Published online Aug 21, 2017. doi: 10.3748/wjg.v23.i31.5739
Peer-review started: April 12, 2017
First decision: May 12, 2017
Revised: May 29, 2017
Accepted: July 12, 2017
Article in press: July 12, 2017
Published online: August 21, 2017
Processing time: 130 Days and 12.4 Hours
To evaluate early and late outcomes of endoscopic papillary large balloon dilation (EPLBD) with minor endoscopic sphincterotomy (mEST) for stone removal.
A total of 149 consecutive patients with difficult common bile duct (CBD) stones (diameter ≥ 10 mm or ≥ 3 stones) underwent conventional endoscopic sphincterotomy (EST) or mEST plus EPLBD from May 2012 to April 2016. Their demographic, laboratory and procedural data were collected, and pancreaticobiliary complications were recorded.
Sixty-nine (94.5%) of the patients in the EPLBD + mEST group and 64 (84.2%) in the conventional EST group achieved stone clearance following the first session (P = 0.0421). The procedure time for EPLBD + mEST was shorter than for EST alone (42.1 ± 13.6 min vs 47.3 ± 11.8 min, P = 0.0128). The overall rate of early complications in the EPLBD + mEST group (11%) was lower than in the EST group (21.1%); however, the difference was not significant (P = 0.0938). The cumulative recurrence rate of cholangitis and CBD stones between the two groups was also similar. The procedure time was independently associated with post-endoscopic retrograde cholangiopancreatography pancreatitis (OR = 6.374, 95%CI: 1.193-22.624, P = 0.023), CBD stone diameter ≥ 16 mm (OR = 7.463, 95%CI: 2.705-21.246, P = 0.0452) and use of mechanical lithotripsy (OR = 9.913, 95%CI: 3.446-23.154, P = 0.0133) were independent risk factors for stone recurrence.
EPLBD with mEST is more effective than EST alone for difficult CBD stone removal, with shorter procedure time and fewer early complications.
Core tip: This is a retrospective comparative study to investigate the efficacy and safety of endoscopic papillary large balloon dilation (EPLBD) with minor endoscopic sphincterotomy (mEST) for the removal of difficult common bile duct stones. EPLBD + mEST was found to be more effective than conventional endoscopic sphincterotomy alone for difficult stone removal, with shorter procedure time and potentially fewer early complications.
- Citation: Xu XD, Chen B, Dai JJ, Qian JQ, Xu CF. Minor endoscopic sphincterotomy followed by large balloon dilation for large choledocholith treatment. World J Gastroenterol 2017; 23(31): 5739-5745
- URL: https://www.wjgnet.com/1007-9327/full/v23/i31/5739.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i31.5739
Endoscopic retrograde cholangiopancreatography (ERCP) combined with endoscopic sphincterotomy (EST) is now widely accepted as the first-line procedure for treatment of choledocholithiasis[1]. Stone extraction with EST is successful in > 90% of cases, but adverse events such as bleeding, perforation, pancreatitis and cholangitis occur in 5%-10% of patients, with a mortality rate of < 1%[2,3]. Endoscopic papillary balloon dilation (EPBD; with a 6-mm to 10-mm dilating balloon) with conventional EST, was regarded as a safer and easier option than EST alone in patients with coagulopathy, Billroth II anastomosis, or periampullary diverticulum because of the lower risk of bleeding and perforation, as well as preservation of sphincter of Oddi function[4-8].
In patients with difficult common bile duct (CBD) stones (diameter ≥ 10 mm or ≥ 3 stones), EPBD limits the extent of orifice dilation to a diameter of ≤ 10 mm; as such, mechanical lithotripsy (MLT) is more frequently required to facilitate stone extraction, and this adjunct procedure is associated with a higher risk of post-ERCP pancreatitis (PEP)[9-12]. Recent studies have reported that endoscopic papillary large balloon dilation (EPLBD), as an extension of EPBD, might be effective for removal of difficult stones[13-16]. However, these studies were based on different definitions and few have focused on late outcomes.
Thus, we carried out a retrospective comparative study to investigate the efficacy and safety of EPLBD with minor (m)EST for the removal of difficult CBD stones.
