Published online Nov 14, 2017. doi: 10.3748/wjg.v23.i42.7626
Peer-review started: July 9, 2017
First decision: July 28, 2017
Revised: August 9, 2017
Accepted: August 25, 2017
Article in press: August 25, 2017
Published online: November 14, 2017
Processing time: 128 Days and 3.2 Hours
To characterize the understanding of hepatitis B virus (HBV) and determine if outreach improves HBV understanding among Greater Boston Area immigrants.
Six outreach sessions were held in various community venues in the Greater Boston Area. Verbal consent was obtained from participants prior to starting each session. Each session included a pre-session questionnaire, followed by a teaching session, and then a post-session questionnaire. In person interpreters were present for translation during the teaching session and assistance for questionnaire completion when needed. The questions were developed based on the HBV clinical experience of physicians who serve largely immigrant populations. Questionnaires included Likert-type scale, open-ended, and true-false questions. All results were anonymous.
One hundred and one people participated in this study. Participants were 30% male with ages ranging from 19 to 87 years. The study population included immigrants from 21 countries, as well as seven United States-born participants. The greatest numbers of participants were from Somalia (44%), Morocco (10%), and Cameroon (8%). Pre session questionnaires revealed that 42% of participants were unaware that HBV can cause cancer, and 50% were unaware that therapies for HBV exist. Our brief teaching intervention led to improved scores on post session questionnaires. For example, at baseline, 58% of participants responded correctly to the question “HBV infection can cause scarring of the liver and liver cancer”, whereas 79% of participants responded correctly after the teaching session (P = 0.01). Furthermore, the mean of total correct answers in the true or false portion of the questionnaire increased from 5.5 to 7.6 (P < 0.001).
A teaching session targeting Boston Immigrants at-risk for HBV helped improve scores on HBV knowledge questionnaires. Outreach may empower at-risk patients to pro-actively seek HBV care.
Core tip: Awareness is the key to the mitigation of transmittable diseases such as hepatitis B virus (HBV). Therefore, characterizing the baseline understanding of HBV, and improving that baseline, are the first steps toward improving HBV linkage to care among at-risk persons. To characterize and improve the baseline understanding of HBV we performed HBV teaching sessions with pre and post session questionnaires in multiple community venues in and around Boston. These sessions revealed that (1) baseline understanding of risks related to HBV are limited; and (2) a brief teaching session can significantly improve understanding of HBV risks.
- Citation: Djoufack R, Cheon SSY, Mohamed A, Faye F, Diouf K, Colvin R, Morrill J, Duffy-Keane AM, Perumalswami P, Jourdain G, Fusco D. Hepatitis B virus outreach to immigrant population in Greater Boston Area: Key to improving hepatitis B knowledge. World J Gastroenterol 2017; 23(42): 7626-7634
- URL: https://www.wjgnet.com/1007-9327/full/v23/i42/7626.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i42.7626
Roughly 240 million people worldwide are chronically infected with hepatitis B virus (HBV), defined as hepatitis B surface antigen (HBsAg) positive for over 6 mo[1]. Over 686000 people are estimated to die every year due to complications of HBV infection, including cirrhosis and liver cancer[1]. HBV prevalence varies worldwide, with highest prevalence in sub-Saharan Africa and East Asia, where between 5%-10% of the adult population is chronically infected[1,2,13]. While precise data on some countries in sub-Saharan Africa are limited, prevalence estimates have been generated from studies of migrant populations, and estimate high prevalence[5,17]. Roughly half of the 800000 to 1.4 million United States residents chronically infected with HBV were born in other countries. The Center for Disease Control and Prevention current recommendations for HBV testing and evaluation have evolved during the last two decades to include more and more persons born abroad (currently countries with HBsAg prevalence of greater than 2%). Appropriate HBV care can both prevent progression of HBV related disease in infected persons and may decrease the likelihood of spread to others[1].
A recent study in the United States found that of 277 health care providers, only 42% reported performing HBV screening in over 50% of patients at risk for HBV[12]. This study identified language as a major barrier to care. Providers speaking an Asian language or caring for > 25% Asian patients were more likely to screen for HBV. Fewer studies have focused on barriers to HBV care among African immigrants in the United States, though they are at high risk, similar to Asian immigrants[3,15]. Between 1980 and 2009, there was a seven-fold increase in the number of African-born United States residents, underscoring a need for HBV outreach targeting these at-risk populations[3,9,10]. While the United States Department of Health and Human Services have initiated efforts to increase HBV services among minority populations, there is an ongoing need for population-specific HBV linkage-to-care strategies[3,6,8].
