Published online Oct 21, 2018. doi: 10.3748/wjg.v24.i39.4472
Peer-review started: July 30, 2018
First decision: August 27, 2018
Revised: September 3, 2018
Accepted: October 5, 2018
Article in press: October 5, 2018
Published online: October 21, 2018
Processing time: 80 Days and 15.2 Hours
To study factors associated with esophageal and non-esophageal cancer morbidity among Barrett’s esophagus (BE) patients.
A cohort study within a single tertiary center included 386 consecutive patients with biopsy proven BE, who were recruited between 2004-2014. Endoscopic and histologic data were prospectively recorded. Cancer morbidity was obtained from the national cancer registry. Main outcomes were BE related (defined as esophagus and cardia) and non-BE related cancers (all other cancers). Cancer incidence and all-cause mortality were compared between patients with high-grade dysplasia (HGD) and with low-grade or no dysplasia (non-HGD) using Kaplan-Meier curves and cox regression models.
Of the 386 patients, 12 had HGD, 7 had a BE related cancer. There were 75 (19.4%) patients with 86 cases of lifetime cancers, 76 of these cases were non-BE cancers. Seven (1.8%) and 18 (4.7%) patients had BE and non-BE incident cancers, respectively. Twelve (3.1%) patients had HGD as worst histologic result. Two (16.7%) and 16 (4.4%) incident non-BE cancers occurred in the HGD and non-HGD group, respectively. Ten-year any cancer and non-BE cancer free survival was 63% and 82% in the HGD group compared to 93% and 95% at the non-HGD group, respectively. Log-rank test for patients with more than one endoscopy, assuring longer follow up, showed a significant difference (P < 0.001 and P = 0.017 respectively). All-cause mortality was not significantly associated with BE HGD.
Patients with BE and HGD, may have a higher risk for all-cause cancer morbidity. The implications on cancer prevention recommendations should be further studied.
Core tip: Barrett’s esophagus (BE) is known to be associated with esophageal carcinoma (EAC) and increased all cause and cancer specific mortality, but EAC is responsible only for a minority of BE mortality cases. We found patients with high-grade dysplasia to be more prone to non-BE related cancers, on top of BE related cancers. Such information can affect the recommended extraesophageal surveillance, and contribute the debate about the cost-effectiveness of endoscopic surveillance and to health systems decision making.
- Citation: Bar N, Schwartz N, Nissim M, Fliss-Isacov N, Zelber-Sagi S, Kariv R. Barrett’s esophagus with high grade dysplasia is associated with non-esophageal cancer. World J Gastroenterol 2018; 24(39): 4472-4481
- URL: https://www.wjgnet.com/1007-9327/full/v24/i39/4472.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i39.4472
Barrett’s esophagus (BE) is a premalignant condition in which intestinal metaplasia replaces normal squamous epithelium at the distal esophagus[1,2]. BE predisposes for esophageal adenocarcinoma (EAC), and current guidelines recommend endoscopic surveillance for early detection[1,2] and endoscopic treatment of early esophageal neoplasia[3-7]. BE surveillance is associated with earlier stage EAC and increased survival[8,9]. In addition, endoscopic treatment can result in complete eradication of both dysplasia and intestinal metaplasia and a reduced risk of disease progression[7,10-12].
Mortality in the overwhelming majority of BE patients is not related to EAC but is rather due to non-esophageal malignancies and cardiovascular disorders[11,13,14]. All-cause mortality is higher in patients with advanced grades of BE dysplasia compared to matched controls[11,14]. Non-esophageal cancer mortality in Danish patients with high grade dysplasia (HGD) was higher than non-dysplastic BE and matched controls, though comparing HGD to non-dysplastic BE was not an endpoint, and was not analyzed for significance[14]. Another population based cohort study conducted in Israel showed increased prevalence of colorectal, prostate, kidney, bladder and thyroid cancer in BE patients occurring at a younger age compared to matched controls[15]. To the best of our knowledge, no other publications examined the potential association between histologic features of BE and non-EAC cancer morbidity. Better characterization of cancer morbidity among patients with BE may identify risk factors and enable better surveillance, cancer prevention and optimal resource use[16]. Therefore, the primary aim of the current study was to study cancer morbidity and overall mortality within a prospectively followed cohort of BE patients according to grade of dysplasia.
All consecutive BE patients undergoing upper endoscopy at the Tel-Aviv Sourasky medical center between 2009-2014 were included, thus determining sample size. Clinical, endoscopic, and histologic data were collected from patient files in a prospective manner between 2009 and 2014. Pre-study data was retrospectively collected, as far back as 2004.
BE was defined as having a characteristic endoscopic appearance of any length, and histologic diagnosis of intestinal metaplasia with goblet cells on biopsies taken from the columnar esophageal mucosa[1].
This is a retrospective cohort study.
Tel-Aviv Sourasky medical center - a tertiary referral center for BE.