Patients receiving ERCP for the removal of CBD stones at our hospital between May 2012 and April 2016 were included in this study. Inclusion criteria were as follows: (1) age ≥ 18 years; (2) maximum stone diameter ≥ 10 mm or ≥ 3 stones; and (3) diameter of the distal common bile duct ≥ 12 mm. Exclusion criteria were: (1) pre-existing acute pancreatitis; (2) previous ERCP-related procedures; (3) presence of intrahepatic duct stones, distal bile duct strictures or malignant biliary obstruction; and (4) coagulopathy with platelet count < 50000/mL or anticoagulation therapy within 1 wk. Patients’ medical records, laboratory tests, imaging findings, and records of ERCP were reviewed.
All ERCP-related procedures were performed according to a standardized protocol by three endoscopy specialists, each with > 15 years of ERCP experience, using a side-viewing duodenoscope (TJF-260; Olympus, Tokyo, Japan) with a large accessory channel. Local anesthesia of the pharynx was required using 10% xylocaine and intramuscular injection of 40 mg hyoscine butylbromide, and 50-100 mg meperidine was administered as premedication. EST or EPLBD + mEST were chosen at the discretion of the endoscopists for stone removal.
EST was performed according to the conventional method. mEST was performed proximally from the orifice of the papilla, but did not extend beyond the horizontal fold or the transverse fold of the papilla. EPLBD was performed following mEST and using a dilating balloon (CRE balloon 5.5 cm long, 12-20 mm diameter; Boston Scientific, Boston, MA, United States). The diameter of the balloons was set at 12-20 mm based on the size of the stones and distal bile duct. The balloon was then filled gradually with diluted contrast medium under endoscopic and fluoroscopic guidance, to observe the gradual disappearance of the waist in the balloon. Once the waist disappeared, the balloon remained inflated for 60 s before stone extraction.
Complete stone removal was determined by final cholangiography. An endoscopic nasobiliary drainage catheter (7.5 Fr; Boston Scientific) was inserted routinely following endoscopic clearance of the CBD stones. It was withdrawn at 48 h after ERCP if no remnant stones were visualized by magnetic resonance cholangiopancreatography after improvement of symptoms and abnormal laboratory values. Initial success was defined as complete CBD stone removal when only one session of the stone removal procedure was performed independent of MLT use; otherwise, a second session of ERCP was performed to retrieve the remnant stones. All patients enrolled were hospitalized and received antibiotics routinely following ERCP.
Complications were evaluated according to the 1991 consensus guidelines[17]. PEP was defined as abdominal pain with at least a 3-fold elevation of serum amylase > 24 h after the procedure that required treatment for > 2 d. Post-ERCP cholangitis was defined as a fever higher than 38 °C lasting > 48 h due to biliary causes. Post-ERCP hemorrhage was defined as mild when there was a decrease in hemoglobin level, moderate when transfusion was required (< 4 U) and severe when > 5 U was needed or when intervention was required.
Each patient who received ERCP procedures in our hospital was followed up routinely. They were interviewed by telephone or advised to visit our outpatient clinic after discharge. If there was any suspicion of recurrence during follow-up, liver function tests and imaging studies were performed. Patients with recurrent pancreaticobiliary complications treated with or without ERCP-related procedures, patients with gallstones undergoing cholecystectomy, or patients who had died were all recorded in our database with SPSS software (SPSS Inc., Chicago, IL, United States).
Statistical analysis was performed on an intention-to-treat basis with SPSS version 20.0. For analysis of categorical data, a χ2 test with a Yates correction, or Fisher’s exact test was used. A normality test was applied for continuous data, which were then analyzed with Student’s t or Mann-Whitney U test. Patient characteristics are expressed as mean ± SD or as percentages. All statistical tests were two-tailed and the threshold for statistical significance was set at P < 0.05. It was assumed that 90% of cases would achieve stone clearance, and a 20% decrease in clearance rate was considered to be clinically significant. Fisher’s exact two-sided test was performed to detect a significant difference (α = 0.05) for a sample of 126 patients (63 in each group) with 80% power.
From May 2012 to April 2016, 879 consecutive patients who underwent ERCP procedures in our hospital were reviewed and 149 fulfilled the inclusion criteria of the current study. Of these, 73 patients were treated with EPLBD + mEST for CBD stone removal, while the other 76 were treated with EST alone. The mean diameter of CBD stones was 15.7 mm (range: 10.0-21.1 mm).
