Endoscopic Ultrasonography for the Management of Pancreatic Neuroendocrine Neoplasms. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 489] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 7. | Binmoeller KF, Shah J. A novel lumen-apposing stent for transluminal drainage of nonadherent extraintestinal fluid collections. Endoscopy. 2011;43:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc. 2012;75:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 320] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 9. | Itoi T, Binmoeller KF. EUS-guided choledochoduodenostomy by using a biflanged lumen-apposing metal stent. Gastrointest Endosc. 2014;79:715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Walter D, Will U, Sanchez-Yague A, Brenke D, Hampe J, Wollny H, López-Jamar JM, Jechart G, Vilmann P, Gornals JB, Ullrich S, Fähndrich M, de Tejada AH, Junquera F, Gonzalez-Huix F, Siersema PD, Vleggaar FP. A novel lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a prospective cohort study. Endoscopy. 2015;47:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 11. | Stier MW, Waxman I. Lumen-Apposing Metal Stents: Which One and Why? Gastrointest Endosc Clin N Am. 2018;28:207-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Zhang LY, Kunda R, Aerts M, Messaoudi N, Pawa R, Pawa S, Robles-Medranda C, Oleas R, Al-Haddad MA, Obaitan I, Muniraj T, Fabbri C, Binda C, Anderloni A, Tarantino I, Bejjani M, Ghandour B, Singh V, Khashab MA. Novel 15-mm-long lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections located ≥10 mm from the luminal wall. Endoscopy. 2022;54:706-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Rimbaş M, Anderloni A, Napoléon B, Seicean A, Forti E, Crinò SF, Tarantino I, Arcidiacono PG, Fabbri C, Rizzatti G, Amato A, Voiosu T, Fugazza A, Moșteanu O, Ginès À, de Nucci G, Fusaroli P, Nguyen NQ, Di Mitri R, Minelli Grazioli L, Mutignani M, Archibugi L, Binda C, Cominardi A, Barbera C, Fernández-Esparrach G, Palazzo L, Palazzo M, Poley JW, Spada C, Valerii G, Itoi T, Matsunami Y, Mateescu RB, Băicuș C, Costamagna G, Larghi A. Common bile duct size in malignant distal obstruction and lumen-apposing metal stents: a multicenter prospective study. Endosc Int Open. 2021;9:E1801-E1810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 336] [Article Influence: 84.0] [Reference Citation Analysis (3)] |
| 15. | Kunda R, Pérez-Miranda M, Will U, Ullrich S, Brenke D, Dollhopf M, Meier M, Larghi A. EUS-guided choledochoduodenostomy for malignant distal biliary obstruction using a lumen-apposing fully covered metal stent after failed ERCP. Surg Endosc. 2016;30:5002-5008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 146] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 16. | Tsuchiya T, Teoh AYB, Itoi T, Yamao K, Hara K, Nakai Y, Isayama H, Kitano M. Long-term outcomes of EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction: a prospective multicenter study. Gastrointest Endosc. 2018;87:1138-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 17. | Anderloni A, Buda A, Carrara S, Di Leo M, Fugazza A, Maselli R, Repici A. Single-session double-stent placement in concomitant malignant biliary and duodenal obstruction with a cautery-tipped lumen apposing metal stent. Endoscopy. 2016;48:E321-E322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Yoo HW, Moon JH, Jo SJ, Lee YN, Park JK, Lee TH, Cha SW, Cho YD, Park SH, Park SI, Jeong S, Lee DH. A novel electrocautery-enhanced delivery system for one-step endoscopic ultrasound-guided drainage of the gallbladder and bile duct using a lumen-apposing metal stent: a feasibility study. Endoscopy. 2021;53:922-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Sawas T, Bailey NJ, Yeung KYKA, James TW, Reddy S, Fleming CJ, Marya NB, Storm AC, Abu Dayyeh BK, Petersen BT, Martin JA, Levy MJ, Baron TH, Bun Teoh AY, Chandrasekhara V. Comparison of EUS-guided choledochoduodenostomy and percutaneous drainage for distal biliary obstruction: A multicenter cohort study. Endosc Ultrasound. 2022;11:223-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Anderloni A, Fugazza A, Troncone E, Auriemma F, Carrara S, Semeraro R, Maselli R, Di Leo M, D'Amico F, Sethi A, Repici A. Single-stage EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction. Gastrointest Endosc. 