Published online Apr 14, 2017. doi: 10.3748/wjg.v23.i14.2625
Peer-review started: November 2, 2016
First decision: January 19, 2017
Revised: January 22, 2017
Accepted: February 16, 2017
Article in press: February 16, 2017
Published online: April 14, 2017
Processing time: 163 Days and 7 Hours
To investigate the incidence and mortality rates of upper gastrointestinal cancer (UGIC) in Hebei Province, China, and to identify high-risk populations to improve UGIC prevention and control.
Data for UGIC patients were collected from 21 population-based cancer registries covering 15.25% of the population in Hebei Province. Mortality data were extracted from three national retrospective death surveys (1973-1975, 1990-1992 and 2004-2005). The data were stratified by 5-year age groups, gender and area (high-risk/non-high-risk areas) for analysis. The age-period-cohort and grey system model were used.
The crude incidence rate of UGIC was 55.47/100000, and the adjusted rate (Segi’s population) was 44.90/100000. Males in rural areas had the highest incidence rate (world age-standardized rate = 87.89/100000). The crude mortality rate of UGIC displayed a decreasing trend in Hebei Province from the 1970s to 2013, and the adjusted rate decreased by 43.81% from the 1970s (58.07/100000) to 2013 (32.63/100000). The mortality rate declined more significantly in the high-risk areas (57.26%) than in the non-high-risk areas (55.02%) from the 1970s to 2013. The median age at diagnosis of UGIC was 65.06 years in 2013. There was a notable delay in the median age at death from the 1970s (66.15 years) to 2013 (70.39 years), especially in the high-risk areas. In Cixian, the total trend of the cohort effect declined, and people aged 65-69 years were a population at relatively high risk for UGIC. We predicted that the crude mortality rates of UGIC in Cixian and Shexian would decrease to 98.80 and 133.99 per 100000 in 2018, respectively.
UGIC was the major cause of cancer death in Hebei Province, and males in rural areas were a high-risk population. We should strengthen early detection and treatment of UGIC in this population.
Core tip: This study is the first to examine the incidence and mortality trends of UGIC in Hebei Province. Data were collected from 21 population-based cancer registries covering 15.25% of the total population of Hebei Province in 2013. An age-period-cohort model was established to analyse the incidence rate of UGIC in a high-risk area of Hebei Province (Cixian). Additionally, we established the grey system model to predict the mortality rates of UGIC in high-risk areas of Hebei Province (Cixian and Shexian). The aim of the study was to provide epidemiological evidence for developing strategies for UGIC prevention and control.
- Citation: Li DJ, Liang D, Song GH, Li YW, Wen DG, Jin J, He YT. Upper gastrointestinal cancer burden in Hebei Province, China: A population-based study. World J Gastroenterol 2017; 23(14): 2625-2634
- URL: https://www.wjgnet.com/1007-9327/full/v23/i14/2625.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i14.2625
According to GLOBOCAN 2012, upper gastrointestinal cancer (UGIC) is the third most common cancer worldwide and the second leading cause of death among all cancer types. Approximately 45% of all cases occur in China[1]. The incidence and mortality proportions of UGIC are approximately 19.8% and 23.3% of all malignancies in China, respectively[2]. Thus, monitoring and studying the incidence and mortality of UGIC can provide important information, enable effective assessment and potentially generate a strategy for UGIC prevention and control based on its distribution pattern.
Hebei Province is located in northern China along the Taihang Mountain chain and has a relatively less developed economy. This province was recognized as a high-risk area for UGIC in the 1970s. In 2015, Hebei Province had 21 population-based cancer registries that covered 11185626 registered individuals (approximately 15.25% of the total population of Hebei Province). Additionally, Hebei Province participated in three national death surveys that were conducted during the periods from 1973-1975[3], 1990-1992[4] and 2004-2005[5]. Cixian and Shexian in Hebei Province exhibit a high frequency of UGIC; their cancer registries were established in 1974 and 2000, respectively. Several investigations[6-8] have been conducted to assess the potential risk factors and the corresponding aetiological intervention methods and screening measures for UGIC.
This study combined the data for esophageal cancer and stomach cancer to investigate the real burden of UGIC in Hebei Province and to provide information on its prevention and treatment.
The Hebei Provincial Cancer Registry was established in 2009 and is responsible for cancer data collection, evaluation and publication. Data were collected from 21 local population-based registries in 2013, including 16 counties (Cixian, Shexian, Qianxi County, Wuan County, Zanhuang County, Fengning County, Xinji County, Xingtai County, Zhangbei County, Anguo County, Haixing County, Yanshan County, Neiqiu County, Renxian, Xuanhua County and Shenze County) and 5 cities (Baoding City, Qinhuangdao City, Cangzhou City, Shijiazhuang City and Shuangqiao District of Chengde City). These counties and cities represented urban areas and rural areas, respectively. The reported cases were from multiple sources, including local hospitals, community health centres, the Urban Resident Basic Medical Insurance Program and the New Rural Cooperative Medical Scheme. All data on cancer in Hebei Province were obtained from the Hebei Provincial Cancer Registry Database. Population information was collected from the local statistical bureau or household register department in the local public security bureau. We also extracted data on UGIC in Cixian from 1989 to 2013 and Shexian from 2004 to 2013. According to the International Classification of Diseases, 10th revision (ICD-10), C15 (esophageal cancer) and C16 (gastric cancer), which are UGIC, were extracted for the analysis.