Data collection included the following parameters for each endoscopy: BE segment length-circumferential and maximal lengths were calculated and recorded according to the Prague classification[17]. We categorized the BE segment length as long (BE segment measuring 3 cm and above), short (1-2.9 cm), and ultra-short (< 1 cm). Presence of endoscopic abnormalities was also recorded. Histologic results for each endoscopy were classified as no dysplasia, low grade dysplasia (LGD), HGD, intramucosal adenocarcinoma (IMC), and EAC[18]. All biopsies with suspected dysplasia were reviewed by 2 expert GI-pathologists. If a patient had more than one dysplasia result or endoscopic report, the most severe dysplasia as well as the longest BE segment during follow up were chosen for analysis, respectively. Individual follow up was censored either by a diagnosis of cancer, at the end of the follow up period (December 2014), or death. Patient information collected included age, gender, cancer history (including type of cancer), individual number of endoscopies during the study period, and date of death.
The primary outcome of this study was non-BE cancer incidence, and secondary aims included BE related cancer and overall mortality. In order to determine the difference in cancer morbidity in patients with higher degrees of dysplasia, we compared patients who had HGD and patients with LGD or non-dysplastic BE (non-HGD group).
Cancer morbidity data was retrieved from the Israeli national cancer registry (NCR). The NCR records all incident cases of malignant neoplasms other than basal or squamous cell skin cancers. Trained registrars review available documents from hospitals, pathology labs, and death certificates from local health authorities. Upon retrieval of data from the NCR, its records were updated until December 2014.
Cancers were categorized as BE related or non-BE related. As diagnostic inaccuracies between EAC and gastric cardia adenocarcinoma are known to occur[19], we classified them both as BE cancers. All other malignancies were recorded as non-BE cancer. For all cancer free analysis, we used cancer cases which occurred within the follow up period. We also recorded cases occurring before the first available endoscopy as pre-study cancer, and reported the total life-time cancers retrieved from the NCR.
The date of death information was retrieved from the Central Bureau of Statistics.
This study was approved by our center’s institutional review board - approval number 0022-09. As data were collected from medical records throughout the study, informed consent was waivered by the institutional review board.
Categorical variables were described as frequency and percentage and continuous variables were presented with mean (standard deviation) median, (range) as needed. Comparisons between patients with HGD and patients with lower degrees of dysplasia (non-HGD) were performed using Chi-square test (or Fisher’s exact test) for categorical variables. For continuous variables, the independent-sample t-tests (or Mann-Whitney test) were used.
For each patient, the cancer free survival time was calculated based on the first endoscopy date (i.e., start date) and the first cancer date or the end of the follow-up date (December 2014) for patients who were cancer free. For non-BE cancer, we used the first non-BE cancer date for the calculation. Kaplan-Meier curve was utilized to compare survival trends, using the Log-rank test. All Kaplan-Meier analysis was done for patients with multiple endoscopies to avoid confounding. In addition, the Cox regression was used to perform univariate and multivariable regression in all patients (adjusting for potential confounders, found to be associated with HGD in the univariate analysis), displaying the hazard ratios (HRs) and adjusted HR (Adj.HR) with 95% confidence intervals (95%CI).
The statistical analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC, United States). Significance was set at P < 0.05.
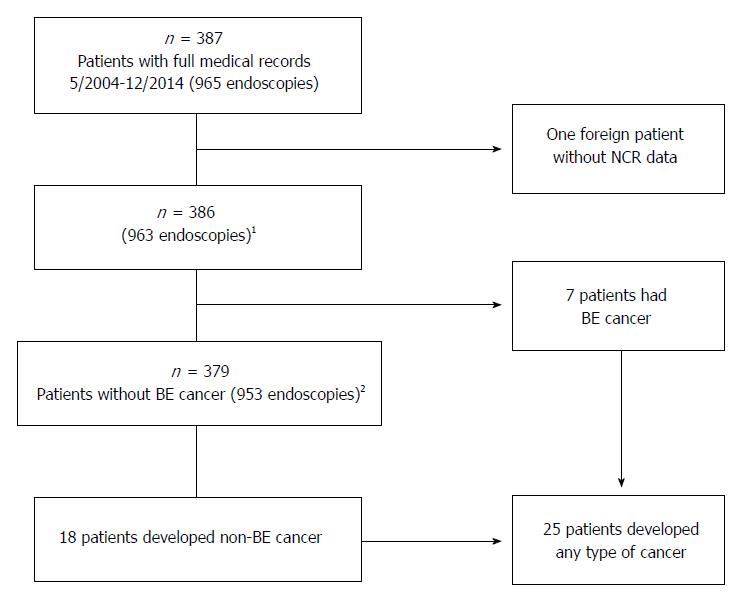
A total of 387 patients with biopsy proven BE were included with endoscopic data starting at May 2004 until December 2014. One foreign patient with missing NCR data was excluded, leaving 386 for analysis, see Figure 1. The analysis for non-BE cancer among BE patients with or without dysplasia, included 379 patients who did not develop IMC or BE-cancer during the study follow-up. The total cohort number of endoscopies was 963, with a mean of 2.5 ± 2.0 endoscopies per patient. Two hundred sixty-eight (69.4%) were males with an overall mean age of 60.0 ± 13.1 years (Table 1). Long segment BE was found in 225 (59.7%) of patients. The worst degrees of dysplasia/neoplasia were LGD, HGD, IMC, and EAC in 19 (4.9%), 12 (3.1%), 1 (0.3%), and 6 (1.6%), respectively. Study inclusion per year is shown in Supplementary Table 1 in the supplementary section.
