Published online Jun 7, 2018. doi: 10.3748/wjg.v24.i21.2211
Peer-review started: March 27, 2018
First decision: April 11, 2018
Revised: April 26, 2018
Accepted: May 11, 2018
Article in press: May 11, 2018
Published online: June 7, 2018
Processing time: 70 Days and 1.7 Hours
Irritable bowel syndrome (IBS) is a common and troublesome disorder in children with an increasing prevalence noted during the past two decades. It has a significant effect on the lives of affected children and their families and poses a significant burden on healthcare systems. Standard symptom-based criteria for diagnosis of pediatric IBS have changed several times during the past two decades and there are some differences in interpreting symptoms between different cultures. This has posed a problem when using them to diagnose IBS in clinical practice. A number of potential patho-physiological mechanisms have been described, but so far the exact underlying etiology of IBS is unclear. A few potential therapeutic modalities have been tested in children and only a small number of them have shown some benefit. In addition, most of the described patho-physiological mechanisms and treatment options are based on adult studies. These have surfaced as challenges when dealing with pediatric IBS and they need to be overcome for effective management of children with IBS. Recently suggested top-down and bottom-up models help integrating reported patho-physiological mechanisms and will provide an opportunity for better understanding of the diseases process. Treatment trials targeting single treatment modalities are unlikely to have clinically meaningful therapeutic effects on IBS with multiple integrating patho-physiologies. Trials focusing on multiple combined pharmacological and non-pharmacological therapies are likely to yield more benefit. In addition to treatment, in the future, attention should be paid for possible prevention strategies for IBS.
Core tip: Even though irritable bowel syndrome (IBS) is a common worldwide pediatric problem, little is known of its exact patho-physiology and management. Therefore, a large number of children are suffering from its intestinal and extra-intestinal symptoms. Novel research using new advanced technologies based on proposed top-down and bottom-up models of patho-physiology and treatment trials focusing on multiple combined interventions are likely to be more beneficial in understating and treating pediatric IBS. In addition, the time has come to explore possible prevention strategies for this problem.
- Citation: Devanarayana NM, Rajindrajith S. Irritable bowel syndrome in children: Current knowledge, challenges and opportunities. World J Gastroenterol 2018; 24(21): 2211-2235
- URL: https://www.wjgnet.com/1007-9327/full/v24/i21/2211.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i21.2211
Irritable bowel syndrome (IBS) is a common pediatric functional gastrointestinal disorder (FGID)[1-10] with severe disabling upper and lower gastrointestinal symptoms[11] and extra-intestinal symptoms[1,11]. It has a significant impact on daily activities[2,11,12], education[11-13] and health related quality of life[9,10,13,14] of affected children. The healthcare consultation rate is high in affected children[1,9,15] and it leads to a significant annual healthcare cost[15-17].
Unlike many other gastrointestinal disorders, IBS and other FGIDs have major challenges in terms of diagnosis, underlying patho-physiology and management. In the absence of detectable biomarkers, IBS is a purely symptom based diagnosis[18]. However, the accepted diagnostic criteria for IBS have changed several times in the past[18-20] and are quite likely to change in the future. Keeping up with these changes is a major test for both clinicians and researchers dealing with IBS and in the past numerous disagreements have been reported even among medical professionals in terms of interpreting them[21,22]. Numerous mechanisms have been suggested as possible underlying causes for symptoms of IBS[23]. During the past decade the number of research on pediatric neuro-gastroenterology have increased at a global level and more and more studies have been conducted using non-invasive, sophisticated, cutting edge technologies to understand motility of the digestive tract, intestinal microbiota, underlying genetic and epigenetic mechanisms, gastrointestinal signaling molecules and different areas of the brain in relation to stimuli from the gut[23]. However, up to now these findings have failed to give a clear holistic picture on the underlying patho-physiology of IBS. Without a clear and proven understanding of the patho-physiology, it is not easy to design and conduct effective clinical trials for IBS. In addition, the therapeutic options of managing IBS is not all that well researched in children[24]. With all the research and clinical interest on non-communicable diseases including IBS around the globe, and emerging novel investigation techniques, there are more opportunities to understand the likely patho-physiology of childhood IBS, develop more therapeutic modalities to support children and moreover, to develop potential preventive methods.
In this review, we have attempted to highlight the main challenges concerning the diagnosis, patho-physiology and management of childhood IBS while summarizing the current knowledge on epidemiology, risk factors, patho-physiology, diagnosis and management. Furthermore, we have also outlined a road map for possible directions for future research which would of benefit to children with IBS.
IBS is a symptom based diagnosis. Therefore, defining the exact symptom based diagnostic criteria for childhood IBS has always been a major challenge.
At the beginning, all abdominal pain disorders in children were classified into one group labelled as recurrent abdominal pain by John Apley. He defined it as at least three episodes of abdominal pain, severe enough to affect their activities over a period longer than three months[25]. This definition was accepted by both clinicians and researchers all over the world for almost five decades. The formation of the Rome Foundation paved the way for developing a new diagnostic classification system for functional abdominal pain disorders. Introduction of Rome Criteria in 1989 for chronic abdominal pain in adults provided the opportunity to use the same criteria for the pediatric age group and it was demonstrated that a large proportion of children with chronic abdominal pain also fulfilled the adult criteria for IBS[26]. Based on these findings, Rome II criteria released in 1999, and subsequently the Rome III criteria released in 2006, included symptom-based diagnostic criteria for IBS in children[19,20]. Pediatric Rome criteria gained popularity immediately after they were released and have been adopted in subsequent research conducted in IBS[27-30]. However, both Rome II and Rome III criteria had their own deficiencies which were often directed to the difficulties in reporting and interpreting the symptoms between different cultures, populations, communities and social classes. Schurman et al[28], comparing the child report, parental report and the physician diagnosis, showed a diagnostic disagreement between the 3 groups when they used the Rome II criteria. Most of the time the reasons for the discrepancies in the diagnoses were due to disagreement on symptoms related to defecation. The diagnostic agreement (both Rome II and Rome III) was also poor when pediatric gastroenterologists were compared to gastroenterology fellows[21,22].
The deficiencies mentioned above, the expansion of knowledge and better understanding of childhood FGIDs paved the way for development of Rome IV criteria[18], released in 2016, after summarizing a decade of research on FGIDs[18]. In that venture, the label of abdominal pain related functional gastrointestinal disorders was replaced by the term functional abdominal pain disorders (FAPDs). In addition, the frequency of pain symptoms was differently worded from once a week for at least 2 mo in Rome III to at least 4 d per month for at least 2 mo[18]. However, the 4 main FAPDs; IBS, functional dyspepsia (FD), abdominal migraine (AM) and functional abdominal pain not specified (FAP-NS) remain the same. The new Rome IV criteria for IBS are summarized in Table 1. Exact validity of these Rome IV criteria need to be studied in the future.
| Diagnostic criteria for irritable bowel syndrome (IBS)[18] |
| Must include all of the following |
| Abdominal pain at least 4 d per month associated with one or more of the following: |
| Related to defecation |
| A change in frequency of stool |
| A change in form (appearance) of stool |
| In children with constipation, the pain does not resolve with resolution of the constipation (children in whom the pain resolves have functional constipation, not irritable bowel syndrome) |
| After appropriate evaluation, the symptoms cannot be fully explained by another medical condition |
| Above criteria needs to be fulfilled for at least 2 mo before diagnosis. |
| Diagnostic criteria for IBS subtypes[31] |
| IBS with predominant constipation |
| More than one-fourth (25%) of bowel movements with Bristol stool form types 1 or 2 and less than one fourth (25%) lf bowel movements with Bristol stool form types 6 or 7 |
| IBS with predominant diarrhea |
| More than one-fourth (25%) of bowel movements with Bristol stool form types 6 or 7 and less than one fourth (25%) lf bowel movements with Bristol stool form types 1 or 2 |
| IBS with mixed bowel habits |
| More than one-fourth (25%) of bowel movements with Bristol stool form types 1 or 2 and more than one fourth (25%) lf bowel movements with Bristol stool form types 6 or 7 |
| IBS unclassified |
| Patients who meet diagnostic criteria for IBS but whose bowel habits cannot be accurately categorized into 1 of the 3 groups above |
The sub-categories of IBS in children [IBS with predominant diarrhea (IBS-D), IBS with predominant constipation (IBS-C), IBS with mixed bowel habits (IBS-M) and IBS unclassified (IBS-U)] are included in Rome IV for the first time, in parallel with adult criteria (Table 1)[31]. Subcategories are very important in the management of affected children.
IBS is often reported as one of the commonest FGIDs in children. A recent meta-analysis conducted on epidemiologic studies on abdominal pain from 1957 to 2014, noted IBS in 8.8%, FD and FAP in 4.5% and 3.5% respectively. Another systematic review and meta- analysis on IBS in Asian children showed a higher prevalence of 12.4%[32]. Several studies from Greece, Nigeria, South America and Sri Lanka have recognized IBS as the most prevalent FGID among children and adolescents (2.9%, 9.9%, 3.8%-6.4% and 3.6%-7% respectively)[6-9,33-36]. Many other studies have also reported a high prevalence of IBS in China (13.25%)[1], Nigeria (16%)[2] and Turkey (22.6%)[3]. In contrast to this, studies from United States have shown lower prevalence rates of IBS (2.8% and 5.1%)[37,38]. A recent study from the Mediterranean region also reported IBS in 4% of children and adolescents[39]. However, it is not clear whether the differences in reported prevalence are true differences or are due to the differences in interpreting Rome criteria between different cultures in terms of pain characteristics and bowel habits.
Different subgroups of IBS have different bowel symptoms and because of that, the exact approach to the management differs between subgroups. Therefore, recognizing sub-types of IBS is of utmost importance in effective management of children with this conditions. Even though IBS sub-groups were only recently recognized in Rome IV criteria, in the past some researchers have used adult criteria to differentiate between sub-groups of IBS in children. A prospective, hospital based study from Italy reported IBS-C as the most prevalent IBS sub-type (45%) followed by IBS with mixed bowel habit and IBS unspecified (29%), and IBS-D (26%)[12]. Some other studies have reported IBS-C as the most common IBS sub-type too[3]. However, two more recent epidemiological from Greece and Nigeria reported higher prevalence of IBS-M (47.9% and 53.6% respectively). In these two studies IBS-D and IBS-C were noted in 16.7%-19% and 27.4%-6.3% respectively[2,33]. In contrast, an Asian study noted an almost similar prevalence of IBS-C, IBS-D and IBS-M (29%-30%)[11]. The changing nature of IBS subtypes is well established and in a 1 year of follow up study, a significant number of children changed their sub-type or outgrew their symptoms, indicating the instability of the proposed sub-types [12,40].
Numerous factors have been suggested as possible predisposing factors for IBS in children. However, pinpointing exact predisposing factors and avoiding them is a major challenge in the management of this condition.
Studies conducted so far have not shown gender as a clear risk factor for development of IBS. Some studies have reported a high prevalence of IBS in girls[2,11], while others failed to show such a difference[41]. Some studies have suggested that fluctuations in ovarian hormones may have an effect on development of symptoms in IBS[42,43]. However, the exact role of sex hormones on IBS is not yet clear.
Many studies have reported higher prevalence of IBS in children between 8-12 years and decrease in prevalence with advancing age[2,4,11,41]. The decreased rates of prevalence with age are most likely due to spontaneous resolution of IBS with time.
Several psychological factors have been recognized as risk factors for development of IBS. They include psychological stress[11,44,45], excess worry[45], anxiety[1,41], depression[1], physical, emotional and sexual abuse[46] and abnormal personality traits[1,10]. Furthermore, the adult studies have shown that these exposures lead to persistence of symptoms of FAPDs such as IBS into adulthood[47].
Exact relationship between early life events and paediatric IBS is not clear. Some studies have reported high prevalence of FAPDs in patients exposed to gastric suction during neonatal period[48], born to mothers with gestational diabetes and pregnancy induced hypertension[49], admitted to a special care baby unit[49], having an umbilical hernia[50], having pyloric stenosis[51], with Henoch-Schonlein purpura[52] and with a history of cow’s milk allergy[53]. However, further studies are needed to confirm these associations with IBS.
Past history of gastroenteritis is a well-recognized predisposing factor for development of IBS in children and adults[2,41,54,55]. A meta-analysis has reported a mean prevalence rate of IBS as 9.8% in individuals with history of infectious gastroenteritis, while it was 1.2% in controls[56]. In another systematic review, pooled incidence of IBS is 10% following acute gastroenteritis[57]. Even higher incidence of IBS (10%-15%) has been reported after bacterial gastroenteritis[58]. The gastrointestinal infections commonly associated with post-infectious IBS are Campylobacter species, Escherichia coli and Salmonella species[54,55]. Studies conducted so far have failed to demonstrate a clear association between viral gastroenteritis and IBS[59].
IBS and asthma-related symptoms occur frequently together and are independently associated with each other in adults[60-65]. Similarly other studies have reported an increased risk of IBS in children with allergic diseases[66]. In contrast, some other studies have failed to find an association between asthma and IBS[67].
Gastrointestinal disorders such as IBS are commonly attributed to ingestion of different food items such as certain carbohydrates and fats[68,69]. There is some evidence that higher intake of spicy food and fried food increase the risk of IBS[1,70]. However, the exact relationship between IBS and diet is not clear. The exact role of food allergy in the development of IBS is not well researched either[71]. There is some evidence that food allergy is also associated with IBS in children[41]. In contrast some other adult studies failed to demonstrate such an association[62]. However, a significant percentage of patients with IBS have a restricted diet with exclusion of certain foods and drinks[69,72,73].
Out of all the FGIDs, perhaps IBS is the most researched diseases entity in terms of its patho-physiology. These studies have reported large number of different and possible patho-physiological mechanisms. However, at the moment all these studies have only possibly touched on the surface of this complicated disease entity and have failed to demonstrate an exact patho-physiological mechanism/s. The majority of the patho-physiological studies include small samples, sometimes do not included a control group and the reported mean differences are too small to provide a statistical power to obtain meaningful conclusions[75]. In addition, some of the studies were conducted in a heterogeneous group of patients with chronic functional abdominal pain rather than in specifically in those with IBS and therefore could not be exactly applied to IBS. Several controversies exist in the proposed patho-physiology of IBS[76]. Strangely, most of the proposed mechanisms do not correlate with the clinical symptoms.
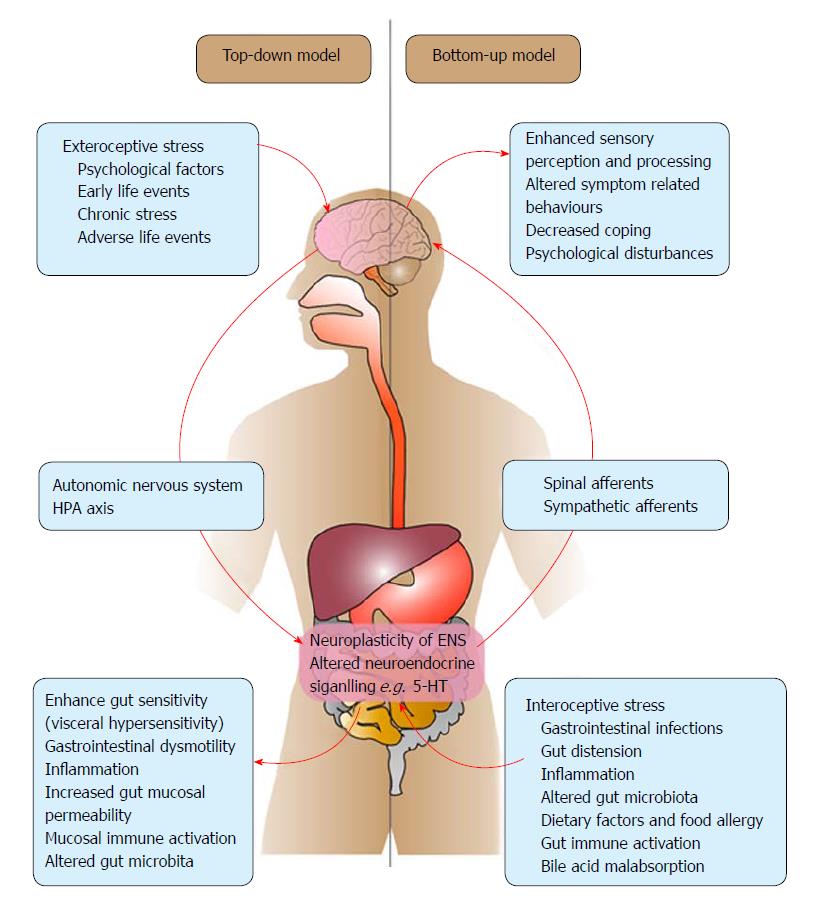
Two models have been proposed to explain the patho-physiology of IBS[77]. First is the “top-down model” which suggest that the main patho-physiological changes are initiated in the brain. According to this model, the primary disease processes in the brain interact with the peripheral organs through the brain-gut axis to generate alterations in the gut leading to clinical expression of IBS[78]. The proponents of the “bottom-up model” which proposes that peripheral factors in the gut play the a key role and the alteration in cerebral functions are secondary to brain-gut interactions[79].
