Published online Aug 14, 2022. doi: 10.3748/wjg.v28.i30.4163
Peer-review started: March 10, 2022
First decision: April 11, 2022
Revised: April 21, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: August 14, 2022
Processing time: 152 Days and 16.5 Hours
The critical diagnostic criteria for esophagogastric junction outflow obstruction (EGJOO) were published in the latest Chicago Classification version 4.0 (CCv4.0). In addition to the previous criterion [elevated integrated relaxation pressure (IRP) in supine position], manometric diagnosis of EGJOO requires meeting the criteria of elevated median-IRP during upright wet swallows and elevated intrabolus pressure. However, with the diagnostic criteria modification, the change in manometric features of EGJOO remained unclear.
To evaluate the esophageal motility characteristics of patients with EGJOO and select valuable parameters for confirming the diagnosis of EGJOO.
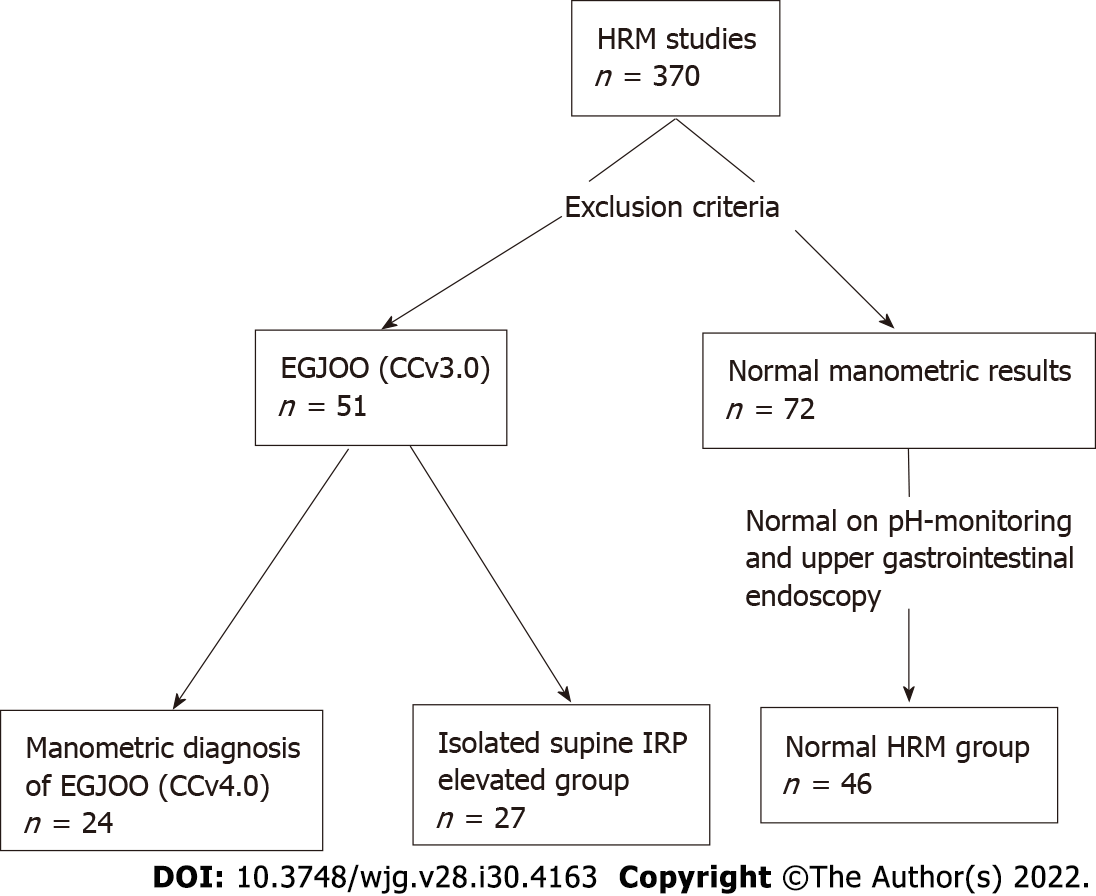
We performed a retrospective analysis of 370 patients who underwent high-resolution manometry with 5 mL water swallows × 10 in supine, × 5 in upright position and the rapid drink challenge (RDC) with 200 mL water from November 2016 to November 2021 at Peking University First Hospital. Fifty-one patients with elevated integrated supine IRP and evidence of peristalsis were enrolled, with 24 patients meeting the updated manometric EGJOO diagnosis (CCv4.0) as the EGJOO group and 27 patients not meeting the updated EGJOO criteria as the isolated supine IRP elevated group (either normal median IRP in upright position or less than 20% of supine swallows with elevated IBP). Forty-six patients with normal manometric features were collected as the normal high-resolution manometry (HRM) group. Upper esophageal sphincter (UES), esophageal body, and lower esophageal sphincter (LES) parameters were compared between groups.