2019;89:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 111] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 21. | Di Mitri R, Amata M, Mocciaro F, Conte E, Bonaccorso A, Scrivo B, Scimeca D. EUS-guided biliary drainage with LAMS for distal malignant biliary obstruction when ERCP fails: single-center retrospective study and maldeployment management. Surg Endosc. 2022;36:4553-4569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 22. | Rajadurai A, Zorron Cheng Tao Pu L, Cameron R, Tagkalidis P, Holt B, Bassan M, Gupta S, Croagh D, Swan M, Saxena P, Efthymiou M, Vaughan R, Chandran S; ANZEC. Endoscopic ultrasound-guided gallbladder and bile duct drainage with lumen apposing metal stent: A large multicenter cohort (with videos). J Gastroenterol Hepatol. 2022;37:179-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 23. | Jacques J, Privat J, Pinard F, Fumex F, Valats JC, Chaoui A, Cholet F, Godard B, Grandval P, Legros R, Kerever S, Napoleon B. Endoscopic ultrasound-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing stents: a retrospective analysis. Endoscopy. 2019;51:540-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 24. | Jacques J, Privat J, Pinard F, Fumex F, Chaput U, Valats JC, Cholet F, Jezequel J, Grandval P, Legros R, Lepetit H, Albouys J, Napoleon B. EUS-guided choledochoduodenostomy by use of electrocautery-enhanced lumen-apposing metal stents: a French multicenter study after implementation of the technique (with video). Gastrointest Endosc. 2020;92:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 25. | El Chafic AH, Shah JN, Hamerski C, Binmoeller KF, Irani S, James TW, Baron TH, Nieto J, Romero RV, Evans JA, Kahaleh M. EUS-Guided Choledochoduodenostomy for Distal Malignant Biliary Obstruction Using Electrocautery-Enhanced Lumen-Apposing Metal Stents: First US, Multicenter Experience. Dig Dis Sci. 2019;64:3321-3327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 26. | Fugazza A, Fabbri C, Di Mitri R, Petrone MC, Colombo M, Cugia L, Amato A, Forti E, Binda C, Maida M, Sinagra E, Repici A, Tarantino I, Anderloni A; i-EUS Group. EUS-guided choledochoduodenostomy for malignant distal biliary obstruction after failed ERCP: a retrospective nationwide analysis. Gastrointest Endosc. 2022;95:896-904.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 27. | Hindryckx P, Degroote H. Lumen-apposing metal stents for approved and off-label indications: a single-centre experience. Surg Endosc. 2021;35:6013-6020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Armellini E, Metelli F, Piazzini Albani A, Vescovi L, Spinelli L, Pace F. Fast endoscopic rendezvous to the rescue after maldeployment of lumen-apposing metal stent during endoscopic ultrasound-guided choledochoduodenostomy. Endoscopy. 2023;55:E37-E38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 29. | Teoh AYB, Kongkam P, Bapaye A, Ratanachu T, Reknimitr R, Lakthakia S, Chan SM, Gadhikar HP, Korrapati SK, Lee YN, Medarapalem J, Ridtitid W, Moon JH. Use of a novel lumen apposing metallic stent for drainage of the bile duct and gallbladder: Long term outcomes of a prospective international trial. Dig Endosc. 2021;33:1139-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (1)] |
| 30. | Fugazza A, Gabbiadini R, Colombo M, Carrara S, Maselli R, Repici A, Anderloni A. Self-expandable metal stent placement as a rescue procedure for lumen-apposing metal stent misdeployment in biliary drainage. Endoscopy. 2020;52:E430-E431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Brückner S, Arlt A, Hampe J. Endoscopic ultrasound-guided biliary drainage using a lumen-apposing self-expanding metal stent: a case series. Endoscopy. 2015;47:858-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Vanella G, Bronswijk M, Dell'Anna G, Voermans RP, Laleman W, Petrone MC, van Malenstein H, Fockens P, Arcidiacono PG, van der Merwe S, van Wanrooij RLJ. Classification, risk factors, and management of lumen apposing metal stent dysfunction during follow-up of endoscopic ultrasound-guided choledochoduodenostomy: Multicenter evaluation from the Leuven-Amsterdam-Milan Study Group. Dig Endosc. 2023;35:377-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 33. | de Benito Sanz M, Nájera-Muñoz R, de la Serna-Higuera C, Fuentes-Valenzuela E, Fanjul I, Chavarría C, García-Alonso FJ, Sanchez-Ocana R, Carbajo AY, Bazaga S, Perez-Miranda M. Lumen apposing metal stents versus tubular self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy in malignant biliary obstruction. Surg Endosc. 