The inclusion criteria for the data were based on the Guidelines of the Chinese Cancer Registration[9] and the International Agency for Research on Cancer/International Association of Cancer Registries (IARC/IACR). The analysed data had a morphological verification percentage (MV%) higher than 66%, a percentage of cancer cases identified with death certification only (DCO%) less than 15% and a mortality to incidence ratio (M/I) between 0.6 and 0.8. All of the data were checked and evaluated based on the data quality criteria.
In the mid-1970s, a nationwide retrospective survey of causes of mortality was conducted in 29 provinces, including all 153 cities and counties. This survey covered 47.725 million people in Hebei Province[3] and provided a profile of cancer mortality in Hebei Province.
The second national retrospective sampling survey of cancer mortality was conducted from 1990 to 1992. This survey used a stratified sampling method and covered approximately 10% of the population in China[4]. A total of 21 cities and counties, including 6.375 million people in Hebei Province, were enrolled in the sampling areas.
The third national retrospective stratified sampling survey of all causes of death was performed during the period from 2004-2005 in 31 provinces/municipalities/autonomous regions, which included Hebei Province. A total of 18 cities and counties were selected as sampling areas, covering 13.79 million people and 20.15% of the total population of Hebei Province[5].
The pooled data for UGIC from the three national retrospective sampling surveys were stratified by area (high-risk/non-high-risk areas) and gender. Cixian, Shexian and Zanhuang counties were selected as the high-risk areas; the rest counties were considered non-high-risk areas.
The data analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, United States), SAS version 9.4 (SAS Institute Inc., Cary, NC, United States) and Microsoft Excel 2003 (Microsoft, United States). The world age-standardized rate (ASR World) and Chinese age-standardized rate (ASR China) were calculated based on Segi’s population and the Chinese population in 2000, respectively. Long-term trends of UGIC in Cixian and Shexian were analysed using an age-period-cohort model and grey system (GM) (1, 1) model. We used an age-period-cohort model to estimate the relative risks by age, period, and birth cohort based on the Cixian data collected from 1989 to 2013. Additionally, we extracted thirteen 5-year age groups from 25-29 to 85+ years old and five 5-year periods ranging from 1989-1993 to 2009-2013 to produce birth cohorts from 1904-1908 to 1984-1988. The three components (i.e., cohort, period, and age) in the age-period-cohort model were linearly dependent. Thus, we adopted the common method of including an additional arbitrary reference constraint for the period effect[10,11]. Additionally, the periods from 2004-2008 and 2009-2013 and the birth cohort from 1934-1938 were chosen as reference groups for the 85+ age group.
Based on the crude mortality rates of UGIC in Cixian and Shexian from 2004-2013, an Excel table was used to establish the GM (1, 1)[12]. The posterior error ratio (C) and small error probability (P) were used to determine the prediction accuracy, the relative error between the predicted value and the actual value, and the extrapolated prediction of mortality of UGIC in Cixian and Shexian from 2014-2018.
In 2013, there were 6205 new UGIC cases (4328 in males and 1877 in females), accounting for 24.62% of all types of cancer in the Hebei Provincial Cancer Registry areas. The crude incidence rate of the total areas was 55.47 per 100000 people. The ASR World and the ASR China in 2000 were 44.90 and 44.16/100000 people, respectively (Table 1). The incidence rate of UGIC was higher in males than in females. The incidence rate was 2.62 times higher in rural areas (75.17/100000) than in urban areas (28.69/100000). Almost 78% of the new cases were from rural cancer registries, and more than 50% of the cases were males from rural areas. The male incidence rate was highest in rural areas (101.35/100000). The median age at diagnosis of UGIC was 65.06 years (64.73 years in males and 66.03 years in females) in Hebei Province. The median age was 4.36 years younger in rural areas (64.37 years) than in urban areas (68.74 years).