Prior studies among immigrants in the New York City area have revealed that HBV outreach to immigrants from countries where HBV is endemic, including immigrants from Sub Saharan Africa, leads to improved HBV diagnosis and engagement in follow up care[3,7,14,16,18]., including HCC screening in those who are infected Awareness and knowledge of the disease are prerequisites to screening for HBV infection, then monitoring and treatment. We undertook a study in Boston, which has a large Sub-Saharan African immigrant population[4] to determine (1) baseline HBV knowledge among Greater Boston Area immigrants from HBV endemic regions; and (2) whether a brief teaching intervention could improve HBV knowledge among these at-risk persons.
Approval by the Partners/Massachusetts General Hospital Institutional Review Board (Protocol 2014P000921, DNF) was obtained prior to initiating this study. Verbal consent was provided by all participants.
After obtaining IRB approval, six “HBV Linkage to Care” community outreach sessions were conducted in the Greater Boston Area targeting foreign-born communities. Although the study targeted foreign born persons, we did not exclude any United States born persons who attended from participating. Event one was held at a Somali restaurant. Event two was held at a Community Health Center. Events three, four, and five were held at private residences/recreation rooms in apartment complexes throughout Boston. Event six was held at a Turkish community center. Food was provided for hospitality at each event. Participants for each event were solicited by word of mouth by a local community outreach liaison, including several members of the Somali community. Each event included the following structure: participants were greeted and informed that the session was part of a study, and verbal consent obtained in native language or in English. In person interpreters were present for Somali events (Somali speaking), Cambodian event (Khmer speaking), and the Turkish Center event (Arabic and Spanish speaking). Interpreters translated the teaching session verbally and assisted participants in questionnaire completion. Participants were then asked to complete a pre-session (baseline) questionnaire within about 30 min. The questionnaire was developed by physicians based on HBV clinical experience in Community Health Centers serving largely immigrant populations. Participants were asked three types of questions (1) six questions answered with a Likert-type scale where responses were scored along a range from 1 to 5); (2) seven open ended questions; and (3) ten true/false questions (Figure S1). The complete teaching session was developed by the study team and then presented to community-based clinicians who manage patients with viral hepatitis and outreach workers serving both immigrant and non-immigrant health center populations for input and editing prior to IRB submission and approval. During outreach events, the teaching session was presented by a member of the study team and took approximately 45 min including time for questions after the session. Participants were then asked to complete a post-session questionnaire (identical to the pre-session questionnaire), though a significant number of participants left without completing the post-session questionnaire. Of note, participants were not instructed to complete their questionnaires alone, and many participants worked in small subgroups, completing questionnaires together. At the end of each event, participants were given (1) a navigator card, in English, which stated a request for HBV testing (Figure S2); and (2) a list of local HBV providers verified to be accepting new patients and their contact information, with contents of each document translated by interpreters. The list of local providers was developed by members of the study team who identified five major medical centers and two community health centers in the Greater Boston area with whom linkage to care agreements were established by contacting outpatient Gastroenterology and/or Infectious Disease clinics at each site, and verification of each site contact information and ongoing acceptance of new patients. All participation was anonymous with no study identifiers being collected.
All questionnaires were stored in a secure file cabinet accessed only by study staff for entry into a secure database. We used the Kruskal-Wallis test or Fisher’s exact test for comparisons. A P value < 0.05 was considered significant, with no correction for multiple comparisons.
There were 101 participants in the pre-session questionnaire, 56 of whom also completed the postsession questionnaires. All 101 pre-session questionnaires were included in data. Participants were male and female, ranging from 19 to 87 years of age (Figure 1). Several female-only teaching sessions were requested by the Somali community leader, leading to greater number of female (62) than male (26) participants overall (Table 1). The study population included immigrants born in 21 countries outside the United States, as well as seven participants born in the United States (Table 1, Figure S3). Countries with the greatest number of participants were Somalia (44%), Morocco (10%), and Cameroon (8%) (Table 1, Figure S3). The mean number of years the participants had spent in the United States was 13 (SD = 12), with 24% participants having been in the United States for less than 5 years (Table 1).
| Characteristics | n (%) or mean ± SD |
| Age (yr) | 47 (18) |
| 19-30 | 20 (22) |
| 31-40 | 16 (18) |
| 41-50 | 17 (19) |
| 51-60 | 15 (17) |
| > 60 | 22 (24) |
| Gender | |
| F | 62 (70) |
| M | 26 (30) |
| Years in the United States | 13 (12) |
| 0-5 | 24 (28) |
| 6-10 | 14 (16) |
| 11-15 | 12 (14) |
| 16-20 | 21 (24) |
| > 20 | 16 (18) |
| Country of origin | |
| Somalia | 44 (44) |
| Morocco | 10 (10) |
| Cameroon | 8 (8) |
| Others1 | 39 (39) |
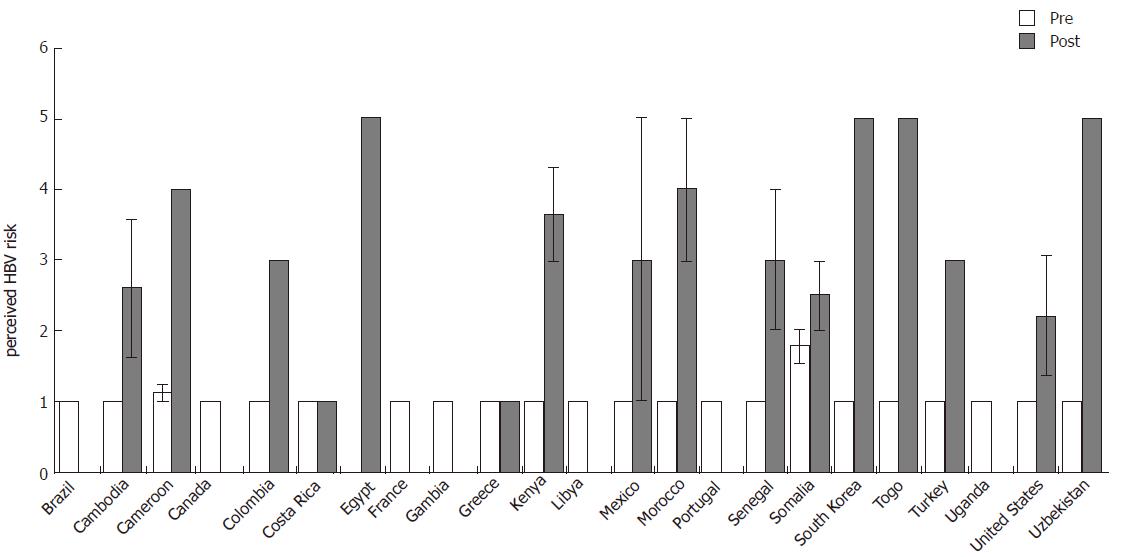
Responses to the “How high is your risk for having HBV infection?” question were scaled from 1 (lowest risk) to 5 (highest risk) (Figure 1, Figure S1). For this question of perceived HBV risk, mean response scores from pre-teaching session participants from all countries scored at or near 1 except Somalia (1.78). Following the teaching session, mean perceived risk scores increased for participants from the following countries (pre, post mean score): Cambodia (1, 2.6), Cameroon (1.1, 4), Colombia 1, 3), Kenya (1, 3.7), Mexico (1,3), Morocco (1, 4), Senegal (1, 3), Somalia (1.8, 2.5), South Korea (1, 5), Togo (1, 5), Turkey (1, 3), United States (1, 2.2), Uzbekistan (1, 5), though the statistical significance of many of these values is limited by small number of participants (Figure 1). Overall, the mean score for perceived HBV risk was 1.34 prior to the teaching session and increased to 3.26 following the teaching session (P < 0.001; Table 2), independent of gender, age, or the number of years since immigration to the United States (logistic regression, data not shown). Among reasons for possible increased risk of infection, foreign origin was the most cited (40%). Interestingly, the major cause of infection in high prevalence countries, i.e., mother-to-child transmission, was cited only once, post teaching.
| Perceived at least some risk of being HBV infected | Pre session(n = 101) | Post session(n = 56) | P value |
| Mean | 1.34 | 3.26 | < 0.001 |
| At least some risk | 11 (11) | 35 (70) | |
| Gender | |||
| Female | 7 (12) | 24 (71) | |
| Male | 3 (12) | 5 (63) | |
| Age (yr) | |||
| < 45 | 2 (5) | 23 (70) | |
| > 45 | 8 (18) | 9 (75) | |
| Years in the United States | |||
| < 5 | 2 (9) | 11 (79) | |
| > 5 | 9 (13) | 19 (63) | |
| Continent of Origin1 | |||
| Africa | 11 (16) | 19 (73) | |
| Asia | 0 | 6 (67) | |
| Europe | 0 | 4 (57) | |
| America | 0 | 1 (50) | |
| Reasons why your risk is high | |||
| Country of origin | 30 (40) | 22 (44) | |
| Needle exposure | 15 (20) | 9 (18) | |
| Sexual exposure | 14 (19) | 9 (18) | |
| I don’t know | 11 (15) | 9 (18) | |
| I am not at risk | 15 (20) | 6 (12) | |
| Other reasons2 | 8 (10) | 9 (18) | |
| Mother to child transmission | 0 | 1 (0.02) |
Participants were asked 5 open-ended questions regarding HBV testing including barriers, associated stigma and treatment knowledge (Figure S1). For the open-ended question “What makes your risk for HBV infection higher?” the percent of participants responding “Country of origin” increased slightly from 40% (pre) to 44% (post), following the teaching session (Table 2). The percent of participants answering “I am not at risk” decreased from 20 % (pre) to 12% (post) following the teaching session (Table 2). Responses to additional open ended questions revealed that 73% (pre) -81% (post) of participants reported that HBV testing is important, and 31%-40% of participants cited concerns regarding insurance coverage as a barrier to access to HBV care (Table 3).
| Variable | Pre | Post |
| Why is it important to test those at risk for HBV? | ||
| Prevent the spread of infection | 21 (24) | 8 (16) |
| Initiate the treatment early | 14 (16) | 10 (20) |
| To be aware of our status | 12 (14) | 8 (16) |
| Prevent long term complications | 9 (10) | 8 (16) |
| Because no symptoms are present until late stage | 2 (2) | |
| I don’t know | 27 (31) | 11 (22) |
| To vaccinate those unaffected | 2 (4) | |
| 2 of the above | 2 (2) | 2 (4) |
| Why you do not think it is important to test | ||
| It is important | 36 (73) | 22 (81) |
| It is not important | 3 (6) | 1 (3) |
| I don’t know | 6 (12) | 2 (7) |
| Because it is not very common | 1 (2) | |
| I don’t have enough information to recommend the test | 2 (4) | |
| Patient has the right to decide if he wants it | 1 (2) | 1 (3) |
| Because everybody has Hepatitis B | 1 (3) | |
| Barriers of access to medical care | ||
| Insurance coverage | 18 (31) | 17 (40) |
| It is easy for me | 28 (48) | 16 (38) |
| I don't know | 3 (5) | 2 (5) |
| Absence of good doctors | 1 (2) | |
| Lack of available doctors | 2 (3) | 1 (2) |
| Lack of time | 2 (3) | |
| Language barrier | 1 (2) | 1 (2) |
| Others reasons | 2 (3) | 3 (7) |
| 2 factors above | 1 (2) | 2 (5) |
| Uncomfortable asking for Hepatitis B testing | ||
| I don’t find it uncomfortable | 45 (90) | 26 (76) |
| I am afraid of the result/consequences of the infection | 2 (4) | 2 (6) |
| Shyness/fear of what he might think | 2 (4) | 2 (6) |
| Because it is sexually transmitted | 1 (2) | |
| Because I feel well | 1 (3) | |
| Because it is taboo | 3 (9) | |
| Why it will be difficult to get tested for HBV | ||
| It would not be difficult for me | 38 (64) | 24 (61) |
| Insurance coverage | 6 (10) | 5 (13) |
| Fear of the results | 4 (7) | 5 (13) |
| I don't know | 5 (8) | 1 (2.5) |
| Cost of the test | 4 (7) | 1 (2.5) |
| Concerns about confidentiality | 2 (3) | 1 (2.5) |
| Lack of time | 1 (2.5) | |
| 2 or 3 factors above | 2 (3) | 1 (2.5) |
| Why it could be difficult to get treated for HBV | ||
| It would not be difficult for me | 37 (65) | 19 (59) |
| Insurance coverage | 7 (12) | 2 (7) |
| Cost of treatment | 4 (7) | 3 (9) |
| Treatment side effects | 2 (3.5) | |
| I don't know | 3 ( (5)) | |
| Lifelong treatment | 2 (7) | |
| Lack of treatment providers | 1 (2) | |
| Other reasons | 1 (2) | |
| 2 0r 3 factors above | 2 (3.5) | 6 (19) |
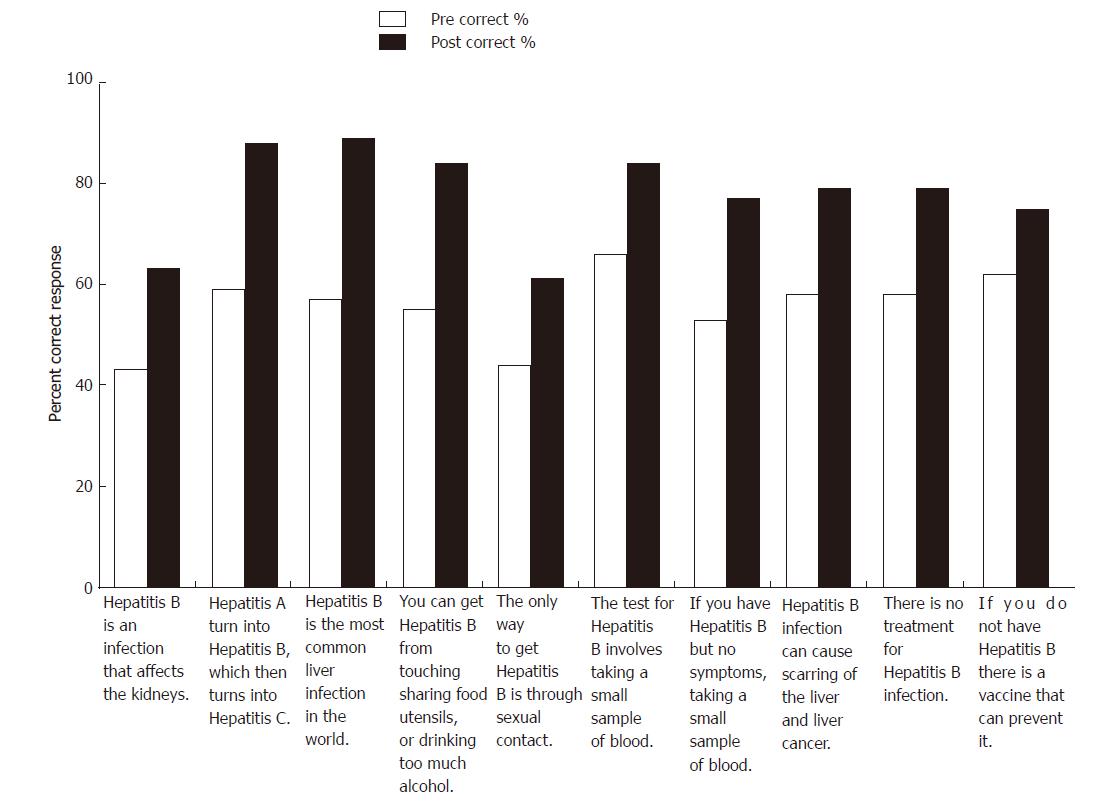
Participants were asked to answer ten true/false questions prior to (pre) and after (post) the teaching session (Figure 2, Table 4). The percentage of participants answering each true/false HBV question correctly increased following the teaching session (Figure 2, Table 4), from a mean of 5.5 (report SD) out of 10 correct answers, to a mean of 7.6 (report SD) out of 10 correct answers (P < 0.001). For the question “The only way to get HBV is through sexual contact” (false), the percentage of correct answers increased from 45 (pre) to 61 (post) (P = 0.04). For the question “If you have HBV but no symptoms, no need to worry about your liver” (false), the percentage of accurate answers increased from 53 (pre) to 77 (post) (P = 0.006). For the question “HBV can cause scarring of the liver and liver cancer” (true), the percentage of correct answers increased from 58 (pre) to 79 (post) (P = 0.01). For the question “There is no treatment for HBV” (false), the percentage increased from 50 (pre) to 66 (post), but was not statistically significant (P = 0.06). For the question “If you do not have HBV, there is a vaccine that can prevent HBV” (true), the percentage increased from 62 (pre) to 75 (post), but, again, was not statistically significant (P = 0.2).
| Variable | Pre Correct | Post correct | P value1 |
| Mean of total correct answers (Std.dev) (mean ± SD) | 5.5 ± 3.3 | 7.6 ± 2.9 | < 0.001 |
| 1 Hepatitis B is an infection that affects the kidneys | 43(43) | 35 (63) | 0.02 |
| 2 Hepatitis A turns into Hepatitis B, which then turns into Hepatitis C | 60 (59) | 49 (88) | < 0.0001 |
| 3 Hepatitis B is the most common liver infection in the world | 58 (57) | 50 (89) | < 0.0001 |
| 4 You can get hepatitis B from touching, sharing food utensils, or drinking too much alcohol | 56 (55) | 47 (84) | < 0.0001 |
| 5 The only way to get hepatitis B is through sexual contact | 44 (45) | 34 (61) | 0.04 |
| 6 The test for hepatitis B involves taking a small sample of blood | 67 (66) | 47 (84) | 0.02 |
| 7 If you have Hep B but no symptoms, no need to worry about your liver | 54 (53) | 43 (77) | 0.006 |
| 8 Hepatitis B infection can cause scarring of the liver and liver cancer | 59 (58) | 44 (79) | 0.01 |
| 9 There is no treatment for hepatitis B | 50 (50) | 37 (66) | 0.06 |
| 10 If you do not have hepatitis B, there is a vaccine that can prevent it | 65 (64) | 42 (75) | 0.20 |
Several participants from Somalia clarified that, although they were originally from Somalia, they had spent multiple years in Kenya in refugee camps prior to their arrival to the United States, disrupting both formal education and access to health care for many. Several Somali participants stated that access to vaccines prior to immigration, even when they were available at some sites in their native country, were not accessible due to political instability.
The goals of this study were to determine the baseline HBV knowledge state of at-risk immigrants in the Greater Boston Area, as well as the ability to improve HBV understanding through a brief teaching intervention. Of all immigrant populations, the highest number of participants by far was among Somali immigrants, suggesting a particular openness to seek health education and highly effective community networking (recruiting participants) within this community in Boston, likely due to the pre-existing community network established by our Somali liaison.
There were several limitations to our study. One limitation was the lack of retention of participants for the entire event, with many (45%) participants leaving before answering the post-session questionnaire. Furthermore, the sample size of this study was relatively small as this was exploratory research, and there had been no a priori calculation of a target sample size based on a specific hypothesis to be tested. The data collected in our study may help determine the design and sample size of future studies. Another limitation was language barrier, despite presence of in-person interpreters, due to the high ratio of participants per interpreter, and failure to obtain education information, which may have influenced questionnaire responses, from participants. Another limitation of this study was that the questionnaire was not validated. There was some difficulty interpreting changes in answers to open ended questions between pre- and post- teaching sessions. For example, for the open-ended question “Why is it important to test those at risk for HBV”, in the pre-session questionnaire, 24% of participants answered that HBV testing could prevent the spread of infection, whereas in the post-session questionnaire, 16% of participants answered that HBV testing could prevent spread of infection. In contrast, post session responses to this question increased for “initiate treatment early” (from 16% to 20%), and “prevent long term complications” (from 10% to 16%), indicating that participants likely shifted the focus of their answers, without any clear evidence of loss of knowledge. These results highlight the complexity of interpreting open-ended questions in a quantitative manner, an area for improvement in future studies. Another limitation is that the impact of this education intervention on longer term knowledge retention as well as accessing HBV screening is not known and should be included in a future study.
While knowledge overall improved after the teaching intervention (report the overall change score with P value), there were two areas that demonstrated more room for improvement including vaccination and treatment. During teaching sessions, it was explained that treatment for HBV exists, but is not curative, and must be taken for the long-term, rather than a discrete time course. It is possible that this description of a suppressive but not curative treatment led to confusion. Regarding vaccines, it was explained that they are effective if given prior to infection, but not if given once someone is already infected. This point was repeated several times in an attempt to clearly communicate that the simple receipt of an HBV vaccine does not eradicate HBV if a person from an endemic area was already infected. In fact, the authors note that communication of this message was one of the reasons for the study: multiple patients interactions reveal that patients often perceive that they cannot be HBV infected because they have been vaccinated, although some may have been infected before vaccination. Results of this study reveal that, while knowledge related to HBV vaccines and treatments did improve following teaching intervention, additional refinement in these areas to the teaching intervention could enhance HBV knowledge. Specifically, additional slides illustrating the populations in whom vaccine will and will not work should be included.