2021;35:6754-6762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 34. | Garcia-Sumalla A, Loras C, Guarner-Argente C, Velasquez-Rodriguez JG, Andujar X, Salord S, Busquets J, Tebe C, Laquente B, Gornals JB. Is a coaxial plastic stent within a lumen-apposing metal stent useful for the management of distal malignant biliary obstruction? Surg Endosc. 2021;35:4873-4881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 35. | Sanchez-Ocana R, de Benito Sanz M, Nájera-Muñoz R, Chavarria C, de la Serna-Higuera C, Perez-Miranda M. Rendezvous ERCP via endoscopic ultrasound-guided gallbladder drainage to salvage a dislodged lumen-apposing metal stent during choledochoduodenostomy. Endoscopy. 2022;54:E65-E67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 36. | Graves M, Krafft M, Nasr J. EUS-guided choledochoduodenostomy creation using a biliary fully covered self-expanding metal stent after maldeployment of lumen-apposing metal stent. VideoGIE. 2021;6:234-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Chin JY, Seleq S, Weilert F. Safety and outcomes of endoscopic ultrasound-guided drainage for malignant biliary obstruction using cautery-enabled lumen-apposing metal stent. Endosc Int Open. 2020;8:E1633-E1638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 38. | On W, Paranandi B, Smith AM, Venkatachalapathy SV, James MW, Aithal GP, Varbobitis I, Cheriyan D, McDonald C, Leeds JS, Nayar MK, Oppong KW, Geraghty J, Devlin J, Ahmed W, Scott R, Wong T, Huggett MT. EUS-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing metal stents in patients with malignant distal biliary obstruction: multicenter collaboration from the United Kingdom and Ireland. Gastrointest Endosc. 2022;95:432-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 39. | Ligresti D, Amata M, Granata A, Cipolletta F, Barresi L, Traina M, Tarantino I. Salvage procedure following lumen-apposing metal stent maldeployment during endoscopic ultrasound-guided biliary drainage. Endoscopy. 2018;50:E190-E191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Sharaiha RZ, Tyberg A, Desai AP. Novel applications for lumen apposing metal stents: how far can we go? Gastrointest Endosc. 2015;81:AB425-AB426. [DOI] [Full Text] |
| 41. | Moon JH, Choi HJ, Kim DC, Lee YN, Kim HK, Jeong SA, Lee TH, Cha SW, Cho YD, Park SH, Jeong S, Lee DH, Isayama H, Itoi T. A newly designed fully covered metal stent for lumen apposition in EUS-guided drainage and access: a feasibility study (with videos). Gastrointest Endosc. 2014;79:990-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 42. | Law R, Grimm IS, Stavas JM, Baron TH. Conversion of Percutaneous Cholecystostomy to Internal Transmural Gallbladder Drainage Using an Endoscopic Ultrasound-Guided, Lumen-Apposing Metal Stent. Clin Gastroenterol Hepatol. 2016;14:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 43. | Teoh AYB, Kitano M, Itoi T, Pérez-Miranda M, Ogura T, Chan SM, Serna-Higuera C, Omoto S, Torres-Yuste R, Tsuichiya T, Wong KT, Leung CH, Chiu PWY, Ng EKW, Lau JYW. Endosonography-guided gallbladder drainage versus percutaneous cholecystostomy in very high-risk surgical patients with acute cholecystitis: an international randomised multicentre controlled superiority trial (DRAC 1). Gut. 2020;69:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 215] [Article Influence: 35.8] [Reference Citation Analysis (2)] |
| 44. | Anderloni A, Leo MD, Carrara S, Fugazza A, Maselli R, Buda A, Amato A, Auriemma F, Repici A. Endoscopic ultrasound-guided transmural drainage by cautery-tipped lumen-apposing metal stent: exploring the possible indications. Ann Gastroenterol. 2018;31:735-741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Issa D, Irani S, Law R, Shah S, Bhalla S, Mahadev S, Hajifathalian K, Sampath K, Mukewar S, Carr-Locke DL, Khashab MA, Sharaiha RZ. Endoscopic ultrasound-guided gallbladder drainage as a rescue therapy for unresectable malignant biliary obstruction: a multicenter experience. Endoscopy. 2021;53:827-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 46. | Nishiguchi K, Ogura T, Okuda A, Ueno S, Nishioka N, Yamada M, Matsuno J, Ueshima K, Yamamoto Y, Higuchi K. Endoscopic gallbladder drainage for acute cholecystitis with high-risk surgical patients between transduodenal and transpapillary stenting. Endosc Ultrasound. 