| Area | Gender | Upper gastrointestinal cancer | Esophageal cancer | Stomach cancer | |||||||||
| No. | Crude rate (1/105) | ASR China (1/105) | ASR World (1/105) | No. | Crude rate (1/105) | ASR China (1/105) | ASR World (1/105) | No. | Crude rate (1/105) | ASR China (1/105) | ASR World (1/105) | ||
| Total | Both genders | 6205 | 55.47 | 44.16 | 44.90 | 2349 | 21.00 | 16.63 | 16.91 | 3856 | 34.47 | 27.54 | 27.99 |
| Male | 4328 | 75.8 | 62.43 | 63.50 | 1517 | 26.57 | 21.83 | 22.16 | 2811 | 49.23 | 40.60 | 41.34 | |
| Female | 1877 | 34.28 | 26.43 | 26.75 | 832 | 15.19 | 11.59 | 11.81 | 1045 | 19.08 | 14.84 | 14.94 | |
| Urban | Both genders | 1360 | 28.69 | 21.73 | 21.65 | 449 | 9.47 | 7.12 | 7.16 | 911 | 19.22 | 14.61 | 14.49 |
| Male | 969 | 40.46 | 32.51 | 32.5 | 315 | 13.15 | 10.51 | 10.48 | 654 | 27.31 | 22.00 | 22.02 | |
| Female | 391 | 16.67 | 12.03 | 11.74 | 134 | 5.71 | 4.00 | 4.05 | 257 | 10.96 | 8.03 | 7.69 | |
| Rural | Both genders | 4845 | 75.17 | 62.3 | 63.75 | 1900 | 29.48 | 24.45 | 24.97 | 2945 | 45.69 | 37.85 | 38.79 |
| Male | 3359 | 101.35 | 85.84 | 87.89 | 1202 | 36.27 | 30.92 | 31.67 | 2157 | 65.08 | 54.91 | 56.22 | |
| Female | 1486 | 47.46 | 38.79 | 39.69 | 698 | 22.29 | 18.05 | 18.37 | 788 | 25.17 | 20.73 | 21.31 | |
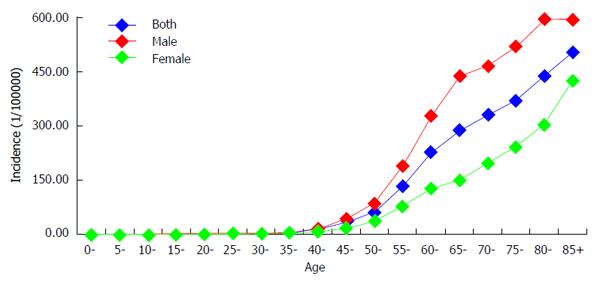
The age-specific incidence rate was relatively low for individuals younger than 40 years of age and then increased dramatically. The incidence rate reached the peak in the 85+ age group (504.44/100000), although the incidence rate reached the peak in the 80-84 age group (598.17/100000) for males. The trend in the urban and rural areas was similar to the overall trend (Figure 1).
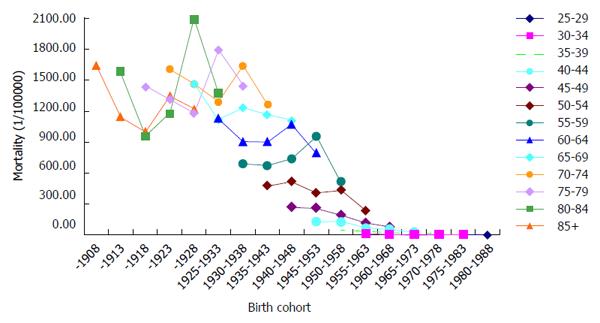
Generally, the trend of the incidence rates of UGIC decreased with the year of birth. The incidence rate increased after a decrease and then decreased again for individuals age older than 55 years but remained steady for the 25-to-54-year-old age groups (Figure 2).
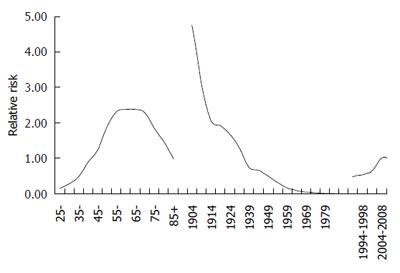
Age, period and cohort effects contributed to the observed changes in the UGIC incidence. The model including all three components had the best goodness of fit, i.e., the model had the lowest Akaike’s information criterion value (691.267).
The incidence rate increased with age but decreased with the cohort. Figure 3 details the age effect and shows an increasing trend for individuals aged 25-65 years. The 65-69 age group had the highest relative risk (RR = 2.38) compared with the reference group (85+ age group). The birth cohort effect showed a consistent decline in the incidence rate in all cohorts after those born in the early 1900s. The RR of the period effects was lower from 1989-1993 compared to the reference group (Figure 3).
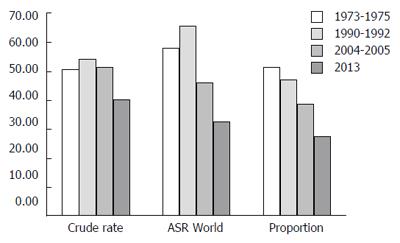
A decreasing trend in the mortality rates of UGIC was observed in the period from 1973-1975 (50.53/100000) to 2013 (40.21/100000). The mortality rates increased slightly from the 1970s to 1990s and then dropped sharply. In Hebei Province, the data from the four periods of the death survey indicated that the mortality rate in 2013 had decreased by 20.42%, 25.15% and 21.53% compared with the three periods from the national sampling surveys of causes of death (1973-1975, 1990-1992, and 2004-2005, respectively). Age standardization decreased the rates by 43.81%, 50.27% and 29.08%, respectively. For males, the ASR World in 1973-1975 (80.04/100000) was 1.79 times higher than that in 2013 (44.77/100000). In females, the rate decreased from 36.30/100000 in 1973-1975 to 21.03/100000 in 2013 (Table 2, Figure 4). The proportions of UGIC among all types of cancers were 51.29%, 47.00%, 38.55% and 27.64% during the periods from 1973-1975, 1990-1992, 2004-2005, and 2013, respectively, and showed a stepwise decrease, especially for males. The mortality rates of UGIC dropped in both the high-risk and non-high-risk areas from the 1970s to 2013. The mortality rates in 2013 decreased by 57.26%, 54.17% and 29.44% in the high-risk areas compared with the three periods from the sampling surveys of national causes of death (1973-1975, 1990-1992, and 2004-2005) and by 55.02%, 39.67% and 21.65% in the non-high-risk areas, respectively. The mortality rates in the high-risk areas were 3.76 times higher than those in the non-high-risk areas in 2013. Additionally, the ASR World ratio between the high-risk areas and non-high-risk areas was lower than those from the three death survey periods (3.95, 4.94 and 4.17, respectively) (Table 3).
| 1973-1975 | 1990-1992 | 2004-2005 | 2013 | |||||||||
| Both | Male | Female | Both | Male | Female | Both | Male | Female | Both | Male | Female | |
| Deaths | 72347 | 49516 | 22831 | 10429 | 7049 | 3380 | 7103 | 4927 | 2176 | 4498 | 3000 | 1498 |
| Crude rate (1/105) | 50.53 | 67.68 | 32.61 | 53.72 | 70.82 | 35.72 | 51.24 | 69.16 | 32.29 | 40.21 | 52.54 | 27.35 |
| ASR China (1/105) | 57.61 | 79.19 | 36.29 | 65.24 | 90.35 | 41.46 | 45.84 | 64.49 | 27.71 | 32.76 | 44.86 | 21.28 |
| ASR World (1/105) | 58.07 | 80.04 | 36.30 | 65.62 | 91.02 | 41.45 | 46.01 | 64.75 | 27.70 | 32.63 | 44.77 | 21.03 |
| Ratio (%) | 51.29 | 58.14 | 40.86 | 47.00 | 49.75 | 42.13 | 38.55 | 41.94 | 32.59 | 27.64 | 29.55 | 24.49 |
| Median age (yr) | 66.15 | 65.78 | 67.04 | 66.22 | 65.81 | 67.11 | 68.09 | 67.64 | 69.23 | 70.39 | 69.21 | 72.95 |
| 1973-1975 | 1990-1992 | 2004-2005 | 2013 | |||||||||||||
| Deaths | Crude rate (1/105) | ASR World (1/105) | Median age (yr) | Deaths | Crude rate (1/105) | ASR World (1/105) | Median age (yr) | Deaths | Crude rate (1/105) | ASR World (1/105) | Median age (yr) | Deaths | Crude rate (1/105) | ASR World (1/105) | Median age (yr) | |
| High-risk areas | ||||||||||||||||
| Male | 2975 | 214.94 | 286.44 | 62.99 | 3182 | 189.69 | 300.62 | 62.91 | 2005 | 158.63 | 188.08 | 65.46 | 969 | 143.19 | 131.41 | 69.22 |
| Female | 1536 | 118.93 | 150.76 | 64.70 | 1645 | 98.63 | 133.82 | 64.55 | 910 | 76.25 | 80.50 | 67.21 | 489 | 75.68 | 59.43 | 73.04 |
| Both genders | 4511 | 168.60 | 218.69 | 63.54 | 4827 | 140.79 | 203.94 | 63.48 | 2915 | 118.62 | 132.47 | 66.01 | 1458 | 110.22 | 93.46 | 70.37 |
| Non-high-risk areas | ||||||||||||||||
| Male | 46541 | 64.85 | 76.49 | 65.95 | 3867 | 46.73 | 58.14 | 66.10 | 2922 | 49.87 | 45.00 | 67.12 | 2031 | 40.36 | 34.22 | 69.21 |
| Female | 21295 | 30.99 | 34.39 | 67.22 | 1735 | 22.26 | 24.85 | 66.36 | 1266 | 22.83 | 18.91 | 68.11 | 1009 | 20.89 | 15.91 | 72.91 |
| Both genders | 67836 | 48.28 | 55.34 | 66.32 | 5602 | 35.04 | 41.26 | 66.18 | 4188 | 36.72 | 31.77 | 67.41 | 3040 | 30.82 | 24.89 | 70.40 |
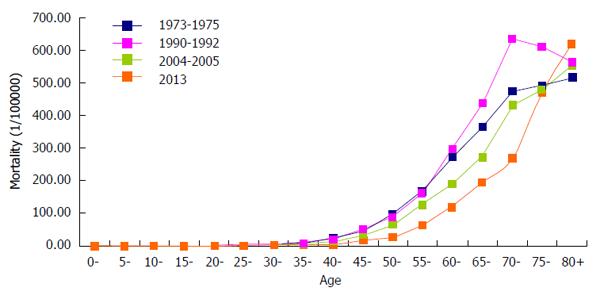
According to the graph depicting the age-specific rates in different periods, the periods from 1973-1975, 2004-2005 and 2013 had similar trends. Beginning with the 45-49 age group, the mortality rate of UGIC increased. The mortality rate reached the peak in the 80-84 age group. In contrast, the mortality rate of the 70-74 age group was highest from 1990-1992. The age-specific mortality rates were lower in 2013 than in 1973-1975, 1990-1992 and 2004-2005 for those younger than 75 years of age but dramatically increased thereafter, with reports of mortality rates higher than the rates in the three sampling surveys of national causes of death (Figure 5).
The median age at death caused by UGIC gradually increased. The median was 66.15 years in 1973-1975 and 66.22 years in 1990-1992.The median age at death increased from 68.09 years in 2004-2005 to 70.39 years in 2013. The median age at death for females increased to 72.95 years in 2013.
There was a notable delay in the median age at death caused by UGIC from the 1970s to 2013 in the high-risk areas. The median age of death was delayed by 6.84 years in the high-risk areas compared to only 4.08 years in the non-high-risk regions. The median age at death for females was delayed by 8.34 and 5.69 years in the high-risk areas and non-high-risk areas, respectively. In 2013, the median age at death in the high-risk areas (70.37) was similar to that in the non-high-risk areas (70.40).
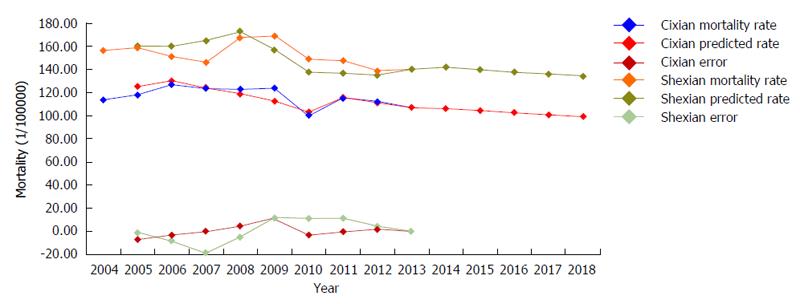
The mortality rate of UGIC in Cixian was 113.41 per 100000 in 2004. The mortality rate decreased to 106.87 per 100000 in 2013. The GM (1, 1) equation was Yt = -6992.90e-0.01802(t-1) + 7106.31, which predicted that the mortality rate of UGIC in Cixian would decrease to 98.80 per 100000 in 2018, with a maximum relative error of 9.10%. The C was 0.58, and the P was 0.78, which indicated that the model was qualified (Table 4, Figure 6).
| Year | t | Cixian | Shexian | ||||
| Mortality rate | Predicted rate | Error | Mortality rate | Predicted rate | Error | ||
| 2004 | 1 | 113.41 | 156.08 | ||||
| 2005 | 2 | 117.74 | 124.88 | -7.13 | 158.66 | 160.24 | -1.57 |
| 2006 | 3 | 126.51 | 129.78 | -3.27 | 150.89 | 159.62 | -8.73 |
| 2007 | 4 | 123.38 | 123.73 | -0.35 | 145.89 | 164.62 | -18.73 |
| 2008 | 5 | 122.51 | 118.66 | 3.85 | 167.40 | 172.49 | -5.09 |
| 2009 | 6 | 123.59 | 112.34 | 11.25 | 168.63 | 156.75 | 11.88 |
| 2010 | 7 | 99.45 | 102.87 | -3.42 | 148.73 | 137.70 | 11.02 |
| 2011 | 8 | 114.65 | 115.50 | -0.85 | 147.39 | 136.52 | 10.88 |
| 2012 | 9 | 112.17 | 110.93 | 1.24 | 138.28 | 134.65 | 3.63 |
| 2013 | 10 | 106.87 | 106.87 | 0.00 | 139.88 | 139.90 | -0.02 |
| 2014 | 11 | 106.18 | 141.57 | ||||
| 2015 | 12 | 104.29 | 139.64 | ||||
| 2016 | 13 | 102.42 | 137.73 | ||||
| 2017 | 14 | 100.59 | 135.85 | ||||
| 2018 | 15 | 98.80 | 133.99 | ||||
The mortality rate of UGIC in Shexian was decreased by 10.38% from 2004 to 2013. The GM (1, 1) equation was Yt = -11725.81e-0.01376(t-1) + 11881.89, which predicted that the mortality rate of UGIC in Shexian would decrease to 133.99 per 100000 in 2018, with a maximum relative error of 12.84%. The C and P were 0.94 and 0.44, respectively, indicating that the model was up to standard (Table 4, Figure 6).
This study is the first to examine the incidence and mortality trends of UGIC in Hebei Province, China. The study collected data from 21 population-based cancer registries covering 15.25% of the total population of Hebei Province in 2013, which had not achieved maximal coverage in this province to date. The aim was to provide epidemiological evidence for developing strategies to control UGIC. The crude incidence rate of UGIC was 55.47/100000 in Hebei Province, which was approximately 1.06 times higher than the rate in the Chinese population (52.45/100000) and far higher than the global rate (19.95/100000)[1,2]. In Hebei Province, newly diagnosed UGIC cases comprised 24.62% of all cancer types, whereas the cases accounted for only 10.0% of all cancer types worldwide. The mortality rate of UGIC in males in the rural areas of Hebei Province was approximately 5.08 times higher than the global statistics. Males in rural areas of Hebei Province were a population at high risk of developing UGIC.
Our data showed that the burden of UGIC was heavy in Hebei Province. UGIC resulted from lifestyle habits, such as an unreasonable dietary structure, tobacco smoking, alcohol drinking, smoked food consumption and poor oral health[13-17]. A significant inverse association has been reported between fruit consumption and UGIC (esophageal cancer, RR = 0.60; gastric cancer, odds ratio (OR) = 0.43)[18,19]. An intake of cereal fibre was significantly inversely associated with the risk of cancers of the gastrointestinal tract[18]. One recent study showed that insufficient consumption of fresh fruits may be a serious risk factor in Hebei Province, and the dietary fibre intake was only 37.3% of the reference intake from 2010-2013[20]. Heavy smoking and chronic alcohol consumption were reported to be major risk factors for UGIC[21]. People who were current cigarette smokers were associated with an increased risk of esophageal cancer (RR = 1.67) and gastric cancer (RR=1.60) compared with people who had never smoked[22]. In China, the smoking rate was 52.9% for males, and the second-hand smoking rate was approximately 72.4%, which was significantly higher than the global level[23]. In Hebei Province, the cigarette smoking rate was 26.08% for both genders and 48.09% for males[24]. Additionally, the smoking prevalence is still increasing. According to an investigation on alcohol consumption in adult residents in Hebei Province[25], the total drinking rate was 41.1% and was higher in males (71.8%) than in females (19.7%). Males were the primary population that drank alcohol. Because maintaining good life habits is necessary for health, we suggest that people, especially males in rural areas, quit smoking and limit alcohol consumption.
Economic, environmental and genetic risk factors can also lead to the high incidence and mortality rates of UGIC[26-28]. UGIC is a disease of the poor and the socially disadvantaged. A large number of epidemiological studies have confirmed that the UGIC risk is higher in populations with a lower socioeconomic status due to limited medical care, limited education and poor living conditions[29-33]. Almost 78% of the new cases occurred in rural areas of Hebei Province in 2013. The per capita annual net income of urban households (¥17278) was approximately 2.64 times higher than that of rural households (¥6539) in Hebei Province in the 2010s[34]. The low income sets constraints on the involvement of the population in health care for the prevention or treatment of illnesses and injuries, the possibility of a good education level, which would improve their health awareness and lifestyle, the ability to live in a favourable environment where they could avoid exposure to bacteria, viruses and other infection-causing agents, and their dietary choices. One study identified risk factors for esophageal cancer in residents of Hebei Province and showed that living in rural areas (OR = 3.14) and eating mildewed food (OR = 7.44) were risk factors for esophageal cancer[35].
A family history of cancer is an important risk factor for UGIC. A first-degree family history of esophageal or gastric cancer was significantly associated with UGIC development, with an adjusted OR of 4.7 (95%CI: 2.6-8.4)[36]. A study on residents of Hebei Province found that having a family history of esophageal cancer was a risk factor for this malignancy, with an OR of 3.23[35]. In Cixian, a family history of gastric cancer was shown to be a risk factor for this malignancy (OR = 1.84)[7]. Therefore, appropriate screening strategies, especially for relatives of patients, should be considered for the prevention and control of UGIC in Hebei Province.
Moreover, UGIC was associated with geographic factors. Liang et al[8] showed that the nitrate, nitrite, nitrogen and ammonia levels in high-risk areas of Hebei Province were seven times higher than those in low-risk regions and exceeded the national standards for drinking water. Cao et al[6] also found that the nitrate level in Shexian (a high-risk area), Hebei Province was five times higher than that in Chicheng County (a low-risk area) and that the nitrogen and ammonia levels in Shexian were also higher. This finding suggests that nitrate and ammonia were important risk factors for UGIC. Therefore, we should improve drinking water quality and provide safe water to the high-risk areas of Hebei Province.
The mortality rate of UGIC in Hebei Province dropped from the 1970s to 2013. In Hebei Province, the data from the four periods of the death survey indicated that the mortality rate in 2013 had decreased by 20.42% compared with the mortality rate in 1973-1975 in the sampling survey of national causes of death. In both high-risk and non-high-risk areas, the mortality rates of UGIC dropped from the 1970s to 2013, although the rates declined more in the high-risk areas than in the non-high-risk areas.
The age-specific mortality rate was lower in 2013 than in 1973-1975, 1990-1992 and 2004-2005 for individuals younger than 75 years but was dramatically increased in the 75-79 age group. This latter group had an age-specific mortality rate in 2013 that was higher than the rates in 1973-1975, 1990-1992 and 2004-2005, showing the ageing population trend. At present, as economic growth drives the standards of living higher, the median age at death caused by UGIC increases. The median age at death caused by UGIC increased approximately 4 years from the 1970s to 2013. This rate is increasing faster in high-risk areas than in non-high-risk areas; indeed, the median age at death in high-risk areas (70.37) was basically the same as that in non-high-risk areas (70.40) in 2013. This finding indicated that we had achieved a great success in the screening, early detection and treatment of UGIC in Hebei Province, especially in high-risk areas. Additionally, diagnosis and treatment have improved, which can extend people’s lifespan. However, we need to continue efforts to reduce the mortality rate.
The prognosis of UGIC is poor. The main reason is that most cases are asymptomatic during early stages and thus are detected at an advanced stage when they are no longer amenable to surgical resection. Therefore, screening and treating patients with upper gastrointestinal precancerous lesions is important for preventing the development of UGIC in high-risk individuals. Cixian and Shexian have been chosen as demonstration bases for the early detection and treatment of UGIC. Endoscopy with mucosal iodine staining is a sensitive technique to identify clinically relevant UGIC. Since 2000, a national screening programme using endoscopy with mucosal iodine staining and an index biopsy combined with a pathological examination to confirm and stage the disease has become available at 17 sites in Hebei Province, including Cixian and Shexian. At present, 25000 high-risk individuals in Hebei Province are screened every year. The screening programme has reduced the total cancer mortality rates in the Cixian and Shexian populations and may be one reason for the decreasing trend of mortality.
We showed the age, period and birth cohort effects of the condition in Cixian from 1989 to 2013 via an age-period-cohort model. The age and cohort effects played an important role. People aged between 65 and 69 years were a population at relatively high risk for UGIC. The total trend of the cohort effect was a decline, and the early birth cohort had higher risk of developing UGIC. One reason could be that long-term unhealthy lifestyle behaviours, such as heavy smoking, chronic alcohol consumption, and a weakened immune system, increased the birth cohort effect of the incidence risk in rural areas during these time periods. The period effect did not show large variation. Using the grey system model, we found that the mortality rates of UGIC in Cixian and Shexian exhibited a downward trend that should be attributed to the early diagnosis and treatment in these high-risk areas of Hebei Province. The model predicted that the mortality rates of UGIC would decrease to 98.80 and 133.99 per 100000 in 2018, respectively. However, we should still enhance UGIC control and prevention measures.
In summary, the mortality rate of UGIC has been decreasing over the past 40 years. However, UGIC was the major cause of cancer death in Hebei Province. Intensifying the primary prevention by adopting a healthy lifestyle and the secondary prevention with endoscopic iodine staining are priorities for the reduction of the morbidity and mortality of UGIC in Hebei Province.
Globally, approximately 45% of upper gastrointestinal cancer cases (including esophageal cancer and stomach cancer) occur in China. The incidence and mortality proportions of these cancers account for approximately 19.8% and 23.3% of all malignancies in China, respectively. Hebei Province is recognized as a high-risk area for upper gastrointestinal cancer.
In China, the burden of upper gastrointestinal cancer is heavy. However, few studies have investigated the epidemiological trends of upper gastrointestinal cancer. This research focused on the analysis of the real burden of upper gastrointestinal cancer in Hebei Province and the trend in the high-risk regions of Hebei Province and China to provide epidemiological evidence for developing strategies to control upper gastrointestinal cancer.
The study collected data from 21 population-based cancer registries covering 11185626 individuals in Hebei Province in 2013. The authors applied the age-period-cohort model to analyse the incidence rate of upper gastrointestinal cancer in one high-risk area of Hebei Province (Cixian), and predicted the mortality rates of upper gastrointestinal cancer in the high-risk areas of Hebei Province (Cixian and Shexian) using a grey system model.
This study investigated the real burden of upper gastrointestinal cancer in Hebei Province. This study analysed the reasons why the incidence and mortality rates of upper gastrointestinal cancer were higher in the high-risk areas than in the non-high-risk areas and why the mortality rates decreased. The results will provide reference values for upper gastrointestinal cancer control.
The aim of this study was to provide epidemiological evidence for developing strategies to control upper gastrointestinal cancer (UGIC), which is defined as the principle cause of death in a large area of China(i.e., Hebei Province, which has a risk that is 5.08 times higher than the estimated global risk). All of the epidemiological data are of enormous importance since they represent the basis for a smart health policy that should be oriented and balanced on actual risk data for different regions and populations. The manuscript is well written and organized.
| 1. | GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Available from: http:www.//globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.2012. |
| 2. | Chen W, Zheng R, Zhang S, Zeng H, Zuo T, Jia M, Xia C, Zou X, He J. Report of Cancer Incidence and Mortality in China, 2012. China Cancer. 2016;25:8. |
| 3. | Office for Cancer Preventionand Control, Ministry of Health, P.R.China. 1st ed. 1980;. |
| 4. | National Office for Cancer Prevention and Control. Survey of cancer mortality in China 1990-1992. 1993;. |
| 5. | Office for Cancer Prevention Control, Ministry of Health, P. R. China. Malignant tumor mortality survey report (2004-2005), 1st edition. Beijing: People’s Medical Publishing House 2007; . |
| 6. | Cao Y, Liang S, Akazawa K, Zhang F, Huang S, Wang S. Correlation between esophageal cancer and nitrogen compounds in drinking water. Linchuang Huicui. 2011;26:2036-2038. |
| 7. | Hou J, Zhang G, He Y, Chen Z, Qiao C, Liu J, Meng F, Song G, Li S, Hao S. A case-control study on risk factor of gastric carcinoma in Cixian of Hebei Province. Zhongliu Fangzhi Yangjiu. 2000;27:415-417. |
| 8. | Liang S, CY . Research of the “three nitrogen” content in drinking water in rural of high incidence of esophageal, Cixian. Zhonghua Zhongliu Yufang Zazhi. 2012;19:649-651. |
| 9. | National Cancer CenterDisease Prevention and Control Bureau, Ministry of Health. Chinese Cancer Registry Annual Report 2012. Beijing: China Ministry of Health 2012; . |
| 10. | Wong IO, Cowling BJ, Law SC, Mang OW, Schooling CM, Leung GM. Understanding sociohistorical imprint on cancer risk by age-period-cohort decomposition in Hong Kong. J Epidemiol Community Health. 2010;64:596-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Piontek D, Kraus L, Pabst A, Legleye S. An age-period-cohort analysis of cannabis use prevalence and frequency in Germany, 1990-2009. J Epidemiol Community Health. 2012;66:908-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Zhang Y. Medical statistical forecast. Beijing: China Science and Technology Publishing House 1995; . |