In both models, a large number of patho-physiological mechanism have been suggested and interactions between these mechanisms are believed to result in the development of IBS in susceptible individuals. Main suggested patho-physiological mechanisms for IBS are illustrated in Figure 1 according to the top-down and bottom-up models.
In top-down model, the symptoms of IBS are believed to be caused by alternations in the central nervous system initiated by various stressors directed at the central nervous system (exteroceptive stress) such as adverse life events[11,45,46]. anxiety[1,41] and depression[1]. It is believed that several neural networks of the brain interact with each other in an intricate manner to generate symptoms. Studies conducted in adult patients with IBS have reported interactions between central executive network (involving attention, working memory planning and response selection), salient network (responding to external and internal stimuli that reach to the brain), sensory motor network and autonomic networks (central control of autonomic function)[76,78,80]. These interactions are believed to alter the activity of the enteric nervous system through the autonomic nervous system and hypothalamo-pituitary-adrenal axis (HPA axis), causing physiological changes in the gut including visceral hypersensitivity and alteration in motility, permeability, secretion, immune reactions and the microbiome[78,80].
The bottom-up model suggests that various stressors directed at the gut can influence central nervous system and alter the cortical response to the visceral stimuli causing symptoms in IBS[77]. Intestinal infections, mucosal inflammation, gut distension, immune mediated reactions, food allergy, alterations in gut microbial flora, increased intestinal permeability and abnormal responses of the enteric nervous system to gut stimuli (e.g., alterations in neurotransmitters such as serotonin) in combination or in isolation trigger symptom generation in this model. The gut may influence the brain via the intrinsic primary afferents neurons, whose cell bodies are located in cranial and dorsal nerve root ganglia. The sympathetic afferents from gut are believed to be the main mediator of nociceptive stimuli while vagal afferents are mainly believed to be involved in non-nociceptive sensations (e.g., local reflexes, gastric accommodation etc.)[77].
The main problem is that the patho-physiological changes reported in the gut and the central nervous system in patients of IBS up to now can be attributed to both these models and identifying which comes first is like a chicken or the egg situation. However, the introduction of these two models has laid some foundations for direction of further research in the patho-physiology of IBS.
Both conceptual models recognize interactions between brain and the gut as the main patho-physiological mechanism in IBS[77]. This bidirectional communication is called as the brain-gut axis and consists of the central and autonomic nervous systems, enteric nervous system and neuro-endocrine system and the neuro-immune system[23,81].
Autonomic nervous system: Autonomic nervous system has been considered to be one of the main communicators between the brain and the gut[82] in both top-down and bottom-up models of pathogenesis of IBS. However, so far very few studies have been conducted to assess the autonomic nervous system in IBS and its exact role in generation of symptoms is not clear.
Studies conducted in adults have shown a correlation between vagal response and post-prandial abdominal symptoms of IBS-D and IBS-C[83]. Some other studies have reported abnormal gastric motility and underlying vagal defects[83,84]. Another study has reported abnormal fingertip blood flow responses in subjects with IBS suggesting excess sympathetic activity[85]. Findings of the above studies suggest that a shifting of sympathetic-parasympathetic balance may contributes to the pathogenesis of IBS. However, some other studies failed to demonstrate abnormalities in autonomic functions in patients with IBS[86].
However, all these studies have assessed either cardiovascular or ocular autonomic functions, but not the autonomic functions of the gut specifically. How these findings can be directly applied to the autonomic functions of the gastrointestinal tract is far from clear. Currently no exact technique is available to assess the gastrointestinal autonomic functions. Therefore, development of such a technique is a major challenge and will provide better opportunities to understand the role of the autonomic nervous system in gut functions in both health and disease.
Hypothalamo-pituitary-adrenal axis: The hypothalamic-pituitary-adrenal axis (HPA axis) is considered to be an important communicator in the brain-gut axis. HPA axis is activated by both exteroreceptive and interoceptive stress and therefore likely to be involved in both patho-physiological models. Activation of HPA axis ultimately results in increased release of corticotrophin releasing hormone (CRH), adrenocorticotrophic hormone (ACTH) and cortisol. Increased release of CRH is believed to promote central sensitization while ACTH and cortisol tend to activate resident immune cells and extrinsic primary afferents in the gastrointestinal tract causing peripheral sensitization[23].
Corticotrophin releasing factor (CRF) is increasingly recognized as an important factor in the development of FGIDs including IBS. However, only a few human studies have been conducted so far and most of the assumptions are based on results of animal studies. One study reported an upregulation of CRF-Receptor type 1 (CRF-R1) in patients with IBS[87]. In addition, long-lasting epigenetic changes in the CRF expression have been reported in those exposed to neonatal stress, which results in the transcriptional responses to stress in adulthood[88]. In contrast, another study assessed the diurnal rhythm of cortisol and stress reactivity and showed that cortisol as a marker of stress does not have a major role in abdominal pain in infants[89]. Similar to humans, CRF-R1 upregulation, reversible mitochondrial damage and IBS like gut dysfunction were reported in rats after exposure to psychological stress. In this study, the increased CRF-R1 expression, reversible mucosal inflammation, increased epithelial permeability and conductance, and abnormal colonic response after exposure to stress lasted for a short duration (7 d) while visceral hypersensitivity observed after administration of exogenous CRF persisted for 30 d after exposure[90]. In agreement, others have reported that CRF and its receptors play an important role in stress related alterations of visceral sensitivity and gastrointestinal motility[91-93].
Numerous studies have been conducted in adults and children with IBS and large number of possible patho-physiological mechanisms have been suggested. However, they are like individual pieces of a large jig-saw puzzle and we are far from solving this complicated problem. Fitting up available information on patho-physiology and finding the missing pieces of this puzzle is a major challenge.
Visceral hypersensitivity: Visceral hypersensitivity is defined as an enhanced perception of mechanical triggers applied to the bowel which seem as pain and discomfort[94]. In normal individuals, physiological changes in the gastrointestinal tract such as motility and distension do not cause pain. When there is altered sensory response to physiological stimuli, it is called visceral hypersensitivity. Two main types of visceral hypersensitivity have been identified so far. They are hyperalgesia and allodynia. Hyperalgesia is defined as in intensified pain sensation in response to normal stimuli which usually do not provoke pain, while allodynia is the elevated nociceptive sensation in response to normal stimuli[95].
Visceral hypersensitivity is considered to be the cornerstone in the patho-physiology of IBS[76]. One pediatric study has reported decreased rectal sensory threshold for pain in IBS and functional abdominal pain[96]. Another study in children with IBS has demonstrated that abdominal pain is associated with abnormal perception of visceral sensations and hypersensitivity[97]. Similar results have been reported in several other pediatric studies too[98-100]. Adults studies have also reported lowered rectal pain threshold in patients with IBS[101]. Several factors such as psychological stress, gastrointestinal infections, alterations in gut microbiota, inflammation, immunological factors, food, as well as genes, have been suggested to induce visceral hypersensitivity[98,102,103]. Visceral hypersensitivity is believed to be results from pain modulation at both peripheral level as well as at central nervous system[95].
Modulation of pain: (1) At the enteric nervous system: Main function of the enteric nervous system is to regulate local gastrointestinal reflexes and to transmit sensory information to the central nervous system for processing and integration[104]. A vast majority of afferent information received from the gut is used for regulation of normal functions such as motility and secretion[105]. Information regarding the sensory perception and modulation at the level of enteric nervous system is limited. One study assessing mast cell-induced excitation of visceral nociceptive sensory neurons in adults with IBS has suggested the possibility of initiation and perpetuation of symptoms through modulation of sensory neurons in the enteric nervous system[106]. (2) At the central nervous system: Increased pain perception in IBS is considered to be at least partly related to altered descending inhibition and pain affecting at the peripheral level and catastrophizing of pain at the central level[107]. It is reported that increased pain perception in IBS is not due to the tendency to report more pain but because of increased spinal nociceptive transmission[107] and impaired endogenous inhibition of somatic pain[108]. When functional magnetic resonance imaging (fMRI) was used, insular cortex and pre-frontal cortex are recognized as the main areas of the central nervous system which are involved in the processing of visceral pain in IBS[109]. It is also possible that alterations in pain appraisal, hypervigilance to interoceptive signals from the gut and engagement of emotional arousal could also contribute to the patho-physiology[110].
Alterations in neurotransmitters and receptors: More and more emerging evidence have recognized alterations in serotonin as important mediator in pathogenesis of IBS[111]. Serotonin (5-hydrodytryptamine; 5-HT) is an important neurotransmitter in enteric neurons and paracrine signaling substance secreted by enterochromaffin (EC) cells in the intestinal mucosa[112]. It mediates communication between the brain and the gut[95], and has been shown to be the responsible agent for bloating, nausea and vomiting[113,114]. In addition, it is considered to be an important signaling molecule in the central nervous system involved in mood, appetite, sleep, memory and learning. Alterations in serotonin is implicated in central nervous system disorders such as anxiety, depression and some psychiatric disorders[115]. Serotonin is removed by a highly selective transporter called the serotonin transporter (SERT). Gene polymorphisms of SERT receptors have been shown to be associated with IBS[116-118]. In addition, some distinct changes in EC cell numbers and content as well as release and uptake of serotonin appear to have relevance to the patho-physiology of IBS[115,119,120].
Gastrointestinal dysmotility: A large number of studies have demonstrated abnormalities in gastric myoelectrical activity[121-124], gastric motility[123-130] and accommodation[131,132] and intestinal and colonic transit[125,133-135] in patients with IBS and other FAPDs. Few have reported an association between motility abnormalities and exposure to stress[128]. It is suggested that stress can lead to alterations in central aminergic network involving serotonin and noradrenaline[136] and therefore believed to play an important role in the pathogenesis of IBS, especially in the top-down model. However, so far no clear relationship has been demonstrated between motility abnormalities and symptoms in children with IBS[128]. Therefore, whether the observed gastrointestinal motor abnormities are a cause for IBS or an effect of IBS is yet to be determined.
Immune mediated mechanisms: Increased prevalence of allergies and atopic disorders including asthma have been shown in patients with IBS[137-139]. But the small number of research ventures conducted up to now with small sample sizes have failed to demonstrate an exact link with immunoglobulin E (IgE )[140,141]. Increased numbers of mass cells have been reported throughout the gastrointestinal tract in patients with IBS[102,142,143]. It is suggested that serotonin is released during degranulation of these cells and stimulates peripheral nerves in the submucosa and increases visceral sensitivity.
Infection, inflammation and intestinal barrier functions: It is suggested that visceral hypersensitivity observed in patient with IBS can be secondary to the activation of immune cells and to the development of low-grade inflammation. Studies conducted in children with IBS have demonstrated an accumulation of inflammatory cells in the intestinal mucosa[144]. A previous study conducted in children with FAP or IBS has reported an increased gut permeability and low grade inflammation. It has also been shown that the low grade inflammation was related to the degree to which pain interfered with activities[145]. The increased permeability is attributed to the enlarged spaces between epithelial cells, cytoskeletal condensation, abnormal gene and protein expression in tight junction proteins of intestinal epithelial cells and reduction in the expression of occluding and zonula occludens protein 1[146,147]. Bacterial mediated and proteasome mediated alterations have also been suggested as possible triggers for low grade inflammation which ultimately leads to increase intestinal permeability (“leaky gut”)[148].
IBS is common after gastroenteritis and it is often of the IBS-D type[149]. In post-infectious IBS, gastrointestinal infections are believed to stimulate the immune system causing low-grade inflammation[150]. Post-infectious IBS is associated with hyperplasia of EC cells, increased counts of neutrophils, mast cells and T cells in the colonic mucosa. It is believed that gastrointestinal infections stimulate the immune system causing low-grade inflammation leading to post-infectious IBS[150].
Microbiota: Gut microbiota is reported to be different in patients with IBS that in healthy individuals, with increased Firmicutes/Bacteroids ratio, increased relative abundance of fecal Ruminoccus torque like phenotypes and reduced bacterial diversity with increase in certain bacterial species (Enterobacteriaceae, Veillonella, Dorea) and reduction of other species (Bifidobacterium, Collinsella, Clostridiales)[110,151]. Children with IBS have significantly higher percentage of Haemophilus parainfluenzae in their gut[152-154]. Increasing visceral sensitivity, altered gastrointestinal transit and increase in permeability of the intestine is reported in experimental studies using germ free animals receiving gut microbiota of patients with IBS, indicating a potential pathogenic role of gut microbiota[155]. Some other studies have reported an association between differences in short chain fatty acid production by colonic bacteria and the development of symptoms in diarrhea predominant IBS[156]. Interactions between the gut microbiota and food (fermented protein products, generation of gases) are potential sources for cell damage, altered barrier function as well as symptoms such as bloating and distension[157]. In addition, gut microbiota may influence other patho-physiological factors such as intestinal permeability, brain function, enteric nervous system, gastrointestinal motility and visceral pain, contributing to the patho-physiology of FGIDs[151]. However, further studies are needed, especially in children, to confirm the role of gut microbiota in IBS.
Food: Even though children have identified a large number of food items which exacerbates their symptoms only a few have been reported to be associated with IBS. IBS has been shown to be associated with fermentable oligo-, di- and monosaccharides carbohydrates and polyols (FODMAPs)[158]. However, the exact relationship between lactose and fructose mal-digestion and IBS is not clear[159]. Its relationship with fiber is rather controversial[160,161].
Genetic, epigenetic and environmental factors: Previous studies have reported that those with a family history of IBS or other bowel symptoms are more likely develop IBS[41,162]. Similarly, twin studies have suggested that there is a higher concordance of occurrence of IBS in monozygotic twins than in dizygotic twins[163]. The concordance rate of IBS in monozygotic twins was 17.2% while that was 8.4% in dizygotic twins[163]. However, if genetic factors play a major role in development of IBS, the concordance rate in monozygotic twins needs to be much higher. Therefore, it is possible that social and environmental factors also play an important role in development of IBS, in addition to the genetic predisposition[163]. This finding is further strengthened by other studies which reported that parents of children with FAPDs have higher tendency to develop similar illnesses[37,164].
A large number of genetic polymorphisms were considered to be associated with IBS. However, overall there is limited evidence of a genetic association[165]. The most frequently studied genetic associations are related to the serotonergic system, including serotonin transporter (SERT) gene polymorphisms[116,117]. MicroRNAs considered to play a role in the pathogenesis of IBS through regulating serotonin reuptake transport expression[166] and single-nucleotide polymorphisms rs56109847 led to reduce microRNA binding and overexpression of the target gene in intestinal cells increasing IBS-D risk[167].
Other gene polymorphisms involved in IBS include mitochondrial DNA polymorphism[168], alpha 2 receptor gene C-1291G polymorphism[169], cytokine gene polymorphisms (e.g., IL-10 and IL 12 C (-1188) A)[170,171] and tumor necrosing factor super family (TNFSF) 15 polymorphism[172-174].
