Published online Mar 7, 2022. doi: 10.3748/wjg.v28.i9.948
Peer-review started: September 1, 2021
First decision: November 17, 2021
Revised: November 25, 2021
Accepted: January 29, 2022
Article in press: January 29, 2022
Published online: March 7, 2022
Processing time: 182 Days and 15.3 Hours
Postoperative morbidity after curative resection for hilar cholangiocarcinoma (HCCA) is common; however, whether it has an impact on oncological prognosis is unknown.
To evaluate the influence of postoperative morbidity on tumor recurrence and mortality after curative resection for HCCA.
Patients with recently diagnosed HCCA who had undergone curative resection between January 2010 and December 2017 at The First Affiliated Hospital of Army Medical University in China were enrolled. The independent risk factors for morbidity in the 30 d after surgery were investigated, and links between postoperative morbidity and patient characteristics and outcomes were assessed. Postoperative morbidities were divided into five grades based on the Clavien-Dindo classification, and major morbidities were defined as Clavien-Dindo ≥ 3. Univariate and multivariate Cox regression analyses were used to evaluate the risk factors for recurrence-free survival (RFS) and overall survival (OS).
Postoperative morbidity occurred in 146 out of 239 patients (61.1%). Multivariate logistic regression revealed that cirrhosis, intraoperative blood loss > 500 mL, diabetes mellitus, and obesity were independent risk factors. Postoperative morbidity was associated with decreased OS and RFS (OS: 18.0 mo vs 31.0 mo, respectively, P = 0.003; RFS: 16.0 mo vs 26.0 mo, respectively, P = 0.002). Multivariate Cox regression analysis indicated that postoperative morbidity was independently associated with decreased OS [hazard ratios (HR): 1.557, 95% confidence interval (CI): 1.119-2.167, P = 0.009] and RFS (HR: 1.535, 95%CI: 1.117-2.108, P = 0.008). Moreover, major morbidity was independently associated with decreased OS (HR: 2.175; 95%CI: 1.470-3.216, P < 0.001) and RFS (HR: 2.054; 95%CI: 1.400-3.014, P < 0.001) after curative resection for HCCA.
Postoperative morbidity (especially major morbidity) may be an independent risk factor for unfavorable prognosis in HCCA patients following curative resection.
Core Tip: In this study, postoperative morbidity was found to be an independent risk factor for poor overall survival and recurrence-free survival following curative resection for hilar cholangiocarcinoma. In addition, this study revealed the independent risk factors associated with increased postoperative morbidity, which could help to reduce the incidence of postoperative morbidity and improve oncological prognosis.
- Citation: Liu ZP, Chen WY, Zhang YQ, Jiang Y, Bai J, Pan Y, Zhong SY, Zhong YP, Chen ZY, Dai HS. Postoperative morbidity adversely impacts oncological prognosis after curative resection for hilar cholangiocarcinoma. World J Gastroenterol 2022; 28(9): 948-960
- URL: https://www.wjgnet.com/1007-9327/full/v28/i9/948.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i9.948
Cholangiocarcinoma is a common malignancy of the liver, second only to hepatocellular carcinoma (HCC) in incidence and accounting for approximately 10% of primary liver tumors[1,2]. Hilar cholangiocarcinoma (HCCA), also referred to as a Klatskin tumor, represents 60% of cholangiocarcinomas[3]. The HCCA incidence is increasing, and tumors have a poorer prognosis than any other hepatobiliary tumor, such as HCC, with five-year survival rates of 20% to 40%[4,5]. Radical surgery offers a possible cure for eligible HCCA patients. However, the oncological prognosis after liver resection for HCCA is often uncertain, as the tumor recurs within five years in over 60% of patients[6,7]. Consequently, identifying the risk factors that influence HCCA recurrence is important to improve outcomes.
Previous studies have demonstrated that postoperative morbidity is linked to greater recurrence and lower survival rates than many other gastrointestinal tumors, such as HCC[8], pancreatic[9], gastric[10,11], and colorectal carcinomas[12,13], as well as intrahepatic cholangiocarcinoma[14]. Systemic inflammation may result from postoperative morbidity, which could, in turn, reduce the effectiveness of the immune response against the tumor[15]. This may explain the relationship between poorer prognosis and postoperative morbidity. Regrettably, because HCCA surgery is one of the most complicated operations in hepatobiliary surgery, there is a high incidence of postoperative morbidity, ranging from 30% to 70%[16]. Postoperative morbidity is linked to both surgical factors and patients' underlying diseases[17-19]. From our point of view, surgery should be both safe and effective, avoiding postoperative morbidity to improve oncological prognosis. However, few studies have investigated the effects of postoperative morbidity on oncological prognosis in patients with HCCA after curative resection.
Therefore, this study aimed to determine if there is a link between the presence of postoperative morbidity and oncological prognosis following curative resection for HCCA. Additionally, the study assessed the independent risk factors for the occurrence of postoperative morbidity.