2021;10:448-454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 47. | Chang JI, Dong E, Kwok KK. Endoscopic ultrasound-guided transmural gallbladder drainage in malignant obstruction using a novel lumen-apposing stent: a case series (with video). Endosc Int Open. 2019;7:E655-E661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 48. | Saumoy M, Tyberg A, Brown E, Eachempati SR, Lieberman M, Afaneh C, Kunda R, Cosgrove N, Siddiqui A, Gaidhane M, Kahaleh M. Successful Cholecystectomy After Endoscopic Ultrasound Gallbladder Drainage Compared With Percutaneous Cholecystostomy, Can it Be Done? J Clin Gastroenterol. 2019;53:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 49. | Anderloni A, Attili F, Sferrazza A, Rimbaș M, Costamagna G, Repici A, Larghi A. EUS-guided gallbladder drainage using a lumen-apposing self-expandable metal stent in patients with coagulopathy or anticoagulation therapy: a case series. Endosc Int Open. 2017;5:E1100-E1103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 50. | Ngamruengphong S, Kumbhari V, Tieu AH, Haito-Chavez Y, El-Zein MH, Aguila G, Khashab MA. EUS-guided rescue of early dislodgement of a lumen-apposing stent. Gastrointest Endosc. 2015;82:1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 51. | Cho DH, Jo SJ, Lee JH, Song TJ, Park DH, Lee SK, Kim MH, Lee SS. Feasibility and safety of endoscopic ultrasound-guided gallbladder drainage using a newly designed lumen-apposing metal stent. Surg Endosc. 2019;33:2135-2141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 52. | Walter D, Teoh AY, Itoi T, Pérez-Miranda M, Larghi A, Sanchez-Yague A, Siersema PD, Vleggaar FP. EUS-guided gall bladder drainage with a lumen-apposing metal stent: a prospective long-term evaluation. Gut. 2016;65:6-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 159] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 53. | Irani S, Baron TH, Grimm IS, Khashab MA. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video). Gastrointest Endosc. 2015;82:1110-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 54. | de la Serna-Higuera C, Pérez-Miranda M, Gil-Simón P, Ruiz-Zorrilla R, Diez-Redondo P, Alcaide N, Sancho-del Val L, Nuñez-Rodriguez H. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 55. | Dollhopf M, Larghi A, Will U, Rimbaş M, Anderloni A, Sanchez-Yague A, Teoh AYB, Kunda R. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 126] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 56. | Teoh AYB, Serna C, Penas I, Chong CCN, Perez-Miranda M, Ng EKW, Lau JYW. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy. 2017;49:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 57. | Mangiavillano B, Moon JH, Crinò SF, Larghi A, Pham KD, Teoh AYB, Paduano D, Lee YN, Yoo HW, Shin IS, Rizzatti G, Robles-Medranda C, Oleas R, Conti Bellocchi MC, Auriemma F, Lamonaca L, Spatola F, Conigliaro R, Facciorusso A, Gabbrielli A, Repici A. Safety and efficacy of a novel electrocautery-enhanced lumen-apposing metal stent in interventional EUS procedures (with video). Gastrointest Endosc. 2022;95:115-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 58. | Higa JT, Sahar N, Kozarek RA, La Selva D, Larsen MC, Gan SI, Ross AS, Irani SS. EUS-guided gallbladder drainage with a lumen-apposing metal stent versus endoscopic transpapillary gallbladder drainage for the treatment of acute cholecystitis (with videos). Gastrointest Endosc. 2019;90:483-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 59. | Garg R, Barawi M. A Guidewire May Save the Day. Korean J Gastroenterol. 2018;72:83-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 60. | Torres Yuste R, Garcia-Alonso FJ, Sanchez-Ocana R, Cimavilla Roman M, Peñas Herrero I, Carbajo AY, De Benito Sanz M, Mora Cuadrado N, De la Serna Higuera C, Perez-Miranda M. Safety and efficacy of endoscopic ultrasound-guided gallbladder drainage combined with endoscopic retrograde cholangiopancreatography in the same session. Dig Endosc. 2020;32:608-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 61. | James TW, Krafft M, Croglio M, Nasr J, Baron T. EUS-guided gallbladder drainage in patients with cirrhosis: results of a multicenter retrospective study. Endosc Int Open. 2019;7:E1099-E1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 62. | Irani S, Ngamruengphong S, Teoh A, Will U, Nieto J, Abu Dayyeh BK, Gan SI, Larsen M, Yip HC, Topazian MD, Levy MJ, Thompson CC, Storm AC, Hajiyeva G, Ismail A, Chen YI, Bukhari M, Chavez YH, Kumbhari V, Khashab MA. Similar Efficacies of Endoscopic Ultrasound Gallbladder Drainage With a Lumen-Apposing Metal Stent Versus Percutaneous Transhepatic Gallbladder Drainage for Acute Cholecystitis. Clin Gastroenterol Hepatol. 