Published online Nov 7, 2020. doi: 10.3748/wjg.v26.i41.6442
Peer-review started: August 3, 2020
First decision: August 22, 2020
Revised: September 5, 2020
Accepted: October 1, 2020
Article in press: October 1, 2020
Published online: November 7, 2020
Processing time: 94 Days and 19.7 Hours
Enema administration is a common procedure in the emergency department (ED). However, several published case reports on enema-related ischemic colitis (IC) have raised the concerns regarding the safety of enema agents. Nevertheless, information on its true incidence and characteristics are still lacking.
To investigate the incidence, timing, and risk factors of IC in patients receiving enema.
We consecutively collected the data of all adult patients receiving various enema administrations in the ED from January 2010 to December 2018 and identified patients confirmed with IC following enema. Of 8320 patients receiving glycerin enema, 19 diagnosed of IC were compared with an age-matched control group without IC.
The incidence of IC was 0.23% among 8320 patients receiving glycerin enema; however, there was no occurrence of IC among those who used other enema agents. The mean age ± standard deviation (SD) of patients with glycerin enema-related IC was 70.2 ± 11.7. The mean time interval ± SD from glycerin enema administration to IC occurrence was 5.5 h ± 3.9 h (range 1-15 h). Of the 19 glycerin enema-related IC cases, 15 (79.0%) were diagnosed within 8 h. The independent risk factors for glycerin-related IC were the constipation score [Odds ratio (OR), 2.0; 95% confidence interval (CI): 1.1-3.5, P = 0.017] and leukocytosis (OR, 4.5; 95%CI: 1.4-14.7, P = 0.012).
The incidence of glycerin enema-related IC was 0.23% and occurred mostly in the elderly in the early period following enema administration. Glycerin enema-related IC was associated with the constipation score and leukocytosis.
Core Tip: Enema is a very safe and common procedure in the emergency department (ED). However, clinical information regarding ischemic colitis (IC) following enema is lacking. Our data shows that the incidence of IC was 0.23 % and occurred mostly in the elderly in the early period after administration of glycerin enema only. Despite the rarity of this disease, it can become relatively severe, resulting in the need for surgical resection. The independent predictive factors of glycerin enema-related IC were constipation scores and leukocytosis. Our data could provide useful information for the triage of patients necessitating observation after glycerin enema in the ED.
- Citation: Ahn Y, Hong GS, Lee JH, Lee CW, Kim SO. Ischemic colitis after enema administration: Incidence, timing, and clinical features. World J Gastroenterol 2020; 26(41): 6442-6454
- URL: https://www.wjgnet.com/1007-9327/full/v26/i41/6442.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i41.6442
Enema administration is a procedure used to stimulate stool evacuation and is generally considered to be safe[1]. It is most commonly performed to relieve severe constipation[2,3]. In addition, it is also used for the treatment of hyperkalemia and hepatic encephalopathy. Enemas function through several different mechanisms. All cleansing enemas induce rectal distension and subsequently stimulate colon contraction and stool elimination[2]. Other enemas such as phosphate enema function by direct stimulation of the muscles of the colon. There are several enema agents: Phosphate, saline, tap water, glycerin, and a synthetic sugar for the cleaning of the colon; and Kalimate for the treatment of hyperkalemia. The elderly are five times more prone to constipation because of the effect of medication, immobility, and a blunted urge to defecate[4]. Many patients usually give themselves enemas at home owing to the availability of over-the-counter medications. However, some patients need urgent care and are referred to the emergency department (ED) for the aforementioned medical conditions. The number of patients referred to the ED for enema administration has increased over time[5]. Given the surge in the elderly population, the number of patients requiring this urgent care in hospitals is expected to rise.
Adverse events after enema administration are rarely reported in the literatures but may cause critical conditions in patients. Enema-related complications include bowel perforation, ischemic colitis (IC), malignant hyperthermia, and colonic mural hematoma[6-10]. In general, IC is known to be transitional or self-limited, but sometimes requires surgical intervention or leads to death especially in the postoperative period[11]. The existence of a relationship between IC and enema administration has been suggested in the literature. Several case reports have reported IC following enema administration for the treatment of constipation, preoperative bowel cleansing and the correction of hyperkalemia[12-15]. Therefore, in some studies, enema administration has been considered to be a risk factor for the development of IC[16,17]. However, despite the popularity of this procedure, there have been no studies to systemically investigate enema-related IC.
The present study aimed to investigate the incidence, timing and risk factors of IC in patients receiving enema.
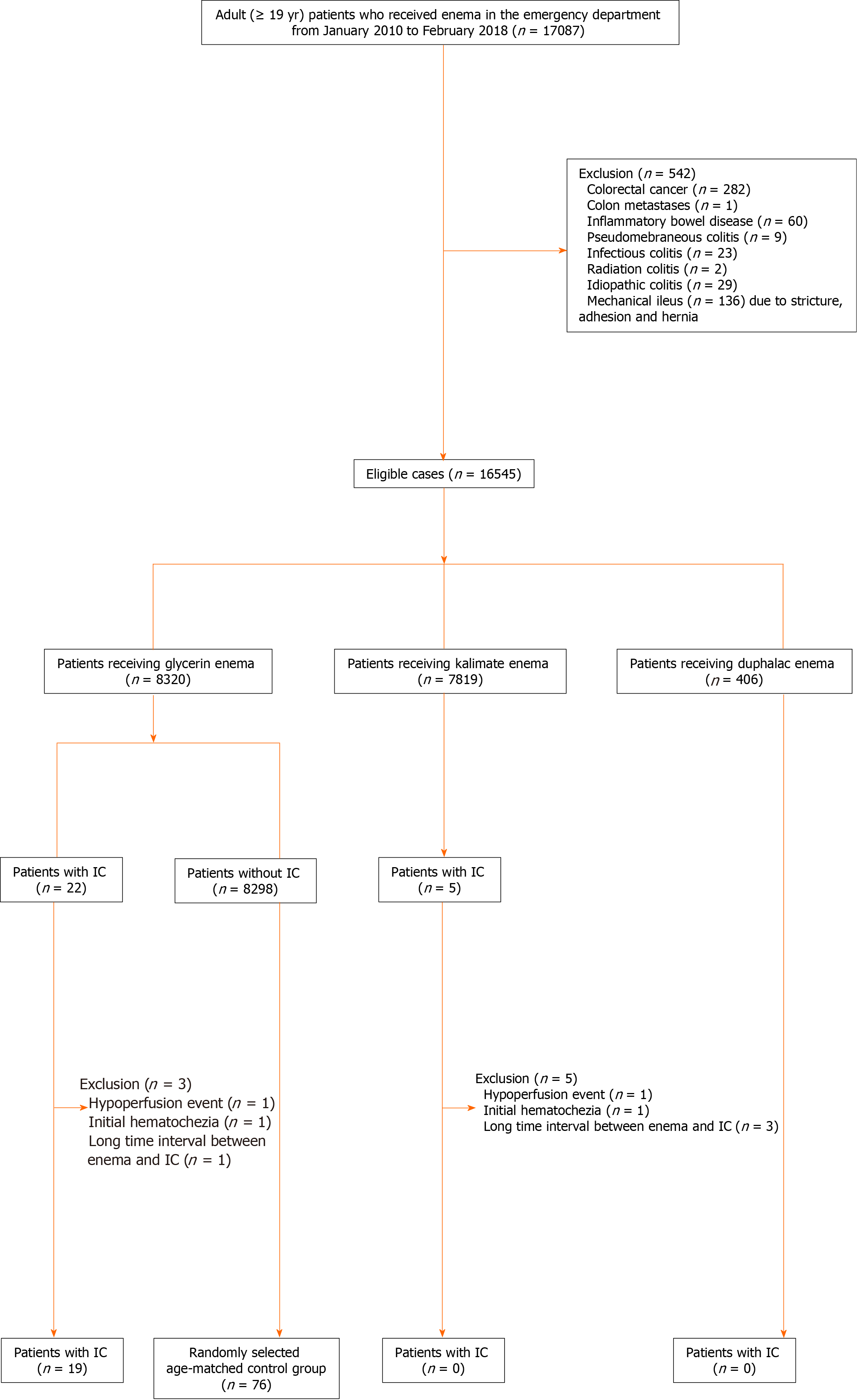
In this retrospective study, we analyzed the data of adult patients with confirmed IC after enema administration in the ED between January 2010 and February 2018. The inclusion criteria were as follows: (1) Adults aged > 19 years; and (2) Patients with confirmed IC after enema administration but without suspected IC symptoms and clinical examination results (e.g., hematochezia, sudden drop in blood pressure, abdominal tenderness, and guarding) before enema. The exclusion criteria were as follows: (1) Patients with unspecific vascular hypoperfusion or its similar condition (e.g., cardiac failure, septic shock, hemodynamic shock, hemodialysis, and aortic surgery), colonic obstruction (volvulus, adhesion, stricture, hernia, colon cancer, or metastasis), vascular occlusion (based on the findings of follow-up CTs performed after enema), and infectious or inflammatory bowel disease (e.g., inflammatory bowel disease, radiation colitis, and infectious colitis); and (2) Time interval from enema administration to IC occurrence of > 24 h based on the prior case reports[13-15]. Among 17087 adult patients receiving enema in the ED, 542 patients were excluded due to infectious or inflammatory bowel disease (n = 123), colonic malignancy (n = 283), and mechanical ileus (n = 136). The remnant patients received one of three types of enema agents: 8320 received glycerin enema (150 g of glycerin in 150 mL of purified water); 7819 received Kalimate enema (calcium polystyrene sulfonate; 30 g of Kalimate in 200 mL of purified water); and 406 received Duphalac enema [300 mL of lactulose solution (composition: 3.335 g lactulose/5 mL)]. After excluding patients with predisposing events, hematochezia, or long-time interval, 19 patients in the glycerin enema group were finally included. For a case-control study with a case to control ratio of 1:4, an age-matched control group was randomly selected from patients receiving glycerin enema. Figure 1 shows the flow diagram of the study population.
The clinical data included age, sex, age-adjusted Charlson comorbidity index (ACCI) score, constipation score, medication, enema agents, time of enema administration, initial symptoms, initial vital signs, and laboratory findings [C-reactive protein (CRP) and white blood cell count (WBC)] at the time before enema administration. The ACCI score was calculated using the algorithm proposed by Charlson et al[18], in which 19 comorbid conditions were weighted and scored and additional points were added for age. The constipation score was calculated using modified simple criteria based on the Wexner constipation scoring system[19]. Four conditions of these criteria were: History of chronic constipation; recurrent usage of defecation assistance; last defecation ≥ 5 d prior to admission to the ED; unsuccessful evacuation attempts using enema within 24 h. Each condition was scored on a two-point scale (0-1). IC-related medications were classified into two groups — drugs with a moderate evidence level and those with a low evidence level — according to the drugs reported to predispose patients to IC in a previous report[20]. The clinical data on the post-enema administration duration included symptom change, time of a change in symptom or vital signs, diagnostic method, treatment method, and treatment outcome. The radiologic and endoscopic reports were also recorded. In patients diagnosed with IC, bowel preparation was not performed before colonoscopy because of the risk of perforation or toxic dilation. The time of IC occurrence was defined as the time between enema and a change in symptoms and/or vital signs requiring further examination or treatment in the presence of suspicions of IC.
All analytic images were available on a picture archiving and communications system (PACS). Plain abdominal radiographs were routinely performed in all patients before enema administration in the ED. Of the 19 patients diagnosed with IC following glycerin enema administration, 18 received contrast-enhanced abdominopelvic computed tomography (AP-CT) and one underwent non-contrast enhanced AP-CT. All AP-CT images were acquired using a multidetector CT scanner (Somatom Sensation 16 CT scanners, Siemens Healthcare, Erlangen, Germany) with or without intravenous contrast material (Ultravist 300 or Ultravist 370; Bayer Schering Pharma, Berlin, Germany). AP-CT consisted of a portal phase image with a fixed 60-70 S delay following the injection of intravenous contrast media.
All radiologic images were reviewed by two radiologists (Hong GS and Ahn Y with > 13 years and 4 years of experience in abdominal imaging, respectively) in consensus. Plain abdominal radiographs were reviewed for abnormal gas or abnormal bowel gas patterns except for constipation. The following selected imaging features were reviewed on AP-CT images: Segmental bowel wall thickening [location, bowel wall thickening thickness (one-side wall thickness), wall thickening pattern (circumferential/eccentric), and skip area], decreased bowel wall enhancement [involving layer (no involvement, inner layer, and transmural), target sign, and skip area], mesenteric manifestation (pericolic fluid or fat stranding and peritoneal free fluid or mesenteric edema), pneumatosis coli, portal and/or drain venous gas, pneumoperitoneum, and vascular occlusion.
All variables were tested for normal distribution using the Kolmogorov-Smirnov test. Comparisons between the case and control groups were performed using the chi square test or Fisher’s exact test for categorical variables and the Student’s t-test or the Mann-Whitney U-test for continuous variables. Conditional logistic regression was used to identify risk factors associated with IC. Multivariate logistic regression analysis was performed using backward elimination. Statistical significance was considered when a probability value (P value) was less than 0.05. For all statistical analysis, a commercial software (SPSS, version 23; SPSS, Chicago, IL, United States; and SAS version 9.4; SAS Institute; Cary, NC, United States) was used.
Table 1 shows the incidence of IC following enema administration according to the enema agent used. The incidence of edema-related IC was very low; 0.23 % (19/8320) in the glycerin enema group, but there was no occurrence of IC with the usage of the other enema agents. Major adverse events occurred in 52.6% (10/19) of the patients with glycerin enema-related IC: 47.4% (9/19) requiring surgical resections and 21.1% (4/19) resulting in in-hospital mortality.
| Glycerin | Kalimate | Duphalac | Total | |
| Total number of enemas | 8320 (50.3) | 7819 (47.3) | 406 (2.5) | 16545 |
| Number of IC | 19 (0.23) | 0 (0.0) | 0 (0.0) | 19 (0.11) |
| Major adverse event | 10 (52.6) | N/A | N/A | 10 |
| Surgical resection | 9 (47.4) | N/A | N/A | 9 |
| In-hospital mortality | 4 (21.1) | N/A | N/A | 4 |
The demographic and clinical characteristics of the study population were similar between the two groups with or without glycerin enema-related IC (Table 2). Of note, most patients diagnosed with glycerin-related IC were elderly [mean age ± standard deviation (SD), 70.2 ± 11.7 years]. The main initial symptom of the IC group was abdominal pain [57.9%, (11/19)], followed by constipation [15.8%, (3/19)]. There was no significant difference between the IC and non-IC groups in terms of initial vital signs, symptoms, ACCI, and medication. The review of plain abdominal radiographs showed no significant difference between the IC and non-IC groups. There was a statistically significant difference in the constipation score and WBC count between the two groups. Of the 19 patients diagnosed with glycerin-related IC, 8 (42.1%) had a history of chronic constipation, 3 (15.8%) recurrently used defecation assistance, 4 (21.1%) lastly defecated ≥ 5 d prior to admission to the ED, and 6 (31.6%) had a history of evacuation failure using enema within 24 h. In the 19 patients diagnosed with IC, the mean ± standard deviation of WBC count was 13.4 ± 7.5 × 103/μL before enema administration. Of these patients, 16 had available records of their WBC counts immediately after enema. The WBC count (11.6 ± 6.9 × 103/μL) after enema was slightly decreased as compared with that before enema. After the administration of enema, patients with IC mainly presented hematochezia [57.9%, (11/19)], followed by abdominal pain [26.3%, (5/19)] and a sudden drop in blood pressure [15.8%, (3/19)]. The most common diagnostic tool in the emergency department for patients with IC was CT scan [100%, (19/19)] followed by colonoscopy [73.7%, (14/19)]. Less than half the patients with IC received surgical resection [47.4%, (9/19)].
| Number | IC group (n = 19) | Control (n = 76) | P value |
| Age | 70.2 ± 11.7 | 70.2 ± 11.5 | 0.996 |
| Sex, male | 8 (42.1%) | 32 (42.1%) | 1.000 |
| Initial vital sign | |||
| Systolic blood pressure (mmHg, mean ± SD) | 138.5 ± 34.4 | 135.8 ± 27.3 | 0.716 |
| Diastolic blood pressure (mmHg, mean ± SD) | 83.6 ± 22.1 | 81.7 ± 16.0 | 0.678 |
| Pulse rate | 85.8 ± 22.9 | 84.0 ± 19.4 | 0.727 |
| Respiratory rate | 20.6 ± 2.1 | 19.9 ± 2.3 | 0.146 |
| Initial symptom | 0.847 | ||
| Abdominal pain | 11 (57.9) | 47 (61.8) | |
| Constipation | 3 (15.8) | 7 (9.2) | |
| Vomiting | 2 (10.5) | 9 (11.8) | |
| Miscellaneous symptom | 3 (15.8) | 13 (17.1) | |
| Constipation score1 (mean ± SD) | 1.1 ± 1.2 | 0.5 ± 0.8 | 0.022 |
| Condition | |||
| History of chronic constipation | 8 (42.1) | 17 (22.4) | |
| Recurrent usage of enema agent | 3 (15.8) | 7 (9.2) | |
| Last defection more than 5 d | 4 (21.1) | 10 (13.2) | |
| Failure: Unsuccessful attempts for evacuation before admitting ED | 6 (31.6) | 3 (4.0) | |
| ACCI score | |||
| mean ± SD | 5.8 ± 3.1 | 4.9 ± 2.3 | 0.245 |
| Condition | |||
| Myocardial infarction | 2 | 2 | |
| Congestive heart failure | 3 | 1 | |
| Peripheral vascular disease | 1 | 2 | |
| Cerebral vascular disease | 3 | 7 | |
| Dementia | 2 | 2 | |
| Chronic pulmonary disease | 0 | 1 | |
| Connective tissue disease | 0 | 1 | |
| Peptic ulcer | 2 | 4 | |
| Mild liver disease | 1 | 1 | |
| Hemiplegia | 0 | 1 | |
| Diabetes | 6 | 15 | |
| Moderate or severe renal disease | 3 | 5 | |
| Diabetes with end-organ damage | 1 | 3 | |
| Solid tumor | 5 | 25 | |
| Leukemia | 2 | 1 | |
| Lymphoma | 0 | 2 | |
| Moderate or severe liver disease | 1 | 2 | |
| Metastatic solid tumor | 3 | 11 | |
| AIDS | 0 | 0 | |
| Drug proposed to predispose to IC | |||
| Total No. of patients (moderate + low) | 13 | 57 | 0.560 |
| No. of patients taking drugs with moderate evidence | 7 | 39 | 0.259 |
| Constipation-inducing drugs | 7 | 39 | |
| No. of patients taking drugs with low evidence | 6 | 18 | 0.479 |
| Antibiotics | 4 | 12 | |
| Chemotherapeutic drugs | 2 | 2 | |
| Decongestants | 0 | 1 | |
| Diuretics | 1 | 3 | |
| Laxative | 3 | 7 | |
| Psychotropic drugs | 0 | 6 | |
| Initial Laboratory test | |||
| CRP (mg/dL) | 5.9 ± 1.0 | 1.4 ± 2.8 | 0.429 |
| WBC (× 103/μL) | 13.4 ± 7.5 | 8.4 ± 3.4 | 0.004 |
| Plain abdominal radiograph | |||
| Abnormal findings | 5 (26.3) | 9 (11.8) | 0.146 |
| New symptom after enema | |||
| Hematochezia | 11 (57.9) | 0 | |
| Abdominal pain | 5 (26.3) | 0 | N/A |
| Sudden drop in blood pressure | 3 (15.8) | 0 | |
| Asymptomatic | 0 (0.0) | 76 (100.0) | |
| Diagnostic tools | N/A | ||
| Non contrast-enhanced AP-CT | 1 (5.3) | NA | |
| Contrast-enhanced AP-CT | 18 (94.7) | NA | |
| Colonoscopy | 14 (73.7) | NA | |
| Treatment | N/A | ||
| Supported care | 10 (52.6) | NA | |
| Surgical resection | 9 (47.4) | NA |
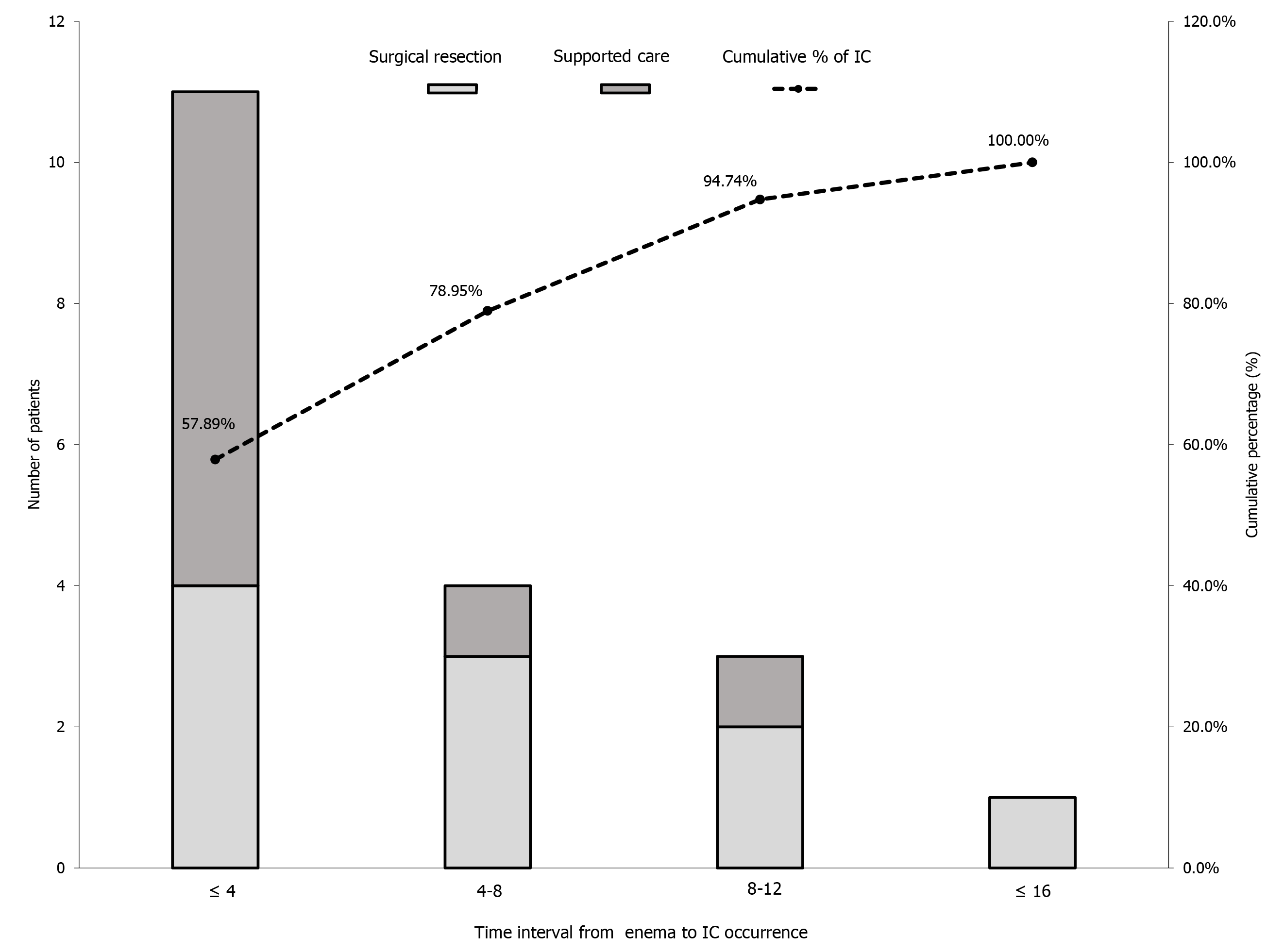
Figure 2 shows the time interval between enema administration and IC occurrence. Mean time interval ± SD from glycerin enema administration to IC occurrence was 5.5 h ± 3.9 h (range: 1-15 h). Of the 19 patients, 15 (79.0%) developed IC within 8 h of glycerin enema administration. Of the 11 patients in whom IC occurred within 4 h of glycerin enema administration, 7 (63.6%) underwent surgical resection, whereas of the 8 patients who experienced IC after 4 h, 2 (25%) underwent surgical resection.
In the conditional logistic regression analysis, the risk factors for the glycerin-related IC were the constipation score [Odds ratio (OR), 2.0; 95% confidence interval (CI): 1.1-3.5, P = 0.017], and leukocytosis (OR, 4.5; 95%CI: 1.4-14.7, P = 0.012) (Table 3).
| Univariate analysis | Multivariate analysis | |||
| Odds ratio (95%CI) | P value | Odds ratio (95%CI) | P value | |
| Constipation score1 | 1.9 (1.1-3.3) | 0.015 | 2.0 (1.1-3.5) | 0.017 |
| ACCI score | 1.2 (0.9-1.4) | 0.144 | ||
| Leukocytosis | 4.4 (1.4-13.5) | 0.009 | 4.5 (1.4-14.7) | 0.012 |
| CRP | 2.2 (0.8-6.1) | 0.151 | ||
| Abnormal abdominal radiograph | 2.5 (0.8-8.6) | 0.132 | ||
| Drug proposed to predispose to IC | 1.9 (0.6-5.7) | 0.260 | ||
Table 4 shows the radiologic features on CT in patients. Among the 19 patients diagnosed with glycerin enema-related IC, 18 patients received contrast-enhanced CT scans and one patient was examined with a non-contrast CT scan. In all patients, CT imaging revealed a circumferential wall thickening of the colon. In most cases, colonic wall thickening was continuous except for three cases with a skip area. The colonic wall thickening was located mainly in the rectosigmoid colon [94.7%, (18/19)], followed by the descending colon [52.6%, (10/19)]. In two patients, colonic wall thickening extended to the ascending colon. Among the 18 contrast-enhanced CT images, a decreased wall enhancement was noted in 10 (55.6%) patients (inner layer, n = 3; transmural, n = 7), but not in 8 patients. Of these, 7 (70.0%) patients showed a skip area of the decreased wall enhancement. Pneumatosis colic and portal venous gas were detected in one [5.3%, (1/19)] patient and pneumoperitoneum in one [5.3%, (1/19)] patient. Regardless of the numerous features of IC, vascular occlusion was not noted in contrast-enhanced CT. Of note, misinterpretation occurred in 7 (36.8%) of 19 patients: These diagnoses consisted of stercoral colitis, infectious colitis, and pseudo-obstruction.
| CE-CT (n = 18) | NCE-CT (n = 1) | |
| Segmental wall thickening | n = 18 | n = 1 |
| Location (Rectum/sigmoid/descending/transverse/ascending colon) | 16/17/10/7/2 | 1/1/0/0/0 |
| Wall thickening thickness (mm), mean ± SD | 9.57 ± 2.39 | 5.6 |
| Wall thickening pattern (circumferential/eccentric) | 18/0 | 1/0 |
| Skip area | 3 | 0 |
| Decreased wall enhancement | n = 10 | N/A |
| Involving layer (no/inner layer/transmural) | 8/3/7 | |
| Target sign | 15 | |
| Skip area | 7 | |
| Pericolic stranding or fluid | 9 | 1 |
| Peritoneal free fluid or mesenteric edema | 2 | 0 |
| Pneumatosis coli | 1 | 0 |
| Portal or drain venous gas | 1 | 0 |
| Pneumoperitoneum | 1 | 0 |
| Vascular occlusion | 0 | N/A |
To best our knowledge, there has been no study on a systemic approach of enema-related IC. Our data suggest a necessity for observation in the early period after enema administration in the elderly with glycerin enema based on the constipation scores and initial laboratory findings.
The present study is the first to investigate the incidence of IC according to enema agent. We showed that the incidence [0.23%, (19/8320)] of glycerin enema-related IC was very low. Niv et al[21] reported that colon perforation after cleansing enema occurred in 1.4% of patients with acute constipation in the ED. However, this is mainly due to the inappropriate positioning of the device tip, even though it might be associated with a localized weakness of the rectal wall. It is known that non-occlusive IC is typically transient, although transmural necrosis can be induced by prolonged non-occlusive ischemia. Approximately 15% of patients with IC progress to gangrenous colitis, resulting in life-threatening conditions[22]. However, in the present study, nearly half of patients with glycerin-related IC received surgical resection for transmural necrosis, and four patients died during hospitalization. This is a higher rate than that reported previously. The higher surgical rate obtained in the present study could be caused by the severe symptoms. However, in all the cases examined, surgical resection was determined not only based on the symptoms but also according to the disease severity assessed by CT and/or colonoscopy findings. In addition, as aforementioned, all the patients who underwent surgical resection were histologically confirmed to have transmural necrosis. Therefore, our data may imply that glycerin enema leads to a relatively severe IC, resulting in a progression to gangrenous colitis. In the present study, we could not define the relationship between Kalimate enema and IC occurrence although all the cases proposed here had crystals with a characteristic crystalline mosaic pattern on the mucosa and ulcer bed tissue similar to those of previous reports. This may be because the cases proposed here had a medication history of repeated use of Kalimate enema solution or oral Kalimate. In addition, IC occurred at a relatively longer time after the last administration of Kalimate. Therefore, it is difficult to definitely indicate its association with IC occurrence, and further studies are warranted.
The eligibility criteria proposed here were based on the clinical conditions (symptoms, signs, and possible etiologies of IC), and not on CT or endoscopy findings. It is mainly because aggressive workup (i.e., CT and colonoscopy) is not usually performed, unless an underlying disease is suspected in patients requiring enema for constipation in the ED. Therefore, existing IC before enema could be overlooked because self-limited or transient IC can often present with vague abdominal symptoms. However, although self-limited or transient IC caused by constipation exists before enema, it is plausible that glycerin enema triggers or aggravates mild IC, considering the high proportion of transmural necrosis in the present study.
Although glycerin enema-related IC rarely occurs, its timing is a notable consideration. Prior studies demonstrated that increased length of stay at the ED contributes to ED crowding[23]. ED crowding is associated with adverse patient outcomes, including increased mortality[24,25]. Therefore, determining the optimal observation time for this patient group in the ED is important, considering that glycerin enema-related IC is a lethal complication despite its rarity. In the present study, IC occurred in 15 (79.0%) of 19 patients within 8 h of glycerin enema administration. Notably, surgical resection was performed in 7 (63.6%) of 11 patients in whom IC occurred in ≤ 4 h. Based on previous case reports, the time interval between cleansing enema and IC occurrence ranged from 30 min to 6 h. Chang et al[13] reported a case wherein IC and hematochezia developed 6 h after glycerin enema for preoperative bowel cleansing for coronary bypass surgery . Park et al[14] reported a case of IC that occurred within 2 h of normal saline enema for preoperative bowel cleansing. Most recently, Yoon et al[15] reported a case of IC that presented abdominal pain and hematochezia within 30 min of enema administration. Our data suggest that it may be necessary to observe patients receiving glycerin enema in the early period after administration (at least 4 to 8 h), considering timing of IC and high surgical resection rates.
In the current study, it is worth noting that the constipation score was one of the significant independent predictive factors of IC among patients receiving glycerin enema at the ED. We used a modified constipation scoring system to obtain an objective definition of constipation. Prior studies demonstrated that constipation may be one of the predisposing factors for IC[26-30]. The reasonable mechanism for this was advanced by Anon et al[31]: The increased colonic luminal pressure could cause poorer blood flow in the colonic wall. Therefore, in this setting, edema could aggravate the increased intraluminal pressure and cause vascular spasm due to the lower temperature of the enema fluid than the body temperature, resulting in a reduced mucosal circulation. In our study, we also identified leukocytosis as another predisposing factor for glycerin enema-related IC, as shown in other studies on the risk factors of IC[30,32]. Leukocytosis is a common sign of infection, but not a definitive marker of significant infection. Reactive leukocytosis can occur because of various etiologies, including constipation. Obokhare[33] showed that constipation and fecal impaction can mildly elevate the WBC count. In the present study, the WBC count after enema was slightly lower than that before enema. In addition, none of the patients showed any signs and symptoms of infection. Therefore, leukocytosis may be associated with chronic constipation. According to a prior study, leukocytosis may imply the presence of transient IC in patients with chronic constipation. In conclusion, leukocytosis is not a specific clinical marker of IC but may be associated with chronic constipation or transient IC. Regardless of its cause, in older patients with leukocytosis and chronic constipation, glycerin enema may trigger or induce a relatively severe ischemic colitis. However, in clinical practice, these conditions (i.e., high constipation score and leukocytosis) predisposing to IC are commonly seen in the elderly. They might have little discriminatory power in the elderly, although we conducted our study with an age-matched control group to identify the best predisposing factors. Nevertheless, our study showed the possibility of constipation conditions and initial laboratory findings being of great importance in portending IC after glycerin enema administration.
CT plays an important role in the assessment and triage of patients with IC in the acute phase[34]: Defining the injured colonic segment, suggesting irreversibility of bowel necrosis, detecting the complication, and excluding non-ischemic causes. However, our study identified diagnostic difficulties and errors on CT in diagnosing glycerin enema-related IC, which was 36.8% of the IC group. In the current study, contrast-enhanced CT did not show a decreased enhancement of the colonic wall in 44.4% of the IC group. This may reflect an early episode of IC, making it difficult to distinguish IC from non-ischemic colitis. However, the imaging findings and regional distribution of glycerin enema-related IC in our study were not significantly different from those in the published literature on non-occlusive IC[32,35]. Therefore, this may be due to a lack of knowledge and awareness regarding the acute clinical setting (i.e., IC) occurring in the elderly following glycerin-enema administration. Therefore, in this setting, the interpretation of CT findings may require more attention, although the misdiagnosis may not be of clinical relevance due to the full consideration of all the available evidence in diagnosing IC.
Our study has some limitations. First, the retrospective nature of the study may cause a selection bias in the data analysis. Second, the small number of study patients may lead to a lack of statistical power in our results. However, the rarity of the disease entity investigated here can offset these weaknesses of our study. Third, our study was conducted based on a single center experience. Therefore, the general application of our results may not be appropriate. Fourth, the clinical information regarding IC-related medications and medical history may not be sufficient, although the clinical information is not as comprehensive for patients hospitalized in the ED. Fifth, the incidence of enema-related IC can be underestimated because the current study may have consisted of patients with high suspicion of IC. A previous study showed that this condition was initially suspected in only 25% of patients[36]. The diagnosis of IC depends on the severity of the presentation. Patients with transient IC may be asymptomatic after enema administration. Moreover, the initial presentation of IC is nonspecific. As a result, there could be a number of cases that were lost to follow-up in our study. Finally, as previously mentioned, we did not clarify whether the crystal deposition of Kalimate in the colon induces IC or not. To resolve this issue, it is essential to investigate the presence or absence and the amount of crystal deposition in the non-IC group receiving Kalimate enema, although they do not receive endoscopic biopsy in the colon unless acute abdominal symptoms exist. Therefore, this is an inevitable limitation in a retrospective observational study.
In conclusion, glycerin enema-related IC occurred in 0.23% of the patients, occurring mostly in the elderly in the early period following enema administration. Despite the rarity of this disease entity, it can lead to a relatively severe IC, resulting in the need for surgical resection. Glycerin enema-related IC was associated with the constipation score, and leukocytosis. These data could provide useful clues for the triage of patients necessitating observation after glycerin enema in the ED.
Many patients usually give themselves enema at home due to over-the-counter medications. However, the number of patients referred to the emergency department for enema has increased over time. Enema administration is one of the most common procedures in the emergency department.
Several published case reports of enema-related ischemic colitis (IC) have raised concerns regarding the safety of enema agents. However, information on its true incidence and characteristics are still lacking. There have been no studies that systemically investigate enema-related IC.
Our purpose is to investigate the incidence, timing and risk factors of IC in patients receiving enema.
We analyzed data from the database of patients with IC after enema administration at the Emergency Department of the Asan Medical Center from 2010 to 2018. The symptoms, laboratory findings, age-adjusted Charlson comorbidity index score, constipation score, medication, time interval from enema administration to occurrence of IC, treatment, and treatment outcome were analyzed.
The incidence of IC was 0.23%, and it occurred mostly in elderly patients in the early period following glycerin enema administration but not after the use of other enema agents. The constipation score and leukocytosis were independent risk factors for glycerin-related IC.
We found out that glycerin-related IC is very rare, but mainly occurs in the elderly in the early post-enema period. The constipation score and leukocytosis could help in prediction of an IC following glycerin enema.
This could provide useful information for the triage of patients necessitating observation after glycerin enema administration in the emergency department.
| 1. | Portalatin M, Winstead N. Medical management of constipation. Clin Colon Rectal Surg. 2012;25:12-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Shin JE, Jung HK, Lee TH, Jo Y, Lee H, Song KH, Hong SN, Lim HC, Lee SJ, Chung SS, Lee JS, Rhee PL, Lee KJ, Choi SC, Shin ES; Clinical Management Guideline Group under the Korean Society of Neurogastroenterology and Motility. Guidelines for the Diagnosis and Treatment of Chronic Functional Constipation in Korea, 2015 Revised Edition. J Neurogastroenterol Motil. 2016;22:383-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Sun SX, Dibonaventura M, Purayidathil FW, Wagner JS, Dabbous O, Mody R. Impact of chronic constipation on health-related quality of life, work productivity, and healthcare resource use: an analysis of the National Health and Wellness Survey. Dig Dis Sci. 2011;56:2688-2695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 146] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 4. | Bouras EP, Tangalos EG. Chronic constipation in the elderly. Gastroenterol Clin North Am. 2009;38:463-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Sommers T, Corban C, Sengupta N, Jones M, Cheng V, Bollom A, Nurko S, Kelley J, Lembo A. Emergency department burden of constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Mori H, Kobara H, Fujihara S, Nishiyama N, Kobayashi M, Masaki T, Izuishi K, Suzuki Y. Rectal perforations and fistulae secondary to a glycerin enema: closure by over-the-scope-clip. World J Gastroenterol. 2012;18:3177-3180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Tanswell IJ, Irfan K, Kossakowski T, Townson G. Rectal perforation in ulcerative colitis: complication of an enema tip. Gastrointest Endosc. 2009;69:344; discussion 344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Maeda E, Mori Y, Amano E, Akamatsu T, Okada T. [A case of the complications following glycerin enema which suggested malignant hyperthermia]. Masui. 2010;59:914-917. [PubMed] |
| 9. | Rentea RM, Fehring CH. Rectal colonic mural hematoma following enema for constipation while on therapeutic anticoagulation. J Surg Case Rep. 2017;2017:rjx001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Joo M, Bae WK, Kim NH, Han SR. Colonic mucosal necrosis following administration of calcium polystryrene sulfonate (Kalimate) in a uremic patient. J Korean Med Sci. 2009;24:1207-1211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Antolovic D, Koch M, Hinz U, Schöttler D, Schmidt T, Heger U, Schmidt J, Büchler MW, Weitz J. Ischemic colitis: analysis of risk factors for postoperative mortality. Langenbecks Arch Surg. 2008;393:507-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Berenguer J, Cabades F, Gras MD, Pertejo V, Rayon M, Sala T. Ischemic colitis attributable to a cleansing enema. Hepatogastroenterology. 1981;28:173-175. [PubMed] |