The two groups showed no significant difference in baseline characteristics. Laboratory and imaging findings were also similar between the two groups (Table 1). CBD stone clearance was successfully performed in all patients (Table 2). Sixty-eight (93.2%) of the patients in the EPLBD + mEST group achieved stone clearance without MLT, as well as 62 (81.6%) in the EST group (P = 0.0343). Sixty-nine (94.5%) of the patients in the EPLBD + mEST group and 64 (84.2%) in the EST group achieved stone clearance following the first session (P = 0.0421) and the procedure time of EPLBD + mEST was shorter than EST alone (42.1 ± 13.6 min vs 47.3 ± 11.8 min, P = 0.0128). Duration of hospital stay following ERCP was similar between the two groups (5.1 ± 2.2 d vs 5.7 ± 1.9 d, P = 0.0753). Early and late complications are listed in Table 2, and there were no differences between the two groups (11.0% vs 21.1%, P = 0.0938) in early complications. Six (8.2%) of the patients in the EPLBD + mEST group and 7 (9.2%) in the control group had PEP (P = 0.8303). All cases of PEP were mild and recovered after conservative treatment. More patients had intraprocedural hemorrhage in the EST (7.9%) group than in the EPLBD + mEST group (1.4%), although there was no significant difference (P = 0.1351). Additionally, serious complications such as perforation, post-procedural hemorrhage, or severe pancreatitis were not observed in any patient.
| Variable | EPLBD + mEST | EST | P value |
| n = 73 | n = 76 | ||
| Age in yr | 59.7 ± 12.4 | 62.1 ± 13.7 | 0.2647 |
| Sex, male/female | 47/26 | 45/31 | 0.5160 |
| Cholecystolithiasis | 22 (30.1) | 19 (25) | 0.4828 |
| Cirrhosis | 5 (6.8) | 6 (7.9) | 0.8073 |
| History of cholecystectomy | 7 (9.6) | 7 (9.2) | 0.9369 |
| Periampullary diverticulum | 9 (12.3) | 11 (14.5) | 0.7010 |
| Billroth II gastrectomy | 2 (2.7) | 3 (3.9) | 0.9635 |
| AMY in U/L | 84.1 ± 21.9 | 90.1 ± 24.3 | 0.1160 |
| TB in mg/dL | 4.9 ± 2.1 | 5.3 ± 2.6 | 0.3007 |
| ALT in IU/L | 121.8 ± 27.6 | 117.3 ± 37.2 | 0.4005 |
| AST in IU/L | 91.1 ± 27.7 | 95.6 ± 31.3 | 0.3550 |
| PT in s | 11.2 ± 2.1 | 11.7 ± 2.3 | 0.1684 |
| PC as × 106/L | 157.2 ± 31.3 | 158.1 ± 31.2 | 0.8896 |
| Maximum CBD diameter in mm | 17.5 ± 4.6 | 18.1 ± 5.7 | 0.4817 |
| Maximum stone diameter in mm | 16.9 ± 4.1 | 16.5 ± 4.7 | 0.5813 |
| CBD stones | 2.9 ± 1.1 | 2.3 ± 1.9 | 0.4354 |
| Outcome | EPLBD + mEST | EST | P value |
| n = 73 | n = 76 | ||
| Stone removal succeeded without MLT | 68 (93.2) | 62 (81.6) | 0.0343 |
| Procedure time in min | 42.1 ± 13.6 | 47.3 ± 11.8 | 0.0128 |
| Initial success | 69 (94.5) | 64 (84.2) | 0.0421 |
| Overall success | 73 (100) | 76 (100) | - |
| ENBD placement time in d | 2.6 ± 0.7 | 2.5 ± 0.6 | 0.3990 |
| Duration of hospital stay in d | 5.1 ± 2.2 | 5.7 ± 1.9 | 0.0753 |