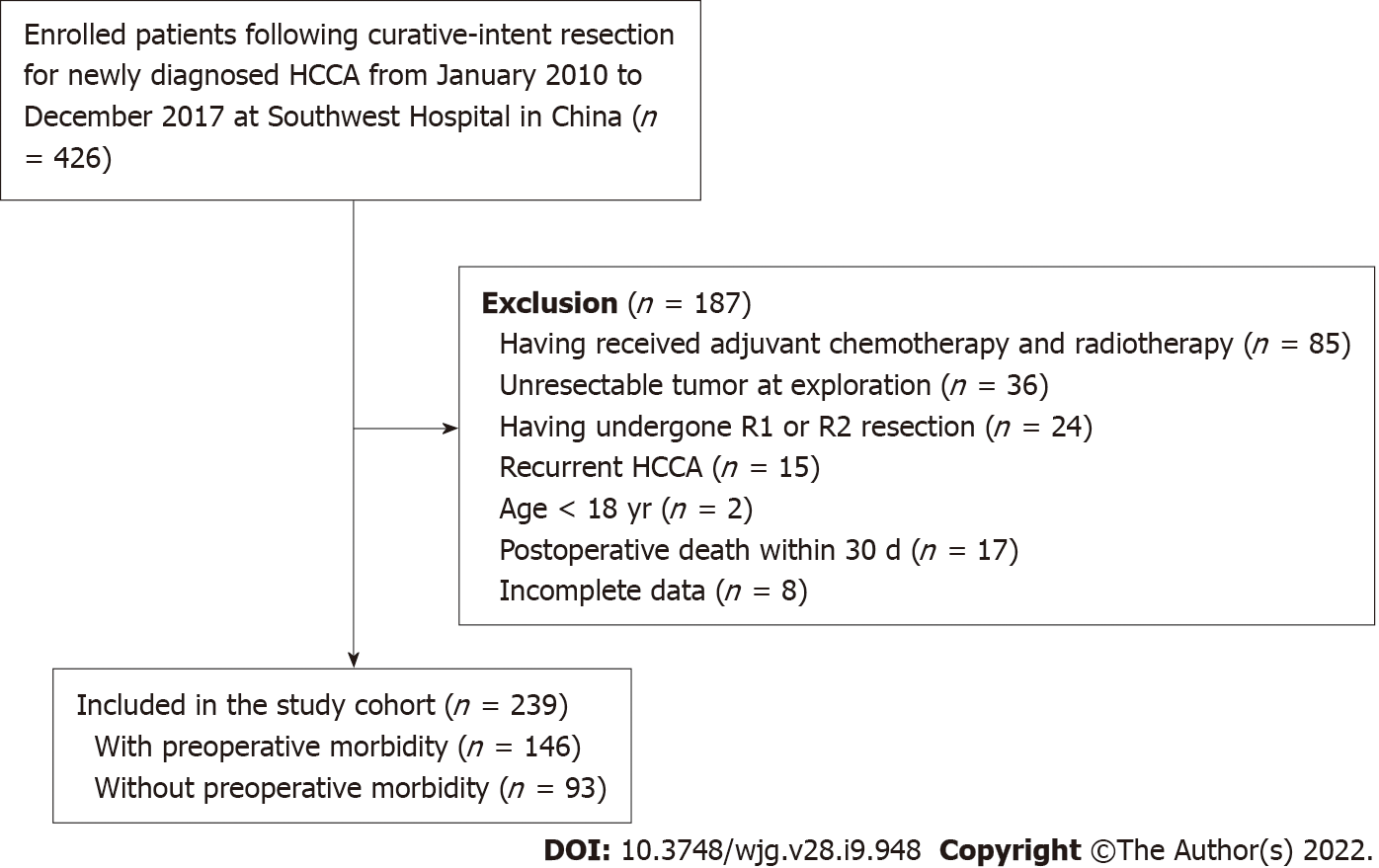
The data of patients with HCCA who had undergone curative resection for newly diagnosed HCCA between January 2010 and December 2017 at The First Affiliated Hospital of Army Medical University (Southwest Hospital) in China were collected and analyzed. The HCCA diagnosis was confirmed by postoperative pathological evaluation. Extrahepatic bile duct resection and partial hepatectomy were performed on all patients. Regardless of preoperative computed tomography (CT), magnetic resonance imaging (MRI) or suspicion of lymph node metastasis, all patients underwent locoregional lymphadenectomy. To achieve curative resection, combined pancreaticoduodenectomy and/or vascular resection was conducted, with curative resection classified as complete tumor (both macroscopic and microscopic) removal, with clear resection margins visible on microscopy (R0 resection). Patient exclusion criteria were: (1) Having received adjuvant chemotherapy and radiotherapy; (2) Unresectable tumor at exploration; (3) Having undergone R1 or R2 resection; (4) Recurrent HCCA; (5) Age < 18 years; (6) Postoperative death within 30 d; and (7) Incomplete data. The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Institutional Review Board of the South-West Hospital of Chongqing, China (No. KY2021129). Patients were not required to give informed consent for the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Variables related to patients and liver pathology included age, sex, American Society of Anesthesiologists (ASA) score, obesity (BMI > 30), diabetes mellitus, cirrhosis, and preoperative drainage. Cirrhosis was verified by postoperative histopathology. Tumor-related variables included preoperative carbohydrate antigen 19-9 (CA19-9) levels, maximum tumor size, macrovascular and microvascular invasion, peripheral nerve invasion, metastasis to lymph nodes, Bismuth type, and poorly differentiated tumors. A preoperative CA19-9 level of 150 U/L was used as a threshold to separate patients into two groups[20]. The operative variables were intraoperative blood loss, blood transfusion, and the extent of hepatectomy (minor or major). Resection of three or more Couinaud liver segments was called major hepatectomy, whereas resection of fewer segments was labeled minor hepatectomy.
Postoperative morbidity was classified according to the Clavien-Dindo classification[21], with minor morbidity defined as Clavien-Dindo grades I-II and major morbidity defined as grades III-V. The occurrence of postoperative morbidity within 30 d was recorded, as was the postoperative morbidity hospital stay. Morbidity included posthepatectomy liver failure (PHLF); blood, lung, abdominal, and biliary infection; pleural effusion; bile leakage; ascites; intestinal leakage cholangitis; abdominal hemorrhage; delayed gastric emptying; and wound dehiscence, among others. PHLF was recognized by the “50-50 criteria” five days or more after surgery[22]. A severe drop of > 3 g/dL in the postoperative hemoglobin level compared with the preoperative level was indicative of abdominal hemorrhage, with or without the need for transfusion and/or reoperation. Bile leakage was defined as a drain bilirubin concentration of more than three times higher than that of serum. Ascites or pleural effusions requiring diuretic administration or paracentesis were also recognized. Surgical site infection was diagnosed based on the Prevention of the National Nosocomial Infections Surveillance and Centers for Disease Control[23].
The patients were followed up at regular intervals (approximately 1-2 mo) after discharge. A standard protocol was used to evaluate the presence of HCCA recurrence. This included clinical symptoms, physical examinations, laboratory tests (liver function and tumor biomarkers), and abdominal ultrasonography. CT, MRI, or ultrasonic contrast was performed every two months after surgery or when tumor recurrence was suspected. The presence of new lesions seen on MRI or CT was defined as recurrence that was treated by surgery, drugs, or supportive therapy.
The primary endpoint was overall survival (OS), and the secondary endpoint was recurrence-free survival (RFS). OS was considered to be the interval from curative resection to death or last follow-up. For patients with recurrence, RFS was considered to be the interval from curative resection to the diagnosis of tumor recurrence. For patients without recurrence, RFS was taken as the interval from curative resection to death or last follow-up. Until the study's termination on July 15, 2020, all patients were followed up on until death or loss to follow-up.
Continuous variables are expressed as the means ± SD or medians (range), and categorical variables are expressed as the frequencies and percentages. Student’s t test or the Mann–Whitney U test was used for continuous variables, and Pearson’s chi-square test was used for categorical variables. The Kaplan–Meier method and log-rank test were used to calculate and compare the OS and RFS rates. Variables showing significance levels of P < 0.1 on univariate analyses were used for multivariate analysis by the Cox proportional hazard model. In univariate and multivariate Cox regression studies, hazard ratios (HRs) and their 95 percent confidence intervals (CIs) were calculated. SPSS® version 26.0 (IBM, Armonk, New York, United States) was used for statistical analysis. P values were two-sided, and statistical significance was defined as a P value of less than 0.05.