Compared with the normal HRM group, patients with EGJOO (CCv4.0) had significantly lower proximal esophageal contractile integral (PECI) and proximal esophageal length (PEL), with elevated IRP on RDC (P < 0.05 for each comparison), while isolated supine IRP elevated patients had no such feature. Patients with EGJOO also had more significant abnormalities in the esophagogastric junction than isolated supine IRP elevated patients, including higher LES resting pressure (LESP), intrabolus pressure, median supine IRP, median upright IRP, and IRP on RDC (P < 0.05 for each comparison). Patients with dysphagia had significantly lower PECI and PEL than patients without dysphagia among the fifty-one with elevated supine IRP. Further multivariate analysis revealed that PEL, LESP, and IRP on RDC are factors associated with EGJOO. The receiver-operating characteristic analysis showed UES nadir pressure, PEL, PECI, LESP, and IRP on RDC are parameters supportive for confirming the diagnosis of EGJOO.
Based on CCv4.0, patients with EGJOO have more severe esophagogastric junction dysfunction and are implicated in the proximal esophagus. Additionally, several parameters are supportive for confirming the diagnosis of EGJOO.
Core Tip: This is a retrospective study to evaluate the motility features of esophagogastric junction outflow obstruction (EGJOO). This is the first detailed study of EGJOO based on the latest Chicago Classification. Patients with EGJOO showed more substantial abnormalities at the esophagogastric junction than patients who met the previous criteria, and the motility disorder of EGJOO is implicated in the proximal esophagus. Additionally, the upper esophageal sphincter nadir pressure, proximal esophageal contractile integral, proximal esophageal length, lower esophageal sphincter resting pressure, and integrated relaxation pressure on rapid drink challenge contribute to confirming the diagnosis of EGJOO.
- Citation: Li YY, Lu WT, Liu JX, Wu LH, Chen M, Jiao HM. Changes in the esophagogastric junction outflow obstruction manometric feature based on the Chicago Classification updates. World J Gastroenterol 2022; 28(30): 4163-4173
- URL: https://www.wjgnet.com/1007-9327/full/v28/i30/4163.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i30.4163
Esophagogastric junction outflow obstruction (EGJOO) is a common type of esophageal motility disorder in patients with dysphagia or chest pain. EGJOO includes a group of heterogeneous disorders with common manometric features for esophageal outflow obstruction. Progress has been made toward understanding the manometric features and symptoms of patients who meet the EGJOO criteria[1-5]. The Chicago Classification version 4.0 (CCv4.0) updated the critical diagnostic criteria for the manometric diagnosis of EGJOO, including increased median-integrated relaxation pressure (IRP) in supine and upright positions, ≥ 20% elevated intrabolus pressure (IBP) in the supine position, and evidence of peristalsis[1]. A clinically relevant conclusive diagnosis of EGJOO requires a manometric diagnosis of EGJOO as described above, and clinically relevant symptoms with at least one of the complementary tests, including timed barium esophagram and functional lumen imaging probe. Additional provocative tests including rapid drink challenge (RDC), solid test swallows, or pharmacologic provocation may also strengthen the confidence in an EGJOO diagnosis and helps to identify the causes of symptoms, particularly in borderline cases. Compared with the previous version (v3.0)[6], the new diagnostic criteria provided a more rigorous definition for EGJOO by adding criteria for median IRP in the secondary position, IBP, clinically relevant symptoms, and complementary tests, which aid in distinguishing pathological motility disorder and abnormal manometry caused by mechanical effect, opioid use, or other nonpathological motility disorders[7]. However, the change in manometric features of EGJOO with the diagnostic criteria modification remained unclear. This study aims to investigate the esophageal motility features of patients with the manometric diagnosis of EGJOO and to identify high-resolution manometry (HRM) parameters that are supportive for confirming the diagnosis of EGJOO.
Patients who completed esophageal HRM and upper gastrointestinal endoscopy from November 2016 to November 2021 at Peking University First Hospital were retrospectively analyzed. Exclusion criteria included: (1) Patients under 18 years of age; (2) A history of upper gastrointestinal or mediastinal surgery; (3) Previous endoscopic treatment for esophageal motor disorders; (4) Diseases with abnormal intraabdominal pressure, such as intestinal obstruction or ascites; (5) Use of opiates; and (6) Secondary factors identified by upper gastrointestinal endoscopy or endoscopic ultrasonography, especially for hiatal hernia, infiltrative disease, mechanical obstruction, and extrinsic compression. The normal HRM group was obtained from patients who underwent HRM for mild symptoms such as dysphagia, retrosternal pain, regurgitation, or heartburn, with normal HRM results. The patients also fulfilled normal results in pH-monitoring and upper gastrointestinal endoscopy, in order to exclude the possibility of organic diseases. Demographic data, including age, gender, body mass index (BMI), previous medical and surgical history were collected, and symptoms were extracted from self-report questionnaires completed by patients before HRM. The Institutional Review Board (IRB) of the Peking University First Hospital approved the study protocol (2022-099). The IRB waived the requirement for informed consent because our retrospective analysis used completely anonymized data.
HRM studies were conducted according to standard clinical protocol, using a 4.2-mm outer diameter, 36-sensor solid-state HRM catheter (ManoScan™, Medtronic, Los Angeles, CA, United States)[8]. Experienced nurses performed nasal canal anesthesia and transnasal placement of the solid-state manometry catheter with the patient sitting upright after an 8-h fast. Sensors were positioned to ensure a complete record of the hypopharynx, esophagus, and proximal stomach. The manometric protocol consisted of a landmark phase captured during a quiet rest in the supine position at the beginning, followed by ten 5-mL ambient temperature water swallows in the supine position, then five 5-mL water swallows in the upright position, with 30 s between each swallow, and finally a RDC of 200 mL water in the upright position.