| Early complications | 8 (11.0) | 16 (21.1) | 0.0938 |
| PEP | 6 (8.2) | 7 (9.2) | 0.8303 |
| Mild | 6 | 7 | 0.8303 |
| Moderate | 0 | 0 | - |
| Severe | 0 | 0 | - |
| Cholangitis | 1 (1.4) | 3 (4.0) | 0.6411 |
| Hemorrhage | 0 | - | |
| Intraprocedural | 1 (1.4) | 6 (7.9) | 0.1351 |
| Post-procedural | 0 | 0 | - |
| Perforation | 0 | 0 | - |
| Late complications | 4 (5.5) | 4 (5.2) | 0.7604 |
| Recurrence of cholangitis | 0 | 1 (1.3) | 1.0000 |
| Recurrence of CBD stones | 4 (5.5) | 3 (3.9) | 0.9565 |
| CBD stricture | 0 | 0 | - |
| Duration of follow-up in mo | 14.1 ± 5.5 | 12.9 ± 5.5 | 0.2140 |
| Cholecystectomy | 5 (6.8) | 7 (9.2) | 0.5965 |
| Loss to follow-up | 0 | 0 | - |
| Death | 0 | 0 | - |
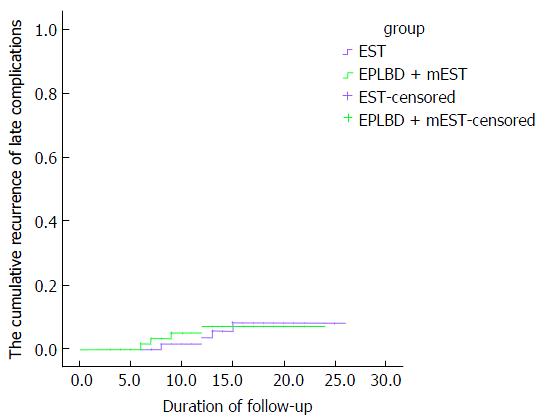
The median follow-up duration was 13.5 mo (range: 3-26 mo) for all patients, and there was no significant difference between the two groups (Table 2). There was no death or loss to follow-up. Cholecystectomy was performed in 5 (6.8%) patients in the EPLBD + mEST group and 7 (9.2%) in the EST group (P = 0.5965). The overall rate of late complications was similar between the two groups (5.5% vs 5.2%, P = 0.7604). There was only 1 patient in the EST group (1.3%) who experienced recurrence of cholangitis during follow-up. A total of 7 patients, 4 (5.5%) in the EPLBD + mEST group and 3 (3.9%) in the EST group (P = 0.9565), had CBD stone recurrence and were treated again by ERCP. The cumulative recurrence rate of cholangitis and CBD stones between the two groups did not differ significantly (log rank, P = 0.859; Figure 1).
According to PEP and stone recurrence, which comprised the majority of early and late complications, patients were divided into two subgroups: those who developed PEP (PEP group, n = 13; No-PEP group, n = 136) or recurrence of CBD stones (Stone recurrence group, n = 7; No-stone recurrence group, n = 142). Univariate and multivariate logistic regression analyses were performed to identify independent risk factors. Compared to the No-PEP group, significantly longer procedure times (51.3 ± 11.7 min vs 43.6 ± 12.5 min, P = 0.0346) and CBD stone diameters ≥ 16 mm (53.8% vs 16.9%, P = 0.0049) were observed in the PEP group (Table 3). Further analysis with multivariate logistic regression indicated that the procedure time was independently associated with PEP (OR = 6.374, 95%CI: 1.193-22.624, P = 0.023). For stone recurrence, maximum stone diameter (19.9 ± 7.7 mm vs 15.3 ± 5.1 mm, P = 0.0246), patients whose CBD stone diameter was ≥ 16 mm (57.1% vs 18.3%, P = 0.0435) and use of MLT (57.1% vs 10.6%, P = 0.0053) were significantly different between the two subgroups. CBD stone diameter ≥ 16 mm (OR = 7.463, 95%CI: 2.705-21.246, P = 0.0452) (Table 3) and MLT (OR = 9.913, 95%CI: 3.446-23.154, P = 0.0133) were independent risk factors for stone recurrence.