In our study, 239 patients were included based on established inclusion criteria (Figure 1). All patients performed open surgery. Table 1 presents the perioperative outcomes for the 239 patients. Of these patients, 146 (61.1%) experienced morbidity within 30 d of surgery, with minor morbidity occurring in 78 (32.6%) and major morbidity in 68 (28.5%) patients. The top three causes of morbidity were surgical site infection (36/239, 15.1%), bile leak (32/239, 13.4%), and pleural effusion (24/239, 10.0%).
| Postoperative outcomes (n = 239) | Patients (%) |
| Postoperative 30-d morbidity | 146 (61.1) |
| Minor morbidity (Clavien-Dindo grade I-II) | 78 (32.6) |
| Major morbidity (Clavien-Dindo grade III-IV) | 68 (28.5) |
| Types of postoperative 30-d morbidity | |
| PHLF | 15 (6.3) |
| Blood infection | 14 (5.9) |
| Lung infection | 12 (5.0) |
| Bile leakage | 32 (13.4) |
| Pleural effusion | 24 (10.0) |
| Ascites | 4 (1.7) |
| Intestines leak | 9 (3.8) |
| Abdominal hemorrhage | 10 (6.8) |
| Delayed gastric emptying | 17 (7.1) |
| Surgical site infection | 36 (15.1) |
| Others | 11 (4.6) |
| Postoperative hospital stay, days1 | 19 (15, 26) |
Table 2 shows the comparisons of patients’ clinicopathologic and operative variables between those with and without postoperative morbidity. Notably, obesity, diabetes mellitus, cirrhosis, and intraoperative blood loss > 500 mL were more common in patients with morbidity (P < 0.05).
| Variables | Total (n = 239) | Without postoperative morbidity (n = 93) | With postoperative morbidity (n = 146) | P value |
| Age > 60 yr | 54 (22.6) | 22 (23.7) | 32 (21.9) | 0.754 |
| Male sex | 144 (60.3) | 54 (58.1) | 90 (61.6) | 0.581 |
| ASA score > 2 | 23 (9.6) | 6 (6.5) | 17 (11.6) | 0.185 |
| Obesity | 28 (11.7) | 4 (4.3) | 24 (16.4) | 0.004 |
| Diabetes mellitus | 24 (10.0) | 4 (4.3) | 20 (13.7) | 0.018 |
| Cirrhosis | 39 (16.3) | 8 (8.6) | 31 (21.2) | 0.010 |
| Preoperative CA19-9 > 150 U/L | 129 (54.0) | 44 (47.3) | 85 (58.2) | 0.099 |
| Maximum tumor size > 3 cm | 68 (25.8) | 21 (22.6) | 47 (32.2) | 0.108 |
| Macrovascular invasion | 144 (60.3) | 55 (59.1) | 89 (61.0) | 0.779 |
| Microvascular invasion | 85 (35.6) | 28 (30.1) | 57 (39.0) | 0.160 |
| Peripheral nerve invasion | 80 (33.5) | 30 (32.3) | 50 (34.2) | 0.751 |
| Poor tumor differentiation | 77 (32.2) | 29 (31.2) | 48 (32.9) | 0.785 |
| Intraoperative blood transfusion | 159 (66.5) | 57 (61.3) | 102 (69.9) | 0.171 |
| Intraoperative blood loss > 500 mL | 185 (77.4) | 65 (69.9) | 120 (82.2) | 0.027 |
| Major hepatectomy | 171 (71.5) | 65 (69.9) | 106 (72.6) | 0.651 |
| Hepatic artery reconstruction | 12 (5.0) | 5 (5.4) | 7 (4.8) | 0.841 |
| Portal vein reconstruction | 45 (19.6) | 22 (23.7) | 23 (15.8) | 0.128 |
| Pringle maneuver | 175 (73.2) | 73 (78.5) | 102 (69.9) | 0.142 |
| Number of examined LNs > 4 | 125 (52.3) | 52 (55.9) | 73 (50.0) | 0.372 |
| LN metastasis | 54 (22.6) | 18 (19.4) | 36 (24.7) | 0.339 |
| Bismuth type, III-IV | 135 (56.5) | 52 (55.9) | 83 (56.8) | 0.887 |
| Preoperative drainage | 71 (29.7) | 28 (30.1) | 43 (29.5) | 0.914 |
