Published online Sep 21, 2017. doi: 10.3748/wjg.v23.i35.6546
Peer-review started: June 19, 2017
First decision: July 17, 2017
Revised: July 31, 2017
Accepted: August 25, 2017
Article in press: August 25, 2017
Published online: September 21, 2017
Processing time: 96 Days and 14.8 Hours
Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic ga-strostomy. It involves the internal fixation device, or “bumper”, migrating into the gastric wall and subsequent mucosal overgrowth. We described a case series of four patients with BBS treated with a novel endoscopic technique using a HookKnife between June 2016 and February 2017. The HookKnife is a rotating L-shaped cutting wire designed for hooking tissue and pulling it away from the gastric wall towards the lumen. The technique was successful in all four cases with no complications. Each patient was discharged on the day of treatment. The HookKnife is a manoeuvrable, safe and effective device for endoscopic removal of buried bumpers and could avoid surgery in a high risk group of patients. To our knowledge this technique has not been described previously. We suggest that this technique should be added to the treatment algorithms for managing BBS.
Core tip: This letter to the editor describes a case series of four patients who underwent a novel endoscopic technique for managing buried bumper syndrome using the Olympus HookKnife. This technique was successful in all four patients and no complications were recorded. We propose that this technique may be a safe and effective treatment for buried bumper syndrome in percutaneous endoscopic gastrostomy feeding.
- Citation: Wolpert LE, Summers DM, Tsang A. Novel endoscopic management of buried bumper syndrome in percutaneous endoscopic gastrostomy: The Olympus HookKnife. World J Gastroenterol 2017; 23(35): 6546-6548
- URL: https://www.wjgnet.com/1007-9327/full/v23/i35/6546.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i35.6546
We enjoyed Cyrany et al[1] article on “Buried bumper syndrome : A complication of percutaneous endoscopic gastrostomy”. Buried bumper syndrome (BBS) is an uncommon but serious complication of percutaneous endoscopic gastrostomy (PEG) with an incidence of 0.3%-2.4% per PEG patient year[1]. Symptoms include inability to insert the PEG tube, loss of patency and leakage from the PEG.
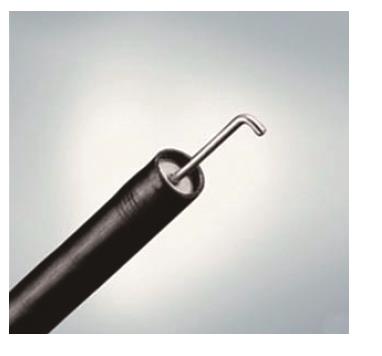
Here, we describe a case series of four patients with BBS treated with a novel endoscopic technique using a HookKnife (Olympus EndoTherapy) (Figure 1). The HookKnife is a rotating L-shaped cutting wire designed for hooking tissue and pulling it away from the gastric wall towards the lumen[2] and intended for use in colonic polypectomies. Other applications have been described in the literature; Oyama et al[3] describe a technique whereby the HookKnife was used to endoscopically resect lymph node metastases of gastric and oesophageal mucosal cancer.
Three patients were referred to our centre by their general practitioner due to inflammation around the PEG site and an inability to advance the PEG tube. The fourth patient was referred after their original PEG had stopped functioning and a new PEG had been inserted by the medical team. Patients were selected for treatment following referral for suspected BBS which was then evaluated by endoscopy. The patients ranged in age from 28 to 61 and had PEG placement for multiple sclerosis, Huntington’s disease, cerebral palsy and tetraplegia. Two patients underwent the procedure in theatre under general anaesthetic whilst the other two underwent the procedure in endoscopy under sedation.