2017;15:738-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 156] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 63. | Cho SH, Oh D, Song TJ, Park DH, Seo DW, Lee SK, Kim MH, Lee YN, Moon JH, Lee SS. Comparison of the effectiveness and safety of lumen-apposing metal stents and anti-migrating tubular self-expandable metal stents for EUS-guided gallbladder drainage in high surgical risk patients with acute cholecystitis. Gastrointest Endosc. 2020;91:543-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 64. | Larghi A, Crinò SF, Vanella G, Rizzatti G, Bernardoni L, Arcidiacono PG. Preliminary experience of EUS-guided pancreatic fluid collections drainage using a new lumen-apposing metal stent mounted on a cautery device. Endosc Ultrasound. 2022;11:84-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 65. | Garg R, Chaar A, Szpunar S, Mohan BP, Barawi M. Efficacy and Safety of Lumen-Apposing Stents for Management of Pancreatic Fluid Collections in a Community Hospital Setting. Clin Endosc. 2020;53:480-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 66. | Anderloni A, Fabbri C, Nieto J, Uwe W, Dollhopf M, Aparicio JR, Perez-Miranda M, Tarantino I, Arlt A, Vleggaar F, Vanbiervliet G, Hampe J, Kahaleh M, Vila JJ, Dayyeh BKA, Storm AC, Fugazza A, Binda C, Charachon A, Sevilla-Ribota S, Tyberg A, Robert M, Wani S, Repici A, Sethi A, Khashab MA, Kunda R. The safety and efficacy of a new 20-mm lumen apposing metal stent (lams) for the endoscopic treatment of pancreatic and peripancreatic fluid collections: a large international, multicenter study. Surg Endosc. 2021;35:1741-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 67. | Olaiya B, Mekaroonkamol P, Li BW, Massaad J, Vachaparambil CT, Xu J, Lamm V, Luo H, Shen SS, Chen HM, Keilin S, Willingham FF, Cai Q. Outcomes of a single-step endoscopic ultrasound-guided drainage of pancreatic-fluid collections using an electrocautery-enhanced coaxial lumen-apposing, self-expanding metal stent with and without fluoroscopy. Gastroenterol Rep (Oxf). 2020;8:425-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 68. | Li J, Zhang Q, Zhou A, Zhao G, Li P. Comparative outcomes of endoscopic ultrasound-guided lumen-apposing mental stents drainage for pancreatic pseudocysts and walled-off necrosis: Case series and meta-analysis. Chronic Dis Transl Med. 2021;7:157-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 69. | Garcia Garcia de Paredes A, Gonzalez Martin JA, Foruny Olcina JR, Juzgado Lucas D, Gonzalez Panizo F, Lopez Duran S, Martinez Sanchez A, Sanjuanbenito A, Caminoa A, Albillos A, Vazquez-Sequeiros E. Lumen-apposing metal stents versus biliary fully-covered metal stents for EUS-guided drainage of pancreatic fluid collections: a case control study: Meeting presentations: European Society of Gastrointestinal Endoscopy ESGE Days 2018. Endosc Int Open. 2020;8:E6-E12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Adler DG. Single-operator experience with a 20-mm diameter lumen apposing metal stent to treat patients with large pancreatic fluid collections from pancreatic necrosis. Endosc Ultrasound. 2018;7:422-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 71. | Adler DG, Shah J, Nieto J, Binmoeller K, Bhat Y, Taylor LJ, Siddiqui AA. Placement of lumen-apposing metal stents to drain pseudocysts and walled-off pancreatic necrosis can be safely performed on an outpatient basis: A multicenter study. Endosc Ultrasound. 2019;8:36-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | Sharaiha RZ, Tyberg A, Khashab MA, Kumta NA, Karia K, Nieto J, Siddiqui UD, Waxman I, Joshi V, Benias PC, Darwin P, DiMaio CJ, Mulder CJ, Friedland S, Forcione DG, Sejpal DV, Gonda TA, Gress FG, Gaidhane M, Koons A, DeFilippis EM, Salgado S, Weaver KR, Poneros JM, Sethi A, Ho S, Kumbhari V, Singh VK, Tieu AH, Parra V, Likhitsup A, Womeldorph C, Casey B, Jonnalagadda SS, Desai AP, Carr-Locke DL, Kahaleh M, Siddiqui AA. Endoscopic Therapy With Lumen-apposing Metal Stents Is Safe and Effective for Patients With Pancreatic Walled-off Necrosis. Clin Gastroenterol Hepatol. 2016;14:1797-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 186] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 73. | Teoh AYB, Bapaye A, Lakhtakia S, Ratanachu T, Reknimitr R, Chan SM, Choi HJ, Gadhikar HP, Kongkam P, Korrapati SK, Lee YN, Medarapalem J, Ridtitid W, Moon JH. Prospective multicenter international study on the outcomes of a newly developed self-approximating lumen-apposing metallic stent for drainage of pancreatic fluid collections and endoscopic necrosectomy. Dig Endosc. 