In the multiple logistic regression model using significant (P < 0.1) factors shown in Table 2, cirrhosis [odds ratio (OR): 2.867; 95%CI: 1.207-6.810; P = 0.017], intraoperative blood loss > 500 mL (OR: 2.240; 95%CI: 1.162-4.318; P = 0.016), diabetes mellitus (OR: 3.395; 95%CI: 1.082-10.651; P = 0.036), and obesity (OR: 3.694; 95%CI: 1.197-11.394; P = 0.023) were identified as independent risk factors for postoperative morbidity (Table 3).
| Variables | Multivariable analyses1 | |
| P value | OR (95%CI) | |
| Obesity | 0.023 | 3.694 (1.197-11.394) |
| Diabetes mellitus | 0.036 | 3.395 (1.082-10.651) |
| Cirrhosis | 0.017 | 2.867 (1.207-6.810) |
| Preoperative CA19-9 > 150 U/L | 0.155 | 1.493 (0.859-2.593) |
| Intraoperative blood loss > 500 mL | 0.016 | 2.240 (1.162-4.318) |
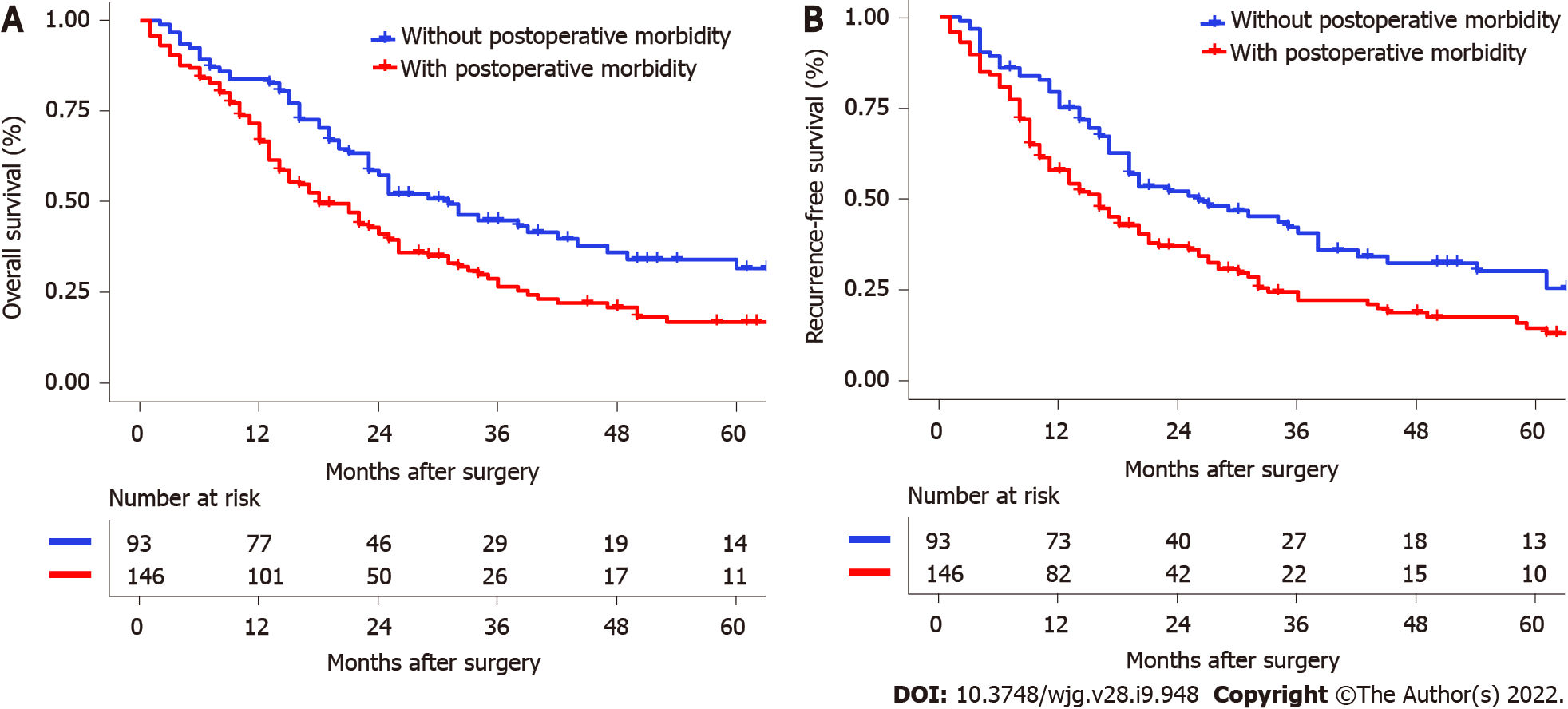
Table 4 shows the relationships between the patient survival outcomes and perioperative morbidity. Over the median 19.0-mo follow-up period, tumor recurrence and death were apparent in 76.7% (112/146) and 71.9% (105/146), respectively, of patients with postoperative morbidity and in 64.5% (60/93) and 59.1% (55/93), respectively, of patients who did not experience morbidity (recurrence, P = 0.041; death, P = 0.041). The median OS and RFS were significantly lower in the patients with postoperative morbidity, as shown in Figure 2 (OS: 18.0 mo vs 31.0 mo, P = 0.003; RFS: 16.0 mo vs 26.0 mo, P = 0.002).
| Survival outcomes | Total (n = 239) | Without postoperative morbidity (n = 93) | With postoperative morbidity (n = 146) | P value |
| Period of follow-up, months1 | 19.0 (11.0, 34.0) | 15.0 (23.0, 41.0) | 16.0 (9.8, 30.0) | 0.001 |
| Death during the follow-up | 160 (66.9) | 55 (59.1) | 105 (71.9) | 0.041 |
| Recurrence during the follow-up | 172 (72.0) | 60 (64.5) | 112 (76.7) | 0.041 |
| OS, months2 | 23.0 (20.0-26.0) | 31.0 (22.4-39.6) | 18.0 (13.0-23.0) | 0.003 |
| 1-yr OS rate, % | 73.4 | 83.8 | 66.7 | |
| 3-yr OS rate, % | 34.0 | 45.5 | 26.7 | |
| 5-yr OS rate, % | 22.9 | 31.7 | 17.0 | |
| RFS, month2 | 19.0 (16.1-21.9) | 26.0 (14.1-37.9) | 16.0 (12.2-19.8) | 0.002 |
| 1-yr RFS rate, % | 64.6 | 75.1 | 54.3 | |
| 3-yr RFS rate, % | 28.7 | 40.8 | 22.4 | |
| 5-yr RFS rate, % | 18.2 | 30.4 | 13.3 |
Tables 5 and 6 present the results of the univariate and multivariate Cox regression analyses, respectively, for survival prediction. The multivariate analysis identified postoperative morbidity was independently associated with decreased OS (HR: 1.557, 95%CI: 1.119-2.167, P = 0.009) and RFS (HR: 1.535, 95%CI: 1.117-2.108, P = 0.008). Furthermore, preoperative CA19-9 > 150 U/L, maximum tumor size > 3 cm, lymph node metastasis, macrovascular invasion, and poor tumor differentiation were also observed to be risk factors for both OS and RFS.
| Variables | Univariable analyses | Multivariable analyses1 | ||
| P value | HR (95%CI) | P value | HR (95%CI) | |
| Age > 60 yr | 0.341 | 1.190 (0.832-1.730) | ||
| Male sex | 0.754 | 1.052 (0.766-1.445) | ||
| ASA score > 2 | 0.333 | 1.282 (0.775-2.120) | ||
| Obesity | 0.772 | 0.928 (0.561-1.536) | ||
| Diabetes mellitus | 0.063 | 1.595 (0.975-2.609) | 0.288 | 1.324 (0.789-2.224) |
| Cirrhosis | 0.222 | 1.283 (0.861-1.912) | ||
| Preoperative CA19-9 > 150 U/L | 0.009 | 1.522 (1.112-2.083) | 0.015 | 1.485 (1.079-2.044) |
| Maximum tumor size > 3 cm | < 0.001 | 1.809 (1.296-2.525) | 0.001 | 1.805 (1.290-2.526) |
