Published online Nov 21, 2016. doi: 10.3748/wjg.v22.i43.9654
Peer-review started: September 8, 2016
First decision: September 28, 2016
Revised: October 10, 2016
Accepted: October 19, 2016
Article in press: October 19, 2016
Published online: November 21, 2016
Processing time: 72 Days and 13.9 Hours
Myelolipoma is a rare tumor composed of fat and bone marrow components, most of which are located in the adrenal gland. Myelolipoma in the liver is extremely rare. To date, only 10 cases have been reported in the English-language medical literature. In one of these cases, the hepatic myelolipoma was found within a hepatocellular carcinoma (HCC). In the present study, we report the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient, a 26-year-old female who was admitted to our hospital because of a 4-d history of upper abdominal pain. The unenhanced computed tomography (CT) images showed a well-defined low-density mass with adipose components in the right liver lobe, 4.2 cm × 4.1 cm in size. Two inhomogeneous low-density masses were found in the left liver lobe, 8.6 cm × 7.7 cm and 2.6 cm × 2.6 cm in size. The masses in both the right and left liver lobes were heterogeneously enhanced in the contrast-enhanced CT images. Based on the results of the imaging examination, the mass in the right liver lobe was preliminarily considered to be a hamartoma, and the two masses in the left liver were preliminarily considered to be HCCs. We performed a right hepatectomy, a left hepatic lobectomy, and a cholecystectomy. Microscopic and immunohistochemical results revealed that the tumor in the right liver lobe was a hepatic myelolipoma, and that the two tumors in the left liver lobe were HCCs.
Core tip: Hepatic myelolipoma is extremely rare. To date, only 10 cases have been reported in the English-language medical literature. In the present study, we report the first case of the synchronous occurrence of a hepatic myelolipoma and two hepatocellular carcinomas in different liver sections of one patient, who received a right hepatectomy, a left hepatic lobectomy, and a cholecystectomy. We also highlight the diagnosis and treatment of a hepatic myelolipoma and conduct a literature review to deepen the understanding of the subject.
- Citation: Xu SY, Xie HY, Zhou L, Zheng SS, Wang WL. Synchronous occurrence of a hepatic myelolipoma and two hepatocellular carcinomas. World J Gastroenterol 2016; 22(43): 9654-9660
- URL: https://www.wjgnet.com/1007-9327/full/v22/i43/9654.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i43.9654
Myelolipoma is a rare benign tumor composed of fat and bone marrow components. The adrenal gland is the most common location[1,2]. Myelolipoma in the liver is extremely rare. To our knowledge, 10 cases have been reported in the English-language medical literature as individual case reports[3-12]. In one of the cases, the hepatic myelolipoma was found within a hepatocellular carcinoma (HCC)[6]. Hepatic myelolipomas are usually incidentally discovered by ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), or autopsy examination. The first case of hepatic myelolipoma was reported in France by Grosdidier et al[13] in 1973, and it was found on a plain abdominal X-ray during a regular checkup for diabetes and obesity. Although hepatic imaging modalities will lead to detection of the tumor, the diagnosis of a hepatic myelolipoma has to be confirmed by a histopathologic examination of the resected specimen. In the present study, we present the eleventh case of hepatic myelolipoma to be reported in the English-language medical literature. This is also the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient. The clinical, imaging, and pathologic features of this case are described, and the subject of hepatic myelolipoma is briefly reviewed to deepen our understanding of it.