2020;32:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 74. | Yoo J, Yan L, Hasan R, Somalya S, Nieto J, Siddiqui AA. Feasibility, safety, and outcomes of a single-step endoscopic ultrasonography-guided drainage of pancreatic fluid collections without fluoroscopy using a novel electrocautery-enhanced lumen-apposing, self-expanding metal stent. Endosc Ultrasound. 2017;6:131-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 75. | Adler DG, Mallery S, Amateau S, Nieto J, Taylor LJ, Siddiqui A. A pilot study of a 20-mm lumen-apposing metal stent to treat pancreatic fluid collections: First reported multicenter use of a new device. Endosc Ultrasound. 2019;8:136-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 76. | Nieto J, Mekaroonkamol P, Shah R, Khashab MA, Loren DE, Waxman I, Edmundowicz SA, Willingham FF. Electrocautery-enhanced Lumen-apposing Metal Stents in the Management of Symptomatic Pancreatic Fluid Collections: Results From the Multicenter Prospective Pivotal Trial. J Clin Gastroenterol. 2023;57:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 77. | Venkatachalapathy SV, Bekkali N, Pereira S, Johnson G, Oppong K, Nayar M, Leeds J, Paranandi B, Penman I, Carroll N, Godfrey E, James M, Aithal G, McKay C, Devlin J, Wong T, Makin A, Ryan B, Huggett M. Multicenter experience from the UK and Ireland of use of lumen-apposing metal stent for transluminal drainage of pancreatic fluid collections. Endosc Int Open. 2018;6:E259-E265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 78. | Khan S, Chandran S, Chin J, Karim S, Mangira D, Nasr M, Ermerak G, Trinh A, Kia CYH, Mules T, Zad M, Ang TL, Johns E, Tee D, Kaul A, Ratanachu-Ek T, Jirathan-Opas J, Fisher L, Cameron R, Welch C, Lim G, Metz AJ, Moss A, Bassan M, Saxena P, Kaffes A, St John A, Hourigan LF, Tagkalidis P, Weilert F, Vaughan R, Devereaux B. Drainage of pancreatic fluid collections using a lumen-apposing metal stent with an electrocautery-enhanced delivery system. J Gastroenterol Hepatol. 2021;36:3395-3401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 79. | Law ST, De La SernaHiguera C, Simón PG, Pérez-MirandaCastillo M. Comparison of clinical efficacies and safeties of lumen-apposing metal stent and conventional-type metal stent-assisted EUS-guided pancreatic wall-off necrosis drainage: a real-life experience in a tertiary hospital. Surg Endosc. 2018;32:2448-2453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 80. | Siddiqui AA, Adler DG, Nieto J, Shah JN, Binmoeller KF, Kane S, Yan L, Laique SN, Kowalski T, Loren DE, Taylor LJ, Munigala S, Bhat YM. EUS-guided drainage of peripancreatic fluid collections and necrosis by using a novel lumen-apposing stent: a large retrospective, multicenter U.S. experience (with videos). Gastrointest Endosc. 2016;83:699-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 219] [Article Influence: 21.9] [Reference Citation Analysis (1)] |
| 81. | Mendoza Ladd A, Bashashati M, Contreras A, Umeanaeto O, Robles A. Endoscopic pancreatic necrosectomy in the United States-Mexico border: A cross sectional study. World J Gastrointest Endosc. 2020;12:149-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 82. | Shah RJ, Shah JN, Waxman I, Kowalski TE, Sanchez-Yague A, Nieto J, Brauer BC, Gaidhane M, Kahaleh M. Safety and efficacy of endoscopic ultrasound-guided drainage of pancreatic fluid collections with lumen-apposing covered self-expanding metal stents. Clin Gastroenterol Hepatol. 2015;13:747-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 182] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 83. | Despott EJ, Lazaridis N, Johnson G, Yano T, Murino A. Over-the-scope clip closure of an iatrogenic gastro-colic fistula following maldeployment of a lumen-apposing metal stent. Endoscopy. 2020;52:E300-E302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 84. | Rinninella E, Kunda R, Dollhopf M, Sanchez-Yague A, Will U, Tarantino I, Gornals Soler J, Ullrich S, Meining A, Esteban JM, Enz T, Vanbiervliet G, Vleggaar F, Attili F, Larghi A. EUS-guided drainage of pancreatic fluid collections using a novel lumen-apposing metal stent on an electrocautery-enhanced delivery system: a large retrospective study (with video). Gastrointest Endosc. 