| Macrovascular invasion | 0.014 | 1.507 (1.088-2.087) | 0.012 | 1.527 (1.099-2.122) |
| Microvascular invasion | 0.005 | 1.588 (1.151-2.192) | 0.102 | 1.324 (0.946-1.853) |
| Peripheral nerve invasion | 0.663 | 1.075 (0.776-1.488) | ||
| Poor tumor differentiation | 0.005 | 1.608 (1.158-2.231) | 0.003 | 1.654 (1.188-2.302) |
| Intraoperative blood transfusion | 0.316 | 1.186 (0.850-1.654) | ||
| Intraoperative blood loss > 500 mL | 0.593 | 1.108 (0.761-1.612) | ||
| Major hepatectomy | 0.634 | 1.087 (0.771-1.531) | ||
| LN metastasis | 0.016 | 1.551 (1.086-2.215) | 0.021 | 1.527 (1.067-2.186) |
| Bismuth type, III-IV | 0.346 | 1.163 (0.849-1.593) | ||
| Preoperative drainage | 0.721 | 0.939 (0.665-1.326) | ||
| Postoperative morbidity | 0.003 | 1.635 (1.178-2.269) | 0.009 | 1.557 (1.119-2.167) |
| Variables | Univariable analyses | Multivariable analyses1 | ||
| P value | HR (95%CI) | P value | HR (95%CI) | |
| Age > 60 yr | 0.330 | 1.201 (0.850-1.696) | ||
| Male sex | 0.998 | 1.002 (0.793-1.136) | ||
| ASA score > 2 | 0.457 | 1.210 (0.732-1.997) | ||
| Obesity | 0.911 | 0.973 (0.604-1.568) | ||
| Diabetes mellitus | 0.035 | 1.654 (1.036-2.264) | 0.177 | 1.403 (0.858-2.295) |
| Cirrhosis | 0.247 | 1.260 (0.852-1.863) | ||
| Preoperative CA19-9 > 150 U/L | 0.002 | 1.617 (1.193-2.192) | 0.012 | 1.487 (1.092-2.024) |
| Maximum tumor size > 3 cm | 0.002 | 1.695 (1.223-2.351) | 0.002 | 1.665 (1.198-2.314) |
| Macrovascular invasion | 0.008 | 1.534 (1.120-2.100) | 0.011 | 1.514 (1.101-2.081) |
| Microvascular invasion | 0.009 | 1.524 (1.118-2.088) | 0.121 | 1.295 (0.934-1.794) |
| Peripheral nerve invasion | 0.683 | 1.068 (0.780-1.462) | ||
| Poor tumor differentiation | 0.007 | 1.547 (1.124-2.129) | 0.006 | 1.575 (1.141-2.173) |
| Intraoperative blood transfusion | 0.251 | 1.208 (0.875-1.668) | ||
| Intraoperative blood loss > 500 mL | 0.819 | 1.043 (0.729-1.490) | ||
| Major hepatectomy | 0.978 | 0.995 (0.718-1.379) | ||
| LN metastasis | 0.010 | 1.573 (1.114-2.220) | 0.017 | 1.528 (1.080-2.157) |
| Bismuth type, III-IV | 0.788 | 1.042 (0.771-1.410) | ||
| Preoperative drainage | 0.517 | 0.895 (0.640-1.252) | ||
| Postoperative morbidity | 0.003 | 1.169 (1.180-2.220) | 0.008 | 1.535 (1.117-2.108) |
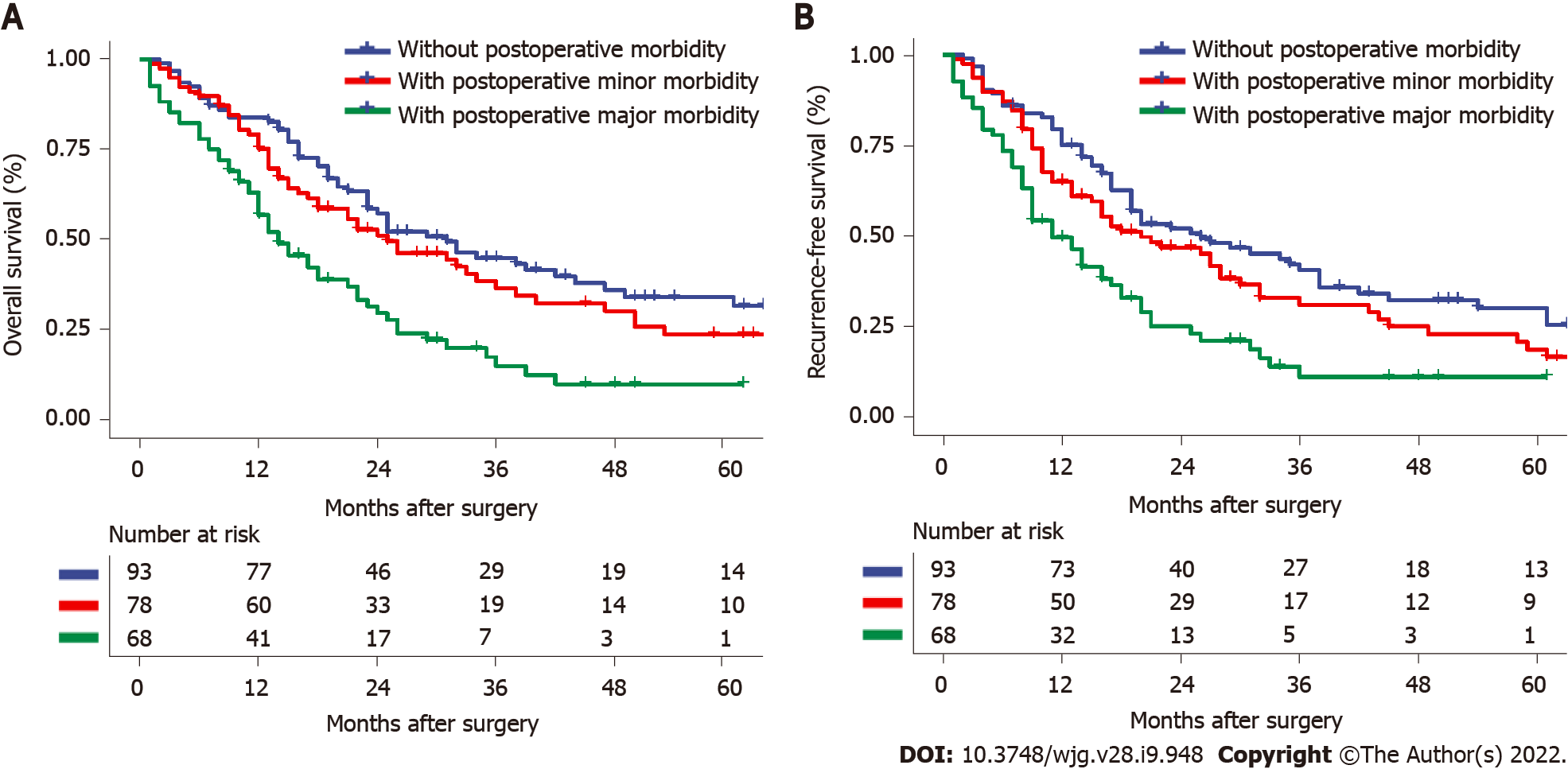
Furthermore, based on the severity of postoperative morbidity, major morbidity was associated with both lower OS and RFS, as shown in Figure 3 (OS: HR: 2.175; 95%CI: 1.470-3.216, P < 0.001; RFS: HR: 2.054; 95%CI: 1.400-3.014, P < 0.001).
It is difficult to verify and define the quality of surgery, whether assessed on the level of outcome, process, or system[24]. As a tumor-related surgical quality measure, postoperative morbidity has been an increasingly interesting topic. In assessing a potential link between postoperative complications and outcomes in cancer patients, it is necessary to determine the factors leading to postoperative morbidity and the level of morbidity that may result in an unfavorable outcome[25]. Postoperative morbidity, therefore, is an indication of the quality of the surgery and may also act as a reliable prognostication of outcomes with the potential for therapeutic application. Thus, to reduce the incidence of perioperative morbidity, it is important to identify its contributory factors.