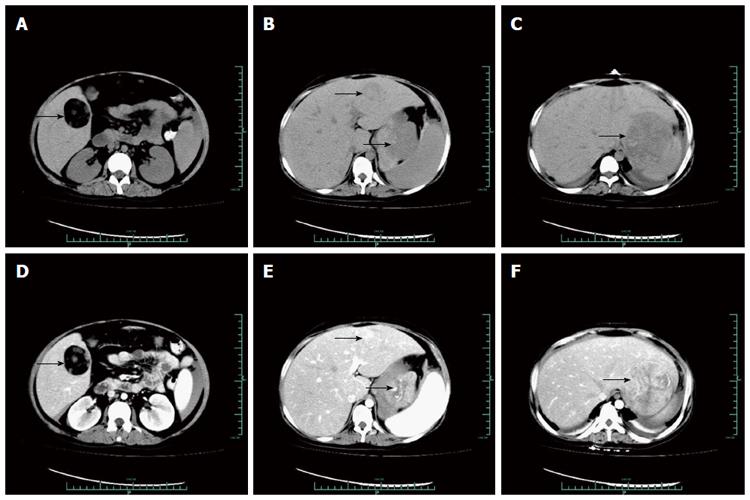
On November 28, 2014, a 26-year-old female was admitted to our hospital because of a 4-d history of upper abdominal pain. Her abdomen was soft, lax, and non-distended, with no palpable mass. The patient had no history of hepatitis B virus infection, hepatitis C virus infection or non-alcoholic fatty liver disease (NAFLD). Her family history was not significant. Abnormal laboratory results including alpha fetoprotein (AFP), 7529.2 ng/mL (normal, 20); carbohydrate antigen 125, 99.4 U/mL (normal, 0-35); serum creatinine, 42 μmol/L (normal, 45-84); serum sodium, 131 mmol/L (normal, 136-145); glutamyl transpeptidase, 103 U/L (normal, 7-32); fibrinogen, 4.45 g/L (normal, 2.00-4.00); and D-2-dimer, 9611 μg/L (normal, 0-700). The unenhanced CT images showed a well-defined low-density mass with adipose components in the right liver lobe, 4.2 cm × 4.1 cm in size (Figure 1A). Two inhomogeneous low-density masses were found in the left liver lobe, 8.6 cm × 7.7 cm and 2.6 cm × 2.6 cm in size (Figure 1B and C). In the contrast-enhanced CT images, the masses in both the right and the left liver lobe were heterogeneously enhanced (Figure 1D-F). Based on the results of the imaging examination, the mass in the right liver lobe was preliminarily considered to be a hamartoma, and the two masses in the left liver lobe were preliminarily considered to be HCCs.
After sufficient pre-operative preparation, a laparotomy was performed. One mass was found in the V section of the right liver lobe, and two masses were found in the left liver lobe, reflecting what was seen in the CT scan. We completed a right hepatectomy and a left hepatic lobectomy. Because the gallbladder was close to the tumor, a cholecystectomy was also performed. The intraoperative frozen pathology revealed that the tumor in the right liver lobe was a hepatic myelolipoma, and that the two tumors in the left liver lobe were HCCs.
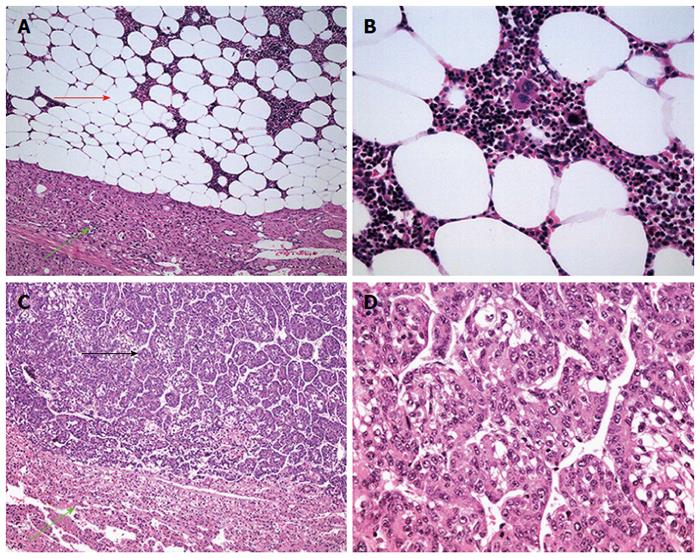
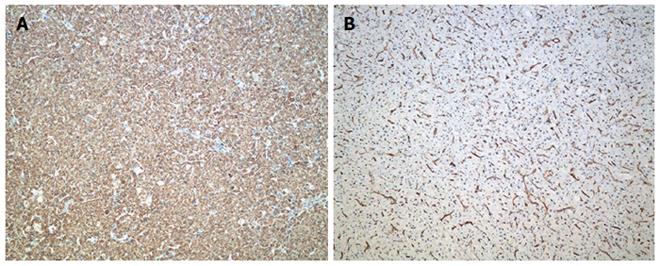
Macroscopically, the mass in the right liver lobe had a solid capsule that was 5.0 cm × 4.0 cm. The two masses in the left liver lobe were solid and were 9.5 cm × 6.5 cm × 5 cm and 3.2 cm × 2.0 cm in size, respectively. Microscopically, the tumor in the right liver lobe consisted of adipose tissue and hematopoietic elements containing erythroid tissue, megakaryocytes and myeloid colonies, consistent with a myelolipoma (Figure 2A and B). Tumor cells in the left liver lobe were in a funicular arrangement and showed invasive growth with significant atypia, compatible