This study revealed that outreach events, in accessible and hospitable community venues, can provide an effective forum for HBV health teaching sessions to raise HBV awareness for at-risk immigrants in the Greater Boston Area. Events held in Health Centers may be more poorly attended, though this requires confirmation as our health center event targeted a Cambodian population, whereas our other events targeted populations of African origin. Therefore multiple factors may have influenced attendance. Baseline knowledge of HBV relation to liver disease and hepatocellular carcinoma among Greater Boston Immigrants ranged among countries of origin. Although HBV status of participants is unknown, most participants came from countries of high HBV endemicity, thus improved HBV knowledge is desirable. Our simple teaching intervention revealed a significant improvement in HBV knowledge, specifically including the information that (1) country of origin can be a factor of HBV risk; (2) HBV causes cancer; and (3) HBV infection may cause pathology long before any symptoms. As noted, a limitation of our teaching sessions was the ability to communicate efficacy of vaccines and treatments. We only observed a modest increase in participants aware that HBV treatment exists (50% to 66%). This may be related to our limitations to communicate that antiviral treatment to prevent or delay complications exists but no cure for HBV highlighting the need for additional outreach on this topic. While outreach into the community does cost money and time, the benefit of added HBV knowledge may outweigh these costs. Additional studies determining the percent of participants that present for HBV testing and, if positive, receive appropriate care would be required to confirm this. This study highlights the finding that (1) persons at-risk for HBV are living in the Greater Boston area; (2) there are important gaps in HBV baseline knowledge in the community; (3) teaching sessions in the community are greeted with warm reception and high participation numbers, particularly among Somalis; and (4) significant improvement in HBV understanding can be made with teaching sessions.
Hepatitis B virus (HBV) infection and HBV related liver disease are a major public health problem worldwide. In 2016 the World Health Organization announced the initiative “Combating hepatitis B and C to reach elimination by 2030”. However, many people at risk for HBV infection and HBV related liver complications are unaware that they are infected or unaware of HBV-related risks.
They propose that reaching the final frontier of HBV elimination requires vigorous efforts to step up HBV awareness, at the global level. Awareness serves as the first step empowering at-risk persons to seek appropriate testing and care. Awareness in a given individual may also catalyze dissemination of information throughout at-risk communities. This pilot study represents a local first step in an effort to trigger rapid and accurate dissemination of HBV knowledge among persons at risk.
This study is innovative in that we worked to disseminate HBV directly to at-risk persons working through social networks who were brought together by community liaisons. While similar work has been initiated in the greater New York City metropolitan area, by co-author Ponni Perumalswami MD, we are not aware of similar initiatives elsewhere in the United States. This study was unique in the engagement of multiple immigrant populations (Somali, Turkish, Moroccan, etc.,) simultaneously, rather than focus on any one particular group.
Practical applications of this study are the following: (1) the authors have demonstrated that a small group of health care workers can effectively increase HBV knowledge among relatively large groups of at-risk persons in community based, brief teaching sessions; and (2) they have further demonstrated that there is a significant need for these teaching sessions, as many participants from extremely high risk regions for HBV are unaware of their HBV risk. They hope that this model for HBV outreach will be directly applied by others around the globe to quickly and effectively prompt at-risk persons to seek HBV care. To underscore that intention, we have provided a “toolkit” with copies of our pre/post-session questionnaire (Figure S1) and navigator card (Figure S2) for immediate use by others toward the concerted effort of 2030 HBV Eradication.