| Variable | PEP | No-PEP | P value | Stone recurrence n = 7 | No-stone recurrence n =142 | P value |
| n =13 | n =136 | |||||
| Age in yr | 60.3 ± 10.7 | 61.1 ± 11.3 | 0.8069 | 59.6 ± 11.4 | 60.7 ± 9.9 | 0.7760 |
| Sex, male/female | 8/5 | 84/52 | 0.7775 | 5/2 | 87/55 | 0.8873 |
| Cholecystolithiasis | 2 (15.4) | 39 (28.7) | 0.4838 | 1 (14.3) | 40 (28.2) | 0.7118 |
| History of cholecystectomy | 1 (7.7) | 13 (9.6) | 0.7817 | 1 (14.3) | 14 (9.9) | 0.5319 |
| Periampullary diverticulum | 0 | 20 (14.7) | 0.2891 | 2 (28.6) | 18 (12.7) | 0.2378 |
| Billroth II gastrectomy | 1 (7.7) | 4 (2.9) | 0.3706 | 0 | 5 (3.5) | 1.0000 |
| Procedure time in min | 51.3 ± 11.7 | 43.6 ± 12.5 | 0.0346 | 50.1 ± 10.8 | 48.1 ± 11.1 | 0.6420 |
| Maximum CBD diameter in mm | 17.1 ± 5.3 | 16.7 ± 4.9 | 0.7804 | 18.7 ± 8.1 | 16.7 ± 7.7 | 0.5043 |
| Maximum stone diameter in mm | 17.3 ± 5.1 | 16.9 ± 6.1 | 0.8194 | 19.9 ± 7.7 | 15.3 ± 5.1 | 0.0246 |
| ≥ 16 | 7 (53.8) | 23 (16.9) | 0.0049 | 4 (57.1) | 26 (18.3) | 0.0435 |
| ≥ 22 | 2 | 3 | 0.0607 | 1 (14.3) | 4 (2.8) | 0.2165 |
| No. of CBD stones | 2.4 ± 1.2 | 2.2 ± 1.0 | 0.4995 | 2.1 ± 1.1 | 1.9 ± 1.0 | 0.6071 |
| MLT performed | 3 (23.1) | 16 (11.7) | 0.4635 | 4 (57.1) | 15 (10.6) | 0.0053 |
| Dilating procedure performed | 6 (46.2) | 67 (49.3) | 0.8303 | 4 (57.1) | 69 (48.6) | 0.6586 |
| ENBD placement time in d | 2.3 ± 0.5 | 2.6 ± 0.7 | 0.0960 | 2.8 ± 0.7 | 2.6 ± 0.7 | 0.5010 |
Since 2003, there have been a series of studies demonstrating the safety and efficacy of EPLBD with a preceding EST, for removal of CBD stones[10,18,19]. However, it is difficult to make an accurate judgment because some technical criteria mentioned in these studies differed, such as the extent of EST, balloon dilation protocol and CBD stone size. Additionally, most of the studies only focused on early complications of these procedures, but not on the late complications.
In the current study, stone clearance was performed successfully in all patients and the results were similar to those in a recent review[20]. That review showed that the initial success rate was also similar between the two groups; however, that was not confirmed by the current study, which showed a higher initial success rate in the EPLBD + mEST group compared with the EST group. Also, the initial success rates of both groups were higher than that reported by the review (EPLBD + EST group: 87% vs EST group: 79%). It is hard to explain this discrepancy because success rates of stone removal are usually associated with the experience of the endoscopist, condition of the patient, shape and size of the CBD stones, time and size of the dilating balloon, and extent of the EST.
Nevertheless, according to our study, large balloon dilation along with mEST facilitated difficult CBD stone removal and could significantly shorten the procedure time (EPLBD + mEST group: 42.1 ± 13.6 min vs EST group: 47.3 ± 11.8 min). A total of 19 patients who failed stone clearance using a Dormia basket or balloon catheter had to undergo MLT. In this study, we also found a significantly lower rate of MLT usage when comparing the EPLBD + mEST group with the control group (EPLBD + EST group: 6.8% vs EST group: 18.4%), and the results were similar to those in the previous review[20]. MLT has proven to be a time-consuming and a challenging technique with related adverse events, such as basket impaction and bile duct injury. The extended ampullary orifice made by EPLBD facilitates difficult CBD stone extraction and it might reduce the need for MLT if EPLBD was used after EST, as compared to EST alone. We found a significantly shorter procedure time in the EPLBD + mEST group than in the EST group. Decreased procedure time indicates a decrease in radiation exposure, which is associated with a reduction in the risk of post-ERCP complications[21].