2015;82:1039-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 167] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 85. | Song TJ, Lee SS, Moon JH, Choi HJ, Cho CM, Lee KH, Park SW, Kim SH, Lee SO, Lee YN, Lee JK. Efficacy of a novel lumen-apposing metal stent for the treatment of symptomatic pancreatic pseudocysts (with video). Gastrointest Endosc. 2019;90:507-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 86. | Fugazza A, Sethi A, Trindade AJ, Troncone E, Devlin J, Khashab MA, Vleggaar FP, Bogte A, Tarantino I, Deprez PH, Fabbri C, Aparicio JR, Fockens P, Voermans RP, Uwe W, Vanbiervliet G, Charachon A, Packey CD, Benias PC, El-Sherif Y, Paiji C, Ligresti D, Binda C, Martínez B, Correale L, Adler DG, Repici A, Anderloni A. International multicenter comprehensive analysis of adverse events associated with lumen-apposing metal stent placement for pancreatic fluid collection drainage. Gastrointest Endosc. 2020;91:574-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 87. | Yang J, Chen YI, Friedland S, Holmes I, Paiji C, Law R, Hosmer A, Stevens T, Matheus F, Pawa R, Mathur N, Sejpal D, Inamdar S, Berzin TM, DiMaio CJ, Gupta S, Yachimski PS, Anderloni A, Repici A, James T, Jamil LH, Ona M, Lo SK, Gaddam S, Dollhopf M, Alammar N, Shieh E, Bukhari M, Kumbhari V, Singh V, Brewer O, Sanaei O, Fayad L, Ngamruengphong S, Shin EJ, Baron TH, Khashab MA. Lumen-apposing stents versus plastic stents in the management of pancreatic pseudocysts: a large, comparative, international, multicenter study. Endoscopy. 2019;51:1035-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 88. | Curieses Luengo M, Consiglieri CF, Puga M, Gornals JB. A novel rescue maneuver for a distal dislodged lumen-apposing metal stent (LAMS): "LAMS-in-LAMS" technique. Rev Esp Enferm Dig. 2019;111:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 89. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 2021] [Article Influence: 126.3] [Reference Citation Analysis (1)] |
| 90. | Han SY, Kim SO, So H, Shin E, Kim DU, Park DH. EUS-guided biliary drainage versus ERCP for first-line palliation of malignant distal biliary obstruction: A systematic review and meta-analysis. Sci Rep. 2019;9:16551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (1)] |
| 91. | Fabbri C, Binda C, Fugazzola P, Sbrancia M, Tomasoni M, Coluccio C, Jung CFM, Prosperi E, Agnoletti V, Ansaloni L. Hybrid gastroenterostomy using a lumen-apposing metal stent: a case report focusing on misdeployment and systematic review of the current literature. World J Emerg Surg. 2022;17:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 92. | Sarkaria S, Sundararajan S, Kahaleh M. Endoscopic ultrasonographic access and drainage of the common bile duct. Gastrointest Endosc Clin N Am. 2013;23:435-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 93. | Sharaiha RZ, Khan MA, Kamal F, Tyberg A, Tombazzi CR, Ali B, Tombazzi C, Kahaleh M. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (2)] |
| 94. | Holt BA, Hawes R, Hasan M, Canipe A, Tharian B, Navaneethan U, Varadarajulu S. Biliary drainage: role of EUS guidance. Gastrointest Endosc. 2016;83:160-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 95. | Hathorn KE, Bazarbashi AN, Sack JS, McCarty TR, Wang TJ, Chan WW, Thompson CC, Ryou M. EUS-guided biliary drainage is equivalent to ERCP for primary treatment of malignant distal biliary obstruction: a systematic review and meta-analysis. Endosc Int Open. 2019;7:E1432-E1441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 96. | Amato A, Sinagra E, Celsa C, Enea M, Buda A, Vieceli F, Scaramella L, Belletrutti P, Fugazza A, Cammà C, Radaelli F, Repici A, Anderloni A. Efficacy of lumen-apposing metal stents or self-expandable metal stents for endoscopic ultrasound-guided choledochoduodenostomy: a systematic review and meta-analysis. Endoscopy. 2021;53:1037-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 97. | Anderloni A, Troncone E, Fugazza A, Cappello A, Del Vecchio Blanco G, Monteleone G, Repici A. Lumen-apposing metal stents for malignant biliary obstruction: Is this the ultimate horizon of our experience? World J Gastroenterol. 