HRM Clouse plots were analyzed using computerized HRM analysis software (Manoview, Medtronic). All pressure measurements were referenced to the gastric pressure.
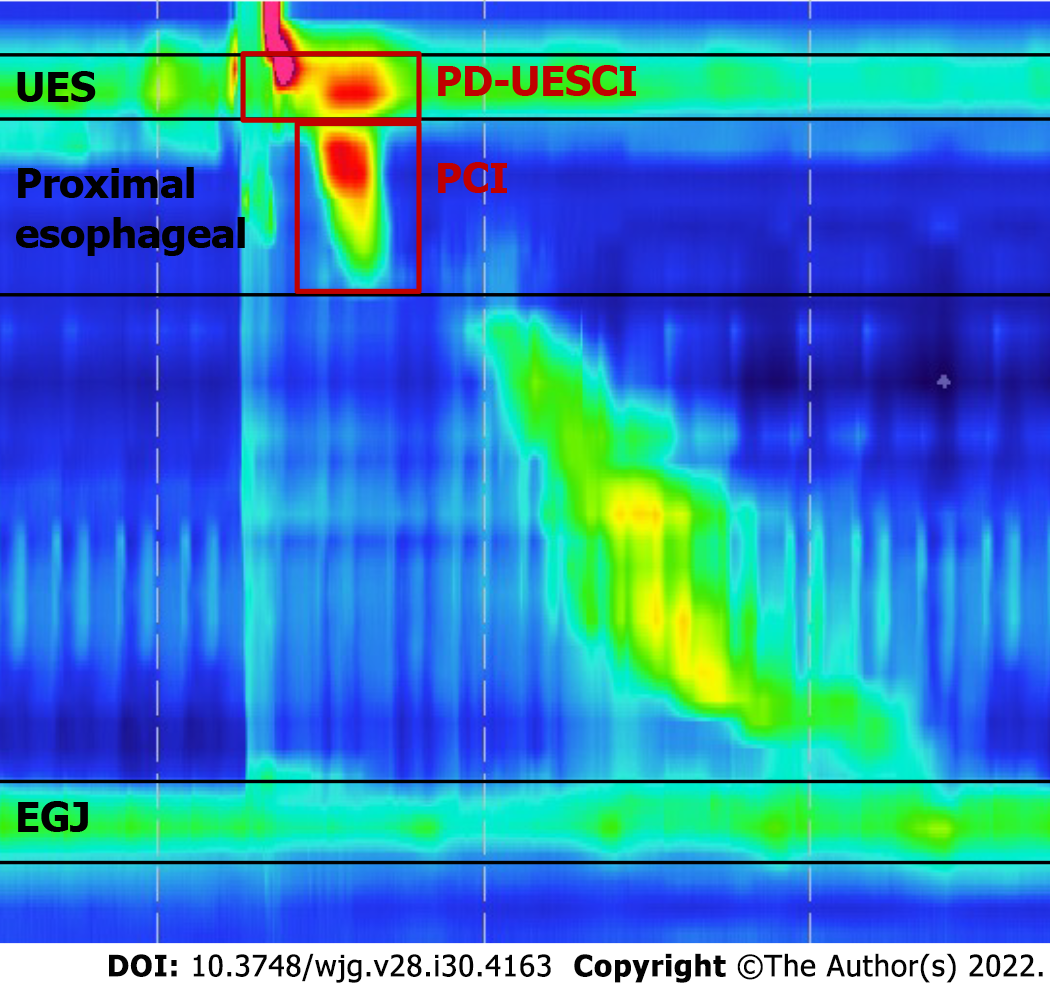
Upper esophageal sphincter parameters[9,10]: Upper esophageal sphincter (UES) parameters were measured within the UES high-pressure zone defined by a 20-mmHg isobaric contour, consisting of UES length (UESL), UES resting pressure (UESP), nadir pressure (UESNP), and postdeglutitive UES contractile integral (PD-UESCI). PD-UESCI was measured by the smart mouse at the beginning of the deglutitive UES relaxation to the end of the proximal esophageal contraction or the beginning of the transition zone (Figure 1).
Proximal esophageal parameters[9,11]: Proximal esophageal parameters measured from the lower border of the UES to either a break between the proximal and distal segment or the area with the lowest pressure between the proximal and distal segment of the contraction in patients showed no break in the 20-mmHg isobaric contour. Measurements of the proximal esophageal segment included proximal esophageal segment length (PEL), proximal latency (PL, defined as the time interval between UES relaxation to the transition zone), and proximal esophageal contractile integral (PECI, = amplitude × duration × length, measured using a 20-mmHg pressure threshold).
Esophageal body parameters[12]: Esophageal shortening during RDC (ES-RDC) was defined as an upward lift of lower esophageal sphincter (LES) for more than 1 cm, as measured by the length variation between the baseline position of the LES before RDC and its maximal axial position during RDC or within 60 s after the start of RDC. The distal latency (DL) and distal contraction integral (DCI) were calculated automatically using the ManoView system.
Esophagogastric junction parameters[13]: The LES resting pressure (LESP), IBP were calculated automatically using the ManoView system. The median IRP in the supine and upright positions was selected from a list of IRP in each position. The IRP on RDC was assessed in the window beginning with dilatative UES relaxation to the end of esophagogastric junction (EGJ) relaxation for free drinking lasting less than 30 s, or during the first 30 s of the window for free drinking lasting longer.