However, identification of a single gene polymorphism in patient with IBS alone would not possibly explain the complex nature of this disease. It is known that epigenetic changes in the genome play a crucial role in pathogenesis of diseases. It is possible that environmental factors, psychological stresses, exposure to child maltreatments and some of the Patho-physiological mechanisms interact with each other in a very intricate manner to alter epigenetic DNA (by DNA methylation, histone modification) and changes in micro-RNA which can alter the gene expression (inhibition of increase transcription) to produce IBS phenotype. However, further evidence needs to be generated in this vital area of association between epigenetic changes and IBS[175].
IBS is a clinical diagnosis. Therefore, a thorough clinical evaluation is the most important part in the diagnosis. The process includes a detailed clinical history, including the past medical history, drug history, social and psychological histories. In addition, the physical examination generally should not reveal abnormalities that could indicate the possibility of an organic disorder. The clinical history is aimed at eliciting criteria laid down by the Rome committee[18]. Therefore, the main components of the clinical history should include details about abdominal pain, relieving and aggravating nature of the pain related to bowel motions and details about stool patterns. The symptoms need to be recurrent and should be at least four time per month for a minimum of 2-mo duration. The sub-type of IBS depends on the presence of a particular stool pattern. Presence of hard stools > 25% of the time with loose watery stools < 25% of the time helps to diagnose IBS-C whereas the opposite denotes the diagnosis of IBS-D. Alteration of stool pattern between diarrhea and constipation over a period of time suggests IBS-M whereas when the stool pattern is not like any of these, it leads to the diagnosis of IBS-U[18] (Table 1). In addition, children with IBS are suffering from a large number of somatic symptoms and psychological problems including maladjustment, depression and anxiety[10,46]. Eliciting these in the history would also help in the diagnosis and long term management of these children.
The diagnosis of IBS heavily depends on the nature of the stools and therefore the assessment of stool pattern is a crucial factor in the diagnosis. The current gold standard to assess the nature of the stools is the Bristol Stool Form Scale which was developed primarily using adult subjects (BSFS)[176]. Nonetheless, the consistency of the stools described by the BSFS correlated with the whole gut transit time in children[177]. More recently, Lane and colleague have developed a modified BSFS for children, which has only 5 stool types and that form has been shown to be reliable in children. Further evaluation of this scale, which looks more child friendly, is needed before using it to assess children[178].
However, the Rome criteria for children are not validated through a standard process as there is no gold standard to compare with. The diagnostic utility of Rome criteria to detect IBS and other FAPDs had a sensitivity of 0.35, specificity of 0.6, with negative and positive predictive values of 0.71 and 0.24 respectively[179]. In addition, the subtypes of IBS are known to change from one type to another over a period of time both in adults and children, questioning the validity of subtypes[12,180]. In addition, a significant percentage of children who fulfilled the Rome criteria for functional abdominal pain disorders were found to have organic pathologies on endoscopic examination of the upper gastrointestinal tract[179,181]. Therefore, further validation and refinement of Rome criteria may be needed to improve its diagnostic utility. Perhaps it is imperative to validate and calculate the likelihood ratios of each symptom of new Rome IV criteria to improve their clinical utility and that endeavor would be a challenge in the years to come.
Red flag features are a group of symptoms and signs that could indicate underlying organic pathology in children with IBS. The red flag features are an important concept as adult guidelines state that a safe diagnosis of IBS can be made using symptom based criteria in the absence of red flag features[182]. The Rome IV committee for childhood FGIDs has identified several features that should be considered as alarm features that indicate the potential of having organic diseases (Table 2)[18]. Clinicians are supposed to look for these features during the clinical evaluation mainly to rule out organic diseases such as inflammatory bowel disease and other disease entities that lead to malabsorption and growth failure. A study involving 606 patients (128 children with Crohn’s disease and 478 with abdominal pain) found presence of anemia, blood in stools and weight loss are most predictive of having Crohn’s disease[183]. Tam et al[184] studied 80 patients fulfilling Rome III criteria for FD. They consider several alarm features including gastrointestinal blood loss, dysphagia, and persistent vomiting. After thorough investigations, including upper gastro-intestinal endoscopies in all these children, the positive and negative predictive value of the presence of alarm symptoms to detect organic pathology were 0.33 and 0.97 respectively[184]. Several other studies have also been conducted to assess the validity of the presence of alarm features in detecting organic disorders in children with recurrent abdominal pain[179,184-186]. However, since these studies have used a variety of symptoms and signs as red flag features it is extremely difficult to develop a validated set of red flag features to use in the day-to-day clinical practice to differentiate organic disorders from IBS. However, it is very valuable to have a set of alarm features to guide the clinician to decide on especially the invasive investigations such as gastrointestinal endoscopies, transit studies and other intrusive radiological procedures. One of the greatest challenges that we have is to develop a correct set of red flag features that have reasonable validity. Once available, these clinical clues could be used as a screening tool to rule out organic disorders and strengthen the clinical diagnosis of IBS based on Rome symptom based criteria. This would undoubtedly minimize subjecting children to unnecessary and invasive investigations. It would be reasonable to use the following symptoms and signs as alarm features (Unintentional weight loss, significant lower gastrointestinal bleeding in the absence of an anal fissure, significant arthritis, any amount of upper gastrointestinal blood loss, persistent fever with abdominal pain, persistent diarrhea, family history of inflammatory bowel disease or celiac disease).
| Family history of inflammatory bowel disease, celiac disease or peptic ulcer disease |
| Persistent right upper or lower abdominal pain |
| Dysphagia |
| Odynophagia |
| Persistent vomiting |
| Gastrointestinal blood loss |
| Nocturnal diarrhea |
| Arthritis |
| Perirectal disease |
| Involuntary weight loss |
| Deceleration of linear growth |
| Delayed puberty |
| Unexplained fever |
It is generally considered that the diagnosis of IBS is solely dependent on fulfilling Rome criteria for children. The current concept is to make a clinical diagnosis using the latest Rome criteria and conduct a set of basic investigations to rule out common organic disorders. However, evidence is emerging that it is not solely a disease where there are no diagnostic biomarkers and thorough investigations would reveal significant pathologies in children who even fulfill Rome criteria for IBS. In this section we will discuss the important investigations that are useful in children with IBS.
Most clinicians order routine investigations including blood count, inflammatory markers, routine biochemistry, urine microscopy, Celiac screening and ultra-sonogram to evaluate children with features of IBS. In a retrospective study, Dhroove and co-workers noted the low yield of commonly conducted blood, urine and stool tests to distinguish organic disorders from FAPDs[187]. In addition, these tests incurred a large sum of money. However, it could also possible that Dhroove and colleagues have selected a well-defined set of patients who have no organic disorders and therefore essentially bound to have no abnormalities in the investigation panel. Furthermore, no studies have assessed the diagnostic utility of these tests in FAPD. Therefore, the value of basic laboratory investigations in the diagnosis of IBS remains questionable. Furthermore, the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHN) committee on chronic abdominal pain also does not recommend performing these investigations in children[188]. It is reassuring for the practicing clinicians to conduct a few basic tests to rule out possible organic diseases that could present with recurrent abdominal pain and strengthen the diagnosis of IBS. This is also an opportunity to convince demanding parents that there are no dangerous organic disorders in the child and at the same time not subjecting them to unnecessary invasive investigations. However, yet again it is a challenge to develop a set of investigations that could help the clinician and the family while not subjecting children to unnecessary invasive procedures as data on this important aspect is sparse. A prospective study selecting children from a broader base rather than fulfilling Rome criteria for IBS and investigating for potential organic diseases and the use of Rome criteria to define IBS would be a useful way of addressing this issue. It is essential to consider the regional differences in the organic pathologies in the different parts of the world when compiling this list of investigations.
Coeliac disease (CD) is a multisystem disease and the gastrointestinal symptoms are similar to IBS with diarrhea. It is well known that gluten is a potential precipitating factor in a subset of patients with IBS even when the serology is negative (non-coeliac gluten sensitivity). A meta-analysis of adult studies has clearly demonstrated that pooled odds ratio for positive IgA anti-gliadin antibodies, endomysial antibodies and/or anti-tissue transglutaminase antibodies, and biopsy-proven CD in IBS subjects against controls were 3.21 (95%CI: 1.55-6.65), 2.75 (95% CI 1.35-5.61), and 4.48 (95%CI: 2.33-8.60), respectively[189]. On par with those results, the Turkish Celiac Study Group has found a borderline significant association between IBS and CD[190]. Furthermore, a study from Iran reported a higher prevalence of CD in children with recurrent abdominal pain compared to the general population[191]. Therefore, it could be recommended to screen children with IBS for celiac disease in areas known to have a high prevalence of that disease. However, prevalence of CD is increasingly noted in other parts of the world. CD is increasingly identified outside the Western world. Prevalence of 1% in children attending a tertiary care hospital was reported from North India[192]. Therefore, screening children present with symptoms of IBS (especially with IBS-D) for celiac disease would be an important step towards early recognition of CD in the future.
Calprotectin is a calcium binding protein that accounts for 60% of the protein in the cytosol of human neutrophils. Elevated calprotectin in feces indicates ongoing neutrophil recruitment due to inflammation. Therefore, estimation of fecal calprotectin is increasingly used as a non-invasive screening for intestinal inflammation. Most pediatric gastroenterologists performed fecal calprotectin assay to rule out the possibility of inflammatory bowel disease (IBD). However, it should be noted that there is a variability of test results depending on the manufacturer[193]. A mild rise (< 50) or positivity of fecal calprotectin does not indicate the possibility of having IBD. It has been shown that children with IBD show a mean value of 349 μg/g whereas the majority of children with other diseases had a mean value of 16.5 μg/g[194]. Studying 126 children with pain predominant FGIDs, Flagstad and co-workers noted that the median calprotectin concentrations were at or lower than 16 mg/kg which was at the lower detection limit and there were no differences between the FGID subgroups. Nine children (7%) had slightly raised values[195]. All these results indicate the value of fecal calprotectin as a useful test in differentiating IBS from other inflammatory disorders presenting with a similar clinical picture.
Endoscopy in pediatric gastroenterology practice is considered as an invasive procedure as it needs general anesthesia. Therefore, convincing parents for their child with features suggestive of IBS to undergo an upper or lower gastrointestinal endoscopy is a challenge to a pediatric gastroenterologist. Previous researchers have found significant number of disease entities when they performed endoscopies in children with recurrent abdominal pain, IBS or FD. Two studies from the Western world have noted 30%-37% of children with chronic abdominal pain and FAPDs had organic pathology such as Helicobacter pylori infection, peptic ulcer disease, inflammatory bowel disease, celiac disease and eosinophilic gastroenteritis to explain their symptoms. In both these studies presence of alarm symptoms did not predict the possibility of an organic disorder[181,186]. However, others have reported very low yield from the endoscopy and they found a changing number of red flag features that could be present in children with organic disorders[184,196]. Obtaining a negative endoscopy in children with chronic abdominal pain including IBS does not improve the clinical outcome[197]. Therefore, it is challenging to decide whether a child with IBS needs routine endoscopy or not. A great deal of clinical competence is needed to decide on this matter rather than depending on individual research findings and guidelines. Disease entities such as celiac disease, peptic ulcer disease, food allergy, and inflammatory bowel disease, including microscopic colitis, could only be confirmed by endoscopic biopsies. Therefore, children with substantial evidence (growth faltering, blood stained stools, chronic diarrhea, hematemesis) suggestive of serious organic pathologies should undergo endoscopy despite fulfilling criteria for IBS. Most of these disorders present with chronic loose stools. Therefore, the clinician should have a lower threshold to perform endoscopies in children presenting with IBS-D when they have some concerns regarding the presence of an organic pathology.
Clinicians tend to order ultra-sonogram of abdomen to evaluate children with IBS. However, performing ultrasonography in the absence of clear cut jaundice, recurrent vomiting and significant urinary symptoms would not yield any added benefit in the search for another cause for abdominal pain in these children[198].
Motility studies would help in some instances where the diagnosis is not straight forward. Non-invasive ultra-sonographic evaluation of the gastric emptying and antral motility is useful in assessing children with IBS as it had been shown that children with IBS do have abnormal gastric emptying and antral motility[128]. Lower rectal sensory threshold for pain had been a prominent feature of children with IBS[99]. Furthermore, children IBS were found to have lower rectal sensory threshold for pain than controls and children with organic disease with abdominal pain[96]. Although not conducted in day-to-day practice, incorporating them into the positive diagnosis of IBS in cases where the diagnosis of IBS is not entirely clear would enhance the overall clinical care of these children. With the evolution of high resolution manometry in children it would be possible to detect novel abnormalities which could help in both understanding the patho-physiology and management.
An effective physician-parent-patient relationship is a major component of effective management of IBS. Management of IBS involves counselling and parental education, pharmacological and non-pharmacological therapies (Table 3).
| Counselling and explanation to parents/child |
| Control maternal response to child’s pain |
| Pharmacological interventions |
| Gastroprokinetics (domperidone) |
| Antidepressants (amitriptyline, citalopram) |
| Acid suppressing agents (famotidine, omeprazole) |
| Antispasmodics (peppermint oil, mebavarine, dotavarine) |
| Antihistamines (cyproheptadine) |
| Antibiotics (rifaximin) |
| Psychological interventions |
| Guided imagery |
| Gut directed hypnotherapy |
| Cognitive behavioral therapy |
| Yoga therapy |
| Neuromodulation |
| Low FODMAP diet |
| Probiotics |
Most parents are anxious to know what is the cause for the abdominal pain in their children. They are often worried about serious medical conditions including possibility of malignancies. Once evaluation is over it is imperative that the clinician explain the negative investigations means that the child does not have a serious organic disorder and is having IBS. At this stage the clinician also needs to explain that the functional nature of the disease using diagrams and illustrations. The relationship between the family and the clinician would not only yield a positive diagnosis but also a global improvement of symptoms[199].
Parental behavior often does not help in childhood FAPDs. The anxiety of the parents would reflect in symptom severity and negatively influence the treatment outcome in children[200]. In a randomized controlled trial Walker et al[201] have shown that parental attention increases the complaints of children with FAPDs. In fact, it is possible to reduce parental solicitous response by cognitive behavioral therapy[202]. It has been shown that on long term follow-up some of these children outgrow their symptoms only with reassurance and education[40]. In addition, it is also possible that the initial diagnosis may change into a different category[40].
Hence, the time invested in counseling and explanation is an important part in the management. The challenge is that most of the gastroenterology clinics are over burdened with children suffering from FGIDs and the counselling would be time consuming[203]. Preparation of educational material for them to refer in the form of booklets and materials in official web sites of the clinics, or forming patient groups under the guidance of the clinicians would be the way forward in the future. Therefore, spending time with explanation of the possibility of functional nature of the disorder will be a very effective method of managing children with FAPDs.
Although many clinicians rely on the pharmacological approach, the overall efficacy of pharmacological agents in IBS is low. Several systematic reviews have pointed out the lack of well-designed high quality clinical trials in this area and lack of therapeutic efficacy of these agents[204,205]. The other issue pertaining to the clinical trials in children with FAPDs is that almost all paediatric trials have lumped together all FAPDs rather than including one specific FAPD such as IBS or FD. One of the major challenges that has come out of this practice is the inability to focus on one disease entity at a time. The small numbers of patient could be overcome by multicentre studies.
Current pharmacological agents to treat children with FAPDs include motility agents, antidepressants, acid suppressing agents, antispasmodics, antihistamines, and anti reflux agents. Most of these studies have included children with IBS under the umbrella term of recurrent abdominal pain and sub-group analysis has not been carried out to highlight the efficacy of the given therapeutic agent for IBS alone. This may partly be due to lack of statistical significance when analyzed according to the disease entities. In the following section the pharmacological and psychological interventions for children with FAPDs will be discussed, highlighting the efficacy of the intervention specifically of IBS when the data are available.
However, it is very difficult to prioritize and recommend one agent over the other in the background of lack of clear evidence and the choice depends upon several factors including availability, cost and the preference of the clinician. The latest guideline from the NASPGHN also does not recommend one agent over the other[188].
Gastroprokinetics: Gastroprokinetics are known to augment gastric motility and improve symptoms especially in adults with FD[206]. One double blind randomized placebo controlled clinical trial has evaluated the clinical efficacy of domperidone in children with FAPDs. In this study a significant cure rates, improvement of the overall clinical condition and reduction in pain severity was noted in the intervention group. The subgroup analysis pointed out that children with FAP-NOS respond better than IBS and FD. However, the clinical improvement had no relationship to the improvement of gastric motility. Although there were concerns regarding cardiac arrhythmias, no adverse reactions were reported during the treatment period[207].
Antidepressants: The brain gut microbiota axis has been implicated in the pathogenesis of FAPDs[208]. It is also well known that various centers and networks in the brain such as salient network, central executive network and sensory motor network have a combined output through autonomic network and the HPA axis, altering motility, secretions and microbiota in IBS[78]. Modulating these mechanisms in order to relive symptoms, tricyclic antidepressants and selective serotonin reuptake inhibitors have been used in clinical trials. However, in one well designed trial, amitriptyline was not superior to the placebo in relieving symptoms in children[209]. Another study with lesser methodological rigor found a significant improvement in health related quality of life in the treatment group[210]. Although there is a theoretical possibility of cardiac arrhythmias, both studies noted no adverse events related to treatment. Similarly, serotonin reuptake inhibitor citalopram has not shown any therapeutic benefit in children with FAPDs[211]. These findings are surprising as studies among adult patients with IBS showed a clear benefit of antidepressants therapy[212].
Although, the evidence is still lacking it is possible to use these drugs in a situation where the child is having central symptoms such as anxiety and depression with abdominal pain. With available evidence, one of the future opportunities is to conduct a randomized trial using children with IBS alone.
Acid suppressing agents: Acid suppressing therapies are commonly used in children with FAPD, thinking that this is due to “gastritis” and suppressing acid in the stomach would reduce the symptoms. In an observational study of 290 children with chronic abdominal pain it was noted 2/3 of the patients were treated with proton pump inhibitors with a mean duration of 11 wk[181]. In other instances, simple H2 receptor blockers are used by the clinicians. However, the evidence for this practice is lacking. In a randomized trial, although famotidine was noted to be superior to placebo in global symptom improvement, the drug fails to reduce abdominal pain[213]. Recent literature concerning adverse effects of long term acid suppression shows significant increase in respiratory and gastrointestinal infections, hypomagnesaemia, vitamin B12 deficiency and increase pathological fractures. In addition, it is worth to remember that it is possible to have rebound hyperacidity after discontinuation of therapy[214]. Therefore, long term acid suppression should be discouraged in children with FAPDs without proven Helicobacter pylori infection. However, this poses a big challenge as a large proportion of practitioners are used to prescribe acid suppression therapy for abdominal pain for generations.
Antispasmodic agents: Antispsmodic agents are known to reduce smooth muscle spasms in the gastrointestinal tract and are thought to reduce symptoms of FAPDs. One such agent is peppermint oil. Studies in adults have shown beneficial effects of peppermint oil in treating patients with IBS[215]. Two trials have been conducted in children with FAPDs testing the therapeutic benefits of peppermint oil[216,217]. Both have methodological flaws and analysis even after combining both studies. The evidence is still insufficient to recommend peppermint oil for the treatment of FAPDs[218].
Mebevarine is an antispasmodic drug which has direct effect on gastrointestinal smooth muscles[219]. It’s efficacy in treating children with FAPDs was assessed in a randomized controlled trial. After 4 and 12 wk of treatment with mebevarine, the treatment group had no superior reduction of pain compared to the placebo group [220].
In another randomized controlled trial, the efficacy of dotavarine was evaluated using 132 children with recurrent abdominal pain. Although the drug reduced the abdominal pain episodes and reduced missed school days when compared to the placebo group, the number of pain-free days after treatment did not differ significantly between both groups[221].
A Cochrane review has clearly indicated the potential benefits of antispasmodic treatment in adult patients with IBS[161]. However, those drugs such as cimetropium, dicyclomine, pinaverum and trimebutine have not been used in clinical trials of children with IBS.
Antihistamines: Cyproheptadine is an antihistaminic agent that has been tested in a small double blind placebo controlled trial as a potential therapeutic modality for children with FAPDs but not specifically IBS alone. Although the authors reported a positive result on reduction of abdominal pain intensity and frequency, small sample size and non-validated assessment tools reduce the legitimacy of the data[222].
Antibiotics: Rifaximin is a semisynthetic poorly absorbed antimicrobial derivative of rifamycin. Rifaximin formulation contains an extra pyrido-imidazole ring to reduce systemic absorption that is less than 1% after oral administration. Rifaximin elicits its antimicrobial properties by binding to the beta-subunit of the bacterial DNA-dependent RNA polymerase and thus inhibiting bacterial RNA syn283 synthesis. It has been approved for the treatment of IBS-D in adults[204].
Two clinical trials have assessed the efficacy of rifaximin in children with FAPDs[223]. Both studies have used children with all FAPDs rather than IBS alone. It is surprising to observe this trend in both trials as the drug is only recommended in IBS-D in adults. One of the well-known trials in adults to assess the efficacy is the TARGET trial which has shown the efficacy of rifaximin in patients who do not have small intestinal bacterial overgrowth[224]. Both pediatric trials have used lactulose breath test to include children into these studies. Although small intestinal bacterial overgrowth (SIBO) is known to produce symptoms similar to IBS, it’s not known to be associated with FD or FAP. It was noted in the double blind placebo controlled trial that 2 wk of rifaximin was not effective in controlling abdominal pain in children[223]. It was surprising to note that 42% of children with positive lactulose breath test (LBT) had FD or IBS where SIBO had not been implicated in the patho-physiology. The other trial is an open label trial including 50 children with FAPDs (15% FD, 30% FAP and 55% IBS)[225]. All underwent LBT and children with positive LBT were treated with rifaximin for 7 d and others remained untreated. LBT became normal in 64% and they had significant improvement of their abdominal pain, bloating, and flatulence. Children who had abnormal LBT after treatment showed no improvement of symptoms. There was no subgroup analysis with regards to IBS in both trials.
Guided imagery: Guided imagery provides a state of engagement in imagery and relaxation[226]. It is considered as an effective intervention in children with pain[227] and could be delivered through an audio recording. In a pilot study comparing guided imagery with standard medical care to standard medical care alone, van Tilburg and co-workers showed that guided imagery is superior to standard medical care in children with FAPD. The results also found that treatment effects were sustained up to 6 mo[228]. Another study compared guided imagery with progressive muscle relaxation with simple breathing exercise. In this study children who received guided imagery with progressive muscle relaxation had greater reduction in the number of days with pain and days with missing activity. However, the follow-up data was available only for 2 mo[227]. Both studies indicate the possibility of using guided imagery as a potential therapeutic option for FAPDs.
Gut directed hypnotherapy: Abnormalities in the brain-gut axis have been implicated with the patho-physiology of FAPDs in children. In addition, abnormal motility in the gastrointestinal tract and the visceral hypersensitivity have also been considered as contributory factors[208]. Gut directed hypnotherapy is used to teach necessary hypnotic skills to control and normalize gut function through several steps[229]. The approach has shown a beneficial therapeutic effect on several studies conducted in adults with refractory IBS[230]. Vlieger and co-workers conducted a randomized trial comparing gut directed hypnotherapy with the standard medical care in children with IBS or functional abdominal pain. Compared to the standard medical care, hypnotherapy was superior in reducing pain scores. In addition, at one year follow up treatment success was noted in 85% of children received gut directed hypnotherapy and 25% of children received standard treatment indicating effectiveness of hypnotherapy in FAPDs[231]. The therapeutic response was sustained even after 4.8 years of follow up[231]. When compared, hypnotherapy delivered using a compact disc is not inferior to the hypnotherapy given by a trained therapist in reducing pain intensity and pain frequency scores at 8 wk, post treatment 6 and 12 mo in children with FAP or IBS. In the subgroup analysis, no indication was found for different treatment effects in children with IBS and FAP. However, the publication provided no direct statistical data on the efficacy of hypnotherapy on IBS alone[232].
Cognitive behavioral therapy (CBT): CBT aims to improve the child’s mental health and coping strategies, specifically in helping them to understand the onset and progress of their abdominal pain. It then offers the child a strategy to help manage it, along with anxiety management and behavioral techniques[233]. A recent Cochrane review has analyzed 10 interventional studies using CBT for chronic abdominal pain in children. In this analysis it was shown that all studies had parental involvement with the child although the number of sessions could vary. Methods they used are also diverse, including teaching of coping and distraction strategies, teaching of relaxation techniques, identification and change of negative pain related thoughts and modifying family responses to illness behavior[233]. When the data were pooled, CBT had a significant degree of success compared to controls in the short term (< 3 mo) follow up. However, the effect was not sustainable at 6 mo and one year. The analysis also found no evidence that CBT is effective on pain intensity scores after the intervention. Therefore, the data is not very supportive of using CBT in managing children with FAPDs. No data on efficacy of CBT on IBS were included in the analysis.
Yoga therapy: Yoga techniques involve a series of physical exercises, breathing techniques, combined with meditation methods aimed to reduce anxiety, improve body tone and increase feelings of wellbeing. When used as a treatment for FAPDs, yoga therapy is thought to improve altered function of the brain-gut-microbiota axis. Up to now, 3 clinical trials have assessed the efficacy of yoga therapy for children with FAPDs compared to controls using standard medical care or in a waiting list. According to a meta-analysis from the Cochrane group, the results show no advantage of yoga therapy on pain intensity, pain frequency and functional disability[233]. The review does not provide details of the efficacy of yoga therapy on IBS in children.
Neuromodulation: Neuromodulation uses a transcutaneous electrical stimulation to stimulate local skin nerve fibers and autonomic nervous system specifically, the efferent parasympathetic outflow to the gastrointestinal tract augmenting gastrointestinal function. There is evidence to prove that delayed gastric emptying and altered antral motility play a major patho-physiological role in IBS[128]. Kovacic et al[234] have tested this concept to treat FAPD in a clinical trial including 115 adolescents. Compared to the sham control group, adolescents who received electrical stimulation had improvement of pain after 3 wk of therapy. Therefore, although promising, it is difficult to recommend neuromodulation therapy for children with FAPDs without further studies. One of the limitations in this study, as in most of the other studies, is that they have not specifically assessed the efficacy of neromodulation on IBS.
Diet: Dietary components had been thought to be involved in the pathogenesis of FAPDs. Most parents tend to point out certain dietary items as sometimes the cause and sometimes the aggravating factor for FAPDs[235]. Studies in adults have shown diet containing fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) tends to alter intestinal function and microbiota and contribute to the pathogenesis of IBS[79]. Chumpitazi and co-workers have investigated the value of low FODMAP diet in treating children with IBS. In this randomized cross over trial, children were randomized to receive 48 h of either low FODMAP diet or typical American diet. The authors found that, compared to the baseline, children had fewer daily abdominal pain episodes during the low FODMAP diet and more while they were on a typical American diet[236]. Although the results are promising, it is necessary to know the long-term efficacy of the intervention, including potential effects on growth and nutrition of children, before recommending low FODMAP diet for childhood IBS.
Fiber: Fiber consumption is thought to be beneficial for intestinal health. There are 4 randomized trials assessing the benefit of different types of fiber supplements in children with FAPDs (e.g., psyllium, glucomannan)[237-240]. Fiber supplementation is believed to be helpful to soften stools, enhance colonic transit and improve fecal output[160,241]. Various measures were used to assess the outcome (Faces pain scale-revised, Birmingham IBS symptom questionnaire, Eong-Baker faces pain rating scale). When all 4 studies were pooled there was no significant difference between the fiber group and the placebo group in improvement of pain (OR = 1.83, 95%CI: 0.92-3.65) and pain intensity (SMD = -1.24, 95%CI: -3.41 to 0.94)[242].
Probiotics: Altered microbiome has been suggested as a potential patho-physiological mechanism of IBS. Reduction in bifidobacteria, lactobacilli and increased ratio of Fermicuticus: Bacteroid ration were noted in patients with IBS[78]. In addition, children with IBS were noted to have greater percentage of proteobacteria[152]. Therefore, probiotics (live microorganisms that improve the balance of intestinal microbiome) have been used in the treatment of FAPDs in children. Three studies have evaluated the efficacy of probiotics in children with IBS. The first study conducted by Bauserman and Michail included 50 children randomized to receive Lactobacillus GG or a placebo. After 6 wk of therapy the authors found no difference between the intervention and the placebo groups in relation to relieving abdominal pain or other gastrointestinal symptoms[243]. The other study that assessed the efficacy of Lactobacillus GG in 52 children (randomized to receive either LGG or placebo) noted a reduction in pain during the follow up period of 4 wk. No improvement in stool scale was noted during the study period[244]. In addition, it was also shown that LGG is effective in reducing frequency and intensity of pain in children with IBS compared to functional abdominal pain[245]. Guandalini et al[246] studied the utility of VSL 3# (probiotic mixture) in treating children with IBS in a double blind randomized cross-over trial. The results were encouraging and noted that VSL 3# could significantly relieve overall symptoms, reduce abdominal pain and bloating. However, no improvement was noted in stool patterns. Newlove-Delgado et al[242] conducted a systematic review and the meta-analysis of the value of probiotics in treating children with recurrent abdominal pain. In this meta-analysis, they conducted a subgroup analysis of the efficacy of probiotics in IBS and concluded that probiotics are effective in treating children with IBS [pooled OR of 3.01 (95%CI: 1.77-5.13; P < 0.001)], and the estimated number need to treat was four[242]. Therefore, probiotics can be recommended as a therapeutic modality for treating children with IBS. However, alteration of stool patterns (diarrhea, constipation) are equally disturbing to patients as well as abdominal pain. Therefore, it is imperative that the probiotic strains that could help in these aspects as well as abdominal pain should be used in future clinical trials. Developing a simple method available at the grass root level to identifying the microbial signature of children with IBS would be very useful as the clinicians can then individualize the probiotic treatment depending on the nature of the gut microbiome.
When consider the summarized evidence it is difficult to recommend one treatment over the other in treating children with FAPDs. It is mainly due to the small number of studies that have been conducted on most of the therapeutic modalities. Available guideline from the North American and European societies of Pediatric Gastroenterology Hepatology and Nutrition for managing children with chronic abdominal pain also does not recommend a clear pathway for using these therapeutic options[188].
However, it is possible to draw some tentative conclusions considering the available evidence. It is very clear that the long term use of acid suppressing agents could cause more harm than benefits and therefore, should be avoided in treating FAPDs. Similarly, encouraging an increase in the fiber content in the diet over the recommended amount (age in years + 5 in grams) is not helpful in the management of these children.
IBS in children is a disease with substantial burden on healthcare systems and the economy. The cost of evaluation and in-patient care of children with IBS was rising from 1997 to 2009 in the United States (from USD 5278 to 18853)[15]. The estimated annual cost of caring for children with FAP/IBS in the European union is likely to be over 15 billion euros[16]. It has also been shown that parental productivity loss accounts for at least 22% of this cost. In addition, IBS also negatively affects the health related quality of life (HRQoL) of children. Several studies have shown the poor HRQoL in children with IBS[9,14,247]. Sagawa et al[13] have clearly illustrated the negative effect of IBS on the quality of school life in children. In addition, the current therapeutic armory is not adequate as most of the treatment for IBS in children are not evidence based. Therefore, it is of paramount importance to plan a preventive strategy to overcome the current challenges.
It has been shown that other functional gastrointestinal disorders such as infantile colic is preventable by prescribing prophylactic probiotic strains to patients who are vulnerable to develop it[248]. In addition, oral administration of Lactobacillus GG to neonatal rats following exposure to intracolonic chemical irritant did not develop visceral hyperalgesia later in the life and less biogenic amines and neurotransmitters involved in pain modulation[249]. Very similarly future research should aim to prevent development of IBS and other similar pain related FGIDs in vulnerable groups such as neonates exposed to interventions by using prophylactic therapeutic interventions.
It is known that exposure to abuse and other adverse life events predispose children to develop IBS and the severity of symptoms are related to the exposure[46]. Studies among adults have plainly illustrated that childhood exposure to abuse increase vulnerability to develop IBS in adults as well[250]. Preventive strategies implemented effectively with education about child protection and law enforcement against child maltreatment would be effective in preventing children being exposed to child abuse. When exposed, proper and prompt rehabilitation of these children will also be helpful in preventing development of IBS. Psychological stress is a key driving force in IBS. It is well known that exposure to stressful home or school related stressful life events predispose children to develop FGIDs including IBS[7]. Therefore, minimizing school related stress by more child friendly curricula and providing diverse educational opportunities for children would be an investment for the future. In addition, educating parents to minimize home related stresses such as alcoholism, frequent punishments etc., which would predispose children to develop IBS and related disorders would be another preventive step.
Exposure to gastrointestinal infection is another well known etiological factor especially in IBS[55]. Ensuring safe water, immunization against gastrointestinal infections and prompt treatment for infective diarrhea to minimize gastrointestinal inflammation need to be ensured across the communities where infections are common.
Attempts at prevention of IBS is a challenge and a future opportunity to reduce the disease burden and minimize the wastage of large sums of public funds. It has been shown that a significant proportion of adults with IBS had childhood chronic abdominal pain and possibly IBS[251]. Therefore, the attempt to prevent FAPDs including IBS in childhood possibly have a compound effect to minimize economic burden of adults with IBS as well.
Epidemiology of pediatric IBS is well researched, but little is known of its patho-physiology and management. Most of the available evidence in this area is based on results of adult studies and how much these finding can be applied to childhood IBS is not clear.
When it comes to IBS, applying the symptom based diagnostic criteria have become a challenge due to differences in interpretation of them between different regions in the world and different cultures. There are some attempts taken to understand cross cultural differences in reporting gastrointestinal symptoms and to overcome this problem.
Patho-physiology is another main grey area in childhood IBS. Even though a lot of mechanisms have been suggested, their exact role in generation of symptoms is not clear. Most of the proposed patho-physiological mechanisms are heavily based on assumed theories rather than exact scientific evidence.
Up to now, almost all researchers and research groups have worked in isolation focusing on a single patho-physiological mechanism that could lead to IBS. However, the multi-factorial nature of IBS cannot be described using a single patho-physiological mechanism. It is quite possible that multiple mechanisms involved in the pathogenesis of IBS in a given child, and these mechanisms are likely to be different from another depending on the sociocultural, genetic and epigenetic factors. Therefore, a multi-professional collaborative research involving researchers and clinicians who have expertise in molecular and cell biology, organ physiology, genetic and epigenetic mechanisms, gastrointestinal motility, modern culture independent microbiological techniques, and cutting edge neurosciences is the only way to solve the enigma of the patho-physiology of IBS in children. The proposed top-down and bottom-up models[77] have laid the foundation for this integrated approach to study and understand the patho-physiology of childhood IBS.
It is difficult to overcome the therapeutic demand of childhood IBS using the same conventional therapeutic agents that had been used during the past decades. Most of these agents are not very promising in the current evidence-based era. There are a number of novel agents that pediatric researchers could use by learning from adult counterparts. Some of these agents are already approved by the drug regulatory authorities for adults. Therefore, using well characterized patients diagnosed based on current Rome IV criteria, the efficacy of the agents such as elobaxibat, lubiprostone, linaclotide, 5-HT 3 receptor antagonists such as alosetron and ondansetron need to be tested for treating children with IBS.
As mentioned earlier the patho-physiology IBS is multifactorial[78,79]. It is believed that more than one patho-physiological mechanism might be operating in generating symptoms in one patient. Most of the drugs that are used in children have tried to address one patho-physiological mechanism in the belief that correction of one such mechanism would alleviate symptoms in a given patient. This approach is probably not the best way of dealing with a child with IBS in real life.
The main feature of children with IBS is pain in the abdomen. Therefore, it is essential to use a pain reliever initially. Depending on the type of pain the clinician could use a smooth muscle relaxant or a gastroprokinetic. In addition, if a child with IBS is having a lot of psychological disturbances including anxiety and somatization with constipation it is better to treat this child with a centrally acting management option (amitriptyline, gut directed hypnotherapy or cognitive behavioral therapy) with a laxative (polyethylene glycol, linocletide, lubiproston) to relieve symptom of constipation. Similarly, if the child is suffering from diarrhea predominant IBS one can approach with a probiotic or rifaximin to restore the gut flora. However, we need to generate evidence through well conducted focused studies using children with IBS alone.
In the recent past, more and more possible predisposing factors are recognized for IBS, including gastrointestinal infections, asthma and allergy, dietary factors and genetic and epigenetic factors. Therefore, the time has come to start focusing on prevention strategies targeting those patients with a high risk of developing IBS, in addition to management of affected individuals.
IBS is a common FGID among children around the world. A large number of children are suffering because of intestinal and extra-intestinal symptoms of IBS. However, little is known of its exact patho-physiology and management. Novel research using advanced technologies based on proposed top-down and bottom-up models of patho-physiology and treatment trials focusing on multiple combined interventions are likely to be more beneficial in understating and treating paediatric IBS. Many risk factors have been recognised for IBS. Therefore, the time has come to explore possible prevention strategies for this problem.
We acknowledge Dr. Perera BJC, Editor, Sri Lanka Journal of Child Health for language editing of this article and Dr. Anton Fernando for creating Figure 1.
| 1. | Dong L, Dingguo L, Xiaoxing X, Hanming L. An epidemiologic study of irritable bowel syndrome in adolescents and children in China: a school-based study. Pediatrics. 2005;116:e393-e396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Adeniyi OF, Adenike Lesi O, Olatona FA, Esezobor CI, Ikobah JM. Irritable bowel syndrome in adolescents in Lagos. Pan Afr Med J. 2017;28:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 3. | Karabulut GS, Beşer OF, Erginöz E, Kutlu T, Cokuğraş FÇ, Erkan T. The Incidence of Irritable Bowel Syndrome in Children Using the Rome III Criteria and the Effect of Trimebutine Treatment. J Neurogastroenterol Motil. 2013;19:90-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Lu PL, Velasco-Benítez CA, Saps M. Sex, Age, and Prevalence of Pediatric Irritable Bowel Syndrome and Constipation in Colombia: A Population-based Study. J Pediatr Gastroenterol Nutr. 2017;64:e137-e141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Korterink JJ, Diederen K, Benninga MA, Tabbers MM. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One. 2015;10:e0126982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 240] [Cited by in RCA: 321] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 6. | Devanarayana NM, Adhikari C, Pannala W, Rajindrajith S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J Trop Pediatr. 2011;57:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | Devanarayana NM, Mettananda S, Liyanarachchi C, Nanayakkara N, Mendis N, Perera N, Rajindrajith S. Abdominal pain-predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J Pediatr Gastroenterol Nutr. 2011;53:659-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Udoh E, Devanarayana NM, Rajindrajith S, Meremikwu M, Benninga MA. Abdominal Pain-predominant Functional Gastrointestinal Disorders in Adolescent Nigerians. J Pediatr Gastroenterol Nutr. 2016;62:588-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Devanarayana NM, Rajindrajith S, Benninga MA. Quality of life and health care consultation in 13 to 18 year olds with abdominal pain predominant functional gastrointestinal diseases. BMC Gastroenterol. 2014;14:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Ranasinghe N, Devanarayana NM, Rajindrajith S, Perera MS, Nishanthinie S, Warnakulasuriya T, de Zoysa PT. Functional gastrointestinal diseases and psychological maladjustment, personality traits and quality of life. BMC Gastroenterol. 2018;18:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 11. | Rajindrajith S, Devanarayana NM. Subtypes and Symptomatology of Irritable Bowel Syndrome in Children and Adolescents: A School-based Survey Using Rome III Criteria. J Neurogastroenterol Motil. 2012;18:298-304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (2)] |
| 12. | Giannetti E, de’Angelis G, Turco R, Campanozzi A, Pensabene L, Salvatore S, de Seta F, Staiano A. Subtypes of irritable bowel syndrome in children: prevalence at diagnosis and at follow-up. J Pediatr. 2014;164:1099-1103.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Sagawa T, Okamura S, Kakizaki S, Zhang Y, Morita K, Mori M. Functional gastrointestinal disorders in adolescents and quality of school life. J Gastroenterol Hepatol. 2013;28:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Varni JW, Lane MM, Burwinkle TM, Fontaine EN, Youssef NN, Schwimmer JB, Pardee PE, Pohl JF, Easley DJ. Health-related quality of life in pediatric patients with irritable bowel syndrome: a comparative analysis. J Dev Behav Pediatr. 2006;27:451-458. [PubMed] |
| 15. | Park R, Mikami S, LeClair J, Bollom A, Lembo C, Sethi S, Lembo A, Jones M, Cheng V, Friedlander E. Inpatient burden of childhood functional GI disorders in the USA: an analysis of national trends in the USA from 1997 to 2009. Neurogastroenterol Motil. 2015;27:684-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Hoekman DR, Rutten JM, Vlieger AM, Benninga MA, Dijkgraaf MG. Annual Costs of Care for Pediatric Irritable Bowel Syndrome, Functional Abdominal Pain, and Functional Abdominal Pain Syndrome. J Pediatr. 2015;167:1103-8.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 17. | Lane MM, Weidler EM, Czyzewski DI, Shulman RJ. Pain symptoms and stooling patterns do not drive diagnostic costs for children with functional abdominal pain and irritable bowel syndrome in primary or tertiary care. Pediatrics. 2009;123:758-764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Functional Disorders: Children and Adolescents. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 809] [Cited by in RCA: 861] [Article Influence: 86.1] [Reference Citation Analysis (5)] |
| 19. | Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, Staiano A. Childhood functional gastrointestinal disorders. Gut. 1999;45 Suppl 2:II60-II68. [PubMed] |
| 20. | Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, Walker LS. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130:1527-1537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1150] [Cited by in RCA: 1089] [Article Influence: 54.5] [Reference Citation Analysis (7)] |
| 21. | Saps M, Di Lorenzo C. Interobserver and intraobserver reliability of the Rome II criteria in children. Am J Gastroenterol. 2005;100:2079-2082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Chogle A, Dhroove G, Sztainberg M, Di Lorenzo C, Saps M. How reliable are the Rome III criteria for the assessment of functional gastrointestinal disorders in children? Am J Gastroenterol. 2010;105:2697-2701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Oświęcimska J, Szymlak A, Roczniak W, Girczys-Połedniok K, Kwiecień J. New insights into the pathogenesis and treatment of irritable bowel syndrome. Adv Med Sci. 2017;62:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 24. | Sandhu BK, Paul SP. Irritable bowel syndrome in children: pathogenesis, diagnosis and evidence-based treatment. World J Gastroenterol. 2014;20:6013-6023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child. 1958;33:165-170. [PubMed] |
| 26. | Hyams JS, Burke G, Davis PM, Rzepski B, Andrulonis PA. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996;129:220-226. [PubMed] |
| 27. | Walker LS, Lipani TA, Greene JW, Caines K, Stutts J, Polk DB, Caplan A, Rasquin-Weber A. Recurrent abdominal pain: symptom subtypes based on the Rome II Criteria for pediatric functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2004;38:187-191. [PubMed] |
| 28. | Schurman JV, Friesen CA, Danda CE, Andre L, Welchert E, Lavenbarg T, Cocjin JT, Hyman PE. Diagnosing functional abdominal pain with the Rome II criteria: parent, child, and clinician agreement. J Pediatr Gastroenterol Nutr. 2005;41:291-295. [PubMed] |
| 29. | Helgeland H, Flagstad G, Grøtta J, Vandvik PO, Kristensen H, Markestad T. Diagnosing pediatric functional abdominal pain in children (4-15 years old) according to the Rome III Criteria: results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr. 2009;49:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 30. | Devanarayana NM, de Silva DG, de Silva HJ. Aetiology of recurrent abdominal pain in a cohort of Sri Lankan children. J Paediatr Child Health. 2008;44:195-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1781] [Cited by in RCA: 2029] [Article Influence: 202.9] [Reference Citation Analysis (4)] |
| 32. | Devanarayana NM, Rajindrajith S, Pathmeswaran A, Abegunasekara C, Gunawardena NK, Benninga MA. Epidemiology of irritable bowel syndrome in children and adolescents in Asia. J Pediatr Gastroenterol Nutr. 2015;60:792-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 33. | Bouzios I, Chouliaras G, Chrousos GP, Roma E, Gemou-Engesaeth V. Functional gastrointestinal disorders in Greek Children based on ROME III criteria: identifying the child at risk. Neurogastroenterol Motil. 2017;29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 34. | Dhroove G, Saps M, Garcia-Bueno C, Leyva Jiménez A, Rodriguez-Reynosa LL, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Mexican schoolchildren. Rev Gastroenterol Mex. 2017;82:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Lu PL, Saps M, Chanis RA, Velasco-Benítez CA. The prevalence of functional gastrointestinal disorders in children in Panama: a school-based study. Acta Paediatr. 2016;105:e232-e236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 36. | Zablah R, Velasco-Benítez CA, Merlos I, Bonilla S, Saps M. Prevalence of functional gastrointestinal disorders in school-aged children in El Salvador. Rev Gastroenterol Mex. 2015;80:186-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 37. | Lewis ML, Palsson OS, Whitehead WE, van Tilburg MAL. Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. J Pediatr. 2016;177:39-43.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 182] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 38. | Robin SG, Keller C, Zwiener R, Hyman PE, Nurko S, Saps M, Di Lorenzo C, Shulman RJ, Hyams JS, Palsson O. Prevalence of Pediatric Functional Gastrointestinal Disorders Utilizing the Rome IV Criteria. J Pediatr. 2018;195:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 232] [Article Influence: 29.0] [Reference Citation Analysis (1)] |
| 39. | Scarpato E, Kolacek S, Jojkic-Pavkov D, Konjik V, Živković N, Roman E, Kostovski A, Zdraveska N, Altamimi E, Papadopoulou A. Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents in the Mediterranean Region of Europe. Clin Gastroenterol Hepatol. 2017; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 40. | Giannetti E, Maglione M, Sciorio E, Coppola V, Miele E, Staiano A. Do Children Just Grow Out of Irritable Bowel Syndrome? J Pediatr. 2017;183:122-126.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Zhu X, Chen W, Zhu X, Shen Y. A cross-sectional study of risk factors for irritable bowel syndrome in children 8-13 years of age in suzhou, china. Gastroenterol Res Pract. 2014;2014:198461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6 Suppl 2:152-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 43. | Chumpitazi BP, Weidler EM, Czyzewski DI, Self MM, Heitkemper M, Shulman RJ. Childhood Irritable Bowel Syndrome Characteristics Are Related to Both Sex and Pubertal Development. J Pediatr. 2017;180:141-147.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Endo Y, Shoji T, Fukudo S, Machida T, Machida T, Noda S, Hongo M. The features of adolescent irritable bowel syndrome in Japan. J Gastroenterol Hepatol. 2011;26 Suppl 3:106-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 45. | Song SW, Park SJ, Kim SH, Kang SG. Relationship between irritable bowel syndrome, worry and stress in adolescent girls. J Korean Med Sci. 2012;27:1398-1404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 46. | Devanarayana NM, Rajindrajith S, Perera MS, Nishanthanie SW, Karunanayake A, Benninga MA. Association between functional gastrointestinal diseases and exposure to abuse in teenagers. J Trop Pediatr. 2014;60:386-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 47. | Drossman DA. Abuse, trauma, and GI illness: is there a link? Am J Gastroenterol. 2011;106:14-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 48. | Anand KJ, Runeson B, Jacobson B. Gastric suction at birth associated with long-term risk for functional intestinal disorders in later life. J Pediatr. 2004;144:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 94] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 49. | Karunanayake A, Devanarayana NM, Rajindrajith S. Impact of early life events (ELE) and family dynamics for development of abdominal apin predominant functional gastrointestinal disorders (AP-FGIDs) in 5-12 age group. J Neurogastroenterol Motil. 2017;23:262. |
| 50. | Rosen JM, Adams PN, Saps M. Umbilical hernia repair increases the rate of functional gastrointestinal disorders in children. J Pediatr. 2013;163:1065-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Saps M, Bonilla S. Early life events: infants with pyloric stenosis have a higher risk of developing chronic abdominal pain in childhood. J Pediatr. 2011;159:551-4.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 52. | Saps M, Dhroove G, Chogle A. Henoch-Schonlein purpura leads to functional gastrointestinal disorders. Dig Dis Sci. 2011;56:1789-1793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 53. | Saps M, Lu P, Bonilla S. Cow’s-milk allergy is a risk factor for the development of FGIDs in children. J Pediatr Gastroenterol Nutr. 2011;52:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 54. | Schwille-Kiuntke J, Enck P, Zendler C, Krieg M, Polster AV, Klosterhalfen S, Autenrieth IB, Zipfel S, Frick JS. Postinfectious irritable bowel syndrome: follow-up of a patient cohort of confirmed cases of bacterial infection with Salmonella or Campylobacter. Neurogastroenterol Motil. 2011;23:e479-e488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 55. | Thabane M, Simunovic M, Akhtar-Danesh N, Garg AX, Clark WF, Collins SM, Salvadori M, Marshall JK. An outbreak of acute bacterial gastroenteritis is associated with an increased incidence of irritable bowel syndrome in children. Am J Gastroenterol. 2010;105:933-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 56. | Halvorson HA, Schlett CD, Riddle MS. Postinfectious irritable bowel syndrome--a meta-analysis. Am J Gastroenterol. 2006;101:1894-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 239] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 57. | Thabane M, Kottachchi DT, Marshall JK. Systematic review and meta-analysis: The incidence and prognosis of post-infectious irritable bowel syndrome. Aliment Pharmacol Ther. 2007;26:535-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 316] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 58. | Rodríguez LA, Ruigómez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ. 1999;318:565-566. [PubMed] |
| 59. | Marshall JK, Thabane M, Borgaonkar MR, James C. Postinfectious irritable bowel syndrome after a food-borne outbreak of acute gastroenteritis attributed to a viral pathogen. Clin Gastroenterol Hepatol. 2007;5:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 164] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 60. | Amra B, Hoseini-Asl MK, Rahmani AR, Golshan M, Mohamad-Zadeh Z. Correlation between asthma and irritable bowel syndrome in a general population in Iran in 2003. Respir Med. 2006;100:110-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 61. | Ekici A, Guliter S, Ekici M, Kalpaklioglu F, Kara T, Keles H, Tunckol M, Akin A, Kocyigit P. Irritable bowel syndrome in young and elderly patients with stable asthma. Dig Liver Dis. 2005;37:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 62. | Ozol D, Uz E, Bozalan R, Türkay C, Yildirim Z. Relationship between asthma and irritable bowel syndrome: role of food allergy. J Asthma. 2006;43:773-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Shen TC, Lin CL, Wei CC, Chen CH, Tu CY, Hsia TC, Shih CM, Hsu WH, Sung FC, Kao CH. Bidirectional Association between Asthma and Irritable Bowel Syndrome: Two Population-Based Retrospective Cohort Studies. PLoS One. 2016;11:e0153911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 64. | Yilmaz A, Cumurcu BE, Tasliyurt T, Sahan AG, Ustun Y, Etikan I. Role of psychiatric disorders and irritable bowel syndrome in asthma patients. Clinics (Sao Paulo). 2011;66:591-597. [PubMed] |
| 65. | Panicker R, Arifhodzic N, Al Ahmad M, Ali SA. Association and symptom characteristics of irritable bowel syndrome among bronchial asthma patients in Kuwait. Ann Thorac Med. 2010;5:37-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 66. | Tan TK, Chen AC, Lin CL, Shen TC, Li TC, Wei CC. Preschoolers With Allergic Diseases Have an Increased Risk of Irritable Bowel Syndrome When Reaching School Age. J Pediatr Gastroenterol Nutr. 2017;64:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 67. | Siddiqui S, Misra SP, Dwivedi M, Pant S. Irritable Bowel Syndrome and Bronchial Asthma: Are They Associated in Indian Population? J Clin Diagn Res. 2017;11:OC21-OC23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 68. | Simrén M, Månsson A, Langkilde AM, Svedlund J, Abrahamsson H, Bengtsson U, Björnsson ES. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 376] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 69. | Hayes P, Corish C, O’Mahony E, Quigley EM. A dietary survey of patients with irritable bowel syndrome. J Hum Nutr Diet. 2014;27 Suppl 2:36-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 70. | Khayyatzadeh SS, Kazemi-Bajestani SMR, Mirmousavi SJ, Heshmati M, Khoshmohabbat S, Ferns GA, Ghayour-Mobarhan M. Dietary behaviors in relation to prevalence of irritable bowel syndrome in adolescent girls. J Gastroenterol Hepatol. 2018;33:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 71. | Mansueto P, D’Alcamo A, Seidita A, Carroccio A. Food allergy in irritable bowel syndrome: The case of non-celiac wheat sensitivity. World J Gastroenterol. 2015;21:7089-7109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 42] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 72. | Monsbakken KW, Vandvik PO, Farup PG. Perceived food intolerance in subjects with irritable bowel syndrome-- etiology, prevalence and consequences. Eur J Clin Nutr. 2006;60:667-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 257] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 73. | Ostgaard H, Hausken T, Gundersen D, El-Salhy M. Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep. 2012;5:1382-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 74. | Howell S, Talley NJ, Quine S, Poulton R. The irritable bowel syndrome has origins in the childhood socioeconomic environment. Am J Gastroenterol. 2004;99:1572-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 75. | Chelimsky G, Boyle JT, Tusing L, Chelimsky TC. Autonomic abnormalities in children with functional abdominal pain: coincidence or etiology? J Pediatr Gastroenterol Nutr. 2001;33:47-53. [PubMed] |
| 76. | Karantanos T, Markoutsaki T, Gazouli M, Anagnou NP, Karamanolis DG. Current insights in to the pathophysiology of Irritable Bowel Syndrome. Gut Pathog. 2010;2:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 77. | Stasi C, Rosselli M, Bellini M, Laffi G, Milani S. Altered neuro-endocrine-immune pathways in the irritable bowel syndrome: the top-down and the bottom-up model. J Gastroenterol. 2012;47:1177-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 78. | Mayer EA, Labus JS, Tillisch K, Cole SW, Baldi P. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol. 2015;12:592-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 203] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 79. | Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2016;1:133-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 400] [Article Influence: 40.0] [Reference Citation Analysis (1)] |
| 80. | Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annu Rev Med. 2011;62:381-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 351] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 81. | Gaman A, Kuo B. Neuromodulatory processes of the brain-gut axis. Neuromodulation. 2008;11:249-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 82. | Tougas G. The autonomic nervous system in functional bowel disorders. Gut. 2000;47 Suppl 4:iv78-80; discussion iv87. [PubMed] |
| 83. | Elsenbruch S, Orr WC. Diarrhea- and constipation-predominant IBS patients differ in postprandial autonomic and cortisol responses. Am J Gastroenterol. 2001;96:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 84. | Aggarwal A, Cutts TF, Abell TL, Cardoso S, Familoni B, Bremer J, Karas J. Predominant symptoms in irritable bowel syndrome correlate with specific autonomic nervous system abnormalities. Gastroenterology. 1994;106:945-950. [PubMed] |
| 85. | Manabe N, Tanaka T, Hata J, Kusunoki H, Haruma K. Pathophysiology underlying irritable bowel syndrome--from the viewpoint of dysfunction of autonomic nervous system activity. J Smooth Muscle Res. 2009;45:15-23. [PubMed] |
| 86. | Spetalen S, Sandvik L, Blomhoff S, Jacobsen MB. Autonomic function at rest and in response to emotional and rectal stimuli in women with irritable bowel syndrome. Dig Dis Sci. 2008;53:1652-1659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 87. | Labus JS, Hubbard CS, Bueller J, Ebrat B, Tillisch K, Chen M, Stains J, Dukes GE, Kelleher DL, Naliboff BD. Impaired emotional learning and involvement of the corticotropin-releasing factor signaling system in patients with irritable bowel syndrome. Gastroenterology. 2013;145:1253-61.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (9)] |
| 88. | Chen J, Evans AN, Liu Y, Honda M, Saavedra JM, Aguilera G. Maternal deprivation in rats is associated with corticotrophin-releasing hormone (CRH) promoter hypomethylation and enhances CRH transcriptional responses to stress in adulthood. J Neuroendocrinol. 2012;24:1055-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 89. | Kiefte-de Jong JC, Saridjan NS, Escher JC, Jaddoe VW, Hofman A, Tiemeier H, Moll HA. Cortisol diurnal rhythm and stress reactivity in constipation and abdominal pain: the Generation R Study. J Pediatr Gastroenterol Nutr. 2011;53:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 90. | Vicario M, Alonso C, Guilarte M, Serra J, Martínez C, González-Castro AM, Lobo B, Antolín M, Andreu AL, García-Arumí E. Chronic psychosocial stress induces reversible mitochondrial damage and corticotropin-releasing factor receptor type-1 upregulation in the rat intestine and IBS-like gut dysfunction. Psychoneuroendocrinology. 2012;37:65-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (3)] |
| 91. | Taché Y, Mönnikes H, Bonaz B, Rivier J. Role of CRF in stress-related alterations of gastric and colonic motor function. Ann N Y Acad Sci. 1993;697:233-243. [PubMed] |
| 92. | Nozu T, Kumei S, Miyagishi S, Takakusaki K, Okumura T. Colorectal distention induces acute and delayed visceral hypersensitivity: role of peripheral corticotropin-releasing factor and interleukin-1 in rats. J Gastroenterol. 2015;50:1153-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 93. | Nozu T, Okumura T. Corticotropin-releasing factor receptor type 1 and type 2 interaction in irritable bowel syndrome. J Gastroenterol. 2015;50:819-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 94. | Camilleri M. Testing the sensitivity hypothesis in practice: tools and methods, assumptions and pitfalls. Gut. 2002;51 Suppl 1:i34-i40. [PubMed] |
| 95. | Farzaei MH, Bahramsoltani R, Abdollahi M, Rahimi R. The Role of Visceral Hypersensitivity in Irritable Bowel Syndrome: Pharmacological Targets and Novel Treatments. J Neurogastroenterol Motil. 2016;22:558-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 96. | Halac U, Noble A, Faure C. Rectal sensory threshold for pain is a diagnostic marker of irritable bowel syndrome and functional abdominal pain in children. J Pediatr. 2010;156:60-65.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 97. | Faure C, Wieckowska A. Somatic referral of visceral sensations and rectal sensory threshold for pain in children with functional gastrointestinal disorders. J Pediatr. 2007;150:66-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 98. | Miranda A. Early life events and the development of visceral hyperalgesia. J Pediatr Gastroenterol Nutr. 2008;47:682-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 99. | Van Ginkel R, Voskuijl WP, Benninga MA, Taminiau JA, Boeckxstaens GE. Alterations in rectal sensitivity and motility in childhood irritable bowel syndrome. Gastroenterology. 2001;120:31-38. [PubMed] |
| 100. | Di Lorenzo C, Youssef NN, Sigurdsson L, Scharff L, Griffiths J, Wald A. Visceral hyperalgesia in children with functional abdominal pain. J Pediatr. 2001;139:838-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 156] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 101. | Bouin M, Plourde V, Boivin M, Riberdy M, Lupien F, Laganière M, Verrier P, Poitras P. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology. 2002;122:1771-1777. [PubMed] |
| 102. | Lee H, Park JH, Park DI, Kim HJ, Cho YK, Sohn CI, Jeon WK, Kim BI, Chae SW. Mucosal mast cell count is associated with intestinal permeability in patients with diarrhea predominant irritable bowel syndrome. J Neurogastroenterol Motil. 2013;19:244-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 103. | Spiller R, Lam C. An Update on Post-infectious Irritable Bowel Syndrome: Role of Genetics, Immune Activation, Serotonin and Altered Microbiome. J Neurogastroenterol Motil. 2012;18:258-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 104. | Boeckxstaens G, Camilleri M, Sifrim D, Houghton LA, Elsenbruch S, Lindberg G, Azpiroz F, Parkman HP. Fundamentals of Neurogastroenterology: Physiology/Motility - Sensation. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 105. | Vanner S, Greenwood-Van Meerveld B, Mawe G, Shea-Donohue T, Verdu EF, Wood J, Grundy D. Fundamentals of Neurogastroenterology: Basic Science. Gastroenterology. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 106. | Barbara G, Wang B, Stanghellini V, de Giorgio R, Cremon C, Di Nardo G, Trevisani M, Campi B, Geppetti P, Tonini M. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132:26-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 610] [Cited by in RCA: 597] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 107. | Piché M, Bouin M, Arsenault M, Poitras P, Rainville P. Decreased pain inhibition in irritable bowel syndrome depends on altered descending modulation and higher-order brain processes. Neuroscience. 2011;195:166-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 108. | Williams AE, Heitkemper M, Self MM, Czyzewski DI, Shulman RJ. Endogenous inhibition of somatic pain is impaired in girls with irritable bowel syndrome compared with healthy girls. J Pain. 2013;14:921-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 109. | Yuan YZ, Tao RJ, Xu B, Sun J, Chen KM, Miao F, Zhang ZW, Xu JY. Functional brain imaging in irritable bowel syndrome with rectal balloon-distention by using fMRI. World J Gastroenterol. 2003;9:1356-1360. [PubMed] |
| 110. | Enck P, Aziz Q, Barbara G, Farmer AD, Fukudo S, Mayer EA, Niesler B, Quigley EM, Rajilić-Stojanović M, Schemann M. Irritable bowel syndrome. Nat Rev Dis Primers. 2016;2:16014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 692] [Article Influence: 69.2] [Reference Citation Analysis (1)] |
| 111. | Gershon MD, Tack J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology. 2007;132:397-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 988] [Cited by in RCA: 1162] [Article Influence: 61.2] [Reference Citation Analysis (2)] |
| 112. | Gershon MD. The enteric nervous system: a second brain. Hosp Pract (1995). 1999;34:31-32, 35-38, 41-42 passim. [PubMed] |
| 113. | Stasi C, Bellini M, Bassotti G, Blandizzi C, Milani S. Serotonin receptors and their role in the pathophysiology and therapy of irritable bowel syndrome. Tech Coloproctol. 2014;18:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 114. | Gershon MD. Plasticity in serotonin control mechanisms in the gut. Curr Opin Pharmacol. 2003;3:600-607. [PubMed] |
| 115. | Crowell MD. Role of serotonin in the pathophysiology of the irritable bowel syndrome. Br J Pharmacol. 2004;141:1285-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 200] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 116. | Colucci R, Blandizzi C, Bellini M, Ghisu N, Tonini M, Del Tacca M. The genetics of the serotonin transporter and irritable bowel syndrome. Trends Mol Med. 2008;14:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 117. | Jarrett ME, Kohen R, Cain KC, Burr RL, Poppe A, Navaja GP, Heitkemper MM. Relationship of SERT polymorphisms to depressive and anxiety symptoms in irritable bowel syndrome. Biol Res Nurs. 2007;9:161-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 118. | Geeraerts B, van Oudenhove L, Tack J. Serotonin transporter gene polymorphisms in irritable bowel syndrome. Neurogastroenterol Motil. 2006;18:957-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 119. | Coates MD, Mahoney CR, Linden DR, Sampson JE, Chen J, Blaszyk H, Crowell MD, Sharkey KA, Gershon MD, Mawe GM. Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and irritable bowel syndrome. Gastroenterology. 2004;126:1657-1664. [PubMed] |