| Patient data | All sample (n = 386) | HGD (n = 12) | Non-HGD (n = 367) |
| Age at study inclusion | 60.0 (13.1) [61.1, 18.4-89.6] | 66.3 (12.8) [66.6, 42.4-85.8] | 59.8 (13.2) [60.6, 18.4-89.6] |
| Gender - male | 268 (69.43) | 9 (75) | 253 (68.94) |
| Number of endoscopies per patient | 2.5 (2.0) [2, 1-17] | 6.6 (2.6) [7, 3-11] | 2.4 (1.7) [2, 1-10]b |
| Patients with multiple endoscopies | 245 (63.47%) | 12 (100) | 227 (61.9)a |
| Circumferential extent of BE (cm) | 3.3 (3.3) [2, 0-19] | 4.5 (2.92) [4.5, 1-11] | 3.2 (3.23) [2, 0-19] |
| Maximal extent of BE (cm) | 4.4 (3.2) [3, 0.2-20] | 6.0 (3.22) [6, 2-14] | 4.25 (3.17) [3, 0.2-20]a |
| Presence of endoscopic abnormalities | 56 (14.51) | 8 (66.67) | 44 (11.99)b |
| Ultra-short BE segment (BE < 1 cm) | 28 (7.43) | 0 (0) | 28 (7.8) |
| Short BE segment (1 cm ≤ BE < 3 cm) | 124 (32.89) | 2 (18.18) | 122 (33.98) |
| Long BE segment (BE ≥ 3 cm) | 225 (59.68) | 9 (81.82) | 209 (58.22) |
| Worst degree of dysplasia | |||
| Esophageal adenocarcinoma | 6 (1.6) | ||
| Intramucosal carcinoma | 1 (0.3) | ||
| High grade dysplasia | 12 (3.1) | ||
| Low grade dysplasia | 19 (4.9) | ||
Seventy-five patients (19.4%) had invasive lifetime cancers, reported by the NCR database, of whom 10 (2.6%) had lifetime BE cancers. There were pre-study cancers in 50 (13%) patients, of which 3 were BE cancers (0.8%) and 47 were non-BE cancers (12.2%). Incident cancers occurred in 7 BE cancers (1.8%) patients and non-BE cancers in 18 (4.7%) patients. The pre-study cancers and incident cancers are detailed in Table 2. Of note, one of the 2 esophageal pre-study cancers was a squamous cell carcinoma and not EAC. Subjects pre-study cancers were not included in cancer outcome analysis as they occurred outside of follow up period as explained in the materials and methods section.
| Pre-study cancers | Incident cancers | Lifetime cancers | |
| Esophagus | 2 (0.5)2 | 4 (1) | 6 (1.6) |
| Cardia | 2 (0.5) | 3 (0.8) | 5 (1.3) |
| Stomach | 3 (0.8) | 0 (0) | 3 (0.8) |
| Colorectal cancer | 9 (2.3) | 1 (0.3) | 10 (2.6) |
| Small intestine | 1 (0.3) | 0 (0) | 1 (0.3) |
| Cholangiocarcinoma | 1 (0.3) | 0 (0) | 1 (0.3) |
| Pancreas | 0 (0) | 2 (0.5) | 2 (0.5) |
| Bladder | 5 (1.3) | 4 (1) | 9 (2.3) |
| Prostate | 11 (2.8) | 0 (0) | 11 (2.8) |
| Kidney | 2 (0.5) | 2 (0.5) | 4 (1) |
| Hematologic cancer | 8 (2.07) | 4 (1) | 12 (3.1) |
| Skin | 4 (1) | 2 (0.5) | 6 (1.6) |
| Breast | 4 (1) | 2 (0.5) | 6 (1.6) |
| Thyroid | 3 (0.8) | 0 (0) | 3 (0.8) |
| Lung | 0 (0) | 2 (0.5) | 2 (0.5) |
| Kaposi | 0 (0) | 1 (0.3) | 1 (0.3) |
| Laryngeal | 3 (0.8) | 0 (0) | 3 (0.8) |
| Cervical | 1 (0.3) | 0 (0) | 1 (0.3) |
| Any type of cancer | 59 (15.3) | 27 (7) | 86 in 75 (19.4) patients1 |
| BE cancer | 3 (0.8) | 7 (1.8) | 10 in 10 (2.6) patients |
| Non-BE cancers | 56 (14.5) | 20 (5.2) | 76 in 65 (16.8) patients |
The HGD group included 12 patients, and the non HGD group (LGD and non-dysplastic BE) 367 patients. Comparison of these 2 groups is presented in Table 2 for demographic and endoscopic characteristics. In the HGD group 2 patients (16.7%) had non-BE incident cancers (lung and pancreatic cancers), compared with 16 (4.4%) patients in the non HGD group who had 18 cancers (in patients with 2 incident cancers the earliest one was included for analysis). As expected, patients with HGD, had a higher frequency of endoscopies, higher rate of endoscopic abnormalities (P < 0.001), and a longer maximal extent of BE compared with non-HGD patients (P < 0.01).