Statistical analysis was performed using SPSS 25.0, and GraphPad Prism 8.0. The chi-square test was used for the comparison of categorical variables. The Student’s t-test and analysis of variance were used to compare quantitative data with normal distribution between groups, and the results are expressed as mean ± SD. Multivariate analysis was performed with stepwise variable selection. The receiver-operating characteristics (ROC) curve was used to illustrate the diagnostic ability of the HRM parameters for EGJOO. A P value < 0.05 was considered statistically significant.
Fifty-one patients (33 female, 59.5 ± 1.7 years) fulfilling the criteria of EGJOO (CCv3.0) were identified, with supine IRP ≥ 15 mmHg (Medtronic) and evidence of peristalsis. Among them, 24 patients (14 female, 62.7 ± 2.7 years) met the manometric definitions of EGJOO (CCv4.0), while 27 patients (19 female, 56.6 ± 11.1 years) failed to meet the updated EGJOO criteria formed the isolated supine IRP elevated group, with either normal median IRP in upright position or less than 20% of supine swallows with elevated IBP. The normal HRM group comprised 46 patients (24 female, 50.2 ± 2.2 years) with normal HRM results (Figure 2). Patients in the EGJOO group were older than the normal HRM group. There was no difference in gender or BMI between these three groups. As for symptoms, among the 24 patients with manometric diagnosis of EGJOO (CCv4.0), there were seven with dysphagia and five with retrosternal pain that might be clinically relevant. Symptoms were also counted in isolated supine IRP elevated group and normal HRM group as shown in Table 1. The occurrence of dysphagia, retrosternal pain, and regurgitation did not differ between these three groups. Among the 24 patients with manometric diagnosis of EGJOO (CCv4.0), there were five patients with spastic features, five with hypercontractile features, two with ineffective motility, and twelve with no evidence of peristalsis disorders.
| EGJOO (n = 24) | Isolated supine IRP elevated (n = 27) | Normal HRM (n = 46) | P value | |
| Demographics | ||||
| Age (yr) | 62.7 ± 2.7a | 56.6 ± 11.1 | 50.2 ± 2.2 | 0.001 |
| Female, n (%) | 14 (58.3) | 19 (70.4) | 24 (52.2) | 0.312 |
| BMI (kg/m2) | 23.29 ± 0.63 | 21.88 ± 2.50 | 23.17 ± 0.68 | 0.300 |
| Dominant symptom | ||||
| Dysphagia, n (%) | 7 (29.2) | 6 (22.2) | 7 (15.2) | 0.380 |
| Retrosternal pain, n (%) | 5 (20.8) | 3 (11.1) | 8 (17.4) | 0.630 |
| Regurgitation, n (%) | 8 (33.3) | 9 (33.3) | 15 (32.6) | 0.997 |
Table 2 details the differences in manometric parameters among EGJOO, isolated supine IRP elevated group, and the normal HRM group.
| HRM findings | EGJOO (n = 24) | Isolated supine IRP elevated (n = 27) | Normal HRM (n = 46) | P value |
| UES parameters | ||||
| UESL (cm) | 3.13 ± 0.18 | 3.01 ± 0.67 | 3.34 ± 0.12 | 0.206 |
| UESP (mmHg) | 53.35 ± 5.28 | 68.12 ± 6.35 | 57.77 ± 3.35 | 0.123 |
| UESNP (mmHg) | 3.00 ± 1.43a | 3.50 ± 6.57a | -4.08 ± 0.84 | < 0.001 |
| PD-UESCI (mmHg∙s∙cm) | 430.01 ± 32.90 | 527.41 ± 37.48 | 534.13 ± 34.40 | 0.118 |
| Proximal esophageal parameters | ||||
| PEL (cm) | 4.89 ± 0.27a | 5.89 ± 0.32b | 6.08 ± 0.14 | 0.001 |
| PL (s) | 1.99 ± 0.08 | 2.05 ± 0.08 | 2.04 ± 0.07 | 0.872 |
| PECI (mmHg∙s∙cm) | 238.34 ± 35.18a | 328.00 ± 35.15 | 367.99 ± 37.88 | 0.048 |
| Esophageal body parameters | ||||
| DL (s) | 6.14 ± 0.25 | 6.85 ± 0.32 | 6.25 ± 0.14 | 0.078 |
| DCI (mmHg∙s∙cm) | 1581.21 ± 276.20 | 1655.80 ± 170.33 | 1705.41 ± 144.27 | 0.897 |
| ES-RDC (%) | 37.5% (9) | 18.5% (5) | 13.0% (6) | 0.053 |
| EGJ parameters | ||||
| LESP (mmHg) | 47.91 ± 4.05a | 35.68 ± 1.80a,b | 23.89 ± 1.34 | < 0.001 |
| IBP (mmHg) | 12.29 ± 1.37a | 7.41 ± 0.84b | 5.45 ± 0.54 | < 0.001 |
| Median supine IRP (mmHg) | 27.76 ± 2.39a | 18.74 ± 0.52a,b | 10.48 ± 0.60 | < 0.001 |
| Median upright IRP (mmHg) | 23.69 ± 2.58a | 7.32 ± 0.53b | 5.41 ± 0.84 | < 0.001 |
| IRP on RDC (mmHg) | 9.96 ± 1.78a | 3.00 ± 0.98b | 2.04 ± 0.58 | < 0.001 |
UES parameters: UESNP was significantly higher in the EGJOO group and the isolated supine IRP elevated group than in the normal HRM group. There was no significant difference in UESL, UESP, and PD-UESCI between the three groups.