2019;25:3857-3869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 98. | Mayumi T, Okamoto K, Takada T, Strasberg SM, Solomkin JS, Schlossberg D, Pitt HA, Yoshida M, Gomi H, Miura F, Garden OJ, Kiriyama S, Yokoe M, Endo I, Asbun HJ, Iwashita Y, Hibi T, Umezawa A, Suzuki K, Itoi T, Hata J, Han HS, Hwang TL, Dervenis C, Asai K, Mori Y, Huang WS, Belli G, Mukai S, Jagannath P, Cherqui D, Kozaka K, Baron TH, de Santibañes E, Higuchi R, Wada K, Gouma DJ, Deziel DJ, Liau KH, Wakabayashi G, Padbury R, Jonas E, Supe AN, Singh H, Gabata T, Chan ACW, Lau WY, Fan ST, Chen MF, Ker CG, Yoon YS, Choi IS, Kim MH, Yoon DS, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: management bundles for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2018;25:96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 181] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 99. | Pisano M, Allievi N, Gurusamy K, Borzellino G, Cimbanassi S, Boerna D, Coccolini F, Tufo A, Di Martino M, Leung J, Sartelli M, Ceresoli M, Maier RV, Poiasina E, De Angelis N, Magnone S, Fugazzola P, Paolillo C, Coimbra R, Di Saverio S, De Simone B, Weber DG, Sakakushev BE, Lucianetti A, Kirkpatrick AW, Fraga GP, Wani I, Biffl WL, Chiara O, Abu-Zidan F, Moore EE, Leppäniemi A, Kluger Y, Catena F, Ansaloni L. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 319] [Article Influence: 53.2] [Reference Citation Analysis (1)] |
| 100. | Chan JHY, Teoh AYB. Current Status of Endoscopic Gallbladder Drainage. Clin Endosc. 2018;51:150-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 101. | Jain D, Bhandari BS, Agrawal N, Singhal S. Endoscopic Ultrasound-Guided Gallbladder Drainage Using a Lumen-Apposing Metal Stent for Acute Cholecystitis: A Systematic Review. Clin Endosc. 2018;51:450-462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 102. | Mohan BP, Asokkumar R, Shakhatreh M, Garg R, Ponnada S, Navaneethan U, Adler DG. Adverse events with lumen-apposing metal stents in endoscopic gallbladder drainage: A systematic review and meta-analysis. Endosc Ultrasound. 2019;8:241-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 103. | McCarty TR, Hathorn KE, Bazarbashi AN, Jajoo K, Ryou M, Thompson CC. Endoscopic gallbladder drainage for symptomatic gallbladder disease: a cumulative systematic review meta-analysis. Surg Endosc. 2021;35:4964-4985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 104. | Luk SW, Irani S, Krishnamoorthi R, Wong Lau JY, Wai Ng EK, Teoh AY. Endoscopic ultrasound-guided gallbladder drainage versus percutaneous cholecystostomy for high risk surgical patients with acute cholecystitis: a systematic review and meta-analysis. Endoscopy. 2019;51:722-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 105. | Teoh AY, Perez-Miranda M, Kunda R, Lee SS, Irani S, Yeaton P, Sun S, Baron TH, Moon JH, Holt B, Khor CJL, Rerknimitr R, Bapaye A, Chan SM, Choi HJ, James TW, Kongkam P, Lee YN, Parekh P, Ridtitid W, Serna-Higuera C, Tan DMY, Torres-Yuste R. Outcomes of an international multicenter registry on EUS-guided gallbladder drainage in patients at high risk for cholecystectomy. Endosc Int Open. 2019;7:E964-E973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 106. | Rana SS. Endoscopic ultrasound-guided gallbladder drainage: a technical review. Ann Gastroenterol. 2021;34:142-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (1)] |
| 107. | Sobani ZA, Ling C, Rustagi T. Endoscopic Ultrasound-Guided Gallbladder Drainage. Dig Dis Sci. 2021;66:2154-2161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 108. | Arvanitakis M, Dumonceau JM, Albert J, Badaoui A, Bali MA, Barthet M, Besselink M, Deviere J, Oliveira Ferreira A, Gyökeres T, Hritz I, Hucl T, Milashka M, Papanikolaou IS, Poley JW, Seewald S, Vanbiervliet G, van Lienden K, van Santvoort H, Voermans R, Delhaye M, van Hooft J. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines. Endoscopy. 2018;50:524-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 335] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 109. | Kawakami H, Itoi T, Sakamoto N. Endoscopic ultrasound-guided transluminal drainage for peripancreatic fluid collections: where are we now? Gut Liver. 2014;8:341-355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 110. | Mussetto A, Fugazza A, Fuccio L, Triossi O, Repici A, Anderloni A. Current uses and outcomes of lumen-apposing metal stents. Ann Gastroenterol. 2018;31:535-540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 111. | Guzmán-Calderón E, Chacaltana A, Díaz R, Li B, Martinez-Moreno B, Aparicio JR. Head-to-head comparison between endoscopic ultrasound guided lumen apposing metal stent and plastic stents for the treatment of pancreatic fluid collections: A systematic review and meta-analysis. J Hepatobiliary Pancreat Sci. 2022;29:198-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mestrovic A, Croatia; Nakamura K, Japan S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY