Published online May 7, 2019. doi: 10.3748/wjg.v25.i17.2122
Peer-review started: January 18, 2019
First decision: January 30, 2019
Revised: February 5, 2019
Accepted: February 22, 2019
Article in press: February 23, 2019
Published online: May 7, 2019
Processing time: 109 Days and 4.9 Hours
Inflammatory bowel disease (IBD) is a chronic, inflammatory disorder characterised by both intestinal and extra-intestinal pathology. Patients may receive both emergency and elective care from several providers, often in different hospital settings. Poorly managed transitions of care between providers can lead to inefficiencies in care and patient safety issues. To ensure that the sharing of patient information between providers is appropriate, timely, accurate and secure, effective data-sharing infrastructure needs to be developed. To optimise inter-hospital data-sharing for IBD patients, we need to better understand patterns of hospital encounters in this group.
To determine the type and location of hospital services accessed by IBD patients in England.
This was a retrospective observational study using Hospital Episode Statistics, a large administrative patient data set from the National Health Service in England. Adult patients with a diagnosis of IBD following admission to hospital were followed over a 2-year period to determine the proportion of care accessed at the same hospital providing their outpatient IBD care, defined as their ‘home provider’. Secondary outcome measures included the geographic distribution of patient-sharing, regional and age-related differences in accessing services, and type and frequency of outpatient encounters.
95055 patients accessed hospital services on 1760156 occasions over a 2-year follow-up period. The proportion of these encounters with their identified IBD ‘home provider’ was 73.3%, 87.8% and 83.1% for accident and emergency, inpatient and outpatient encounters respectively. Patients living in metropolitan centres and younger patients were less likely to attend their ‘home provider’ for hospital services. The most commonly attended specialty services were gastroenterology, general surgery and ophthalmology.
Transitions of care between secondary care settings are common for patients with IBD. Effective systems of data-sharing and care integration are essential to providing safe and effective care for patients. Geographic and age-related patterns of care transitions identified in this study may be used to guide interventions aimed at improving continuity of care.
Core tip: Patients with Inflammatory bowel disease (IBD) are often exposed to transitions of care between providers and settings which negatively impacts care continuity. This is the first paper to identify and measure the location and type of hospital encounters for IBD patients in England at a National level. Patterns of care identified in this study are important to guide the exchange of health information between providers to ensure safe, high quality care for patients with IBD.
- Citation: Warren LR, Clarke JM, Arora S, Barahona M, Arebi N, Darzi A. Transitions of care across hospital settings in patients with inflammatory bowel disease. World J Gastroenterol 2019; 25(17): 2122-2132
- URL: https://www.wjgnet.com/1007-9327/full/v25/i17/2122.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i17.2122
Inflammatory bowel disease (IBD) includes the chronic relapsing inflammatory disorders Crohn’s disease and ulcerative colitis[1]. These are generally lifelong diseases, characterised by periods of remission and flares, with symptoms that include bloody diarrhoea, urgency, fatigue, weight loss, and abdominal pain. IBD affects 1 in 250 people in the United Kingdom giving an estimated prevalence of 240000[2]. The peak incidence occurs in patients between the ages of 15 and 30 years[3]. IBD may impact many aspects of the affected individual's life, accounting for substantial direct and indirect costs to the individual, the health care system and society[4].
A combination of factors including centralisation of healthcare services[5-7], difficulty accessing local services[8] and patient mobility between regions for education, employment or relationships may require IBD patients to access care in multiple settings. Furthermore, many IBD patients require care for extra-intestinal manifestations of disease[9-12] which is often provided by several specialists in multiple settings. The unpredictable nature of disease may also require attendance to acute care services[13] in organisations separate to the patient’s usual IBD care provider. The resulting multidisciplinary ‘patient-sharing’ between healthcare providers is characterised by multiple transitions of care. These transitions may impair continuity of care delivery and lead to care fragmentation[14].
Fragmentation of patient care is characterised by ineffective communication among providers and across healthcare agencies, insufficient patient and caregiver education, poor continuity of care, including medication reconciliation, and limited access to services, which contributes to negative quality and cost outcomes[15]. Fragmented inpatient care has been shown to be associated with a higher likelihood of in-hospital mortality, colonoscopy and longer readmission length of stay[16]. An increasing range of investigations and treatment options for IBD[17] adds further complexity to care transitions and necessitates the transfer of accurate and contemporaneous information at a secondary and tertiary care level.
Quality standards in IBD care specify that services should be coordinated across the multidisciplinary care pathway[18]. Many patients, however, may still ‘fall though the cracks’ between providers[19]. The objective of this study was to determine the type and location of hospital services accessed by IBD patients in England. Identifying and measuring the frequency and distribution of patient-sharing may inform the development of more effective and efficient data-sharing practices between providers and assist in optimising systems at a local, regional and national level.
This was a retrospective observational study using hospital administrative data. Adult patients resident in England that accessed inpatient care and had a recorded ICD-10 IBD disease-specific code (K50, K51) were identified from the Hospital Episode Statistics Admitted Patient Care dataset. Patients were recruited from this data set over a 2-year ‘recruitment period’ from April 2011 to March 2013. Each patient was then followed for a 2-year period from the date of their index admission, with the final patients recruited concluding follow-up by 30th March 2015. Patients that did not have any follow-up events after their index encounter were excluded from further analysis.
In England, healthcare provider organisations, or ‘Trusts’, provide acute hospital services[20]. To accommodate organisational change over the study period, providers that merged or separated over the study period were treated as a single merged provider across the whole study period. Low-volume providers with less than 1000 total IBD patient encounters over the 4-year period of data were excluded.
Each patient recruited into the study was allocated a ‘home provider’, which was identified as the Trust through which more of a patient’s outpatient care in gastroenterology was delivered during the study period than any other provider. Patients that did not have any gastroenterology outpatient appointments were excluded from analysis.
The primary outcome measure was the proportion of encounters that adult IBD patients in England have with their identified ‘home provider’. Secondary outcome measures included the distribution of IBD patient-sharing, regional differences in IBD patient-sharing, age-related differences in accessing services and type and frequency of outpatient specialty services accessed by patients with a diagnosis of IBD.
We identified the frequency and location of accident and emergency, inpatient and outpatient encounters for IBD patients within National Health Service (NHS) England and determined the proportion of attendances to previously identified ‘home providers’.
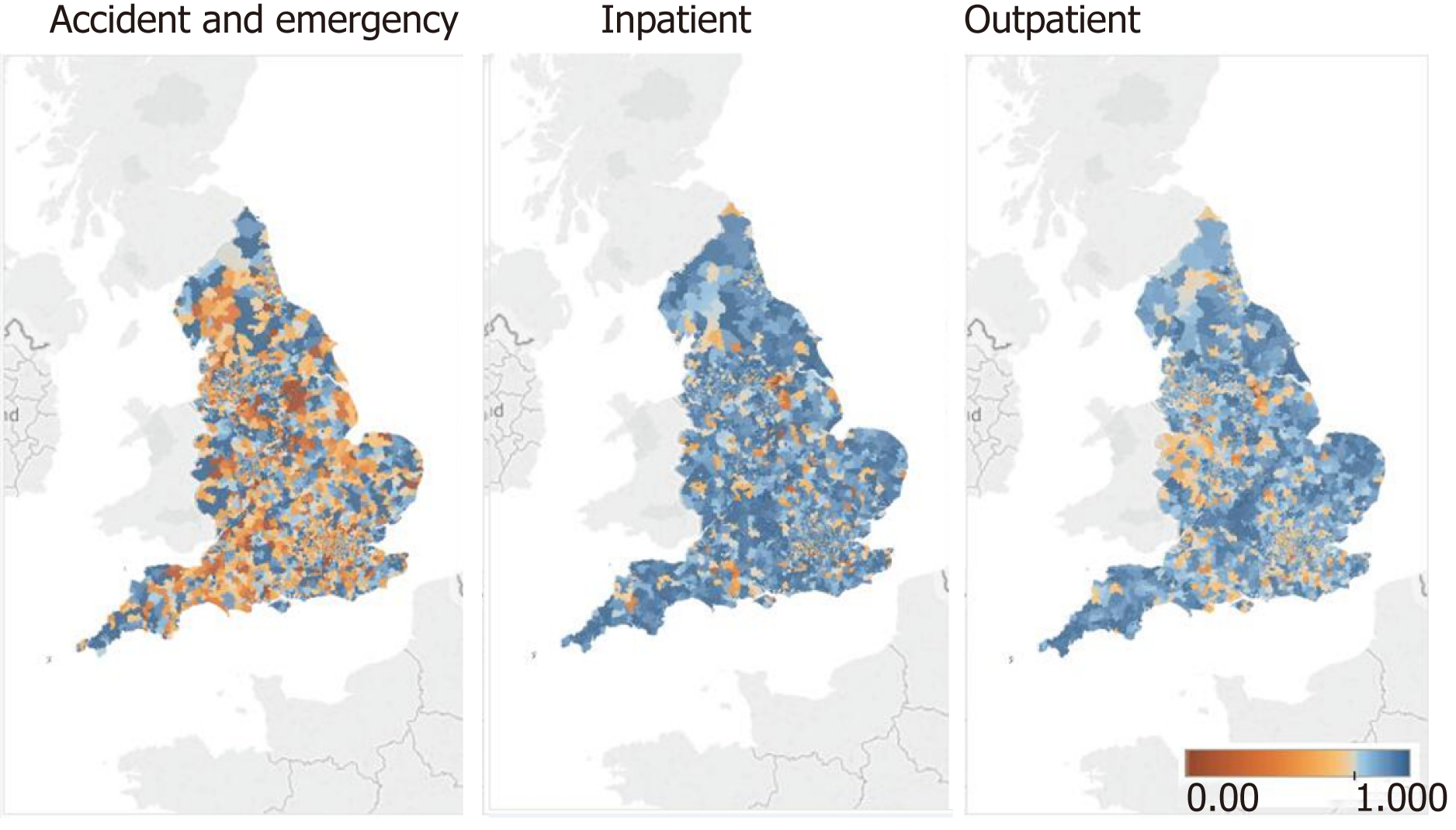
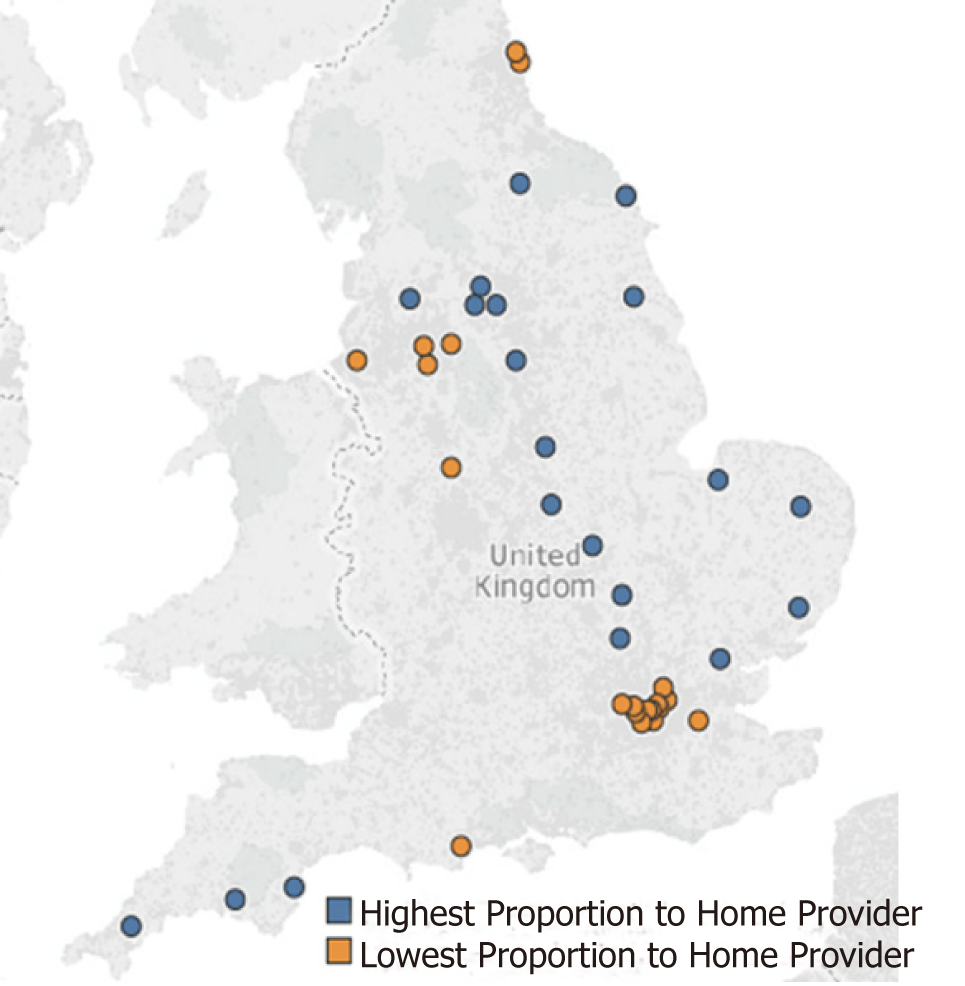
Middle Layer Super Output Areas (MSOA) associated with each patient was used to map their residential region within England. MSOAs represent a geographic region with a population between 5000 and 7200 people[21]. The estimates incidence of IBD in England is 0.5%-1%, yielding around 50 patients per MSOA[22]. To further analyse and illustrate regional differences in patient-sharing, the 20 provider organisations with the highest and lowest proportions of IBD patients attending their identified ‘home provider’ for healthcare were identified and mapped geographically.
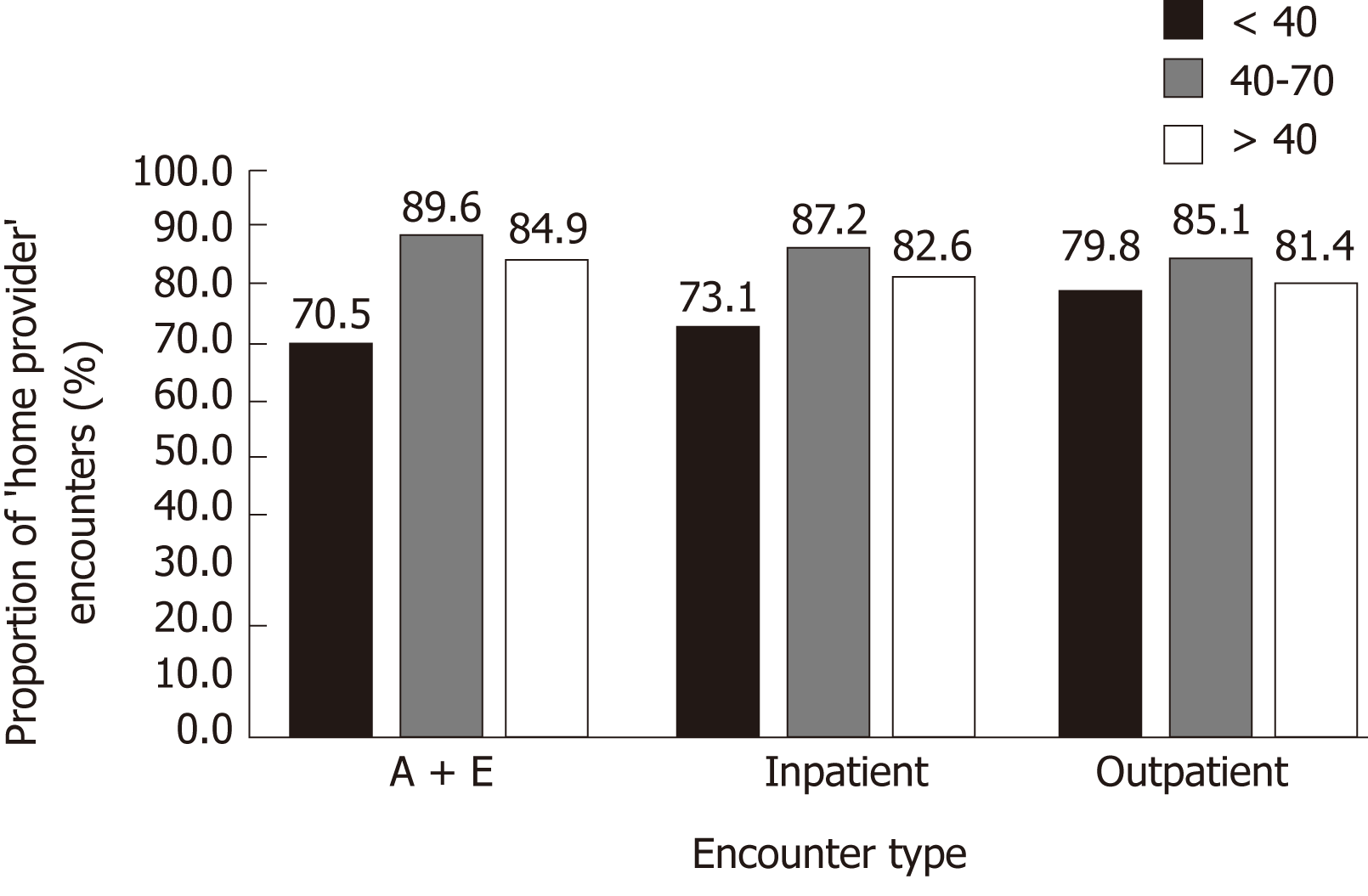
Access to care services was compared for three age bands, < 40, 40-70 and > 70 years, to determine differences in the proportion of patients accessing services through their ‘home provider’ for all patient encounter types.
In NHS England, outpatient encounters are coded using main specialty codes or treatment function codes pertaining to the clinical service provided[23,24]. For recruited patients, we reviewed outpatient encounters within the follow-up period to determine the type of specialty services that IBD patients consulted with and the frequency of these.
The investigators had complete access to the Hospital Episode Statistics (HES) dataset for the study period covering April 2011 to March 2015. Data was cleaned prior to analysis with removal of incomplete and duplicate records. Python (Python Software Foundation) was used for data extraction and analysis and Tableau (Tableau Software) for data visualisation. Statistical analysis and review were performed by biomedical statisticians (JC, MB).
126295 patients fulfilled the inclusion criteria and were recruited from the HES data set during the 2-year recruitment period. 31240 (24.7%) patients did not have gastroenterology appointments during the follow-up period and were therefore unable to be allocated a ‘home provider’ and excluded. 95055 patients remained for further analysis. This patient group had a total of 110300 accident and emergency, 304996 inpatient and 1344860 outpatient events over the 2-year follow-up period, including their first hospital admission through which they were recruited (Table 1).
| Total encounters | ‘Home provider’ encounters | ‘Home provider’ proportion (%/% provider range) | |
| Accident and emergency | 110300 | 80836 | 73.3 (37.0-94.3) |
| Inpatient | 304996 | 267540 | 87.8 (57.2-98.5) |
| Outpatient | 1344860 | 1117779 | 83.1 (55.7-96.9) |
| Total | 1760156 | 1466155 | 83.3 |
76 low-volume providers with less than 1000 IBD patient encounters over the 2-year recruitment period were excluded, comprising a total of 8030 (0.00456%) encounters. A total of 144 providers remained for further analysis.
1466155 of 1760156 (83.3%) IBD patient encounters were with the ‘home provider’. Of those patients recruited who attended accident and emergency departments during the study period, 73.3% of those attendances were to their allocated ‘home provider. 87.8% of inpatient hospital admissions in recruited patients were to their ‘home provider’ while 83.1% of outpatient attendances across all specialties were to their ‘home provider’ (Table 1). The range of proportions of ‘home provider’ encounters per trust was 37.0% to 94.3% for accident and emergency encounters, 57.2% to 98.5% for inpatient encounters and 55.7% to 96.9% for outpatient encounters.
There were regional differences in the proportion of ‘home provider’ encounters for each encounter type by the MSOA of residence of participants (Figure 1). For each ‘home provider’ the proportion of clinical encounters for patients allocated to that provider attending their ‘home provider’ was calculated. The highest and lowest 20 providers per proportion of ‘home-provider’ healthcare encounters is shown in Figure 2. Providers with a low proportion of ‘home provider’ encounters for IBD patients were typically located in metropolitan areas in Greater London and the North West of England and those with a high proportion of ‘home provider’ encounters were based outside major metropolitan areas.
The proportion of ‘home provider’ encounters for all event types in patients aged < 40, 40-70 and > 70 years illustrated in Figure 3. This shows lower ‘home provider’ encounters for patients under 40 years of age for all encounter types. The highest proportion of ‘home provider’ encounters was seen in the 40-70 years age group for all encounter types. All results were significant at P < 0.001 for pairwise χ2 tests.
Specialty service and treatment codes pertaining to 130 different outpatient services were identified for included patients. These services included outpatient consultations and therapies, such as physiotherapy. The 20 most common outpatient medical and specialty services that IBD patients consulted with are listed in Table 2. Encounters with these 20 services constituted 84.3% of total outpatient events for IBD patients. There were 546768 gastroenterology outpatient appointments, accounting for 39.8% of all outpatient services accessed in this group of IBD patients. Between general surgery and colorectal surgery there were 96220 total outpatient encounters, accounting for 7.0% of outpatient encounters in this patient group. Ophthalmology consultations were also common, with 53237 (3.9%) encounters.
| Outpatient service(HES Code) | Frequency (% of total services listed) |
| Gastroenterology (301) | 546768 (39.8) |
| General surgery (100) | 55126 (4.0) |
| Ophthalmology (130) | 53237 (3.9) |
| Trauma and orthopaedics (110) | 52510 (3.8) |
| Rheumatology (410) | 50781 (3.7) |
| Colorectal surgery (104) | 41094 (3.0) |
| Dermatology (330) | 39392 (2.8) |
| Physiotherapy (650) | 36895 (2.7) |
| General medicine (300) | 32595 (2.4) |
| Cardiology (320) | 29748 (2.2) |
| Diagnostic imaging (812) | 29454 (2.1) |
| Urology (101) | 27939 (2.0) |
| Gynaecology (502) | 25260 (1.8) |
| Obstetrics (501) | 22805 (1.7) |
| Respiratory medicine (340) | 22238 (1.6) |
| Ear, nose and throat (120) | 21953 (1.6) |
| Clinical haematology (303) | 21031 (1.5) |
| Anticoagulant service (324) | 18013 (1.3) |
| Nephrology (361) | 14847 (1.1) |
| Clinical oncology (800) | 14522 (1.1) |
Through retrospective analysis of HES data we reviewed the records of 95055 patients with IBD and examined their interactions with NHS England hospitals over a 2-year period. These patients were involved in a total of 1760156 encounters during the 2-year follow-up period from recruitment. A majority of patients accessed accident and emergency, inpatient and outpatient care through the same ‘home provider’ that they attended for gastroenterology outpatient care. A substantial proportion of patients, however, accessed care from different hospital providers, particularly when using accident and emergency services (26.7% of accident and emergency encounters). This is an important finding that is congruent with previous research on the prevalence of fragmentation in IBD care[16] and underscores the need for effective systems to manage transitions of care and sharing of patient information between settings. Centralisation of care between hospitals is increasingly common in healthcare systems around the world and these findings may be replicated in other systems internationally. Poor interoperability of health record systems between organisations remains commonplace in many healthcare systems, including NHS England[25-28]. Primary care services traditionally aided in monitoring and guiding care coordination[29], however many patients in England find General Practitioner services difficult to access[8]. There is increasing momentum towards empowering IBD patients to take control of their own health records and disease management, although this requires infrastructure investment and may not be suitable for all patients[30]. Hospital providers therefore need to continue to improve interoperability or provide alternative effective data-sharing capacity to maintain continuity of care for patients using services across settings.
Analysis of the distribution of ‘home provider’ events by MSOA of participants and provider locations showed a trend towards increased non-‘home provider’ attendance in metropolitan centres. All of the 20 providers with the lowest proportion of IBD patients attending that same provider for healthcare were located in major metropolitan centres including London, Manchester, Birmingham and Liverpool. In these areas, the proportion of encounters with the usual gastroenterology ‘home provider’ was as low as 1 in 3 (37%) for accident and emergency encounters and only half of inpatient (57.2%) or outpatient (55.7%) encounters. Reasons for this may include increased service centralisation in these regions or ease of access to alternative providers for urgent or non-IBD related care. Regardless, this is an important finding as it indicates that within metropolitan centres, there is a more dynamic ecosystem of care and increased need to ensure adequate exchange of health information.
More than one in four (26.7%) accident and emergency encounters were with a different hospital to the patient’s gastroenterology ‘home provider’. This is more than the proportion of non-‘home provider’ events for inpatient (12.2%) and outpatient (16.9%) services. Reasons for this finding may include a lack of accident and emergency services at the ‘home provider’ Trust, a need for urgent care necessitating presentation to the nearest hospital or patient preference. Importantly, this finding indicates that many patients seen acutely may not have comprehensive or up-to-date medical records held at that organisation. This may impact on the timeliness, effectiveness and safety of their care delivered by that provider. Additionally, information from an acute presentation may not be communicated with their usual ‘home provider’, again contributing to potential downstream transition of care errors.
It is also important to note that up to 19% of patients with IBD treated at a referral centre may be readmitted within 30 d[31]. Some patients may re-present to a different organisation than the previous provider, and these presentations may not be identified by those hospitals as readmissions. A lack of comprehensive, recent information regarding the patient may impact negatively on care and reduce the likelihood of avoiding preventable admission.
Improving communication and coordination between specialty services may reduce fragmentation of care and improve continuity for IBD patients. Specialty services accessed by IBD patients in this study reveals a broad range of services covering intraluminal and extraluminal disease. Clearly there is a need for effective information exchange between gastroenterology and general and colorectal surgical services with significant overlap between these specialties in the care of IBD patients. Previous studies estimate that approximately 10% of IBD patients experience eye problems such as uveitis, keratopathy, episcleritis and dry eyes[32,33] which may contribute in part to the frequent usage of ophthalmology services by patients in this study. Likewise, rheumatology and dermatology were some of the most common outpatient specialty services accessed by patients in this study and may reflect the increased predisposition to rheumatology and skin disease in IBD patients[10,34-36].
Some differences were seen in the proportion of ‘home provider’ care accessed by IBD patients across ages. Younger patients had a significantly lower proportion of care events with their ‘home provider’. These differences were most prominent in accident and emergency encounters where patients under the age of 40 attended their ‘home provider’ for care on 70.5% of occasions, compared with 89.6% in patients aged 40-70 and 84.9% aged over 70. This may be explained, in part, by the increased mobility of younger patients who may be more likely to live, study or work in locations away from their ‘home provider’.
This was a retrospective observational study using a large, national administrative data set from 2013 to 2015. This has facilitated a novel analysis of transitions of care between secondary care settings for IBD patients in England. When applying these findings to the current population it is important to note that there may have been changes to organisational structures and systems in addition to evolving regional demographics in the period since collection of this data. It is also important to note the inherent limitations of administrative data due to procedure changes, missing data and miscoding issues.
During patient recruitment and allocation of ‘home providers’ some losses may have resulted from the limitation of only being able to recruit patients from inpatient encounters. This approach was required as disease-specific codes are not allocated to outpatient and accident and emergency encounters within the data set. Additionally, patients that had existing but inactive disease also may not have been allocated an IBD disease code. In essence, only patients receiving care for 'active' IBD may have been recruited in some settings. This paper did not consider the reasons for the hospital events considered beyond the specialty responsible for that care event. This approach provided a clear overview of the services accessed but limited more in-depth interpretation of patient events, such as relevance of presentations to IBD and reasons for readmission.
Transitions of care between hospitals and primary care settings were beyond the scope of this study which used only hospital administrative data. Analysis of linked primary care and hospital-level databases may provide additional insights into hospital-primary transitions of care within this patient group and assist the important care coordination role played by many primary care providers. Patients under the age of 18 were excluded from analysis in this paper. This was necessary to permit an unbiased view of adult IBD patient-sharing. Although beyond the scope of this work, research to identify patterns of care transitions between paediatric and adult services using the methods developed in this paper may improve understanding of this challenging period for many young patients with IBD[37,38].
This paper has focussed on simple directed inter-organisational patient sharing connections. Previous, more complex healthcare network analysis studies have identified significant heterogeneity within patient sharing networks, with certain actors, whether hospitals or individual physicians, exercising different roles within a network[39-41]. More in-depth analysis of the networks studied in this paper may offer further insights into patient sharing within the NHS and further guide interventions. Additional analyses of other hospital-level factors such as hospital size, IBD patient numbers and IBD service availability may provide additional insights in future work. Furthermore, inclusion of existing data-sharing capacity between providers in a more complex analysis may provide additional value to guide future policy development.
The burden of disease for IBD patients can be reduced by improvements to care coordination and transitions of care between services. This study has shown that many patients with IBD in England access care from hospital providers in multiple settings. Younger patients and those residing in metropolitan areas tend to have their care shared between more providers and are at increased risk of transition of care errors in the absence of effective data-sharing practices. These groups are likely to benefit most from improvements to systems of health information exchange and care integration. Critically, this younger patient population may be more willing and able to adopt patient-led tools for medical record keeping, and therefore carry their clinical data with them on their mobile devices to be available to clinicians wherever they present. Similarly, improving transitions of care between specialty services such as gastroenterology, general and colorectal surgery, ophthalmology, trauma and orthopaedics, rheumatology and dermatology are likely to benefit IBD patients. Organisations that regularly share IBD patients would benefit most from improved community data sharing. Further work to identify these patient-sharing networks and the important role of primary care services in these networks would assist in guiding improvements. The approaches used to identify hospitals and specialties that share the care of patents could be applied to other chronic and complex disease processes to better delineate provider care networks across systems.
In conclusion, to ensure quality and safe care for patients with IBD, providers should have access to the right information about the right patient at the right time. Findings from this work have shown that patients with IBD often transition between different hospital providers in multiple settings. This may act as a barrier to accessing up-to-date patient health information and negatively impact care. These findings should encourage and assist the development of mechanisms to enable effective and efficient coordination of care between providers that share the care of IBD patients.
Inflammatory bowel disease (IBD) is a chronic, inflammatory disorder characterised by both intestinal and extra-intestinal pathology. Patients may receive both emergency and elective care from several providers, often in different hospital settings. Poorly managed transitions of care between providers can lead to inefficiencies in care and patient safety issues. To ensure that the sharing of patient information between providers is appropriate, timely, accurate and secure, effective data-sharing infrastructure needs to be developed. To optimise inter-hospital data-sharing for IBD patients, we need to better understand patterns of hospital encounters in this group.
There is limited data on the types of hospital services accessed by patients with IBD and the frequency and location of hospital encounters. Identification of patterns of hospital care can guide inter-hospital data-sharing and care coordination which may improve continuity of care for these patients.
This study aimed to identify and quantify the hospital services accessed by patients with IBD in England.
This retrospective observational study used Hospital Episode Statistics, a large administrative dataset in National Health Service in England, to identify characteristics of hospital care encounters for IBD patients. The proportion of encounters with providers other than the patients usual ‘home provider’ of IBD care was calculated, in addition to associations with patient age, location and type of specialist providers attended.
The proportion of encounters with hospitals other than the usual gastroenterology ‘home provider’ for 95055 IBD patients was up to 26.7% for accident and emergency encounters, followed by 16.9% for outpatient and 12.2% for inpatient encounters. Patients living in cities and younger patients were less likely to attend their ‘home provider’ for hospital services. The most commonly attended outpatient specialty services were gastroenterology, general surgery and ophthalmology.
Up to one in four accident and emergency encounters for patients with IBD in England were with a different provider to the patient’s usual gastroenterology ‘home provider’ of IBD care. IBD patients also often attended other hospitals for a range of outpatient and inpatient services. These findings emphasise the importance of developing effective data-sharing strategies between hospitals to maintain continuity of information and continuity of care for IBD patients.
Findings from this study provide a national-level view of transitions of care between hospitals for patients with IBD in England. We have shown that certain groups of patients, including younger patients and those based in metropolitan areas, have more frequent transitions of care and may be a suitable target for further research and interventions to improve care continuity. Further qualitative and quantitative research is needed to understand the implications of these findings and improve inter-hospital data-sharing.
| 1. | Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011;474:307-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2019] [Cited by in RCA: 1980] [Article Influence: 132.0] [Reference Citation Analysis (2)] |
| 2. | British Society of Gastroenterology. BSG Commissioning ReportI-nflammatory Bowel Disease (IBD) [Internet]. 2017;[cited 2018 Mar 5] Available from: http://www.bsg.org.uk/images/Commissioning_report/BSG_Acute_Inflammatory_Bowel_Disease.pdf. |
| 3. | Johnston RD, Logan RF. What is the peak age for onset of IBD? Inflamm Bowel Dis. 2008;14 Suppl 2:S4-S5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 114] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 4. | Burisch J, Jess T, Martinato M, Lakatos PL; ECCO -EpiCom. The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013;7:322-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 791] [Cited by in RCA: 764] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 5. | Beggs AD, Mcglone ER, Thomas PRS. Impact of centralisation on vascular surgical services. Br J Healthc Manag. 2012;18:468-473. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Boddy AP, Williamson JM, Vipond MN. The effect of centralisation on the outcomes of oesophagogastric surgery--a fifteen year audit. Int J Surg. 2012;10:360-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Woo YL, Kyrgiou M, Bryant A, Everett T, Dickinson HO. Centralisation of services for gynaecological cancer. Cochrane Database Syst Rev. 2012;CD007945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | NHS England. Improving access to general practice [Internet]. 2016;[cited 2018 Mar 5] Available from: https://www.england.nhs.uk/gp/gpfv/redesign/improving-access/. |
| 9. | Danese S, Semeraro S, Papa A, Roberto I, Scaldaferri F, Fedeli G, Gasbarrini G, Gasbarrini A. Extraintestinal manifestations in inflammatory bowel disease. World J Gastroenterol. 2005;11:7227-7236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 223] [Cited by in RCA: 229] [Article Influence: 11.5] [Reference Citation Analysis (2)] |
| 10. | Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol. 2006;12:4819-4831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 204] [Cited by in RCA: 217] [Article Influence: 10.9] [Reference Citation Analysis (1)] |
| 11. | Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2015;21:1982-1992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 546] [Cited by in RCA: 502] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 12. | Harbord M, Annese V, Vavricka SR, Allez M, Barreiro-de Acosta M, Boberg KM, Burisch J, De Vos M, De Vries AM, Dick AD, Juillerat P, Karlsen TH, Koutroubakis I, Lakatos PL, Orchard T, Papay P, Raine T, Reinshagen M, Thaci D, Tilg H, Carbonnel F; European Crohn’s and Colitis Organisation. The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease. J Crohns Colitis. 2016;10:239-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 573] [Article Influence: 57.3] [Reference Citation Analysis (11)] |
| 13. | Huang M, Rose E. Pediatric inflammatory bowel disease in the emergency department: Managing flares and long-term complications. Pediatr Emerg Med Pract. 2014;11:1-16; quiz 17-8. [PubMed] |
| 14. | Boockvar K, Vladeck BC. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2004;52:855-6; author reply 856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 645] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 15. | Coleman EA, Smith JD, Raha D, Min SJ. Posthospital medication discrepancies: Prevalence and contributing factors. Arch Intern Med. 2005;165:1842-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 497] [Cited by in RCA: 525] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 16. | Cohen-Mekelburg S, Rosenblatt R, Gold S, Shen N, Fortune B, Waljee AK, Saini S, Scherl E, Burakoff R, Unruh M. Fragmented Care is Prevalent Among Inflammatory Bowel Disease Readmissions and is Associated With Worse Outcomes. Am J Gastroenterol. 2019;114:276-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2693] [Cited by in RCA: 2773] [Article Influence: 115.5] [Reference Citation Analysis (3)] |
| 19. | Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 671] [Cited by in RCA: 800] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 20. | National Audit Office. A Short Guide to the Department of Health and NHS England [Internet]. 2017;[cited 2018 Mar 11] Available from: https://www.nao.org.uk/wp-content/uploads/2017/09/2017-Short-Guide-to-the-Department-of-Health-and-NHS-England.pdf. |
| 21. | NHS. Middle Layer Super Output Area [Internet]. 2018;[cited 2018 Mar 3] Available from: http://www.datadictionary.nhs.uk/data_dictionary/nhs_business_definitions/m/middle_layer_super_output_area_de.asp?shownav=1. |
| 22. | Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46-54.e42; quiz e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3789] [Cited by in RCA: 3604] [Article Influence: 257.4] [Reference Citation Analysis (6)] |
| 23. | NHS. Main Specialty Code [Internet]. 2018;[cited 2018 Mar 14] Available from: http://www.datadictionary.nhs.uk/data_dictionary/attributes/m/main_specialty_code_de.asp?shownav=1. |
| 24. | NHS. Treatment Function Code [Internet]. 2018;[cited 2018 Mar 14] Available from: http://www.datadictionary.nhs.uk/data_dictionary/attributes/t/tran/treatment_function_code_de.asp?shownav=1. |
| 25. | TechUK. techUK’s Interoperability Charter [Internet]. 2015;[cited 2018 Mar 14] Available from: http://www.techuk.org/insights/news/item/5276-techuk-s-interoperability-charter. |
| 26. | Perlin JB. Health Information Technology Interoperability and Use for Better Care and Evidence. JAMA. 2016;316:1667-1668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Holmgren AJ, Patel V, Adler-Milstein J. Progress In Interoperability: Measuring US Hospitals' Engagement In Sharing Patient Data. Health Aff (Millwood). 2017;36:1820-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 28. | Reis ZSN, Maia TA, Marcolino MS, Becerra-Posada F, Novillo-Ortiz D, Ribeiro ALP. Is There Evidence of Cost Benefits of Electronic Medical Records, Standards, or Interoperability in Hospital Information Systems? Overview of Systematic Reviews. JMIR Med Inform. 2017;5:e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Walsh A, Mabee J, Trivedi K. Inflammatory bowel disease. Prim Care. 2011;38:415-32; vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Panés J, O'Connor M, Peyrin-Biroulet L, Irving P, Petersson J, Colombel JF. Improving quality of care in inflammatory bowel disease: what changes can be made today? J Crohns Colitis. 2014;8:919-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Christian KE, Jambaulikar GD, Hagan MN, Syed AM, Briscoe JA, Brown SA, Campbell EV, Gadani AB, Cross RK. Predictors of Early Readmission in Hospitalized Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017;23:1891-1897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol. 2003;48:663-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 33. | Rosenbaum JT. Uveitis in spondyloarthritis including psoriatic arthritis, ankylosing spondylitis, and inflammatory bowel disease. Clin Rheumatol. 2015;34:999-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 34. | Rhodes JM, Collins P. Lessons for inflammatory bowel disease from rheumatology. Dig Liver Dis. 2006;38:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011;7:235-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Timani S, Mutasim DF. Skin manifestations of inflammatory bowel disease. Clin Dermatol. 2008;26:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (3)] |
| 37. | Cooley WC. Adolescent health care transition in transition. JAMA Pediatr. 2013;167:897-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Campbell F, Biggs K, Aldiss SK, O'Neill PM, Clowes M, McDonagh J, While A, Gibson F. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. 2016;4:CD009794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 230] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 39. | Lee BY, McGlone SM, Song Y, Avery TR, Eubank S, Chang CC, Bailey RR, Wagener DK, Burke DS, Platt R, Huang SS. Social network analysis of patient sharing among hospitals in Orange County, California. Am J Public Health. 2011;101:707-713. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 40. | Landon BE, Onnela JP, Keating NL, Barnett ML, Paul S, O'Malley AJ, Keegan T, Christakis NA. Using administrative data to identify naturally occurring networks of physicians. Med Care. 2013;51:715-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 41. | Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Med Care. 2009;47:787-793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 148] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ierardi E, Serban ED, Sipos F, Suzuki H, Tsujikawa T S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