Here, we examined the prognostic impacts of 30-d morbidity in 239 HCCA patients after curative resection. The findings showed that perioperative morbidity negatively impacted both OS and RFS, indicating the value of reducing postoperative morbidity to improve patient outcomes. In this study, postoperative morbidity occurred in 146 (61.1%) patients, of which 68 (28.5%) experienced major morbidity. These findings support those of other studies. Hasegawa et al[19] observed a major postoperative complication (grade 3 or more) rate of 46.8%[26]. Gerhards et al[27] described a postoperative morbidity rate of 65.0% in patients following hemihepatectomy[27], while Dar et al[28] observed complications in approximately 66.7% of patients within 90 d[28]. In addition, a study from Japan observed that 21 patients (35.0%) had remarkable postoperative complications, while the presence of complications predicted worse outcomes in intrahepatic cholangiocarcinoma patients[14]. A large-sample multicenter study from China indicated that 758 (35.1%) out of 2161 HCC patients experienced morbidity within 30 d, and the median OS and time-to-recurrence in these patients were poorer (48.1 mo vs 91.6 mo and 19.8 mo vs 46.1 mo, respectively)[8]. However, no studies have investigated the link between postoperative morbidity and prognosis in HCCA patients.
Both clinicopathological and operative variables were found to differ significantly in relation to postoperative morbidity, including obesity, diabetes mellitus, cirrhosis, and intraoperative blood loss > 500 mL. Many previous studies have used propensity score matching to balance the intergroup baseline features in evaluating the effect of postoperative complications on outcomes[29,30]. However, as postoperative 30-d morbidity is itself a short-term outcome, it is not appropriate to adopt this statistical approach, which may increase, rather than decrease, selection bias between the groups. In contrast, classical statistical approaches are appropriate to determine the link between postoperative morbidity and outcomes with adjustment for confounding factors.
It is important to identify the risk factors for postoperative morbidity to reduce its incidence. Here, we specifically investigated the independent risk factors for morbidity and identified obesity, diabetes mellitus, cirrhosis, and intraoperative blood loss > 500 mL. These findings are significant for guiding clinical practice. Similar conclusions have been reported; for example, a major morbidity rate of 40% was observed after liver resection in obese or overweight patients[31,32]. There is evidence to explain this phenomenon, namely, hepatic steatosis associated with obesity may adversely affect the regeneration of liver remnants and thus influence morbidity[33]. During the perioperative period, obese patients should be instructed by dieticians to adjust their dietary habits and properly match their nutritional structure. It is known that obesity is closely related to chronic liver diseases, such as steatosis, nonalcoholic steatohepatitis, and other comorbidities, including diabetes[34]. Moreover, the presence of diabetes mellitus is known to be linked to postoperative complications after HCCA surgery[35]. For severe diabetes, the clinician needs to effectively control blood glucose levels before surgery with the assistance of endocrinologists. In addition to the above two risk groups related to metabolism, for patients with cirrhosis, due to their worse liver function, surgeons should evaluate the remaining liver volume and reserve function more carefully before surgery and pay more attention to the prevention of complications, including PHLF, pleural effusion, abdominal hemorrhage, and biliary infection. Notably, cirrhosis may cause poor blood coagulation, making it more difficult to control the amount of bleeding during surgery[36]. For patients with poor liver function and coagulation dysfunction, intraoperative infusion of plasma or cryoprecipitate may help to reduce intraoperative bleeding. For patients with severe liver cirrhosis, the surgeon should use Pringle’s maneuver to obstruct the temporary hilar of the liver for hepatectomy. In addition, the anesthetist should ensure low central venous pressure to reduce the amount of bleeding during the surgery. Moreover, the vast majority of intraoperative bleeding occurs during liver resection. With new medical advances, many kinds of instruments can be used for liver resection: Ultrasonic knife, electrocautery (bipolar, monopolar, or water sealed bipolar), and radiofrequency-assisted liver resection. However, which can better prevent intraoperative bleeding may be related to the patient's liver condition and the operator's habits, and it is worthy of further study. As this study showed that postoperative morbidity (especially major morbidity) can affect the oncological prognosis of HCCA after curative resection, adjusting the above risk factors can reduce complications and also improve the prognosis of patients. In our opinion, only through multidisciplinary treatment can we reduce the postoperative morbidity of patients who undergo curative HCCA resection.
In other cancers, postoperative morbidity may be an independent predictor of poor prognostic outcome, including colorectal liver metastasis[37], HCC[8,38,39], pancreatic cancer[40], and esophageal cancer[41]. Although the precise association between postoperative morbidity and unfavorable prognostic outcomes remains to be elucidated, there are several possible explanations. Previous studies have shown that major surgery can induce systemic inflammation, with increased secretion of inflammatory cytokines, including interleukin-1 and interleukin-6, which contributes to cancer angiogenesis, proliferation, growth, and metastases[42-44]. In addition, severe systematic inflammation caused by postoperative morbidity may lead to an immunosuppressive condition and state, which can regulate the reduction of tumor monitoring and may lead to both metastasis and disease-specific death[15,42]. Notably, the postoperative stress response can inhibit cell-mediated immune function. Consequently, during the period of postoperative morbidity and relative immunosuppression caused by postoperative stress, residual malignant cells may proliferate[45]. Therefore, postoperative 30-d morbidity may negatively impact long-term oncological outcomes.
There are several limitations to this study. Specifically, it was a single-institution study with a retrospective design. Despite this, the database was established by standardized surgical techniques and perioperative management, thus preventing some limitations of multicenter, population-based, or national studies. Nevertheless, the impact of postoperative morbidity on the prognosis of HCCA patients still requires evaluation using a larger prospective study. In addition, in this study, patients who received adjuvant chemotherapy and radiotherapy were excluded. Some previous studies have demonstrated a benefit of prognosis for patients following surgery who received postoperative adjuvant therapy[46,47]. However, adjuvant therapy cannot be administered immediately when morbidities occur after surgery. As a result, we believed it was better to exclude patients who received adjuvant therapy to more accurately reflect the impact of postoperative complications on prognosis.
In summary, the results of this study clearly show that postoperative morbidity both lessens long-term survival and raises tumor recurrence in HCCA patients following curative resection. Independent risk factors for postoperative morbidity included diabetes, obesity, liver cirrhosis, and intraoperative blood loss > 500 mL. Clinicians should further optimize preoperative management, surgical procedures, and perioperative care to prevent complications and thus improve both short-term and long-term oncological prognoses.
Postoperative complications after surgery for hilar cholangiocarcinoma (HCCA) are common; but, whether it has an adverse impact on oncological prognosis is still unknown.
Our study aimed to determine whether there is an association between the presence of postoperative complication and oncological prognosis following surgery for HCCA. Moreover, our study assessed the independent risk factors for the occurrence of postoperative complication.
We aimed to evaluate the influence of postoperative morbidity on tumor recurrence and mortality after curative resection for HCCA.