| 120. | Dunlop SP, Coleman NS, Blackshaw E, Perkins AC, Singh G, Marsden CA, Spiller RC. Abnormalities of 5-hydroxytryptamine metabolism in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2005;3:349-357. [PubMed] |
| 121. | Sha W, Pasricha PJ, Chen JD. Rhythmic and spatial abnormalities of gastric slow waves in patients with functional dyspepsia. J Clin Gastroenterol. 2009;43:123-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 122. | Cucchiara S, Riezzo G, Minella R, Pezzolla F, Giorgio I, Auricchio S. Electrogastrography in non-ulcer dyspepsia. Arch Dis Child. 1992;67:613-617. [PubMed] |
| 123. | Riezzo G, Chiloiro M, Guerra V, Borrelli O, Salvia G, Cucchiara S. Comparison of gastric electrical activity and gastric emptying in healthy and dyspeptic children. Dig Dis Sci. 2000;45:517-524. [PubMed] |
| 124. | Friesen CA, Lin Z, Hyman PE, Andre L, Welchert E, Schurman JV, Cocjin JT, Burchell N, Pulliam S, Moore A. Electrogastrography in pediatric functional dyspepsia: relationship to gastric emptying and symptom severity. J Pediatr Gastroenterol Nutr. 2006;42:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 125. | DuPont AW, Jiang ZD, Harold SA, Snyder N, Galler GW, Garcia-Torres F, DuPont HL. Motility abnormalities in irritable bowel syndrome. Digestion. 2014;89:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 126. | Devanarayana NM, Rajindrajith S, Benninga MA. Abdominal migraine in children: association between gastric motility parameters and clinical characteristics. BMC Gastroenterol. 2016;16:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 127. | Devanarayana NM, Rajindrajith S, Perera MS, Nishanthanie SW, Benninga MA. Gastric emptying and antral motility parameters in children with functional dyspepsia: association with symptom severity. J Gastroenterol Hepatol. 2013;28:1161-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 128. | Devanarayana NM, Rajindrajith S, Bandara C, Shashiprabha G, Benninga MA. Ultrasonographic assessment of liquid gastric emptying and antral motility according to the subtypes of irritable bowel syndrome in children. J Pediatr Gastroenterol Nutr. 2013;56:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 129. | Devanarayana NM, Rajindrajith S, Rathnamalala N, Samaraweera S, Benninga MA. Delayed gastric emptying rates and impaired antral motility in children fulfilling Rome III criteria for functional abdominal pain. Neurogastroenterol Motil. 2012;24:420-425, e207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 130. | Stanghellini V, Tosetti C, Paternico A, Barbara G, Morselli-Labate AM, Monetti N, Marengo M, Corinaldesi R. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996;110:1036-1042. [PubMed] |
| 131. | Gilja OH, Hausken T, Wilhelmsen I, Berstad A. Impaired accommodation of proximal stomach to a meal in functional dyspepsia. Dig Dis Sci. 1996;41:689-696. [PubMed] |
| 132. | Olafsdottir E, Gilja OH, Aslaksen A, Berstad A, Fluge G. Impaired accommodation of the proximal stomach in children with recurrent abdominal pain. J Pediatr Gastroenterol Nutr. 2000;30:157-163. [PubMed] |
| 133. | Portincasa P, Moschetta A, Baldassarre G, Altomare DF, Palasciano G. Pan-enteric dysmotility, impaired quality of life and alexithymia in a large group of patients meeting ROME II criteria for irritable bowel syndrome. World J Gastroenterol. 2003;9:2293-2299. [PubMed] |
| 134. | Serra J, Azpiroz F, Malagelada JR. Impaired transit and tolerance of intestinal gas in the irritable bowel syndrome. Gut. 2001;48:14-19. [PubMed] |
| 135. | Lu CL, Chen CY, Chang FY, Lee SD. Characteristics of small bowel motility in patients with irritable bowel syndrome and normal humans: an Oriental study. Clin Sci (Lond). 1998;95:165-169. [PubMed] |
| 136. | Bremner JD, Innis RB, Ng CK, Staib LH, Salomon RM, Bronen RA, Duncan J, Southwick SM, Krystal JH, Rich D. Positron emission tomography measurement of cerebral metabolic correlates of yohimbine administration in combat-related posttraumatic stress disorder. Arch Gen Psychiatry. 1997;54:246-254. [PubMed] |
| 137. | Jones MP, Walker MM, Ford AC, Talley NJ. The overlap of atopy and functional gastrointestinal disorders among 23,471 patients in primary care. Aliment Pharmacol Ther. 2014;40:382-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 100] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 138. | Huerta C, García Rodríguez LA, Wallander MA, Johansson S. Risk of irritable bowel syndrome among asthma patients. Pharmacoepidemiol Drug Saf. 2002;11:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 139. | Olén O, Neuman Å, Koopmann B, Ludvigsson JF, Ballardini N, Westman M, Melén E, Kull I, Simrén M, Bergström A. Allergy-related diseases and recurrent abdominal pain during childhood - a birth cohort study. Aliment Pharmacol Ther. 2014;40:1349-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 140. | Petitpierre M, Gumowski P, Girard JP. Irritable bowel syndrome and hypersensitivity to food. Ann Allergy. 1985;54:538-540. [PubMed] |
| 141. | Zwetchkenbaum J, Burakoff R. The irritable bowel syndrome and food hypersensitivity. Ann Allergy. 1988;61:47-49. [PubMed] |
| 142. | Libel R, Biddle WL, Miner PB Jr. Evaluation of anorectal physiology in patients with increased mast cells. Dig Dis Sci. 1993;38:877-881. [PubMed] |
| 143. | Guilarte M, Santos J, de Torres I, Alonso C, Vicario M, Ramos L, Martínez C, Casellas F, Saperas E, Malagelada JR. Diarrhoea-predominant IBS patients show mast cell activation and hyperplasia in the jejunum. Gut. 2007;56:203-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 297] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 144. | Faure C, Patey N, Gauthier C, Brooks EM, Mawe GM. Serotonin signaling is altered in irritable bowel syndrome with diarrhea but not in functional dyspepsia in pediatric age patients. Gastroenterology. 2010;139:249-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 116] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 145. | Shulman RJ, Eakin MN, Czyzewski DI, Jarrett M, Ou CN. Increased gastrointestinal permeability and gut inflammation in children with functional abdominal pain and irritable bowel syndrome. J Pediatr. 2008;153:646-650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 126] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 146. | Martínez C, Lobo B, Pigrau M, Ramos L, González-Castro AM, Alonso C, Guilarte M, Guilá M, de Torres I, Azpiroz F. Diarrhoea-predominant irritable bowel syndrome: an organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2013;62:1160-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 216] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 147. | Bertiaux-Vandaële N, Youmba SB, Belmonte L, Lecleire S, Antonietti M, Gourcerol G, Leroi AM, Déchelotte P, Ménard JF, Ducrotté P. The expression and the cellular distribution of the tight junction proteins are altered in irritable bowel syndrome patients with differences according to the disease subtype. Am J Gastroenterol. 2011;106:2165-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 223] [Article Influence: 14.9] [Reference Citation Analysis (1)] |
| 148. | Coëffier M, Gloro R, Boukhettala N, Aziz M, Lecleire S, Vandaele N, Antonietti M, Savoye G, Bôle-Feysot C, Déchelotte P. Increased proteasome-mediated degradation of occludin in irritable bowel syndrome. Am J Gastroenterol. 2010;105:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 147] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 149. | Marshall JK, Thabane M, Garg AX, Clark WF, Salvadori M, Collins SM; Walkerton Health Study Investigators. Incidence and epidemiology of irritable bowel syndrome after a large waterborne outbreak of bacterial dysentery. Gastroenterology. 2006;131:445-450; quiz 660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 231] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 150. | Lee YJ, Park KS. Irritable bowel syndrome: emerging paradigm in pathophysiology. World J Gastroenterol. 2014;20:2456-2469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 102] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (2)] |
| 151. | Sundin J, Öhman L, Simrén M. Understanding the Gut Microbiota in Inflammatory and Functional Gastrointestinal Diseases. Psychosom Med. 2017;79:857-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 152. | Saulnier DM, Riehle K, Mistretta TA, Diaz MA, Mandal D, Raza S, Weidler EM, Qin X, Coarfa C, Milosavljevic A. Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome. Gastroenterology. 2011;141:1782-1791. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 559] [Cited by in RCA: 509] [Article Influence: 33.9] [Reference Citation Analysis (1)] |
| 153. | Shankar V, Agans R, Holmes B, Raymer M, Paliy O. Do gut microbial communities differ in pediatric IBS and health? Gut Microbes. 2013;4:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 154. | Rigsbee L, Agans R, Shankar V, Kenche H, Khamis HJ, Michail S, Paliy O. Quantitative profiling of gut microbiota of children with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2012;107:1740-1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 156] [Article Influence: 11.1] [Reference Citation Analysis (1)] |
| 155. | Crouzet L, Gaultier E, Del’Homme C, Cartier C, Delmas E, Dapoigny M, Fioramonti J, Bernalier-Donadille A. The hypersensitivity to colonic distension of IBS patients can be transferred to rats through their fecal microbiota. Neurogastroenterol Motil. 2013;25:e272-e282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 212] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 156. | Treem WR, Ahsan N, Kastoff G, Hyams JS. Fecal short-chain fatty acids in patients with diarrhea-predominant irritable bowel syndrome: in vitro studies of carbohydrate fermentation. J Pediatr Gastroenterol Nutr. 1996;23:280-286. [PubMed] |
| 157. | Rajilić-Stojanović M, Jonkers DM, Salonen A, Hanevik K, Raes J, Jalanka J, de Vos WM, Manichanh C, Golic N, Enck P. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol. 2015;110:278-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 276] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 158. | Barrett JS, Gearry RB, Muir JG, Irving PM, Rose R, Rosella O, Haines ML, Shepherd SJ, Gibson PR. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010;31:874-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 131] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 159. | Chumpitazi BP, Shulman RJ. Dietary Carbohydrates and Childhood Functional Abdominal Pain. Ann Nutr Metab. 2016;68 Suppl 1:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 160. | Ford AC, Talley NJ, Spiegel BM, Foxx-Orenstein AE, Schiller L, Quigley EM, Moayyedi P. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. 2008;337:a2313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 356] [Article Influence: 19.8] [Reference Citation Analysis (2)] |
| 161. | Ruepert L, Quartero AO, de Wit NJ, van der Heijden GJ, Rubin G, Muris JW. Bulking agents, antispasmodics and antidepressants for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2011;CD003460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 167] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 162. | Locke GR 3rd, Zinsmeister AR, Talley NJ, Fett SL, Melton LJ 3rd. Familial association in adults with functional gastrointestinal disorders. Mayo Clin Proc. 2000;75:907-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 183] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 163. | Levy RL, Jones KR, Whitehead WE, Feld SI, Talley NJ, Corey LA. Irritable bowel syndrome in twins: heredity and social learning both contribute to etiology. Gastroenterology. 2001;121:799-804. [PubMed] |
| 164. | Buonavolontà R, Coccorullo P, Turco R, Boccia G, Greco L, Staiano A. Familial aggregation in children affected by functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2010;50:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 165. | Camilleri M, Katzka DA. Irritable bowel syndrome: methods, mechanisms, and pathophysiology. Genetic epidemiology and pharmacogenetics in irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2012;302:G1075-G1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 166. | Liao XJ, Mao WM, Wang Q, Yang GG, Wu WJ, Shao SX. MicroRNA-24 inhibits serotonin reuptake transporter expression and aggravates irritable bowel syndrome. Biochem Biophys Res Commun. 2016;469:288-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 167. | Zhang Y, Li Y, Hao Z, Li X, Bo P, Gong W. Association of the Serotonin Receptor 3E Gene as a Functional Variant in the MicroRNA-510 Target Site with Diarrhea Predominant Irritable Bowel Syndrome in Chinese Women. J Neurogastroenterol Motil. 2016;22:272-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 168. | Wang WF, Li X, Guo MZ, Chen JD, Yang YS, Peng LH, Wang YH, Zhang CY, Li HH. Mitochondrial ATP 6 and 8 polymorphisms in irritable bowel syndrome with diarrhea. World J Gastroenterol. 2013;19:3847-3853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 169. | Uğur Kantar F, Simşek İ, Ercal D, Ülgenalp A, Bora E. Alpha-2-adrenergic receptor gene polymorphism in Turkish population with irritable bowel syndrome. Turk J Gastroenterol. 2013;24:483-488. [PubMed] |
| 170. | Barkhordari E, Amirzargar AA, Ebrahimi-Daryani N, Mahmoudi M, Ansaripour B, Alighardashi M, Ahmadi-Ashtiani HR, Bashashati M, Rezaei N. Lack of Association between Interleukin 12 C(-1188)A Polymorphism and Irritable Bowel Syndrome. Avicenna J Med Biotechnol. 2011;3:45-48. [PubMed] |
| 171. | Bashashati M, Rezaei N, Bashashati H, Shafieyoun A, Daryani NE, Sharkey KA, Storr M. Cytokine gene polymorphisms are associated with irritable bowel syndrome: a systematic review and meta-analysis. Neurogastroenterol Motil. 2012;24:1102-e566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 172. | Ek WE, Reznichenko A, Ripke S, Niesler B, Zucchelli M, Rivera NV, Schmidt PT, Pedersen NL, Magnusson P, Talley NJ. Exploring the genetics of irritable bowel syndrome: a GWA study in the general population and replication in multinational case-control cohorts. Gut. 2015;64:1774-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 173. | Swan C, Duroudier NP, Campbell E, Zaitoun A, Hastings M, Dukes GE, Cox J, Kelly FM, Wilde J, Lennon MG. Identifying and testing candidate genetic polymorphisms in the irritable bowel syndrome (IBS): association with TNFSF15 and TNFα. Gut. 2013;62:985-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 133] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 174. | Zucchelli M, Camilleri M, Andreasson AN, Bresso F, Dlugosz A, Halfvarson J, Törkvist L, Schmidt PT, Karling P, Ohlsson B. Association of TNFSF15 polymorphism with irritable bowel syndrome. Gut. 2011;60:1671-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 175. | Dinan TG, Cryan J, Shanahan F, Keeling PW, Quigley EM. IBS: An epigenetic perspective. Nat Rev Gastroenterol Hepatol. 2010;7:465-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 176. | Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1858] [Cited by in RCA: 2218] [Article Influence: 76.5] [Reference Citation Analysis (3)] |
| 177. | Russo M, Martinelli M, Sciorio E, Botta C, Miele E, Vallone G, Staiano A. Stool consistency, but not frequency, correlates with total gastrointestinal transit time in children. J Pediatr. 2013;162:1188-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 178. | Lane MM, Czyzewski DI, Chumpitazi BP, Shulman RJ. Reliability and validity of a modified Bristol Stool Form Scale for children. J Pediatr. 2011;159:437-441.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 179. | Gijsbers CF, Benninga MA, Schweizer JJ, Kneepkens CM, Vergouwe Y, Büller HA. Validation of the Rome III criteria and alarm symptoms for recurrent abdominal pain in children. J Pediatr Gastroenterol Nutr. 2014;58:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 180. | Drossman DA, Morris CB, Hu Y, Toner BB, Diamant N, Leserman J, Shetzline M, Dalton C, Bangdiwala SI. A prospective assessment of bowel habit in irritable bowel syndrome in women: defining an alternator. Gastroenterology. 2005;128:580-589. [PubMed] |
| 181. | Thakkar K, Chen L, Tessier ME, Gilger MA. Outcomes of children after esophagogastroduodenoscopy for chronic abdominal pain. Clin Gastroenterol Hepatol. 2014;12:963-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 182. | Spiller R, Aziz Q, Creed F, Emmanuel A, Houghton L, Hungin P, Jones R, Kumar D, Rubin G, Trudgill N. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007;56:1770-1798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 609] [Cited by in RCA: 538] [Article Influence: 28.3] [Reference Citation Analysis (25)] |
| 183. | El-Chammas K, Majeskie A, Simpson P, Sood M, Miranda A. Red flags in children with chronic abdominal pain and Crohn’s disease-a single center experience. J Pediatr. 2013;162:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 184. | Tam YH, Chan KW, To KF, Cheung ST, Mou JW, Pang KK, Wong YS, Sihoe JD, Lee KH. Impact of pediatric Rome III criteria of functional dyspepsia on the diagnostic yield of upper endoscopy and predictors for a positive endoscopic finding. J Pediatr Gastroenterol Nutr. 2011;52:387-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 185. | Motamed F, Mohsenipour R, Seifirad S, Yusefi A, Farahmand F, Khodadad A, Falahi G, Najafi M. Red flags of organic recurrent abdominal pain in children: study on 100 subjects. Iran J Pediatr. 2012;22:457-462. [PubMed] |