with malignant hepatic cancers (Figure 2C and D). Immunohistochemical investigation showed that hepatocyte and CD34 proteins were positive in the tumors of the left liver lobe (Figure 3), while AFP, GPC-3, HMB45, Melan-A and SMA were negative. Finally, the tumor in the right liver lobe was diagnosed as a hepatic myelolipoma, and the tumors in the left liver lobe were diagnosed as HCCs. After surgery, the patient developed an intra-abdominal infection and was hospitalized for 27 d. Unfortunately, two months later, a CT scan of the liver suggested the recurrence of the HCC. The patient received four transcatheter arterial chemoembolization (TACE) procedures and one iodine 131I metuximab injection in our hospital. However, the HCC metastasized to the lung eight months after surgery. The patient was then lost after nine months of follow-up.
Myelolipoma is a rare type of benign, nonfunctioning tumor of mesenchymal origin, which is composed of various proportions of fat and hematopoietic cells[14]. As such, it resembles a site of extramedullary hematopoiesis. The adrenal gland is the most common site of myelolipomas; autopsy series have revealed the prevalence of myelolipomas in the adrenal gland at autopsy to be 0.08%-0.8%[2,15,16]. Extraadrenal myelolipomas are very rare[17]. They have been reported in the parietal pleura[18], presacral area[19], intrathoracic paravertebral area[20], mediastinum[21,22], gastric antrum[23], perirenal tissue[24], and right iliac fossa[25]. To date, only ten cases of hepatic myelolipomas have been reported in the English-language medical literature[3-12] (Table 1). In one of these cases, the hepatic myelolipoma was found in a HCC[6]. In the present study, we report the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient. Table 2 summarizes the clinical data from all 11 cases of hepatic myelolipoma reported in the English-language medical literature, including the present study. Continuous variables were summarized as the mean ± the standard deviation (SD) and the range. Statistical analyses were conducted using SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, United States). The mean age of these patients was 51.45 ± 16.74 years (range 25-76 years) and the male-female ratio was 5:6. Forty percent of patients were asymptomatic; most patients were symptomatic. The right liver lobe was the reported site of the myelolipoma in nine (81.82%) of the patients; the left liver lobe was the reported site in 2 patients. The mean tumor size was 6.69 ± 4.71 cm (range 1.4-15 cm). Seven patients (63.64%) underwent tumor resection.