Patients with diagnosed HCCA following curative resection between January 2010 and December 2017 at our hospital were enrolled. The independent risk factors for postoperative comlication within 30 d after surgery were investigated, and links between postoperative morbidity and patient characteristics and survival outcomes were assessed. Postoperative morbidities were divided into five grades according to the Clavien-Dindo classification, and major morbidities were defined as Clavien-Dindo ≥ 3. Univariate and multivariate Cox regression analyses were used to evaluate the risk factors for recurrence-free survival (RFS) and overall survival (OS).
Postoperative complication occurred in 146 out of 239 patients (61.1%). Multivariate logistic regression revealed that cirrhosis, intraoperative blood loss > 500 mL, diabetes mellitus, and obesity were independently associated with postoperative complication. And, postoperative complication was associated with decreased OS and RFS (OS: 18.0 mo vs 31.0 mo, respectively, P = 0.003; RFS: 16.0 mo vs 26.0 mo, respectively, P = 0.002). Multivariate Cox regression analysis indicated that postoperative morbidity was independently associated with decreased OS [hazard ratios (HR): 1.557, 95% confidence interval (CI): 1.119-2.167, P = 0.009] and RFS (HR: 1.535, 95%CI: 1.117-2.108, P = 0.008). Moreover, major morbidity was independently associated with decreased OS (HR: 2.175; 95%CI: 1.470-3.216, P < 0.001) and RFS (HR: 2.054; 95%CI: 1.400-3.014, P < 0.001) after curative resection for HCCA.
Postoperative complication (especially major complication) may be independently associated with poor prognosis in HCCA patients following curative resection.
Clinicians should further optimize preoperative management, surgical procedures, and perioperative care to prevent complications and thus improve both short-term and long-term oncological prognoses.
| 1. | Blechacz B. Cholangiocarcinoma: Current Knowledge and New Developments. Gut Liver. 2017;11:13-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 244] [Cited by in RCA: 360] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 2. | Robles R, Sánchez-Bueno F, Ramírez P, Brusadin R, Parrilla P. Liver transplantation for hilar cholangiocarcinoma. World J Gastroenterol. 2013;19:9209-9215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med. 1965;38:241-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 577] [Cited by in RCA: 503] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 4. | Ramos Rubio E. [Radical surgery for hilar cholangiocarcinoma (Klatskin tumor)]. Cir Esp. 2007;82:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Lau SH, Lau WY. Current therapy of hilar cholangiocarcinoma. Hepatobiliary Pancreat Dis Int. 2012;11:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Hu HJ, Jin YW, Shrestha A, Ma WJ, Wang JK, Liu F, Zhu YY, Zhou RX, Regmi P, Cheng NS, Li FY. Predictive factors of early recurrence after R0 resection of hilar cholangiocarcinoma: A single institution experience in China. Cancer Med. 2019;8:1567-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Liu ZP, Zhang QY, Chen WY, Huang YY, Zhang YQ, Gong Y, Jiang Y, Bai J, Chen ZY, Dai HS. Evaluation of Four Lymph Node Classifications for the Prediction of Survival in Hilar Cholangiocarcinoma. J Gastrointest Surg. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Li LQ, Liang L, Sun LY, Li C, Wu H, Zhang YM, Zhang WG, Wang H, Zhou YH, Gu WM, Chen TH, Li J, Liang YJ, Xu QR, Diao YK, Jia HD, Wang MD, Zhang CW, Shen F, Huang DS, Yang T. Postoperative morbidity adversely impacts long-term oncologic prognosis following hepatectomy for hepatocellular carcinoma: A multicenter observational study. Eur J Surg Oncol. 2021;47:2551-2560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Ridwelski K, Meyer F, Schmidt U, Lippert H. [Results of surgical treatment in ampullary and pancreatic carcinoma and its prognostic parameters after R0-resection]. Zentralbl Chir. 2005;130:353-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Li QG, Li P, Tang D, Chen J, Wang DR. Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol. 2013;19:4060-4065. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 106] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 11. | Kanda M, Ito S, Mochizuki Y, Teramoto H, Ishigure K, Murai T, Asada T, Ishiyama A, Matsushita H, Tanaka C, Kobayashi D, Fujiwara M, Murotani K, Kodera Y. Multi-institutional analysis of the prognostic significance of postoperative complications after curative resection for gastric cancer. Cancer Med. 2019;8:5194-5201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Zimmermann MS, Wellner U, Laubert T, Ellebrecht DB, Bruch HP, Keck T, Schlöricke E, Benecke CR. Influence of Anastomotic Leak After Elective Colorectal Cancer Resection on Survival and Local Recurrence: A Propensity Score Analysis. Dis Colon Rectum. 2019;62:286-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Nordholm-Carstensen A, Rolff HC, Krarup PM. Differential Impact of Anastomotic Leak in Patients With Stage IV Colonic or Rectal Cancer: A Nationwide Cohort Study. Dis Colon Rectum. 2017;60:497-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Miyata T, Yamashita YI, Yamao T, Umezaki N, Tsukamoto M, Kitano Y, Yamamura K, Arima K, Kaida T, Nakagawa S, Imai K, Hashimoto D, Chikamoto A, Ishiko T, Baba H. Prognostic impacts of postoperative complications in patients with intrahepatic cholangiocarcinoma after curative operations. Int J Clin Oncol. 2017;22:526-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5245] [Cited by in RCA: 5853] [Article Influence: 234.1] [Reference Citation Analysis (1)] |
| 16. | van Keulen AM, Buettner S, Besselink MG, Busch OR, van Gulik TM, Ijzermans JNM, de Jonge J, Polak WG, Swijnenburg RJ, Groot Koerkamp B, Erdmann JI, Olthof PB. Surgical morbidity in the first year after resection for perihilar cholangiocarcinoma. HPB (Oxford). 2021;23:1607-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Ribero D, Zimmitti G, Aloia TA, Shindoh J, Fabio F, Amisano M, Passot G, Ferrero A, Vauthey JN. Preoperative Cholangitis and Future Liver Remnant Volume Determine the Risk of Liver Failure in Patients Undergoing Resection for Hilar Cholangiocarcinoma. J Am Coll Surg. 2016;223:87-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 18. | Kennedy TJ, Yopp A, Qin Y, Zhao B, Guo P, Liu F, Schwartz LH, Allen P, D'Angelica M, Fong Y, DeMatteo RP, Blumgart LH, Jarnagin WR. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB (Oxford). 2009;11:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Hasegawa S, Ikai I, Fujii H, Hatano E, Shimahara Y. Surgical resection of hilar cholangiocarcinoma: analysis of survival and postoperative complications. World J Surg. 2007;31:1256-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 154] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 20. | Wang JK, Hu HJ, Shrestha A, Ma WJ, Yang Q, Liu F, Cheng NS, Li FY. Can preoperative and postoperative CA19-9 levels predict survival and early recurrence in patients with resectable hilar cholangiocarcinoma? Oncotarget. 2017;8:45335-45344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 26155] [Article Influence: 1188.9] [Reference Citation Analysis (2)] |