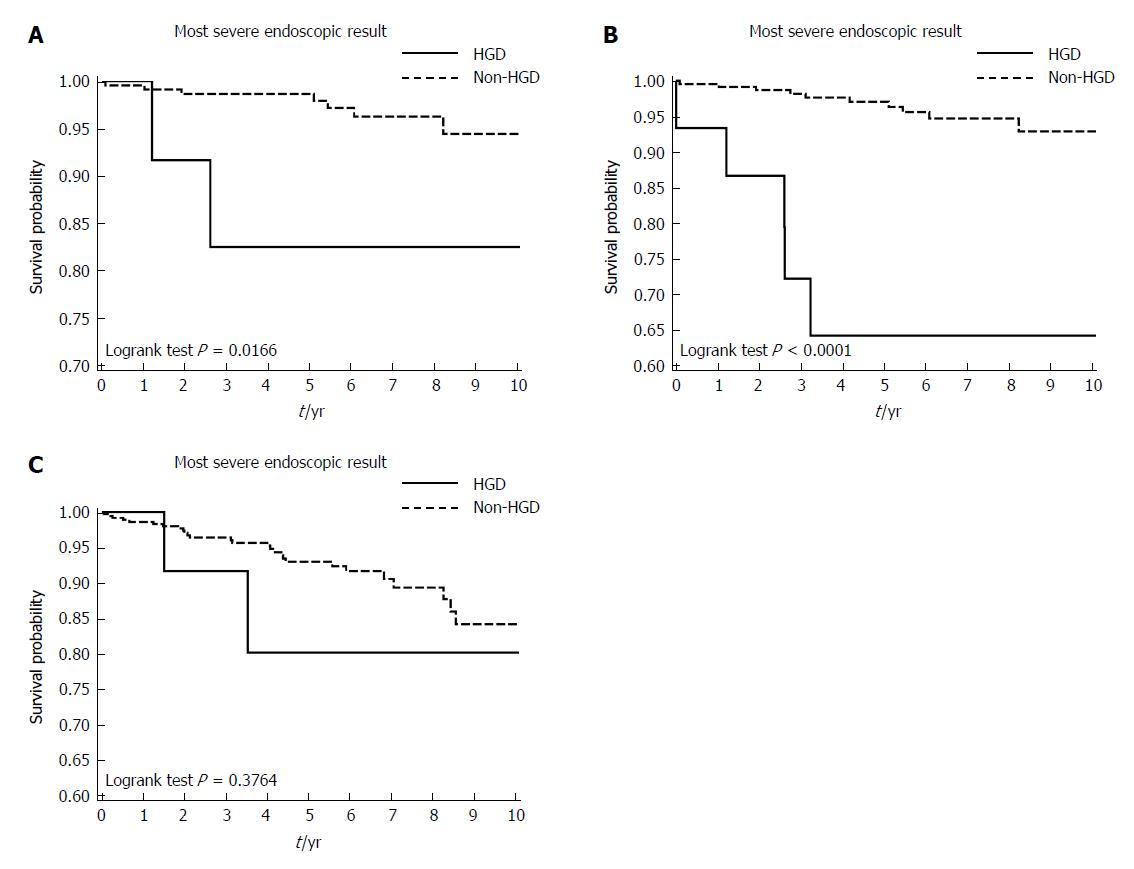
Kaplan-Meier survival curves for cancer free and all-cause survival are presented in Figure 2. To avoid the confounding effect of the number of endoscopies and assuring longer follow-up for all patients, Kaplan Meier analysis was done on patients with at least 2 endoscopies.
For the primary endpoint, non-BE cancer free survival was worse in patients with HGD compared with non-HGD, as shown in the Kaplan-Meier curves, Figure 2A. Log-rank test P-value was 0.0166 (n = 239), The 2-year and 10-year non-BE cancer free survival rates were 91% and 82% and 98% and 95% for the in HGD group and non-HGD group, respectively, in patients with multiple endoscopies. Univariate Cox regression analysis, Table 3, showed that HGD was not a significant predictor non-BE cancer (HR = 3.40, 95%CI: 0.78-14.84, P = 0.104), but in multivariable Cox regression adjusting for age, cancer history and number of endoscopies, HGD was significantly associated with increased risk for non-BE cancer (Adj.HR = 8.32, 95%CI: 1.35-51.33, P = 0.022).
| n = 379 (excluding EAC and IMC) | HR (95%CI) | Adjusted HR (95%CI) |
| Age at study inclusion1 | 1.11 (0.99-1.24) | 1.07 (0.95-1.21) |
| Gender - male | 2.19 (0.63-7.55) | |
| Number of endoscopies per patient | 0.82 (0.59-1.12) | 0.72 (0.50-1.03) |
| Presence of endoscopic abnormalities | 1.19 (0.34-4.09) | |
| Circumferential extent of BE (cm) | 0.99 (0.79-1.26) | |
| Maximal extent of BE (cm) | 1.06 (0.92-1.23) | |
| Ultra-short segment (BE < 1 cm) | 1 | |
| Short segment (1 cm ≤ BE < 3 cm) | 0.96 (0.11-8.24) | |
| Long segment (BE ≥ 3 cm) | 0.99 (0.13-7.85) | |
| Pre-study cancer history | 2.58 (0.92-7.25) | 2.12 (0.73-6.17) |
| HGD vs non-HGD | 3.40 (0.78-14.84) | 8.32 (1.35-51.33)a |
Examining the secondary endpoints, we saw a significant difference in the any-cancer free survival time among patients with HGD and patients with non-HGD, Figure 2B. Again, the worse outcome was in the HGD group, log rank test P < 0.001 (n = 245). For all-cause cancer, the 2-year and 10-year cancer free survival were 86% and 64% in the HGD group compared to 98% and 93% at the non HGD group, respectively.