The manuscript described a teaching session to improve understanding of hepatitis B virus infection by people in a local community. The questionnaire is well designed and the procedure properly conducted.
| 1. | Hepatitis B. World Health Organization 2017. Available from: http://www.who.int/mediacentre/factsheets/fs204/en/. |
| 2. | Bile K, Aden C, Norder H, Magnius L, Lindberg G, Nilsson L. Important role of hepatitis C virus infection as a cause of chronic liver disease in Somalia. Scand J Infect Dis. 1993;25:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Blanas DA, Nichols K, Bekele M, Shankar H, Bekele S, Jandorf L, Izzeldin S, Ndiaye D, Traore A, Bassam M. Adapting the Andersen model to a francophone West African immigrant population: hepatitis B screening and linkage to care in New York City. J Community Health. 2015;40:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Clayton-Matthews A, Watanabe P. Massachusetts Immigrants by the Numbers. Second Edition. Demographic Characteristics and Economic Footprint. In Inc. The Immigrant Learning Center (Ed.). Malden MA. 2012;. |
| 5. | Cochrane A, Collins P, Horwood JP. Barriers and opportunities for hepatitis B testing and contact tracing in a UK Somali population: a qualitative study. Eur J Public Health. 2016;26:389-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | US Department of Human and Health Services (2014-2015). Combating the Silent Epidemic of Viral Hepatitis: Action Plan for the Prevention, Care and Treatment of Viral Hepatitis. Available from: https://www.hhs.gov/ash/initiatives/hepatitis/. |
| 7. | Fitzgerald S, Chao J, Feferman Y, Perumalswami P, Sarpel U. Hepatitis B and Hepatocellular Carcinoma Screening Practices in Chinese and African Immigrant-Rich Neighborhoods in New York City. J Racial Ethn Health Disparities. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Hu DJ, Xing J, Tohme RA, Liao Y, Pollack H, Ward JW, Holmberg SD. Hepatitis B testing and access to care among racial and ethnic minorities in selected communities across the United States, 2009-2010. Hepatology. 2013;58:856-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | McCabe K, African immigrants in the United States. 2011. |
| 10. | Mitchell T, Armstrong GL, Hu DJ, Wasley A, Painter JA. The increasing burden of imported chronic hepatitis B--United States, 1974-2008. PLoS One. 2011;6:e27717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 6.9] [Reference Citation Analysis (1)] |
| 11. | GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5495] [Cited by in RCA: 5356] [Article Influence: 486.9] [Reference Citation Analysis (0)] |
| 12. | Mukhtar NA, Kathpalia P, Hilton JF, Lau G, Yu A, Grumbach K, Nguyen TT, Chan D, Khalili M. Provider, Patient, and Practice Factors Shape Hepatitis B Prevention and Management by Primary Care Providers. J Clin Gastroenterol. 2017;51:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine. 2012;30:2212-2219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1217] [Cited by in RCA: 1344] [Article Influence: 96.0] [Reference Citation Analysis (0)] |
| 14. | Perumalswami PV, Factor SH, Kapelusznik L, Friedman SL, Pan CQ, Chang C, Di Clemente F, Dieterich DT. Hepatitis Outreach Network: a practical strategy for hepatitis screening with linkage to care in foreign-born communities. J Hepatol. 2013;58:890-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Shah SA, Chen K, Marneni S, Benchekroune G, Ariganjoye R, Purswani M, Adeniyi AO, Bainbridge R, Timoney MT, Hagmann S. Hepatitis B awareness and knowledge in hepatitis B surface antigen-positive parturient immigrant women from West Africa in the Bronx, New York. J Immigr Minor Health. 2015;17:302-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Shankar H, Blanas D, Bichoupan K, Ndiaye D, Carmody E, Martel-Laferriere V, Culpepper-Morgan J, Dieterich DT, Branch AD, Bekele M. A Novel Collaborative Community-Based Hepatitis B Screening and Linkage to Care Program for African Immigrants. Clin Infect Dis. 2016;62 Suppl 4:S289-S297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Shire AM, Sandhu DS, Kaiya JK, Oseini AM, Yang JD, Chaiteerakij R, Mettler TA, Giama NH, Roberts RO, Therneau TM. Viral hepatitis among Somali immigrants in Minnesota: association of hepatitis C with hepatocellular carcinoma. Mayo Clin Proc. 2012;87:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (5)] |
| 18. | Sriphanlop P, Jandorf L, Kairouz C, Thelemaque L, Shankar H, Perumalswami P. Factors related to hepatitis B screening among Africans in New York City. Am J Health Behav. 2014;38:745-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Dourakis SP, Guan YS, Sporea I, Wang L S- Editor: Qi Y L- Editor: A E- Editor: Ma YJ