In the current study, the overall rate of early complications in the EPLBD + mEST group (11%) was lower than that in the EST group (21.1%), although the difference was not significant. PEP, which is the major early complication of ERCP, is closely related to the EPBD procedure[11]. However, it was not confirmed in the current study, in which PEP occurred in 8.2% patients in the EPLBD + mEST group and 9.2% in the EST group, and both the incidence and severity were similar. Further analysis demonstrated that the procedure time and CBD stone diameter ≥ 16 mm were associated with PEP. In the current study, balloon dilation of the orifice failed to demonstrate an increased incidence of PEP, as had been noted previously[22-24]. It appears that, with a preceding EST, the dilating force of the balloon is more accurate in the direction of the sphincterotomy, away from the pancreatic duct orifice, and this reduces the likelihood of PEP.
Previous studies have shown a high incidence of hemorrhage (8.3%-9%) during full EST before EPLBD[10,12]. One of the key purposes for developing EPBD was to minimize the risk of hemorrhage by avoiding sphincterotomy. In the current study, the incidence of hemorrhage was controlled to a low level (1.4%) with limited sphincterotomy followed by EPLBD, which was lower than 7.9 in the EST group. However, the difference was not significant. All bleeding complications in this study were mild and easily controlled using argon-plasma coagulation, epinephrine spray, or compression by the balloon. The incidence of cholangitis (1.4% vs 4%) was also comparable and there was no perforation in any patient.
To date, few studies have looked beyond the early complications of EPLBD + EST, paying attention to either mid- or long-term outcomes. Recently, a Greek research team prospectively evaluated the 4-year outcomes of a multicenter randomized trial of EPLBD + EST and found an overall low risk (7.5%) of recurrent CBD stones[25]. They reported that most stone recurrence occurred within the first 2.5 or 3.5 year following stone removal, and the mean interval between ERCP and recurrence of CBD stones was 37.5 ± 5.7 mo (range: 28-42 mo). In our study, 7 patients, 4 (5.5%) in the EPLBD + mEST group and 3 (3.9%) in the EST group, had CBD stone recurrence during follow-up. The incidence was lower than that of the Greek study, which could be because of the short follow-up period in the current study. CBD stone diameter ≥ 16 mm and MLT were found to be independent risk factors for stone recurrence. This explained why MLT was more frequently used with larger stones and increased the risk of recurrence because even a few missed tiny stone fragments may act as a nidus for stone reaggregation[26].
Nevertheless, all the patients enrolled were in a single center and the retrospective nature of the study could bring potential biases in the selection of patients and procedures. Furthermore, large, prospective randomized comparative studies are necessary to evaluate the significant differences between EPLBD + mEST and EST for difficult CBD stone removal.
In conclusion, EPLBD with mEST was more effective than EST alone for difficult CBD stone removal, with a shorter procedure time, reduced use of MLT, and the potential to reduce early complications.
Endoscopic sphincterotomy (EST) is the standard method for enlarging the bile duct opening in the duodenum before stone removal during endoscopic retrograde cholangiopancreatography (ERCP). Although EST is effective, it permanently destroys the biliary sphincter. Endoscopic papillary balloon dilation (EPBD; with a 6-mm to 10-mm dilating balloon) is an alternative technique to enlarge the papillary orifice for stone retrieval, with the potential advantage of biliary sphincter function preservation. However, in patients with difficult common bile duct (CBD) stones (diameter ≥ 10 mm or ≥ 3 stones), EPBD limits the extent of orifice dilation to a diameter of ≤ 10 mm. Thus, mechanical lithotripsy is more frequently required and it is believed to be associated with a higher risk of post-ERCP pancreatitis (PEP).
Minor (m)EST followed by endoscopic papillary large balloon dilation (EPLBD) might be more effective for removal of difficult CBD stones. However, previous studies were ambiguous in their definitions and tended to neglect long-term outcomes, and the conclusions were inconsistent. In the current study, technical criteria, such as the extent of EST and balloon dilation protocol were all precisely defined and both early and late outcomes were observed.
In the current study, more patients in the EPLBD + mEST group achieved stone clearance following the first session and the procedure time was shorter than for EST alone. The procedure time was independently associated with PEP. The cumulative recurrence rate of cholangitis and CBD stones was similar between the two groups. CBD stone diameter ≥ 16 mm and use of mechanical lithotripsy were independent risk factors for stone recurrence.