Occurrence of all-cause cancer was associated with the maximal extent of the BE segment and HGD at the univariate analysis, see Table 4. After adjusting for age, number of endoscopies and pre-study cancer history, HGD was independently associated with all-cause cancer occurrence (Adj.HR = 4.28, 95%CI: 1.17-15.76, P = 0.029) whereas the maximal BE segment length was borderline significant (Adj.HR = 1.13 95%CI: 1-1.27, P = 0.050).
| n = 386 (including EAC and IMC) | HR (95%CI) | Adjusted HR (95%CI) |
| Age at study inclusion1 | 1.09 (0.99-1.20) | 1.08 (0.97-1.21) |
| Gender - male | 2.29 (0.79-6.67) | |
| Number of endoscopies per patient | 1.11 (0.96-1.29) | 0.99 (0.82-1.21) |
| Presence of endoscopic abnormalities | 2.27 (0.95-5.44) | |
| Circumferential extent of BE (cm) | 1.10 (0.96-1.26) | |
| Maximal extent of BE (cm) | 1.12 (1.008-1.24)a | 1.13 (1.000-1.27) |
| Ultra-short segment (BE < 1cm) | 1 | |
| Short segment (1 cm ≤ BE < 3 cm) | 0.97 (0.11-8.30) | |
| Long segment (BE ≥ 3 cm) | 1.77 (0.23-13.34) | |
| Pre-study cancer history | 2.15 (0.86-5.39) | |
| HGD vs non-HGD | 6.33 (2.37-16.91)b | 4.28 (1.17-15.76)a |
As BE cancer outcome was uncommon, we compared it with the Fisher exact test and not by statistical modeling. Among the 7 incident BE-cancer cases, 3 (42%) had HGD previously documented, while among the other 379 BE patients, only 12 (3.2%) had HGD (RR = 18.6, 95%CI: 4.6-75.6, P = 0.002)
There were 31 (8%) patients who died out of the entire cohort during the study period. Two (22.2%) of patients with IMC/EAC, 2 (16.7%), and 27 (7.0%) in the HGD and non-HGD groups respectively. Kaplan-Meier curve for mortality presented no association between HGD and all-cause mortality, Figure 2C. Log rank test P = 0.376 (n = 245). Cox regression analysis maintained this conclusion, after adjusting for age, cancer history and number of endoscopies for HGD (Adj.HR = 3.19, 95%CI: 0.66-15.46, P = 0.149).
The Kaplan-Meier curves for cancer free survival of the total cohort, including patients with a single endoscopy are shown in the online supplementary section, Supplementary Figure 1.
Our study reveals an association between BE with HGD and cancer outcome which, to the best of our knowledge, has not been reported before. Our main finding is that BE patients with HGD had a significantly higher risk of having non-BE cancer compared to patients with lower grades of dysplasia. This association was found in the group of patients who underwent more than a single endoscopy, which decreases the chance of dysplasia grade misclassification.
As expected, the known association between BE with HGD and adenocarcinoma of the esophagus or gastro-esophageal junction was also demonstrated in this study. Since this was an uncommon event, we did not use survival analysis models to investigate the association. We did not find HGD to be associated with all-cause mortality compared to lower levels of dysplasia.
The association between BE and extra-esophageal cancers mortality has long been studied. Most studies established increased cancer mortality risk in BE compared to normal population, even after matching for other risk factors[14,15,20-23]. In a large Danish registry study[14], patients with BE had a 71% increased all-cause mortality compared to matched controls, while the non-esophageal cancer mortality incidence rate was increased by 77% (14.7 cases per 1000 patient years) and was the leading cause for mortality. Moreover, patients with HGD had higher non-esophageal cancer mortality rates than patients with LGD or non-dysplastic BE: HR (95%CI) were 2.47 (1.98-3.07), 1.62 (1.31-2.01), and 1.44 (1.34-1.56), respectively. However, statistical significance of the difference between groups was not reported.
Wolf et al[11] looked at patients following radiofrequency ablation, in a United States based registry. A dose response effect for all-cause mortality to baseline BE degree of dysplasia with HGD having an adjusted odds ratio (95%CI) of 2.7 (1.7-4.4) vs 1.3 (0.7-2.2) for LGD and 1.6 (0.8-3.3) for indefinite dysplasia compared with non-dysplastic BE.
Solaymani-Dodaran et al[13] showed increased cancer specific mortality rates in patients with BE, but did not stratify the population according to dysplasia grade.
The above data described mortality, and not morbidity. Due to the lack of data about non-BE cancer morbidity we aimed to correlate it with BE degree of dysplasia. Assuming patients with dysplastic BE have higher mortality rate, our findings imply that the above association may be related, at least in part, to increased cancer incidence.
The role of gastro-esophageal reflux disease in BE is clear, but what predisposes certain patients to develop BE and neoplasia is still under debate. Studies have linked various factors such as smoking[24,25], abdominal obesity[26,27] genetics[28], and nutrition[29,30] to BE and dysplasia/EAC. Most of these factors are also associated with other non-BE malignancies[31].
The molecular basis of BE and EAC has been studied avidly, P53 and SMAD4 somatic mutations play a role in dysplastic BE and EAC development[32-35]. P53 is also a key player in many non-esophageal neoplasia, such as colorectal cancer, prostate cancer, and melanoma[36]. SMAD4 somatic mutations are prevalent in pancreatic cancer and colorectal cancer[37]. This complex association of molecular and environmental factors with BE dysplasia/neoplasia and other cancers may indicate similar cancer pathways induced by similar exposures.
Our findings imply that HGD in BE may be a marker of increased risk for cancer morbidity and therefore may require extraesophageal surveillance and lifestyle modification to prevent and decrease cancer risk. As for now, it may be prudent to stringently perform routine cancer screening tests among patients with BE and those with HGD in particular, according to age and gender and to recommend adherence to cancer protective lifestyle.
Given the low incidence of EAC mortality rates in BE patients, the risk-benefit and cost effectiveness of surveillance has been a matter of discussion, with conflicting evidence concerning EAC and mortality prevention and cost effectiveness[9,38-40]. We show another potential motivation for BE surveillance to better define overall cancer risk.
Our study carries some limitations. Investigator initiated studies done in teaching hospitals are prone to referral bias and are also smaller in size than population-based studies, limiting generalizability, and perhaps overestimating associations. On the other hand, patients with dysplasia are usually managed in a tertiary center.
We could not ascertain how long patients had BE before study inclusion, which may have influenced the outcomes. However, these estimates are approximate at best, as BE itself may be asymptomatic and this limitation is shared by other studies.
In our study, we adjusted for age and a past history of cancer, but we were not able to adjust for other risk factors such as lifestyle parameters. Our study did not include a population with no BE as a control, but we assume based on previous studies[14,15,20-23], that cancer rates are even lower in subjects with no BE. Death as an outcome was determined in this study according to ministry of health database, but cancer specific mortality was not available and cannot be associated with cancer morbidity. Our major limitation is the low statistical power due to the small number of patients with HGD and incident cancers, which reflects real life clinical data of an uncommon condition. In addition, the majority of patients were male, as prevalent in other studies[41]. Gender may act as a confounder when addressing cancer morbidity (as with prostate and breast cancer). Again, this reflects reality in many centers treating patients with BE.
The advantages of our study include a prospective comprehensive 6 year follow up of a relatively large number of consecutive BE patients within a single referral center, enabling a uniform data collection and fully verified clinical, endoscopic and revised histologic data.
In conclusion, in our cohort we found an endoscopic and histologic profile comparable to other Western world data. Non-BE related malignancies were more prevalent, and significantly associated with HGD as well as BE related malignancies in comparison with non HGD BE. Our findings suggest BE patients with HGD may have a significantly higher overall risk for cancer morbidity. This may imply endoscopic surveillance for BE patients could aid in prediction of all-cause cancer risk and encourage current cancer prevention measures such as lifestyle modification and appropriate cancer screening among patients. Further characterization of cancer morbidity and mortality profile among patients with BE should follow with large population-based studies.
Patients with Barrett’s esophagus (BE) are at risk for esophageal adenocarcinoma, and surveillance is recommended. However, non-esophageal cancer is the leading cause of death in this population. This raises questions about the focus we give to surveillance for esophageal cancer, and the need for broader cancer surveillance.
We wanted to better describe the non-esophageal cancer morbidity in patients with BE, and specifically in patients with high grade dysplasia (HGD). Finding that patients with HGD carry a higher non-esophageal cancer risk can direct efforts and resources for cancer prevention.
We aimed to describe the non-esophageal cancer morbidity in patients with BE, and to test whether patients with HGD have a higher risk as compared to low grade dysplasia. Indeed, in this study we have shown that compared to non-HGD, patients with HGD have a lower all cancer and non-BE cancer free survival. The significance of these findings is in the recognition of the importance of total cancer surveillance in these patients. In addition, by comparing non-esophageal cancer morbidity in HGD and less dysplastic BE, we show the added value of information received in surveillance endoscopies. These findings put the foundations for larger cohort studies, preferably multi-center for reaching a significant number of patients.
Endoscopic and histologic data were collected, and cancer morbidity data were retrieved from the national cancer registry. We compared non-esophageal cancers, all cancers and mortality between patients with HGD and less dysplastic BE. Cancer free survival analysis was done.
We found patients with HGD had a worse non-BE cancer free survival and all cancer free survival. The higher frequency of non-esophageal cancer in patients with HGD raises the question as to the reason for this association. Further population based and mechanistic studies are required to further investigate these reasons.
Our study shows that HGD may act as a marker for all cause cancer outcome, not just esophageal cancer. Perhaps it reflects a behavioral, environmental and genetic inclination towards malignancy. After endoscopic treatment for the dysplasia, we should focus our efforts to teach these patients about healthier lifestyle, and modifiable cancer risk factors such as smoking cessation and weight reduction. Perhaps in this population, screening for other malignancies may hold a different cost-effective profile.