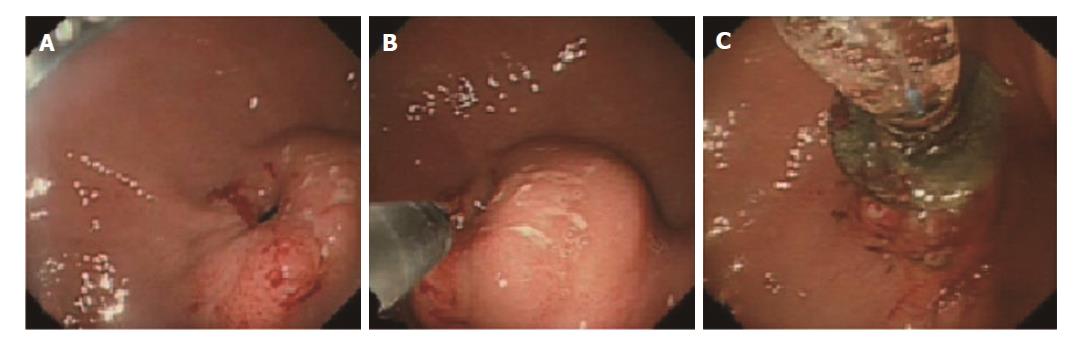
In each case the external PEG tubing was cut short to around 5 cm from the abdominal wall. A 15 mm through-the-scope dilation balloon was passed externally via the PEG tubing and inflated to dilate the mucosal orifice. A mucosal orifice was visible in all the patients in this case series. If a mucosal orifice cannot be clearly visualised then it may be found using the balloon catheter tip inserted externally. If there is no orifice then the mucosa can be cut over the bumper to create an orifice. After dilating the mucosal orifice using the TTS balloon the HookKnife was deployed to incise the gastric mucosa over the buried bumper by hooking the tissue, pulling it towards the lumen and then cutting it using diathermy under direct vision. The balloon was then re-inflated inside the tubing at the level of the PEG bumper to stiffen the PEG system (Figure 2), and both the tubing and balloon catheter clamped together using artery forceps. Short, but firm, controlled pressure was applied towards the gastric lumen to force the bumper into the stomach. The PEG was then removed using a standard technique. In one case a new PEG had already been placed prior to the procedure. In the other 3 cases, a new PEG was placed during the procedure. There were no complications and all four patients were discharged on the day of treatment.
The HookKnife is a manoeuvrable, safe and effective device for endoscopic removal of buried PEG bumpers. There are several benefits of the HookKnife technique. First, compared with techniques that rely on incising the mucosa towards the gastric wall, such as the needle knife technique and papillotome technique discussed in Cyrany et al[1],the HookKnife allows elevation of the gastric mucosa away from the bumper as the mucosal tissue can be hooked using the knife and pulled towards the lumen[2] . This additional level of control allows a more precise incision, more accurate evaluation of the depth of the bumper migration and reduces the risk of inadvertent gastric perforation as the mucosa is cut by pulling it towards the lumen as opposed to cutting towards the gastric wall. Second, the HookKnife could avoid surgery and could therefore be suitable for high risk patients. As this technique can be performed as a day case it avoids the need for an overnight stay in hospital. Finally, none of the patients in this case series experienced bleeding, which was a frequent complication in patients who underwent the needle knife technique[1]. Adequate haemostasis was achieved by using the knife on a coagulation setting of 10-30 watts and by not pulling the hook too quickly. To our knowledge, this technique has not been described previously and we suggest that this technique should be added to the treatment algorithms for the management of BBS[4]. However, as only a small number of cases are included in this series larger numbers of patients may need to be included to establish whether the HookKnife is a safe and effective method of endoscopic removal of buried bumpers. A possible limitation of this method of BBS removal is that it relies on a subjective assessment of the depth that the bumper is buried.
| 1. | Cyrany J, Rejchrt S, Kopacova M, Bures J. Buried bumper syndrome: A complication of percutaneous endoscopic gastrostomy. World J Gastroenterol. 2016;22:618-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 83] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (9)] |
| 2. | Olympus. HookKnife Electrosurgical Knife. Available from: http://medical.olympusamerica.com/products/knives/hookknife-upper-length-kd-620lr. |
| 3. | Oyama T, Kikuchi Y. Aggressive endoscopic mucosal resection in the upper GI tract-Hook knife EMR method. Minim Invasive Ther Allied Technol. 2002;11:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 118] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 4. | British Association for Parenteral and Enteral Nutrition. Percutaneous endoscopic gastrostomy management of buried bumper syndrome-decision tree. BAPEN 2012.. . |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Imaeda H, Kawahara H, Kim GH, Konishi H, Trevisani L, Velayos B, Wong K S- Editor: Qi Y L- Editor: A E- Editor: Ma YJ