Proximal esophageal parameters: Proximal esophageal contractile function was weaker in the EGJOO group than in the normal HRM group, specifically PEL and PECI. Consistently, PEL was lower in the EGJOO group than in the isolated supine IRP elevated group. There was no difference in PL in the EGJOO group, isolated supine IRP elevated group, and the normal HRM group.
Esophageal body parameters: There was no significant difference in DL, DCI, and ES-RDC among the three groups.
EGJ parameters: Patients with EGJOO exhibited stronger contractile function in EGJ than in the isolated supine IRP elevated group and the normal HRM group, including LESP, IBP, median supine IRP, median upright IRP, and IRP on RDC.
The multivariate analysis revealed that PEL, LESP, and IRP on RDC are factors associated with EGJOO (Table 3).
| Effect variables | OR | 95%CI | P value |
| PEL (cm) | 0.543 | 0.30-0.99 | 0.044 |
| LESP (mmHg) | 1.106 | 1.05-1.17 | 0.001 |
| IRP on RDC (mmHg) | 1.197 | 1.02-1.41 | 0.028 |
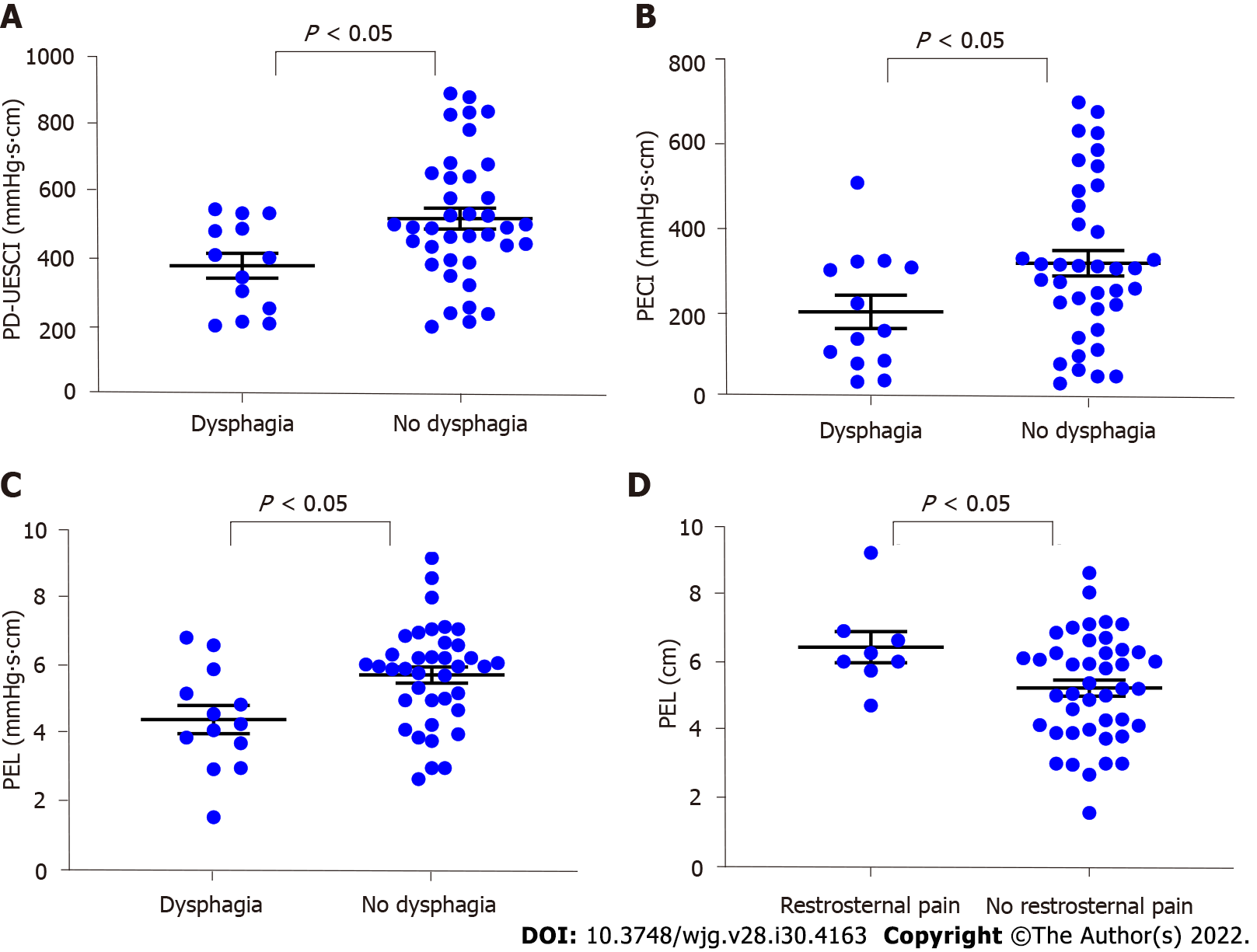
We compared parameters based on symptoms for the 51 patients with elevated IRP. Patients with dysphagia showed significantly lower PD-UESCI (377.60 ± 36.67 vs 517.14 ± 30.47 mmHg∙s∙cm, P = 0.017), PECI (200.25 ± 39.18 vs 315.08 ± 30.24 mmHg∙s∙cm, P = 0.048) and PEL (4.43 ± 0.42 vs 5.75 ± 0.24 cm, P = 0.008) than patients without dysphagia. PEL was higher in patients with retrosternal pain, compared to patients without the symptom (6.43 ± 0.46 vs 5.23 ± 0.24 cm, P = 0.046) (Figure 3).