| 13. | Chen ZM, Peto R, Iona A, Guo Y, Chen YP, Bian Z, Yang L, Zhang WY, Lu F, Chen JS. Emerging tobacco-related cancer risks in China: A nationwide, prospective study of 0.5 million adults. Cancer. 2015;121 Suppl 17:3097-3106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19:5598-5606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 736] [Cited by in RCA: 762] [Article Influence: 58.6] [Reference Citation Analysis (19)] |
| 15. | Mao WM, Zheng WH, Ling ZQ. Epidemiologic risk factors for esophageal cancer development. Asian Pac J Cancer Prev. 2011;12:2461-2466. [PubMed] |
| 16. | Murata A, Fujino Y, Pham TM, Kubo T, Mizoue T, Tokui N, Matsuda S, Yoshimura T. Prospective cohort study evaluating the relationship between salted food intake and gastrointestinal tract cancer mortality in Japan. Asia Pac J Clin Nutr. 2010;19:564-571. [PubMed] |
| 17. | Wang Q, Chen Y, Wang X, Gong G, Li G, Li C. Consumption of fruit, but not vegetables, may reduce risk of gastric cancer: results from a meta-analysis of cohort studies. Eur J Cancer. 2014;50:1498-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Bradbury KE, Appleby PN, Key TJ. Fruit, vegetable, and fiber intake in relation to cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Am J Clin Nutr. 2014;100 Suppl 1:394S-398S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 215] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 19. | Denova-Gutiérrez E, Hernández-Ramírez RU, López-Carrillo L. Dietary patterns and gastric cancer risk in Mexico. Nutr Cancer. 2014;66:369-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Tian M, Chen L, Song L, Liu C, Shi Y, Miao R, Zhu X. Analysis of dietary pattern of residents at 7 monitoring sites in Hebei Province. Xiandai Yufang Yixue. 2015;42:3679-3681. |
| 21. | Pöschl G, Seitz HK. Alcohol and cancer. Alcohol Alcohol. 2004;39:155-165. [PubMed] |
| 22. | Steevens J, Schouten LJ, Goldbohm RA, van den Brandt PA. Alcohol consumption, cigarette smoking and risk of subtypes of oesophageal and gastric cancer: a prospective cohort study. Gut. 2010;59:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 23. | China Health and Family Planning Commission of China. 2015 report on Chinese nutrition and chronic disease. Available from: http://www.nhfpc.gov.cn/jkj/s5879/201506/4505528e65f3460fb88685081ff158a2.shtml. |
| 24. | Lu A, Wang X, Gao G, Ma Y, Sun J, Xue Y. Comparative study on cigarette smoking between urban and rural residents in Hebei province. Zhongguo Gonggong Weisheng. 2005;21:908-909. |
| 25. | Wang L, Li H, Zhang J, Sun J. The investigation of alcohol consumption status in adult residents living in Hebei Province. Xiandai Yufang Yixue. 2007;34:279-283. |
| 26. | Bhat GA, Shah IA, Rafiq R, Nabi S, Iqbal B, Lone MM, Islami F, Boffetta P, Dar NA. Family history of cancer and the risk of squamous cell carcinoma of oesophagus: a case-control study in Kashmir, India. Br J Cancer. 2015;113:524-532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Shin CM, Kim N, Yang HJ, Cho SI, Lee HS, Kim JS, Jung HC, Song IS. Stomach cancer risk in gastric cancer relatives: interaction between Helicobacter pylori infection and family history of gastric cancer for the risk of stomach cancer. J Clin Gastroenterol. 2010;44:e34-e39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 28. | Bryere J, Dejardin O, Bouvier V, Colonna M, Guizard AV, Troussard X, Pornet C, Galateau-Salle F, Bara S, Launay L. Socioeconomic environment and cancer incidence: a French population-based study in Normandy. BMC Cancer. 2014;14:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Kamangar F, Chow WH, Abnet CC, Dawsey SM. Environmental causes of esophageal cancer. Gastroenterol Clin North Am. 2009;38:27-57, vii. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 282] [Cited by in RCA: 297] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 30. | Khatami F, Karbakhsh M. Socioeconomic position and incidence of gastric cancer: a systematic review and meta-analysis. J Epidemiol Community Health. 2015;69:818-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Lagergren J, Andersson G, Talbäck M, Drefahl S, Bihagen E, Härkönen J, Feychting M, Ljung R. Marital status, education, and income in relation to the risk of esophageal and gastric cancer by histological type and site. Cancer. 2016;122:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 32. | Mendoza D, Herrera P, Gilman RH, Lanfranco J, Tapia M, Bussalleu A, Tenorio JH, Guillén-Rodríguez CE, Arróspide MT, Piscoya A. Variation in the prevalence of gastric cancer in Perú. Int J Cancer. 2008;123:414-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Uthman OA, Jadidi E, Moradi T. Socioeconomic position and incidence of gastric cancer: a systematic review and meta-analysis. J Epidemiol Community Health. 2013;67:854-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 34. | Statistics HPBo. 2010. Available from: http://www.hetj.gov.cn/hetj/tjsj/. |
| 35. | Shi J, Peng Y, Ding S, Wang L, Wang R, Gao Y. Influential factors of esophageal cancer in residents of Hebei Province: a case-control study. Zhongguo Gonggong Weisheng. 2012;28:454-457. |
| 36. | Safaee A, MoghimiDehkordi B, Fatemi SR, Maserat E, Ghafarnejad F, Zali MR. Family History as a Risk for Upper Gastrointestinal Tract Cancer: A Case Control Study. Iran J Cancer Prev. 2011;4:114-118. [PubMed] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Aseni P S- Editor: Yu J L- Editor: Wang TQ E- Editor: Wang CH