| Ref. | Year | Sex/age | Symptom | location | Imaging method | Number | Size (cm) | Treatment |
| Present case | 2016 | F/26 | Upper abdomen pain | Right liver lobe | CT | Solitary | 5.0 | Resection |
| Menozzi et al[3] | 2016 | F/72 | Asymptomatic | Right liver lobe | US, CT, CEUS | Solitary | 3.5 | NA |
| Radhi[4] | 2010 | M/76 | Symptoms related to a urinary tract infection | Segment VIII of the right liver | US, CT | Solitary | 3.2 | NA |
| Savoye-Coll et al[5] | 2000 | M/25 | Asymptomatic | Segment IV | MRI | Solitary | 9.0 | Left hepatectomy |
| Van et al[6] | 1994 | M/57 | Asymptomatic | Right liver lobe | US, CT | Solitary | 1.4 | Hemihepatectomy |
| Moreno et al[7] | 1991 | M/40 | Malaise, anorexia, fever | Right liver lobe | X-rays, CT, Radioisotope scan | Solitary | 15.0 | Right hepatic lobectomy |
| Nishizaki et al[8] | 1989 | F/56 | Right upper abdominal pain | Right post segment | US; CT, Hepatic arteriography | Solitary | 5.5 | Right posterior segmentectomy |
| subcapsule | ||||||||
| Kaurich et al[9] | 1988 | F/42 | Asymptomatic | Left liver lobe | US; CT, Hepatic arteriography | Solitary | 6.0 | Resection |
| Mali et al[10] | 1986 | M/63 | Hepatomegaly | Right liver lobe subcapsule | US; CT | Solitary | 15.0 | No treatment |
| Rubin et al[11] | 1984 | F/56 | Abdominal pain, RUQ tenderness | Right post segment subcapsule | CT, Hepatic arteriography | Solitary | 8.0 | Resection |
| AFIP case[12] | 1976 | F/53 | NA | Left liver lobe | NA | Solitary | 2.0 | NA |
| n (%) or mean ± SD (range) | |
| Age (yr) (n = 11) | |
| Mean | 51.45 ± 16.74 (25-76) |
| Sex (male/female), (male %) (n = 11) | 5/6 (45.45) |
| Symptoms (n = 10) | |
| Asymptomatic | 4 (40.00) |
| Symptomatic (n = 10) | |
| Abdominal pain | 3 (30.00) |
| Symptoms related to a urinary tract infection | 1 (10.00) |
| Malaise | 1 (10.00) |
| Anorexia | 1 (10.00) |
| Fever | 1 (10.00) |
| Hepatomegaly | 1 (10.00) |
| Location (n = 11) | |
| Right liver lobe | 9 (81.82) |
| Left liver lobe | 2 (18.18) |
| Mean size (cm) (n = 11) | 6.69 ± 4.71 (1.4-15) |
| Operation (n = 11) | |
| Resection | 7 (63.64) |
| No resection | 1 (9.09) |
| Not available | 3 (27.27) |
The etiology of hepatic myelolipoma remains uncertain. An ectopic adrenal gland is one hypothesis[8]. Most myelolipomas are reported in the adrenal gland. Anatomically, the right adrenal gland is adjacent to the right lobe of the liver, and an ectopic adrenal gland rarely appears in liver parenchyma[8]. Except for two cases, hepatic myelolipomas were found in the subcapsular region of the right liver lobe, including in our case. Emboli from bone marrow represent another hypothesis for the histogenesis of these lesions[4]. Although the gross appearance of a myelolipoma suggests a neoplastic origin, light and electron microscopy studies have revealed the polyclonal character of the hematopoietic cells[26]. The definitive stimulus that causes the hematopoietic and fat cells to proliferate remains enigmatic. Several studies have suggested that tissue necrosis is the basic stimulus[6,26]. For example, Van Hoe et al[6] speculated that the presence of foci of tumor necrosis may be associated with the development of a myelolipoma. Malignant tumors, hypertension, obesity, burns, and endocrinopathies have also been reported to be associated with the development of a myelolipoma[26].
The preoperative diagnosis of a hepatic myelolipoma is challenging. The appearance of myelolipomas on US, CT, and MRI images depends on the proportions of fat relative to myelogenous components[6]. US imaging reveals the myelolipoma to be a hyperechoic lesion[5,8]. Unenhanced CT images usually show that the tumor is well-encapsulated and has low-density areas varying from -69 to 28 HU as a result of intratumoral hemorrhage and varying proportions of fat and bone marrow elements[6,9]. On enhanced CT images, the tumor appears moderately enhanced. The area of low density remains hypoattenuated[27]. On T1-weighted MR images, the mass usually appears well marginated with a capsule, shows heterogeneous hyperintensity and contains necrosis. Hepatic arteriography reveals a hypervascular mass with an avascular zone[8,11]. On T2-weighted images, the mass shows heterogeneous low-signal intensity. After the administration of a gadolinium bolus, the lesion may show delayed heterogeneous enhancement[5,28]. Hepatic myelolipoma should be distinguished from other hepatic lesions that cause lipomatous masses, including lipomas, angiomyolipomas, metastatic dermoid tumors, Langerhans cell histiocytosis, and focal fatty infiltration[29]. Areas of fatty degeneration can also be observed occasionally in HCCs and hepatic adenomas[30].
Although myelolipomas are benign, these types of tumor can be symptomatic and may increase in size. Thus, surgical intervention is warranted when the tumor is symptomatic or difficult to diagnose. In the present study, the hepatic myelolipoma could not be preoperatively diagnosed precisely. Furthermore, two HCCs were synchronously found in the left liver lobe. HCC is the sixth most common malignancy worldwide and has the third highest mortality among cancer patients[31,32], for whom surgical resection is the most common and effective therapeutic method. Accordingly, we performed a right hepatectomy and a left hepatic lobectomy to completely resect the hepatic myelolipoma and HCCs. Because the gallbladder was close to the tumor, a cholecystectomy was also performed. Histopathologic and immunohistochemical analyses of the surgical specimen confirmed the diagnosis of hepatic myelolipoma and HCCs. Microscopically, the hepatic myelolipoma was composed of fat cells and hematopoietic cells, including mature and developing myeloid, erythroid, and megakaryocytic cells. Marrow-like areas were also clearly observed.
In conclusion, hepatic myelolipoma is extremely rare. To our knowledge, only 10 cases have been reported in the English-language medical literature. In one of these cases, the myelolipoma was found within a HCC. In the present study, we report the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient, who received a right hepatectomy, a left hepatic lobectomy, and a cholecystectomy.
A 26-year-old female was admitted to our hospital because of a 4-d history of upper abdominal pain.
Abdomen was soft, lax, and non-distended, with no palpable mass.
Differential diagnoses included lipomas, angiomyolipomas, metastatic dermoid tumor, and Langerhans cell histiocytosis.
Abnormal laboratory results: alpha fetoprotein (AFP), 7529.2 ng/mL (normal, 20); carbohydrate antigen 125, 99.4 U/mL (normal, 0-35); serum creatinine, 42 μmol/L (normal, 45-84); serum sodium 131 mmol/L (normal, 136-145); glutamyl transpeptidase, 103 U/L (normal, 7-32); fibrinogen, 4.45 g/L (normal, 2.00-4.00); and D-2-dimer, 9611 μg/L (normal, 0-700).
The unenhanced computed tomography (CT) images showed a well-defined low-density mass with adipose components in the right liver lobe, 4.2 cm × 4.1 cm in size. Two inhomogeneous low-density masses were found in the left liver lobe, 8.6 cm × 7.7 cm and 2.6 cm × 2.6 cm in size. In the contrast-enhanced CT images, the masses in both the right and left liver lobes were heterogeneously enhanced. Based on the results of the imaging examination, the mass in the right liver lobe was preliminarily considered to be a hamartoma, and the two masses in the left liver lobe were preliminarily considered to be hepatocellular carcinoma (HCC).
Macroscopically, the two masses in the left liver lobe were solid and were 9.5 cm × 6.5 cm × 5 cm and 3.2 cm × 2.0 cm in size, respectively. The mass in the right liver lobe had a capsule, was solid and 5.0 cm × 4.0 cm in size. Microscopically, the tumor in the right liver lobe consisted of adipose tissue and hematopoietic elements containing erythroid tissue, megakaryocytes and myeloid colonies, which was consistent with a myelolipoma. The tumor cells in the left liver lobe were in a funicular arrangement and had invasive growth with significant atypia, which was compatible with malignant hepatic cancer. Immunohistochemical investigation showed that hepatocyte and CD34 proteins were positive in the tumors of the left liver lobe, while AFP, GPC-3, HMB45, Melan-A, and SMA were negative. Finally, the tumor in the right liver lobe was diagnosed as a hepatic myelolipoma, and the tumors in the left liver lobe were diagnosed as HCCs.
The authors performed a right hepatectomy, a left hepatic lobectomy and a cholecystectomy.
Hepatic myelolipoma is extremely rare. To date, only 10 cases have been reported in the English-language medical literature.
In the present study, the authors present the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient. Preoperative diagnosis of hepatic myelolipoma is challenging. Surgery is the most effective treatment for the tumor.
This study highlights the diagnosis and treatment of the first case of the synchronous occurrence of hepatic myelolipoma and HCCs in different liver sections of one patient. This study also presents a literature review to deepen our understanding of hepatic myelolipoma. The information included is worthwhile to the reader.
| 1. | Su HC, Huang X, Zhou WL, Dai J, Huang BX, Cao WL, Sun FK. Pathologic analysis, diagnosis and treatment of adrenal myelolipoma. Can Urol Assoc J. 2014;8:E637-E640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Olsson CA, Krane RJ, Klugo RC, Selikowitz SM. Adrenal myelolipoma. Surgery. 1973;73:665-670. [PubMed] |
| 3. | Menozzi G, Maccabruni V, Marini G, Froio E, Garlassi E. Contrast-enhanced ultrasound (CEUS) appearance of hepatic myelolipoma. J Ultrasound. 2016;19:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Radhi J. Hepatic myelolipoma. J Gastrointestin Liver Dis. 2010;19:106-107. [PubMed] |
| 5. | Savoye-Collet C, Goria O, Scotté M, Hemet J. MR imaging of hepatic myelolipoma. AJR Am J Roentgenol. 2000;174:574-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Van Hoe L, Gryspeerdt S, Van Eycken P, Baert AL, Marchal G. Myelolipoma in a hepatocellular carcinoma: CT-pathologic correlation. AJR Am J Roentgenol. 1994;163:1111-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 7. | Moreno Gonzalez E, Seoane Gonzalez JB, Bercedo Martinez J, Santoyo Santoyo J, Gomez Sanz R, Vargas Castrijon J, Ballestin Carcavilla C, Garcia Mauriño ML, Colina Ruiz-Delgado F. Hepatic myelolipoma: new case and review of the literature. Hepatogastroenterology. 1991;38:60-63. [PubMed] |
| 8. | Nishizaki T, Kanematsu T, Matsumata T, Yasunaga C, Kakizoe S, Sugimachi K. Myelolipoma of the liver. A case report. Cancer. 1989;63:930-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Kaurich JD, Coombs RJ, Zeiss J. Myelolipoma of the liver: CT features. J Comput Assist Tomogr. 1988;12:660-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Mali SP, Gratama S, Mulder H. Myelolipoma of the liver. Rofo. 1986;144:610-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Rubin E, Russinovich NA, Luna RF, Tishler JM, Wilkerson JA. Myelolipoma of the liver. Cancer. 1984;54:2043-2046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Ishak KG. Mesenchymal tumors of the liver. Hepatocellular carcinoma. London: John Wiley and Sons, Inc 1976; 247-307. |
| 13. | Grosdidier J, Boissel P, Macinot C, Drouin P. Hepatic myelolipoma. Apropos of a case. Nouv Presse Med. 1973;2:1777-1779. [PubMed] |
| 14. | Baisakh MR, Chattoraj A, Narayanan R, Mohanty R, Mishra M. Adrenal myelolipoma: A rare lesion of adrenal gland. Indian J Cancer. 2015;52:597-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Mcdonnell WV. Myelolipoma of adrenal. AMA Arch Pathol. 1956;61:416-419. [PubMed] |
| 16. | Snearly RG, Ram MD. Myelolipoma of adrenal. Urology. 1978;11:411-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Suárez-Peñaranda JM, Bermúdez Naveira A, Fraga M, Aliste-Santos C, Cordeiro C, Muñoz-Barús JI. Unusual Forms of Adrenal and Extra-Adrenal Myelolipomas. Int J Surg Pathol. 2014;22:473-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Zhang DS, Li DH, Bi HX, Wu XF. [Gastric adenocarcinoma associated with myelolipoma of parietal pleura: a case report]. Zhonghua Bing Li Xue Za Zhi. 2006;35:437. [PubMed] |
| 19. | Prahlow JA, Loggie BW, Cappellari JO, Scharling ES, Teot LA, Iskandar SS. Extra-adrenal myelolipoma: report of two cases. South Med J. 1995;88:639-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Rigoli E, Dallabernardina L. Intrathoracic myelolipoma. (intrathoracic tumor-like extramedullary erythropoiesis). Riv Anat Patol Oncol. 1964;25:LV-LXXX. [PubMed] |
| 21. | Migliore M, Calvo D, Criscione A, Caltabiano R, Platania N, Barbagallo G, Albanese V. An unsual symptomatic case of mediastinal myelolipoma treated by VATS approach. Ann Ital Chir. 2014;85:85-87. [PubMed] |
| 22. | Himuro N, Minakata T, Oshima Y, Tomita Y, Kataoka D, Yamamoto S, Kadokura M. Video-assisted thoracic surgery for primary myelolipoma of the posterior mediastinum. J Cardiothorac Surg. 2016;11:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Yildiz BD. Giant Extra-Adrenal Retroperitoneal Myelolipoma With Incidental Gastric Mesenchymal Neoplasias. Int Surg. 2015;100:1018-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Brandler TC, Reder I, Kahn L. Perirenal myelolipoma diagnosed on imprint: case report and review of the literature. Diagn Cytopathol. 2015;43:230-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Surabhi VR, Menias C, Prasad SR, Patel AH, Nagar A, Dalrymple NC. Neoplastic and non-neoplastic proliferative disorders of the perirenal space: cross-sectional imaging findings. Radiographics. 2008;28:1005-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Bautista DV, Asch M, Kovacs K, Murray D. Adrenal myelolipomatous nodules mimicking adrenal neoplasms: report of three cases. Can J Surg. 1989;32:51-55. [PubMed] |
| 27. | Orlandi A, Marino B, De Dona G, Cefaro A, Spagnoli LG. [Clinico-pathological considerations about a case of hepatic myelolipoma]. Ann Ital Chir. 1994;65:253-256. [PubMed] |
| 28. | Kenney PJ, Wagner BJ, Rao P, Heffess CS. Myelolipoma: CT and pathologic features. Radiology. 1998;208:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 168] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Roberts JL, Fishman EK, Hartman DS, Sanders R, Goodman Z, Siegelman SS. Lipomatous tumors of the liver: evaluation with CT and US. Radiology. 1986;158:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 52] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Yoshikawa J, Matsui O, Takashima T, Ida M, Takanaka T, Kawamura I, Kakuda K, Miyata S. Fatty metamorphosis in hepatocellular carcinoma: radiologic features in 10 cases. AJR Am J Roentgenol. 1988;151:717-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 87] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20108] [Cited by in RCA: 20722] [Article Influence: 1883.8] [Reference Citation Analysis (23)] |
| 32. | Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3249] [Cited by in RCA: 3630] [Article Influence: 259.3] [Reference Citation Analysis (12)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Goral V, Lee CL S- Editor: Gong ZM L- Editor: A E- Editor: Wang CH