| 22. | Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F. The "50-50 criteria" on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005;242:824-828, discussion 828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 840] [Article Influence: 40.0] [Reference Citation Analysis (1)] |
| 23. | National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32:470-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 632] [Reference Citation Analysis (0)] |
| 24. | Takahashi Y, Ebata T, Yokoyama Y, Igami T, Sugawara G, Nagino M. Surgical treatment of perihilar cholangiocarcinoma in octogenarians: a single center experience. J Hepatobiliary Pancreat Sci. 2013;20:324-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Best WR, Khuri SF, Phelan M, Hur K, Henderson WG, Demakis JG, Daley J. Identifying patient preoperative risk factors and postoperative adverse events in administrative databases: results from the Department of Veterans Affairs National Surgical Quality Improvement Program. J Am Coll Surg. 2002;194:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 209] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 26. | Zhu WH, Xie WY, Zhang ZD, Li S, Zhang DF, Liu YJ, Zhu JY, Leng XS. Postoperative Complications and Survival Analysis of Surgical Resection for Hilar Cholangiocarcinoma: A Retrospective Study of Fifty-Nine Consecutive Patients. Chin Med Sci J. 2020;35:157-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Gerhards MF, van Gulik TM, de Wit LT, Obertop H, Gouma DJ. Evaluation of morbidity and mortality after resection for hilar cholangiocarcinoma--a single center experience. Surgery. 2000;127:395-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 126] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 28. | Dar FS, Atiq M, Shahzadi N, Ainy SK, Rana A, Bhatti ABH. Outcomes after Surgical Resection of Hilar Cholangiocarcinoma. J Coll Physicians Surg Pak. 2019;29:874-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Tam V, Luketich JD, Winger DG, Sarkaria IS, Levy RM, Christie NA, Awais O, Shende MR, Nason KS. Cancer Recurrence After Esophagectomy: Impact of Postoperative Infection in Propensity-Matched Cohorts. Ann Thorac Surg. 2016;102:1638-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Memeo R, de Blasi V, Adam R, Goéré D, Laurent A, de'Angelis N, Piardi T, Lermite E, Herrero A, Navarro F, Sa Cunha A, Pessaux P; French colorectal liver metastases working group - Association Française de Chirurgie (AFC). Postoperative Infectious Complications Impact Long-Term Survival in Patients Who Underwent Hepatectomies for Colorectal Liver Metastases: a Propensity Score Matching Analysis. J Gastrointest Surg. 2018;22:2045-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Langella S, Russolillo N, Forchino F, Lo Tesoriere R, D'Eletto M, Ferrero A. Impact of obesity on postoperative outcome of hepatic resection for colorectal metastases. Surgery. 2015;158:1521-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Balzan S, Nagarajan G, Farges O, Galleano CZ, Dokmak S, Paugam C, Belghiti J. Safety of liver resections in obese and overweight patients. World J Surg. 2010;34:2960-2968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Paternostro R, Sieghart W, Trauner M, Pinter M. Cancer and hepatic steatosis. ESMO Open. 2021;6:100185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | Pi-Sunyer FX. Medical hazards of obesity. Ann Intern Med. 1993;119:655-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 785] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 35. | Kanekiyo S, Takeda S, Iida M, Nishiyama M, Kitahara M, Shindo Y, Tokumitsu Y, Tomochika S, Tsunedomi R, Suzuki N, Abe T, Yoshino S, Hazama S, Ueno T, Nagano H. Efficacy of perioperative immunonutrition in esophageal cancer patients undergoing esophagectomy. Nutrition. 2019;59:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 36. | Hackl C, Schlitt HJ, Renner P, Lang SA. Liver surgery in cirrhosis and portal hypertension. World J Gastroenterol. 2016;22:2725-2735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 59] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 37. | Matsuda A, Matsumoto S, Seya T, Matsutani T, Kishi T, Yokoi K, Wang P, Uchida E. Does postoperative complication have a negative impact on long-term outcomes following hepatic resection for colorectal liver metastasis? Ann Surg Oncol. 2013;20:2485-2492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 38. | Chok KS, Ng KK, Poon RT, Lo CM, Fan ST. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg. 2009;96:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 165] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 39. | Kusano T, Sasaki A, Kai S, Endo Y, Iwaki K, Shibata K, Ohta M, Kitano S. Predictors and prognostic significance of operative complications in patients with hepatocellular carcinoma who underwent hepatic resection. Eur J Surg Oncol. 2009;35:1179-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 40. | Aoyama T, Murakawa M, Katayama Y, Yamaoku K, Kanazawa A, Higuchi A, Shiozawa M, Morimoto M, Yoshikawa T, Yamamoto N, Rino Y, Masuda M, Morinaga S. Impact of postoperative complications on survival and recurrence in pancreatic cancer. Anticancer Res. 2015;35:2401-2409. [PubMed] |
| 41. | Li KK, Wang YJ, Liu XH, Tan QY, Jiang YG, Guo W. The effect of postoperative complications on survival of patients after minimally invasive esophagectomy for esophageal cancer. Surg Endosc. 2017;31:3475-3482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 42. | Wortel CH, van Deventer SJ, Aarden LA, Lygidakis NJ, Büller HR, Hoek FJ, Horikx J, ten Cate JW. Interleukin-6 mediates host defense responses induced by abdominal surgery. Surgery. 1993;114:564-570. [PubMed] |
| 43. | Elaraj DM, Weinreich DM, Varghese S, Puhlmann M, Hewitt SM, Carroll NM, Feldman ED, Turner EM, Alexander HR. The role of interleukin 1 in growth and metastasis of human cancer xenografts. Clin Cancer Res. 2006;12:1088-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 231] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 44. | Wong VK, Malik HZ, Hamady ZZ, Al-Mukhtar A, Gomez D, Prasad KR, Toogood GJ, Lodge JP. C-reactive protein as a predictor of prognosis following curative resection for colorectal liver metastases. Br J Cancer. 2007;96:222-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 45. | McDonald B, Spicer J, Giannais B, Fallavollita L, Brodt P, Ferri LE. Systemic inflammation increases cancer cell adhesion to hepatic sinusoids by neutrophil mediated mechanisms. Int J Cancer. 2009;125:1298-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 184] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 46. | Grendar J, Grendarova P, Sinha R, Dixon E. Neoadjuvant therapy for downstaging of locally advanced hilar cholangiocarcinoma: a systematic review. HPB (Oxford). 2014;16:297-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 47. | Gerhards MF, van Gulik TM, González González D, Rauws EA, Gouma DJ. Results of postoperative radiotherapy for resectable hilar cholangiocarcinoma. World J Surg. 2003;27:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 119] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gusho CA, Isaji S, Kim BS, Ziogas IA S-Editor: Fan JR L-Editor: A P-Editor: Fan JR