The ROC analysis discovered HRM parameters that helped identify EGJOO (Table 4). The area under the curve (AUC) of LESP in predicting EGJOO is 0.85, with the optimal cutoff at 40.20 mmHg, yielding a sensitivity of 68.2% and specificity of 85.1%. IRP on RDC achieved an AUC value of 0.81, with the optimal cutoff at > 10.75 mmHg and sensitivity and specificity of 50.0% and 98.5%, respectively. UESNP, PEL, and PECI showed the best predictive value for EGJOO, with cutoff values of 1.15 mmHg (AUC 0.66), 4.76 cm (AUC 0.67), 312.35 mmHg∙s∙cm (AUC 0.67), respectively.
| Cutoff | AUC | 95%CI | Sensitivity (%) | Specificity (%) | |
| UESNP (mmHg) | > 1.15 | 0.66 | 0.53-0.78 | 63.6 | 68.7 |
| PEL (cm) | < 4.76 | 0.67 | 0.55-0.80 | 50.0 | 87.7 |
| PECI (mmHg∙s∙cm) | < 312.35 | 0.67 | 0.55-0.80 | 83.3 | 46.6 |
| LESP (mmHg) | > 40.20 | 0.85 | 0.75-0.94 | 68.2 | 85.1 |
| IRP on RDC (mmHg) | > 10.75 | 0.81 | 0.70-0.91 | 50.0 | 98.5 |
In this study, we mainly assessed the clinical and manometric characteristics of EGJOO based on the Chicago Classification version 4.0 (CCv4.0) to reveal potential changes in esophageal dynamics based on the new diagnostic criteria, and we identified parameters that help distinguish the EGJOO.
Based on our observations, older people had a higher likelihood of being diagnosed with EGJOO according to manometric results. The EGJOO group showed no significant difference in symptom distribution pattern compared with the isolated supine IRP elevated group and the normal HRM group. Therefore, more manometric features and additional examinations are required for a better understanding of EGJOO.
The nadir UES residual pressure (UESNP) was reported to be higher in EGJOO (CCv3.0) than in normal controls[2,14]. Within EGJOO, higher UESNP was observed in motor disorders compared to mechanical etiologies and was a potential predictor of symptom recurrence after myotomy, with a cutoff level of 2 mmHg[2]. Based on our initial findings, patients with EGJOO and isolated supine IRP had significantly higher UESNP than the normal HRM group. The findings support the hypothesis that the UES is hypertonic with impaired relaxation, which may serve as a protective mechanism to facilitate esophageal clearance and prevent aspiration pneumonitis under IRP elevation[15]. Further ROC analysis revealed that UESNP elevation might serve as a feature for confirming EGJOO.
Previous studies have linked proximal esophageal motility abnormalities to achalasia[9]. The PECI of type 1 achalasia patients was weaker than that of healthy volunteers, but there was no difference between EGJOO (CCv3.0) and health volunteers, and patients with aberrant PECI had more severe upper gastrointestinal symptoms than patients with normal PECI[9]. It is worth noting that EGJOO (CCv4.0) group had weaker PECI than the normal HRM group, while patients with isolated IRP elevation had no difference compared to the normal HRM group. PECI resulted in a limited value for confirming the diagnosis of EGJOO. Furthermore, our findings suggest that PEL is lower in patients with EGJOO than patients with isolated elevated supine IRP or normal HRM, which might also serve as a feature that strengthens the confidence in an EGJOO diagnosis. The above results indicate that based on the updated criteria, EGJOO dysfunction may involve the proximal esophagus, while patients with isolated supine IRP elevated had no such features. It is reasonable to speculate that patients with EGJOO have common changes in proximal esophageal dynamic features, although further studies are required to reveal the underlying pathophysiological mechanism.
With our current analysis of symptoms, postdeglutitive contraction of the UES and proximal esophagus were weaker, and PEL was significantly lower in patients with dysphagia compared to patients without the symptom, indicating that in patients with impaired EGJ relaxation, dysphagia may represent a potential dysfunction of the UES and proximal esophagus.
Esophageal shortening has been proposed as an outcome of longitudinal muscle contraction, and esophageal shortening during the rapid drink test was mainly associated with impaired EGJ relaxation or major peristalsis disorders, particularly achalasia[12]. In our study, the incidence of ES-RDC had a marginal difference between the three groups, which is comparable with the motor pattern observed in achalasia.
In this study, LESP increased progressively from normal HRM to the isolated supine IRP elevated and EGJOO groups, with significant differences between groups. LESP was critical in the evaluation of EGJ obstruction. Furthermore, ROC curve analysis revealed that LESP had the highest differential diagnostic efficacy of EGJOO, indicating that the value of LESP is helpful in the assessment of EGJOO.
CCv4.0 also highlights the role of ancillary manometric evaluations, such as RDC, to identify the causes of symptoms and elicit evidence of obstruction. Our study performed IRP on RDC, which was significantly higher in the EGJOO group than in other groups, while the isolated supine IRP elevated group showed no difference compared with the normal HRM group, indicating that Chicago Classification updates filtered out EGJ dysfunction with more severe obstruction. It is worth noting that IRP on RDC greater than 12 mmHg (Medtronic software) indicates achalasia and may correlate with symptom severity[1,13,16]. The ROC analysis revealed that a high IRP on RDC is useful for confirming the diagnosis of EGJOO with high specificity (98.5%), but low sensitivity (50.0%).
Based on CCv3.0, a significant proportion of EGJOO is associated with the effect of artifact, hiatal hernia, mechanical obstruction, opioid effect, or gastric volvulus, but not primary LES dysfunction. Hence, numerous studies focused on the identification of primary motility disorders and excluded motility patterns secondary to medication use, mechanical obstruction, previous surgery, or endoscopic interventions[3,4,17], which are critical in making appropriate therapeutic decisions. Since the morphology of LES is affected by position, the CCv4.0 defines IRP in the upright position and IBP; thus, the Chicago Classification update has reduced the number of clinically irrelevant diagnoses and improved the specificity for EGJOO diagnosis[7,17,18], enabling us to avoid irreversible treatment for these conditions. According to the results of this study, patients with EGJOO had multiple abnormalities in EGJ parameters compared with the isolated supine IRP elevated group, including LESP, IBP, median supine IRP, median upright IRP, and IRP on RDC, implying that the Chicago Classification update aids in the selection of EGJOO with more severe EGJ dysfunction.
Due to the limitations of the retrospective study, our study lacked data on treatment and outcomes of patients, larger cohorts are required to explore the prognostic value of the parameters mentioned above. Based on CCv4.0, additional provocative tests such as solid test swallows, or pharmacologic provocation were recommended, and complementary tests are required for a conclusive, actionable diagnosis of clinically relevant EGJOO, while our study did not include the tests mentioned above and mainly focused on the changes in the manometric diagnosis of EGJOO. Moreover, it is necessary to further investigate the pathophysiological mechanism of the changes in proximal esophageal motility of patients with EGJOO.
Conclusively, our current analysis revealed that patients with EGJOO had multiple changes in esophageal parameters based on Chicago Classification updates, especially more severe dysfunction at the esophagogastric junction than the previous diagnostic criteria, and showed multiple abnormalities at the proximal esophagus. The results illustrate that EGJOO is implicated in the proximal esophagus, and Chicago Classification updates improved the specificity for EGJOO diagnosis. Accordingly, we have expanded the valuable parameters for confirming the diagnosis of EGJOO based on CCv4.0, including UESNP, PEL, PECI, LESP, and IRP on RDC. With the advancement of EGJOO research, more contributions will be provided to the diagnosis and treatment of this type of disorder.
The critical diagnostic criteria for esophagogastric junction outflow obstruction (EGJOO) were published in the latest Chicago Classification version 4.0 (CCv4.0). However, as a result of the diagnostic criteria modifications, the changes in manometric features of EGJOO remained unclear.
To investigate the changes of EGJOO manometric features according to the Chicago Classification updates.
This study focused on evaluating the esophageal motility characteristics of patients with EGJOO, and selecting valuable parameters that are supportive for confirming the diagnosis of EGJOO.
A total of 97 patients were enrolled, with 24 patients that met the updated manometric diagnosis of EGJOO (CCv4.0), 27 patients that only met the previous criteria, and 46 patients with normal manometric features served as the normal high-resolution manometry (HRM) group for this study. We collected clinical data, HRM parameters, and conducted comparisons among groups. Factors associated with EGJOO were illustrated by multivariate analysis. Furthermore, valuable parameters that strengthen the confidence in an EGJOO diagnosis were selected by the receiver-operating characteristic analysis.
EGJOO patients revealed significantly decreased proximal esophageal contractile integral (PECI) and proximal esophageal length (PEL) compared to the normal HRM group, and the features were related to dysphagia. EGJOO patients also had more severe dysfunction of the esophagogastric junction including lower esophageal sphincter resting pressure (LESP), intrabolus pressure, median supine integrated relaxation pressure (IRP), median upright IRP, and IRP on rapid drink challenge (RDC) than patients that only met the previous criteria. Further multivariate analysis revealed that the PEL, LESP, and IRP on RDC are factors associated with EGJOO. Additionally, the upper esophageal sphincter nadir pressure, PECI, PEL, LESP, and IRP on RDC contributes to confirming the diagnosis of EGJOO.
The updates of Chicago Classification have improved the precision for identification of EGJ dysfunction that may reduce over-diagnosing for EGJOO. The motility disorder of EGJOO is implicated in the proximal esophagus, and the changes of proximal esophagus may relate to dysphagia. Additionally, there are valuable parameters that can be applied for confirming the diagnosis of EGJOO.