This study suggests that the EPLBD + mEST combination was a better choice for difficult CBD stone removal, having shorter procedure time and the potential to reduce development of early complications.
PEP is defined as abdominal pain with at least a 3-fold elevation of serum amylase > 24 h after the procedure that requires treatment for > 2 d. Post-ERCP hemorrhage was defined as mild when there was a decrease in hemoglobin level, moderate when transfusion was required (< 4 U), and severe when > 5 U blood transfusion was needed or when intervention was required.
This is an interesting paper. It would be interesting to know how much time the effects of sphincter dilatation persist. This could be evaluated with imaging controls.
| 1. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 291] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 2. | Kim TH, Kim JH, Seo DW, Lee DK, Reddy ND, Rerknimitr R, Ratanachu-Ek T, Khor CJ, Itoi T, Yasuda I. International consensus guidelines for endoscopic papillary large-balloon dilation. Gastrointest Endosc. 2016;83:37-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Carr-Locke DL. Therapeutic role of ERCP in the management of suspected common bile duct stones. Gastrointest Endosc. 2002;56:S170-174. [DOI] [Full Text] |
| 4. | Kawabe T, Komatsu Y, Tada M, Toda N, Ohashi M, Shiratori Y, Omata M. Endoscopic papillary balloon dilation in cirrhotic patients: removal of common bile duct stones without sphincterotomy. Endoscopy. 1996;28:694-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 77] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrecyomy. Gastrointest Endosc. 2001;53:19-26. [RCA] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 101] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Lin CK, Lai KH, Chan HH, Tsai WL, Wang EM, Wei MC, Fu MT, Lo CC, Hsu PI, Lo GH. Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig Liver Dis. 2004;36:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Yasuda I, Tomita E, Enya M, Kato T, Moriwaki H. Can endoscopic papillary balloon dilation really preserve sphincter of Oddi function? Gut. 2001;49:686-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 158] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Takezawa M, Kida Y, Kida M, Saigenji K. Influence of endoscopic papillary balloon dilation and endoscopic sphincterotomy on sphincter of oddi function: a randomized controlled trial. Endoscopy. 2004;36:631-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Mac Mathuna P, White P, Clarke E, Lennon J, Crowe J. Endoscopic sphincteroplasty: a novel and safe alternative to papillotomy in the management of bile duct stones. Gut. 1994;35:127-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 214] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 263] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 13. | Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720-726; quiz 768, 771. [PubMed] |
| 14. | Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Kim HG, Cheon YK, Cho YD, Moon JH, Park DH, Lee TH, Choi HJ, Park SH, Lee JS, Lee MS. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298-4304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 74] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341-345.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 17. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2086] [Article Influence: 59.6] [Reference Citation Analysis (2)] |
| 18. | Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc. 2011;25:3330-3337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW Jr, Bhattacharya K, Gupta K, Freeman ML, Sherman S, McHenry L, Watkins JL, Fogel EL, Schmidt S, Lehman GA. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 126] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 20. | Madhoun MF, Wani S, Hong S, Tierney WM, Maple JT. Endoscopic papillary large balloon dilation reduces the need for mechanical lithotripsy in patients with large bile duct stones: a systematic review and meta-analysis. Diagn Ther Endosc. 2014;2014:309618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Meine GC, Baron TH. Endoscopic papillary large-balloon dilation combined with endoscopic biliary sphincterotomy for the removal of bile duct stones (with video). Gastrointest Endosc. 2011;74:1119-1126; quiz 1115.e1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Misra SP, Dwivedi M. Endoscopic papillary balloon dilation for choledocholithiasis: does it have a future? Endoscopy. 1999;31:211-212. [PubMed] |
| 23. | Vlavianos P, Chopra K, Mandalia S, Anderson M, Thompson J, Westaby D. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut. 2003;52:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 91] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 244] [Article Influence: 11.1] [Reference Citation Analysis (1)] |
| 25. | Paspatis GA, Paraskeva K, Vardas E, Papastergiou V, Tavernaraki A, Fragaki M, Theodoropoulou A, Chlouverakis G. Long-term recurrence of bile duct stones after endoscopic papillary large balloon dilation with sphincterotomy: 4-year extended follow-up of a randomized trial. Surg Endosc. 2017;31:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763-2767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Manenti A S- Editor: Qi Y L- Editor: Filipodia E- Editor: Huang Y