Published online Jan 7, 2018. doi: 10.3748/wjg.v24.i1.157
Peer-review started: October 26, 2017
First decision: November 21, 2017
Revised: December 1, 2017
Accepted: December 4, 2017
Article in press: December 4, 2017
Published online: January 7, 2018
Processing time: 73 Days and 20.1 Hours
A 28-year-old man presented with anemia symptoms and intermittent tarry stool passage for three days. No stigmata of hemorrhage were identified using esophagogastroduodenoscopy, ileocolonoscopy, and contrast-enhanced computed tomography. He then developed massive tarry stool passage with profound hypovolemic shock and hypoxic respiratory failure. Emergent angiography revealed active bleeder, probably from the jejunal branches of the superior mesenteric artery, but embolization was not performed due to possible subsequent extensive bowel ischemia. His airway was secured via endotracheal intubation with ventilator support, and emergent antegrade single-balloon enteroscopy was performed at 8 h after clinical overt bleeding occurrence; the procedure revealed a 2-cm pulsating subepithelial tumor with a protruding blood plug at the distal jejunum. Laparoscopic segmental resection of the jejunum with end-to-end anastomosis was performed after emergent endoscopic tattooing localization. Pathological examination revealed a vascular malformation in the submucosa with an organizing thrombus. He was uneventfully discharged 5 d later. This case report highlights the benefit of early deep enteroscopy for the treatment of small intestinal bleeding.
Core tip: We believe that emergent deep enteroscopy performed with a secure airway and ventilator support can efficiently identify the stigmata of hemorrhage in clinical overt small intestinal bleeding and guide the operative approach.
- Citation: Chung CS, Chen KC, Chou YH, Chen KH. Emergent single-balloon enteroscopy for overt bleeding of small intestinal vascular malformation. World J Gastroenterol 2018; 24(1): 157-160
- URL: https://www.wjgnet.com/1007-9327/full/v24/i1/157.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i1.157
The small bowel (SB) has been considered as the “dark continent” of gastrointestinal (GI) tract, and the management of SB disease is always surgical because of its inaccessibility via regular endoscopy. The detection and management of SB bleeding remained challenging to gastroenterologists until the introduction of device-assisted enteroscopy (DAE)[1-3]. DAE has been proposed as an efficient diagnostic tool (diagnostic yield rate from 40.7%-87.3%) and safe therapeutic (yield rate up to 48%) approach for the treatment of bleeding from SB vascular lesions[1,2,4-7]. However, it remains unknown whether the benefit provided by early endoscopic intervention in SB bleeding is similar to that provided by emergent esophagogastroduodenoscopy and colonoscopy in upper and lower GI bleeding[8]. We herein report a case of profound SB bleeding from a vascular malformation that was treated by laparoscopic surgery after localization using preoperative emergent deep enteroscopy.
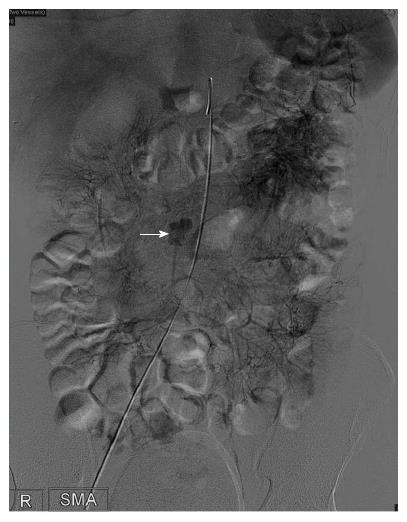
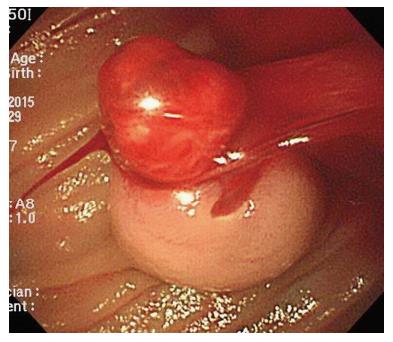
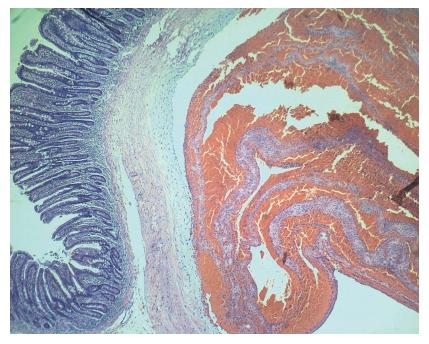
A 28-year-old man without any underlying systemic disease presented to our emergency department with intermittent tarry stool passage and anemia symptoms for 3 d. Physical examination showed pale conjunctiva and tachycardia (heart rate, 104 beats per min). Laboratory studies disclosed severe anemia with a hemoglobin level of 5.2 g/dL (normal range: 13-17 g/dL). Esophagogastroduodenoscopy, ileocolonoscopy, and contrast-enhanced computed tomography detected no evidence of the stigmata of active hemorrhage but identified many blood clots in the colon. He subsequently developed massive tarry stool passage, shock, and hypoxic respiratory failure despite aggressive blood transfusion resuscitation. Emergent angiography revealed an active bleeder, probably from the jejunal branches of superior mesenteric artery, with contrast extravasation into bowel lumen (Figure 1, arrow); however, embolization was not performed due to the possibility of extensive bowel ischemia. He was intubated with ventilator support and received emergent antegrade single-balloon enteroscopy (SIF-Q260; Olympus Medical systems, Tokyo, Japan) immediately (at 8 h) after resuscitation, endotracheal intubation, and angiographic localization for overt small intestinal bleeding. The procedure revealed a 2-cm pulsating subepithelial tumor with a protruding blood plug at the distal jejunum (Figure 2). Endoscopic tattooing using India ink was performed at 1 cm proximal to the lesion, and laparoscopic segmental resection of jejunum (6 cm in length) with end-to-end anastomosis was performed after emergent endoscopic localization. Pathological examination revealed a vascular malformation in the submucosa with an organizing thrombus (Figure 3, HE; original Magnification, 40 ×). His unstable hemodynamics markedly improved, and he was discharged 5 d later uneventfully.
Emergent deep enteroscopy is useful for the early diagnosis of small-bowel bleeding and preoperative localization of overt bleeding from small intestinal vascular malformations.
Great advents have been made in the field of GI endoscopy over the past several decades, and endoscopists have mastered the art of flexible video endoscopy for the diagnosis and treatment of upper and lower GI tract disorders. However, an endoscopic approach to the SB remains challenging because of its length and deep indwelling position in the intraperitoneal cavity. In the 20th century, thorough evaluation of the SB became possible with the development of video capsule endoscopy (VCE) and DAE[1,3]. Although VCE has been recommended as the first-line investigation for SB bleeding, DAE still has an advantage over VCE for the histopathological confirmation of SB lesions and endoscopic hemostasis[2,3]. With regard to the source of SB bleeding, vascular lesions are the most common stigmata of hemorrhage, and DAE endotherapy has been considered as an efficient and safe treatment strategy[9-12]. Additionally, the rebleeding rate of SB vascular lesions is not low, especially in the elderly among individuals with active bleeding (identified by endoscopy), a history of aortic stenosis, or those in whom the bleeding source was angioectasia; the management of rebleeding using repeated endotherapy has favorable outcomes[9,10]. Among SB vascular lesions, arteriovenous malformation bleeding can be life-threatening; hence, prompt identification and timely intervention are very important[13-16]. Although non-invasive radiological imaging or VCE is useful for the diagnosis of SB vascular lesions, lesions of smaller size or with intermittent bleeding can still be missed; meanwhile, early endoscopic intervention can be less problematic[14-16]. Nevertheless, there is scarce data regarding the timing of emergent DAE for SB bleeding. A retrospective cohort study of single-balloon enteroscopy for the management of SB bleeding did not observe a greater diagnostic or therapeutic yield in the emergent (within 24 h) enteroscopy group, but early intervention may allow for earlier stabilization and shorter hospital stays[8]. In this case report of overt bleeding from a vascular malformation in the jejunum, timely identification of the SB bleeder and preoperative localization was achieved using emergent single-balloon enteroscopy. Meanwhile, the approaching route by deep enteroscopy can be decided by pre-endoscopic angiography which assists in identification of bleeders with short endoscopy procedure time. The patient was stabilized rapidly and discharged early after laparoscopic segmental resection of the jejunal vascular malformation.
In conclusion, we successfully treated a patient with unstable hemodynamics due to overt bleeding from an SB vascular malformation using emergent preoperative deep enteroscopy. We conclude that emergent DAE is more useful than other non-invasive diagnostic modalities in the treatment of clinically overt SB bleeding; however, additional prospective studies evaluating this finding are warranted.
A young man presenting massive tarry stool passage with unstable hemodynamics.
Overt small intestinal bleeding.
Vascular lesions of small intestine, Meckel’s diverticulum.
Severe anemia.
An active bleeder, probably from the jejunal branches, with contrast extravasation into the bowel lumen was detected by emergent angiography.
Vascular malformation in the submucosa with organizing thrombus in the jejunum.
Laparoscopic small intestinal resection after localization of bleeder by emergent single-balloon enteroscopy.
Early endoscopic intervention may allow for earlier stabilization and shorter hospital stays.
Emergent DAE is more useful than other non-invasive diagnostic modalities in the treatment of clinically overt small intestinal bleeding.
| 1. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [PubMed] |
| 2. | ASGE Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Yang J, DeWitt JM. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017;85:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 115] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 3. | Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 574] [Article Influence: 52.2] [Reference Citation Analysis (1)] |
| 4. | Samaha E, Rahmi G, Landi B, Lorenceau-Savale C, Malamut G, Canard JM, Bloch F, Jian R, Chatellier G, Cellier C. Long-term outcome of patients treated with double balloon enteroscopy for small bowel vascular lesions. Am J Gastroenterol. 2012;107:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Kawamura T, Yasuda K, Tanaka K, Uno K, Ueda M, Sanada K, Nakajima M. Clinical evaluation of a newly developed single-balloon enteroscope. Gastrointest Endosc. 2008;68:1112-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 111] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 6. | Aktas H, de Ridder L, Haringsma J, Kuipers EJ, Mensink PB. Complications of single-balloon enteroscopy: a prospective evaluation of 166 procedures. Endoscopy. 2010;42:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | May A, Färber M, Aschmoneit I, Pohl J, Manner H, Lotterer E, Möschler O, Kunz J, Gossner L, Mönkemüller K. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol. 2010;105:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 155] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Nelson KK, Lipka S, Davis-Yadley AH, Rodriguez AC, Doraiswamy V, Rabbanifard R, Kumar A, Brady PG. Timing of single balloon enteroscopy: significant or not? Endosc Int Open. 2016;4:E761-E766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Kaufman D, Leslie G, Marya N, Han S, Gillespie W, Holzwanger E, Leslie R, Cave D. Small Intestinal Angioectasia: Characterization, Risk Factors, and Rebleeding. J Clin Gastroenterol. 2017;51:720-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Shinozaki S, Yamamoto H, Yano T, Sunada K, Hayashi Y, Shinhata H, Sato H, Despott EJ, Sugano K. Favorable long-term outcomes of repeat endotherapy for small-intestine vascular lesions by double-balloon endoscopy. Gastrointest Endosc. 2014;80:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Takeshita N, Otsuka Y, Nara S, Noie T, Ito K, Harihara Y, Furushima K, Konishi T. Utility of preoperative small-bowel endoscopy for hemorrhagic lesions in the small intestine. Surg Today. 2012;42:536-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Williamson JB, Judah JR, Gaidos JK, Collins DP, Wagh MS, Chauhan SS, Zoeb S, Buscaglia JM, Yan H, Hou W. Prospective evaluation of the long-term outcomes after deep small-bowel spiral enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2012;76:771-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Cui J, Huang LY, Lin SJ, Yi LZ, Wu CR, Zhang B. Small intestinal vascular malformation bleeding: a case report with imaging findings. World J Gastroenterol. 2014;20:14076-14078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Endo H, Matsuhashi N, Inamori M, Ohya T, Yanagawa T, Asayama M, Hisatomi K, Teratani T, Fujita K, Yoneda M. Tumorous arteriovenous malformation in the jejunum missed by capsule endoscopy. Gastrointest Endosc. 2008;68:773-774; discussion 774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 15. | Fujii T, Morita H, Sutoh T, Takada T, Tsutsumi S, Kuwano H. Arteriovenous malformation detected by small bowel endoscopy. Case Rep Gastroenterol. 2014;8:324-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Huprich JE, Barlow JM, Hansel SL, Alexander JA, Fidler JL. Multiphase CT enterography evaluation of small-bowel vascular lesions. AJR Am J Roentgenol. 2013;201:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Paduani GF S- Editor: Chen K L- Editor: A E- Editor: Wang CH