Further investigations are required to reveal the pathophysiological mechanism of the abnormal proximal esophageal motility showed in EGJOO patients, and larger cohorts are required to explore the prognostic value of the parameters mentioned above.
| 1. | Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, Mittal RK, Rommel N, Savarino E, Sifrim D, Smout A, Vaezi MF, Zerbib F, Akiyama J, Bhatia S, Bor S, Carlson DA, Chen JW, Cisternas D, Cock C, Coss-Adame E, de Bortoli N, Defilippi C, Fass R, Ghoshal UC, Gonlachanvit S, Hani A, Hebbard GS, Wook Jung K, Katz P, Katzka DA, Khan A, Kohn GP, Lazarescu A, Lengliner J, Mittal SK, Omari T, Park MI, Penagini R, Pohl D, Richter JE, Serra J, Sweis R, Tack J, Tatum RP, Tutuian R, Vela MF, Wong RK, Wu JC, Xiao Y, Pandolfino JE. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021;33:e14058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 543] [Cited by in RCA: 704] [Article Influence: 140.8] [Reference Citation Analysis (1)] |
| 2. | Blais P, Bennett MC, Gyawali CP. Upper esophageal sphincter metrics on high-resolution manometry differentiate etiologies of esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2019;31:e13558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE; International Working Group for Disorders of Gastrointestinal Motility and Function. Expert consensus document: Advances in the management of oesophageal motility disorders in the era of high-resolution manometry: a focus on achalasia syndromes. Nat Rev Gastroenterol Hepatol. 2017;14:677-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Lynch KL, Yang YX, Metz DC, Falk GW. Clinical presentation and disease course of patients with esophagogastric junction outflow obstruction. Dis Esophagus. 2017;30:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Samo S, Qayed E. Esophagogastric junction outflow obstruction: Where are we now in diagnosis and management? World J Gastroenterol. 2019;25:411-417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (2)] |
| 6. | Rohof WOA, Bredenoord AJ. Chicago Classification of Esophageal Motility Disorders: Lessons Learned. Curr Gastroenterol Rep. 2017;19:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Triggs JR, Carlson DA, Beveridge C, Jain A, Tye MY, Kahrilas PJ, Pandolfino JE. Upright Integrated Relaxation Pressure Facilitates Characterization of Esophagogastric Junction Outflow Obstruction. Clin Gastroenterol Hepatol. 2019;17:2218-2226.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Gyawali CP, Carlson DA, Chen JW, Patel A, Wong RJ, Yadlapati RH. ACG Clinical Guidelines: Clinical Use of Esophageal Physiologic Testing. Am J Gastroenterol. 2020;115:1412-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 145] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 9. | Jehangir A, Tanner S, Malik Z, Parkman HP. Characterizing the proximal esophageal segment in patients with symptoms of esophageal dysmotility. Neurogastroenterol Motil. 2020;32:e13888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Jiao H, Mei L, Sharma T, Kern M, Sanvanson P, Shaker R. A human model of restricted upper esophageal sphincter opening and its pharyngeal and UES deglutitive pressure phenomena. Am J Physiol Gastrointest Liver Physiol. 2016;311:G84-G90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Peng L, Patel A, Kushnir V, Gyawali CP. Assessment of upper esophageal sphincter function on high-resolution manometry: identification of predictors of globus symptoms. J Clin Gastroenterol. 2015;49:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Biasutto D, Roman S, Garros A, Mion F. Esophageal shortening after rapid drink test during esophageal high-resolution manometry: A relevant finding? United European Gastroenterol J. 2018;6:1323-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Sanagapalli S, McGuire J, Leong RW, Patel K, Raeburn A, Abdul-Razakq H, Plumb A, Banks M, Haidry R, Lovat L, Sehgal V, Graham D, Sami SS, Sweis R. The Clinical Relevance of Manometric Esophagogastric Junction Outflow Obstruction Can Be Determined Using Rapid Drink Challenge and Solid Swallows. Am J Gastroenterol. 2021;116:280-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Chavez YH, Ciarleglio MM, Clarke JO, Nandwani M, Stein E, Roland BC. Upper esophageal sphincter abnormalities: frequent finding on high-resolution esophageal manometry and associated with poorer treatment response in achalasia. J Clin Gastroenterol. 2015;49:17-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Norton P, Herbella FAM, Schlottmann F, Patti MG. The upper esophageal sphincter in the high-resolution manometry era. Langenbecks Arch Surg. 2021;406:2611-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Woodland P, Gabieta-Sonmez S, Arguero J, Ooi J, Nakagawa K, Glasinovic E, Yazaki E, Sifrim D. 200 mL Rapid Drink Challenge During High-resolution Manometry Best Predicts Objective Esophagogastric Junction Obstruction and Correlates With Symptom Severity. J Neurogastroenterol Motil. 2018;24:410-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Patcharatrakul T, Alkaddour A, Pitisuttithum P, Jangsirikul S, Vega KJ, Clarke JO, Gonlachanvit S. How to approach esophagogastric junction outflow obstruction? Ann N Y Acad Sci. 2020;1481:210-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Shahsavari D, Malik Z, Parkman HP. Management of the patient with esophagogastric junction outflow obstruction. Curr Opin Gastroenterol. 2021;37:397-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Association of Digestive Disease, Chinese Geriatrics Society.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Herbella FAM, Brazil; Sweis R, United Kingdom S-Editor: Yan JP L-Editor: A P-Editor: Yan JP