| 186. | El-Matary W, Spray C, Sandhu B. Irritable bowel syndrome: the commonest cause of recurrent abdominal pain in children. Eur J Pediatr. 2004;163:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 187. | Dhroove G, Chogle A, Saps M. A million-dollar work-up for abdominal pain: is it worth it? J Pediatr Gastroenterol Nutr. 2010;51:579-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 160] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 188. | Di Lorenzo C, Colletti RB, Lehmann HP, Boyle JT, Gerson WT, Hyams JS, Squires RH Jr, Walker LS, Kanda PT; AAP Subcommittee; NASPGHAN Committee on Chronic Abdominal Pain. Chronic Abdominal Pain In Children: a Technical Report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2005;40:249-261. [PubMed] |
| 189. | Irvine AJ, Chey WD, Ford AC. Screening for Celiac Disease in Irritable Bowel Syndrome: An Updated Systematic Review and Meta-analysis. Am J Gastroenterol. 2017;112:65-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 190. | Kansu A, Kuloğlu Z, Demir A, Yaman A; Turkish Celiac Study Group. Yield of coeliac screening in abdominal pain-associated functional gastrointestinal system disorders. J Paediatr Child Health. 2015;51:1066-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 191. | Farahmand F, Modaresi V, Najafi M, Khodadad A, Moetamed F, Modarres Z. Prevalence of celiac disease in Iranian children with recurrent abdominal pain referred to a pediatric referral center. Iran J Pediatr. 2011;21:33-38. [PubMed] |
| 192. | Bhattacharya M, Dubey AP, Mathur NB. Prevalence of celiac disease in north Indian children. Indian Pediatr. 2009;46:415-417. [PubMed] |
| 193. | Prell C, Nagel D, Freudenberg F, Schwarzer A, Koletzko S. Comparison of three tests for faecal calprotectin in children and young adults: a retrospective monocentric study. BMJ Open. 2014;4:e004558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 194. | Fagerberg UL, Lööf L, Myrdal U, Hansson LO, Finkel Y. Colorectal inflammation is well predicted by fecal calprotectin in children with gastrointestinal symptoms. J Pediatr Gastroenterol Nutr. 2005;40:450-455. [PubMed] |
| 195. | Flagstad G, Helgeland H, Markestad T. Faecal calprotectin concentrations in children with functional gastrointestinal disorders diagnosed according to the Pediatric Rome III criteria. Acta Paediatr. 2010;99:734-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 196. | Miele E, Giannetti E, Martinelli M, Tramontano A, Greco L, Staiano A. Impact of the Rome II paediatric criteria on the appropriateness of the upper and lower gastrointestinal endoscopy in children. Aliment Pharmacol Ther. 2010;32:582-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 197. | Bonilla S, Deli Wang, Saps M. The prognostic value of obtaining a negative endoscopy in children with functional gastrointestinal disorders. Clin Pediatr (Phila). 2011;50:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 198. | Yip WC, Ho TF, Yip YY, Chan KY. Value of abdominal sonography in the assessment of children with abdominal pain. J Clin Ultrasound. 1998;26:397-400. [PubMed] |
| 199. | Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, Kirsch I, Schyner RN, Nam BH, Nguyen LT. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336:999-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 842] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 200. | Levy RL, Langer SL, Romano JM, Labus J, Walker LS, Murphy TB, Tilburg MA, Feld LD, Christie DL, Whitehead WE. Cognitive mediators of treatment outcomes in pediatric functional abdominal pain. Clin J Pain. 2014;30:1033-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 201. | Walker LS, Williams SE, Smith CA, Garber J, Van Slyke DA, Lipani TA. Parent attention versus distraction: impact on symptom complaints by children with and without chronic functional abdominal pain. Pain. 2006;122:43-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 211] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 202. | Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Ballard SA, Labus J, Welsh E. Twelve-month follow-up of cognitive behavioral therapy for children with functional abdominal pain. JAMA Pediatr. 2013;167:178-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 203. | Rouster AS, Karpinski AC, Silver D, Monagas J, Hyman PE. Functional Gastrointestinal Disorders Dominate Pediatric Gastroenterology Outpatient Practice. J Pediatr Gastroenterol Nutr. 2016;62:847-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 204. | Saps M, Miranda A. Gastrointestinal Pharmacology. Handb Exp Pharmacol. 2017;239:147-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 205. | Korterink JJ, Rutten JM, Venmans L, Benninga MA, Tabbers MM. Pharmacologic treatment in pediatric functional abdominal pain disorders: a systematic review. J Pediatr. 2015;166:424-431.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 206. | Veldhuyzen van Zanten SJ, Jones MJ, Verlinden M, Talley NJ. Efficacy of cisapride and domperidone in functional (nonulcer) dyspepsia: a meta-analysis. Am J Gastroenterol. 2001;96:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 207. | Karunanayake A, Devanarayana NM, de Silva A, Gunawardena S, Rajindrajith S. Randomized controlled clinical trial on value of domperidone in functional abdominal pain in children. J Pediatr Gastroenterol Nutr. 2018;66:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 208. | Korterink J, Devanarayana NM, Rajindrajith S, Vlieger A, Benninga MA. Childhood functional abdominal pain: mechanisms and management. Nat Rev Gastroenterol Hepatol. 2015;12:159-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 209. | Saps M, Youssef N, Miranda A, Nurko S, Hyman P, Cocjin J, Di Lorenzo C. Multicenter, randomized, placebo-controlled trial of amitriptyline in children with functional gastrointestinal disorders. Gastroenterology. 2009;137:1261-1269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 153] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 210. | Bahar RJ, Collins BS, Steinmetz B, Ament ME. Double-blind placebo-controlled trial of amitriptyline for the treatment of irritable bowel syndrome in adolescents. J Pediatr. 2008;152:685-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 211. | Roohafza H, Pourmoghaddas Z, Saneian H, Gholamrezaei A. Citalopram for pediatric functional abdominal pain: a randomized, placebo-controlled trial. Neurogastroenterol Motil. 2014;26:1642-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 212. | Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1350-65; quiz 1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 290] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 213. | See MC, Birnbaum AH, Schechter CB, Goldenberg MM, Benkov KJ. Double-blind, placebo-controlled trial of famotidine in children with abdominal pain and dyspepsia: global and quantitative assessment. Dig Dis Sci. 2001;46:985-992. [PubMed] |
| 214. | De Bruyne P, Ito S. Toxicity of long-term use of proton pump inhibitors in children. Arch Dis Child. 2018;103:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 215. | Cash BD, Epstein MS, Shah SM. A Novel Delivery System of Peppermint Oil Is an Effective Therapy for Irritable Bowel Syndrome Symptoms. Dig Dis Sci. 2016;61:560-571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 104] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 216. | Asgarshirazi M, Shariat M, Dalili H. Comparison of the Effects of pH-Dependent Peppermint Oil and Synbiotic Lactol (Bacillus coagulans + Fructooligosaccharides) on Childhood Functional Abdominal Pain: A Randomized Placebo-Controlled Study. Iran Red Crescent Med J. 2015;17:e23844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 217. | Kline RM, Kline JJ, Di Palma J, Barbero GJ. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J Pediatr. 2001;138:125-128. [PubMed] |
| 218. | Martin AE, Newlove-Delgado TV, Abbott RA, Bethel A, Thompson-Coon J, Whear R, Logan S. Pharmacological interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;3:CD010973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 219. | Annaházi A, Róka R, Rosztóczy A, Wittmann T. Role of antispasmodics in the treatment of irritable bowel syndrome. World J Gastroenterol. 2014;20:6031-6043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 90] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 220. | Pourmoghaddas Z, Saneian H, Roohafza H, Gholamrezaei A. Mebeverine for pediatric functional abdominal pain: a randomized, placebo-controlled trial. Biomed Res Int. 2014;2014:191026. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 221. | Narang M, Shah D, Akhtar H. Efficacy and Safety of Drotaverine Hydrochloride in Children with Recurrent Abdominal Pain: A Randomized Placebo Controlled Trial. Indian Pediatr. 2015;52:847-851. [PubMed] |
| 222. | Sadeghian M, Farahmand F, Fallahi GH, Abbasi A. Cyproheptadine for the treatment of functional abdominal pain in childhood: a double-blinded randomized placebo-controlled trial. Minerva Pediatr. 2008;60:1367-1374. [PubMed] |
| 223. | Collins BS, Lin HC. Double-blind, placebo-controlled antibiotic treatment study of small intestinal bacterial overgrowth in children with chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2011;52:382-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 224. | Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, Mareya SM, Shaw AL, Bortey E, Forbes WP; TARGET Study Group. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 690] [Cited by in RCA: 715] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 225. | Scarpellini E, Giorgio V, Gabrielli M, Filoni S, Vitale G, Tortora A, Ojetti V, Gigante G, Fundarò C, Gasbarrini A. Rifaximin treatment for small intestinal bacterial overgrowth in children with irritable bowel syndrome. Eur Rev Med Pharmacol Sci. 2013;17:1314-1320. [PubMed] |
| 226. | Olness K. Hypnosis and biofeedback with children and adolescents; clinical, research, and educational aspects. Introduction. J Dev Behav Pediatr. 1996;17:299. [PubMed] |
| 227. | Weydert JA, Shapiro DE, Acra SA, Monheim CJ, Chambers AS, Ball TM. Evaluation of guided imagery as treatment for recurrent abdominal pain in children: a randomized controlled trial. BMC Pediatr. 2006;6:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 77] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 228. | van Tilburg MA, Chitkara DK, Palsson OS, Turner M, Blois-Martin N, Ulshen M, Whitehead WE. Audio-recorded guided imagery treatment reduces functional abdominal pain in children: a pilot study. Pediatrics. 2009;124:e890-e897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 229. | Gonsalkorale WM, Whorwell PJ. Hypnotherapy in the treatment of irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2005;17:15-20. [PubMed] |
| 230. | Moser G, Trägner S, Gajowniczek EE, Mikulits A, Michalski M, Kazemi-Shirazi L, Kulnigg-Dabsch S, Führer M, Ponocny-Seliger E, Dejaco C. Long-term success of GUT-directed group hypnosis for patients with refractory irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2013;108:602-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 231. | Vlieger AM, Menko-Frankenhuis C, Wolfkamp SC, Tromp E, Benninga MA. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007;133:1430-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 170] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 232. | Rutten JMTM, Vlieger AM, Frankenhuis C, George EK, Groeneweg M, Norbruis OF, Tjon A Ten W, van Wering HM, Dijkgraaf MGW, Merkus MP. Home-Based Hypnotherapy Self-exercises vs Individual Hypnotherapy With a Therapist for Treatment of Pediatric Irritable Bowel Syndrome, Functional Abdominal Pain, or Functional Abdominal Pain Syndrome: A Randomized Clinical Trial. JAMA Pediatr. 2017;171:470-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 233. | Abbott RA, Martin AE, Newlove-Delgado TV, Bethel A, Thompson-Coon J, Whear R, Logan S. Psychosocial interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;1:CD010971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 234. | Kovacic K, Hainsworth K, Sood M, Chelimsky G, Unteutsch R, Nugent M, Simpson P, Miranda A. Neurostimulation for abdominal pain-related functional gastrointestinal disorders in adolescents: a randomised, double-blind, sham-controlled trial. Lancet Gastroenterol Hepatol. 2017;2:727-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 235. | Chumpitazi BP, Weidler EM, Lu DY, Tsai CM, Shulman RJ. Self-Perceived Food Intolerances Are Common and Associated with Clinical Severity in Childhood Irritable Bowel Syndrome. J Acad Nutr Diet. 2016;116:1458-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 236. | Chumpitazi BP, Cope JL, Hollister EB, Tsai CM, McMeans AR, Luna RA, Versalovic J, Shulman RJ. Randomised clinical trial: gut microbiome biomarkers are associated with clinical response to a low FODMAP diet in children with the irritable bowel syndrome. Aliment Pharmacol Ther. 2015;42:418-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 237. | Christensen MF. Recurrent abdominal pain and dietary fiber. Am J Dis Child. 1986;140:738-739. [PubMed] |
| 238. | Feldman W, McGrath P, Hodgson C, Ritter H, Shipman RT. The use of dietary fiber in the management of simple, childhood, idiopathic, recurrent, abdominal pain. Results in a prospective, double-blind, randomized, controlled trial. Am J Dis Child. 1985;139:1216-1218. [PubMed] |
| 239. | Horvath A, Dziechciarz P, Szajewska H. Glucomannan for abdominal pain-related functional gastrointestinal disorders in children: a randomized trial. World J Gastroenterol. 2013;19:3062-3068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 240. | Shulman RJ, Hollister EB, Cain K, Czyzewski DI, Self MM, Weidler EM, Devaraj S, Luna RA, Versalovic J, Heitkemper M. Psyllium Fiber Reduces Abdominal Pain in Children With Irritable Bowel Syndrome in a Randomized, Double-Blind Trial. Clin Gastroenterol Hepatol. 2017;15:712-719.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 241. | Parisi G, Bottona E, Carrara M, Cardin F, Faedo A, Goldin D, Marino M, Pantalena M, Tafner G, Verdianelli G. Treatment effects of partially hydrolyzed guar gum on symptoms and quality of life of patients with irritable bowel syndrome. A multicenter randomized open trial. Dig Dis Sci. 2005;50:1107-1112. [PubMed] |
| 242. | Newlove-Delgado TV, Martin AE, Abbott RA, Bethel A, Thompson-Coon J, Whear R, Logan S. Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;3:CD010972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 243. | Bauserman M, Michail S. The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. J Pediatr. 2005;147:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 160] [Article Influence: 7.6] [Reference Citation Analysis (1)] |
| 244. | Kianifar H, Jafari SA, Kiani M, Ahanchian H, Ghasemi SV, Grover Z, Mahmoodi LZ, Bagherian R, Khalesi M. Probiotic for irritable bowel syndrome in pediatric patients: a randomized controlled clinical trial. Electron Physician. 2015;7:1255-1260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 245. | Francavilla R, Miniello V, Magistà AM, De Canio A, Bucci N, Gagliardi F, Lionetti E, Castellaneta S, Polimeno L, Peccarisi L. A randomized controlled trial of Lactobacillus GG in children with functional abdominal pain. Pediatrics. 2010;126:e1445-e1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 154] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 246. | Guandalini S, Magazzù G, Chiaro A, La Balestra V, Di Nardo G, Gopalan S, Sibal A, Romano C, Canani RB, Lionetti P. VSL#3 improves symptoms in children with irritable bowel syndrome: a multicenter, randomized, placebo-controlled, double-blind, crossover study. J Pediatr Gastroenterol Nutr. 2010;51:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 175] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 247. | Varni JW, Shulman RJ, Self MM, Nurko S, Saps M, Saeed SA, Patel AS, Dark CV, Bendo CB, Pohl JF; Pediatric Quality of Life Inventory™ Gastrointestinal Symptoms Module Testing Study Consortium. Gastrointestinal symptoms predictors of health-related quality of life in pediatric patients with functional gastrointestinal disorders. Qual Life Res. 2017;26:1015-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 248. | Indrio F, Di Mauro A, Riezzo G, Civardi E, Intini C, Corvaglia L, Ballardini E, Bisceglia M, Cinquetti M, Brazzoduro E. Prophylactic use of a probiotic in the prevention of colic, regurgitation, and functional constipation: a randomized clinical trial. JAMA Pediatr. 2014;168:228-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 140] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 249. | Kannampalli P, Pochiraju S, Chichlowski M, Berg BM, Rudolph C, Bruckert M, Miranda A, Sengupta JN. Probiotic Lactobacillus rhamnosus GG (LGG) and prebiotic prevent neonatal inflammation-induced visceral hypersensitivity in adult rats. Neurogastroenterol Motil. 2014;26:1694-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 250. | Videlock EJ, Adeyemo M, Licudine A, Hirano M, Ohning G, Mayer M, Mayer EA, Chang L. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137:1954-1962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 153] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 251. | Marugán-Miguelsanz JM, Ontoria M, Velayos B, Torres-Hinojal MC, Redondo P, Fernández-Salazar L. Natural history of irritable bowel syndrome. Pediatr Int. 2013;55:204-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Sri Lanka
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Chiba T, Soares RL S- Editor: Gong ZM L- Editor: A E- Editor: Huang Y