| 13. | Chang RY, Tsai CH, Chou YS, Wu TC. Nonocclusive ischemic colitis following glycerin enema in a patient with coronary artery disease. A case report. Angiology. 1995;46:747-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Park JE, Moon W, Nam JH, Kim NH, Kim SH, Park MI, Park SJ, Kim KJ. [A case of ischemic colitis presenting as bloody diarrhea after normal saline enema]. Korean J Gastroenterol. 2007;50:126-130. [PubMed] |
| 15. | Yoon JM, Kim SH, Lee JS, Kim MJ, Jang SW, Kim YJ, Jeon TY. A Case of Ischemic Colitis Presenting as Bloody Diarrhea after Glycerin Enema. Int Res. 2013;11:52-55. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Seo HI, Choi KH, Han KH, Lee SJ, Park JK, Kim YD, Cheon GJ. Predisposing Factors of Ischemic Colitis: Data from 14 Years of Experience in a Single Center. Gastroenterol Res Pract. 2017;2017:1049810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Mohanapriya T, Singh KB, Arulappan T, Shobhana R. Ischemic colitis. Indian J Surg. 2012;74:396-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 39557] [Article Influence: 1014.3] [Reference Citation Analysis (0)] |
| 19. | Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996;39:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 818] [Cited by in RCA: 875] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 20. | Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ; American College of Gastroenterology. ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 2015;110:18-44; quiz 45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 207] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 21. | Niv G, Grinberg T, Dickman R, Wasserberg N, Niv Y. Perforation and mortality after cleansing enema for acute constipation are not rare but are preventable. Int J Gen Med. 2013;6:323-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Greenwald DA, Brandt LJ. Colonic ischemia. J Clin Gastroenterol. 1998;27:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Driesen BEJM, van Riet BHG, Verkerk L, Bonjer HJ, Merten H, Nanayakkara PWB. Long length of stay at the emergency department is mostly caused by organisational factors outside the influence of the emergency department: A root cause analysis. PLoS One. 2018;13:e0202751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, McCarthy M, John McConnell K, Pines JM, Rathlev N, Schafermeyer R, Zwemer F, Schull M, Asplin BR; Society for Academic Emergency Medicine, Emergency Department Crowding Task Force. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 725] [Cited by in RCA: 787] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 25. | Jo S, Jeong T, Jin YH, Lee JB, Yoon J, Park B. ED crowding is associated with inpatient mortality among critically ill patients admitted via the ED: post hoc analysis from a retrospective study. Am J Emerg Med. 2015;33:1725-1731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 26. | Tohda G, Higashi S, Sumiyoshi KI, Sakumoto H, Kato C, Kane T. Evaluation of clinical features of ischemic colitis: comparison between young and elderly. Digest Endosc. 2005;17:123-130. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Matsumoto S, Tsuji K, Shirahama S. Clinical investigation of 41 patients with ischemic colitis accompanied by ulcer. World J Gastroenterol. 2007;13:1236-1239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Suh DC, Kahler KH, Choi IS, Shin H, Kralstein J, Shetzline M. Patients with irritable bowel syndrome or constipation have an increased risk for ischaemic colitis. Aliment Pharmacol Ther. 2007;25:681-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Cubiella Fernández J, Núñez Calvo L, González Vázquez E, García García MJ, Alves Pérez MT, Martínez Silva I, Fernández Seara J. Risk factors associated with the development of ischemic colitis. World J Gastroenterol. 2010;16:4564-4569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 30. | Mosele M, Cardin F, Inelmen EM, Coin A, Perissinotto E, Sergi G, Terranova O, Manzato E. Ischemic colitis in the elderly: predictors of the disease and prognostic factors to negative outcome. Scand J Gastroenterol. 2010;45:428-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Añón R, Boscá MM, Sanchiz V, Tosca J, Almela P, Amorós C, Benages A. Factors predicting poor prognosis in ischemic colitis. World J Gastroenterol. 2006;12:4875-4878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 32. | Tadros M, Majumder S, Birk JW. A review of ischemic colitis: is our clinical recognition and management adequate? Expert Rev Gastroenterol Hepatol. 2013;7:605-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Obokhare I. Fecal impaction: a cause for concern? Clin Colon Rectal Surg. 2012;25:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Wiesner W, Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology. 2003;226:635-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 250] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 35. | Riley LK, Rupert J. Evaluation of Patients with Leukocytosis. Am Fam Physician. 2015;92:1004-1011. [PubMed] |
| 36. | Montoro MA, Brandt LJ, Santolaria S, Gomollon F, Sánchez Puértolas B, Vera J, Bujanda L, Cosme A, Cabriada JL, Durán M, Mata L, Santamaría A, Ceña G, Blas JM, Ponce J, Ponce M, Rodrigo L, Ortiz J, Muñoz C, Arozena G, Ginard D, López-Serrano A, Castro M, Sans M, Campo R, Casalots A, Orive V, Loizate A, Titó L, Portabella E, Otazua P, Calvo M, Botella MT, Thomson C, Mundi JL, Quintero E, Nicolás D, Borda F, Martinez B, Gisbert JP, Chaparro M, Jimenez Bernadó A, Gómez-Camacho F, Cerezo A, Casal Nuñez E; Workgroup for the Study of Ischaemic Colitis of the Spanish Gastroenterological Association (GTECIE-AEG). Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol. 2011;46:236-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yang JL S-Editor: Gong ZM L-Editor: A P-Editor: Wang LL