Patients with BE and HGD have a higher non-esophageal cancer risk, on top of esophageal cancer risk. This should be confirmed in more prospective studies and population-based studies. This may shift the focus of esophageal based surveillance to a more holistic cancer prevention program for certain patients. Future research should include larger cohorts of patients from multiple centers, with detailed endoscopic and histologic data as well as other cancer risk factors including obesity measures and lifestyle behaviors as smoking, physical activity and dietary intake to better encompass risk stratification and prevention potential.
| 1. | Shaheen NJ, Falk GW, Iyer PG, Gerson LB; American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and Management of Barrett’s Esophagus. Am J Gastroenterol. 2016;111:30-50; quiz 51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1084] [Article Influence: 108.4] [Reference Citation Analysis (0)] |
| 2. | Fitzgerald RC, di Pietro M, Ragunath K, Ang Y, Kang JY, Watson P, Trudgill N, Patel P, Kaye PV, Sanders S. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett’s oesophagus. Gut. 2014;63:7-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1016] [Cited by in RCA: 912] [Article Influence: 76.0] [Reference Citation Analysis (1)] |
| 3. | Ell C, May A, Gossner L, Pech O, Günter E, Mayer G, Henrich R, Vieth M, Müller H, Seitz G. Endoscopic mucosal resection of early cancer and high-grade dysplasia in Barrett’s esophagus. Gastroenterology. 2000;118:670-677. [PubMed] |
| 4. | Pech O, Behrens A, May A, Nachbar L, Gossner L, Rabenstein T, Manner H, Guenter E, Huijsmans J, Vieth M. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008;57:1200-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 466] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 5. | Pouw RE, Wirths K, Eisendrath P, Sondermeijer CM, Ten Kate FJ, Fockens P, Devière J, Neuhaus H, Bergman JJ. Efficacy of radiofrequency ablation combined with endoscopic resection for barrett’s esophagus with early neoplasia. Clin Gastroenterol Hepatol. 2010;8:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 211] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 6. | Prasad GA, Wang KK, Buttar NS, Wongkeesong LM, Krishnadath KK, Nichols FC 3rd, Lutzke LS, Borkenhagen LS. Long-term survival following endoscopic and surgical treatment of high-grade dysplasia in Barrett’s esophagus. Gastroenterology. 2007;132:1226-1233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 233] [Cited by in RCA: 190] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 7. | Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277-2288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1146] [Cited by in RCA: 1001] [Article Influence: 58.9] [Reference Citation Analysis (2)] |
| 8. | Incarbone R, Bonavina L, Saino G, Bona D, Peracchia A. Outcome of esophageal adenocarcinoma detected during endoscopic biopsy surveillance for Barrett’s esophagus. Surg Endosc. 2002;16:263-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Corley DA, Levin TR, Habel LA, Weiss NS, Buffler PA. Surveillance and survival in Barrett’s adenocarcinomas: a population-based study. Gastroenterology. 2002;122:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 379] [Cited by in RCA: 344] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 10. | Orman ES, Li N, Shaheen NJ. Efficacy and durability of radiofrequency ablation for Barrett’s Esophagus: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 219] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 11. | Wolf WA, Pasricha S, Cotton C, Li N, Triadafilopoulos G, Muthusamy VR, Chmielewski GW, Corbett FS, Camara DS, Lightdale CJ. Incidence of Esophageal Adenocarcinoma and Causes of Mortality After Radiofrequency Ablation of Barrett’s Esophagus. Gastroenterology. 2015;149:1752-1761.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Brimhall B, Wani S. Current Endoscopic Approaches for the Treatment of Barrett Esophagus. J Clin Gastroenterol. 2017;51:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Solaymani-Dodaran M, Card TR, West J. Cause-specific mortality of people with Barrett’s esophagus compared with the general population: a population-based cohort study. Gastroenterology. 2013;144:1375-1383, 1383.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Erichsen R, Horvath-Puho E, Lund JL, Dellon ES, Shaheen NJ, Pedersen L, Davey Smith G, Sørensen HT. Mortality and cardiovascular diseases risk in patients with Barrett’s oesophagus: a population-based nationwide cohort study. Aliment Pharmacol Ther. 2017;45:973-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Pines G, Dickman R, Niv Y, Kashtan H, Birkenfeld S. Extraesophageal malignancies among patients with Barrett esophagus. J Clin Gastroenterol. 2014;48:e8-e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Richter JE. Editorial: maybe our ‘Barrett’s recommendation speech’ should change? Aliment Pharmacol Ther. 2017;45:1266-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Sharma P, Dent J, Armstrong D, Bergman JJ, Gossner L, Hoshihara Y, Jankowski JA, Junghard O, Lundell L, Tytgat GN. The development and validation of an endoscopic grading system for Barrett’s esophagus: the Prague C & M criteria. Gastroenterology. 2006;131:1392-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 731] [Cited by in RCA: 744] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 18. | Reid BJ, Haggitt RC, Rubin CE, Roth G, Surawicz CM, Van Belle G, Lewin K, Weinstein WM, Antonioli DA, Goldman H. Observer variation in the diagnosis of dysplasia in Barrett’s esophagus. Hum Pathol. 1988;19:166-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 529] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 19. | Lindblad M, Ye W, Lindgren A, Lagergren J. Disparities in the classification of esophageal and cardia adenocarcinomas and their influence on reported incidence rates. Ann Surg. 2006;243:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 124] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Sonnenberg A, Genta RM. Barrett’s metaplasia and colonic neoplasms: a significant association in a 203,534-patient study. Dig Dis Sci. 2013;58:2046-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Andrici J, Tio M, Cox MR, Eslick GD. Meta-analysis: Barrett’s oesophagus and the risk of colonic tumours. Aliment Pharmacol Ther. 2013;37:401-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Khalaf N, Ramsey D, Kramer JR, El-Serag HB. Personal and family history of cancer and the risk of Barrett’s esophagus in men. Dis Esophagus. 2015;28:283-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Solaymani-Dodaran M, Logan RF, West J, Card T, Coupland C. Risk of extra-oesophageal malignancies and colorectal cancer in Barrett’s oesophagus and gastro-oesophageal reflux. Scand J Gastroenterol. 2004;39:680-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 24. | Smith KJ, O’Brien SM, Smithers BM, Gotley DC, Webb PM, Green AC, Whiteman DC. Interactions among smoking, obesity, and symptoms of acid reflux in Barrett’s esophagus. Cancer Epidemiol Biomarkers Prev. 2005;14:2481-2486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 25. | Coleman HG, Bhat S, Johnston BT, McManus D, Gavin AT, Murray LJ. Tobacco smoking increases the risk of high-grade dysplasia and cancer among patients with Barrett’s esophagus. Gastroenterology. 2012;142:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Corley DA, Kubo A, Levin TR, Block G, Habel L, Zhao W, Leighton P, Quesenberry C, Rumore GJ, Buffler PA. Abdominal obesity and body mass index as risk factors for Barrett’s esophagus. Gastroenterology. 2007;133:34-41; quiz 311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 263] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 27. | Nelsen EM, Kirihara Y, Takahashi N, Shi Q, Lewis JT, Namasivayam V, Buttar NS, Dunagan KT, Prasad GA. Distribution of body fat and its influence on esophageal inflammation and dysplasia in patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2012;10:728-734; quiz e61- e62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Su Z, Gay LJ, Strange A, Palles C, Band G, Whiteman DC, Lescai F, Langford C, Nanji M, Edkins S. Common variants at the MHC locus and at chromosome 16q24.1 predispose to Barrett’s esophagus. Nat Genet. 2012;44:1131-1136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 29. | Kubo A, Levin TR, Block G, Rumore GJ, Quesenberry CP Jr, Buffler P, Corley DA. Dietary antioxidants, fruits, and vegetables and the risk of Barrett’s esophagus. Am J Gastroenterol. 2008;103:1614-1623; quiz 1624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 30. | Kubo A, Corley DA, Jensen CD, Kaur R. Dietary factors and the risks of oesophageal adenocarcinoma and Barrett’s oesophagus. Nutr Res Rev. 2010;23:230-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 31. | Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M; Comparative Risk Assessment collaborating group (Cancers). Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet. 2005;366:1784-1793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 831] [Cited by in RCA: 797] [Article Influence: 38.0] [Reference Citation Analysis (2)] |
| 32. | Fléjou JF. Barrett’s oesophagus: from metaplasia to dysplasia and cancer. Gut. 2005;54 Suppl 1:i6-i12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 126] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 33. | Gregson EM, Bornschein J, Fitzgerald RC. Genetic progression of Barrett’s oesophagus to oesophageal adenocarcinoma. Br J Cancer. 2016;115:403-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 34. | Weaver JMJ, Ross-Innes CS, Shannon N, Lynch AG, Forshew T, Barbera M, Murtaza M, Ong CJ, Lao-Sirieix P, Dunning MJ. Ordering of mutations in preinvasive disease stages of esophageal carcinogenesis. Nat Genet. 2014;46:837-843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 301] [Cited by in RCA: 284] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 35. | Dulak AM, Stojanov P, Peng S, Lawrence MS, Fox C, Stewart C, Bandla S, Imamura Y, Schumacher SE, Shefler E. Exome and whole-genome sequencing of esophageal adenocarcinoma identifies recurrent driver events and mutational complexity. Nat Genet. 2013;45:478-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 633] [Cited by in RCA: 617] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 36. | Whibley C, Pharoah PD, Hollstein M. p53 polymorphisms: cancer implications. Nat Rev Cancer. 2009;9:95-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 500] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 37. | Xia X, Wu W, Huang C, Cen G, Jiang T, Cao J, Huang K, Qiu Z. SMAD4 and its role in pancreatic cancer. Tumour Biol. 2015;36:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 38. | Bhat SK, McManus DT, Coleman HG, Johnston BT, Cardwell CR, McMenamin U, Bannon F, Hicks B, Kennedy G, Gavin AT. Oesophageal adenocarcinoma and prior diagnosis of Barrett’s oesophagus: a population-based study. Gut. 2015;64:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 109] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 39. | Corley DA, Mehtani K, Quesenberry C, Zhao W, de Boer J, Weiss NS. Impact of endoscopic surveillance on mortality from Barrett’s esophagus-associated esophageal adenocarcinomas. Gastroenterology. 2013;145:312-319.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 180] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 40. | Provenzale D, Schmitt C, Wong JB. Barrett’s esophagus: a new look at surveillance based on emerging estimates of cancer risk. Am J Gastroenterol. 1999;94:2043-2053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 230] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 41. | Cook MB, Wild CP, Forman D. A systematic review and meta-analysis of the sex ratio for Barrett’s esophagus, erosive reflux disease, and nonerosive reflux disease. Am J Epidemiol. 2005;162:1050-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 168] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Israel
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Hillman LC, Hirahara N, Sanaei O S- Editor: Wang XJ L- Editor: A E- Editor: Huang Y