Published online Nov 14, 2016. doi: 10.3748/wjg.v22.i42.9387
Peer-review started: June 22, 2016
First decision: August 22, 2016
Revised: September 6, 2016
Accepted: October 10, 2016
Article in press: October 10, 2016
Published online: November 14, 2016
Processing time: 143 Days and 18.2 Hours
To examine the influence of night duty (ND) on endoscopic therapy for biliary duct stones.
The subjects consisted of 133 patients who received initial endoscopic therapy for biliary duct stones performed by eight endoscopists after they had been on (ND group, n = 34 patients) or not [day duty (DD) group, n = 99 patients]. Patient characteristics (age, gender, history of abdominal surgery, transverse diameter of the largest stone, number of stones), years of experience of the endoscopists, endoscopic procedures [sphincterotomy, papillary balloon dilation (EPBD), papillary large balloon dilation (EPLBD)], and outcomes of initial endoscopy (procedure time; rate of stone removal by the first endoscopist; procedure success rate by the first endoscopist: removal of stones or endoscopic retrograde biliary drainage; rate of final stone removal; final procedure success rate; complications; hospitalization after the procedure) were compared retrospectively between the two groups. History of abdominal surgery and treatment outcomes were also compared between the groups for each of the four endoscopists who performed most of the procedures in the ND group.
There were no significant differences regarding the number of treatments performed by each endoscopist or the years of experience between the ND and DD groups. The frequency of endoscopic retrograde cholangiopancreatography procedures did not differ significantly between the groups. There were also no significant differences regarding patient characteristics: age, gender, history of abdominal surgery (ND 7: Billroth II 4, R-Y 3; DD 18: double tract reconstruction 1, Billroth I 3, Billroth II 6, R-Y 7, duodenoduodenostomy for annular pancreas 1), transverse diameter of largest stone, and number of stones between the two groups. Among the treatment procedures, the endoscopic sphincterotomy and EPBD rates did not differ significantly between the groups. However, EPLBD was performed more frequently in the ND group [47.1% (16/34) vs 19.2% (19/99)]. Regarding outcomes, there were no significant differences in the rate of stone removal, procedure success rate, complications (ND: pancreatitis 1; DD: pancreatitis 6, duodenal bleeding 1, decreased blood pressure 1, hypoxia 2), or hospitalization after the procedure. However, the procedure time was significantly longer in the ND group (71.5 ± 44.7 vs 54.2 ± 28.8). Among the four endoscopists, there were no significant differences in patient history of abdominal surgery, removal of stones, or procedure success rate. However, the procedure time for one endoscopist was significantly longer in the ND group.
The time required for endoscopic therapy for bile duct stones might be influenced by ND.
Core tip: Sleep deprivation affects brain activation, and therefore disturbs cognitive ability and reduces work efficiency. In the clinical field, night duty (ND) might affect surgical outcomes and the number of medical errors. In this study, we examined the influence of ND on endoscopic therapy for biliary duct stones. The procedure was significantly longer when performed by endoscopists after they had been on ND. The time required for endoscopic therapy for bile duct stones might be influenced by ND.
- Citation: Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Watanabe K, Nakamura J, Kikuchi H, Waragai Y, Takasumi M, Hikichi T, Ohira H. Influence of night duty on endoscopic therapy for bile duct stones. World J Gastroenterol 2016; 22(42): 9387-9393
- URL: https://www.wjgnet.com/1007-9327/full/v22/i42/9387.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i42.9387
Sleep deprivation disturbs cognitive ability, and sleep is important to maintain concentration[1]. Sleep deprivation also reduces work efficiency and changes brain activation[2-7]. However, most reports in the clinical field indicate that sleeping hours or night duty (ND) do not influence surgery. In Ellman et al[8] and Chu et al[9], sleeping hours did not affect outcomes after cardiac surgery. In Sharpe et al[10] complications and re-hospitalization 30 d after abdominal surgery (hernia repair, cholecystectomy, intestinal operations) did not differ significantly between doctors who were and were not on ND on the previous day. Most recently, Govindarajan et al[11] reported that prior night work did not affect outcomes for gastroenterology surgeries, hysterectomy, orthopedic surgeries, lung resection, craniotomy, or angioplasty. However, in Rothschild et al[12], complications were more frequent after surgery performed by surgeons with a prior sleep time of less than 6 h, and serious medical errors have been associated with interns working for more than 24 h[13].
Endoscopic therapy requires considerable concentration, but the dependence of outcomes on sleep time or ND has not been examined. Therefore, in this study, we investigated the influence of ND on endoscopic therapy for bile duct stones.
This study was performed as a retrospective analysis of clinical data. Written consent for endoscopic therapy was obtained from the patients. Informed consent for this study was not required. The ethics committee of Fukushima Medical University approved the study, and the details of the study are published on the homepage of Fukushima Medical University (authorization No. 2453).
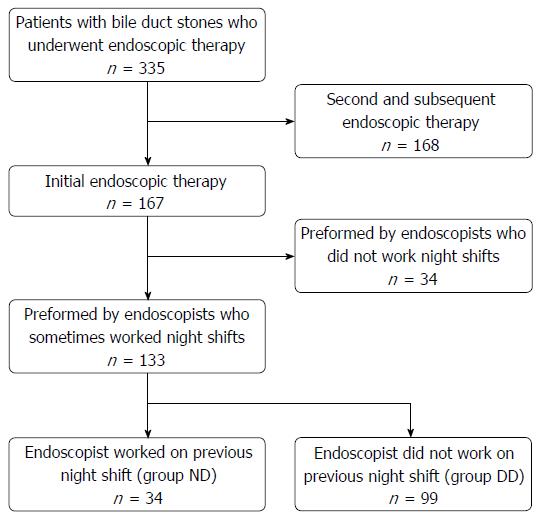
Among 335 patients treated with endoscopic therapy for bile duct stones from January 2011 to December 2015 at Fukushima Medical University Hospital, 167 underwent initial endoscopic therapy and had stones confirmed via computed tomography or endoscopic retrograde cholangiography (Figure 1). Among these patients, data from 133 patients treated by eight endoscopists (A-H) were evaluated in this study. In total, 34 patients were treated by an endoscopist after they had been on ND the previous day (ND group), and 99 patients were treated by the same endoscopists when they had not been on ND the previous day (day duty, DD group) (Table 1). ND was defined as performing normal ward duties in the hospital overnight and sometimes examining emergency patients.
| Item | ND Group | DD Group | P value |
| (n = 34) | (n = 99) | ||
| Endoscopists (years of experience) | 0.527 | ||
| A (14-19) | 5 | 11 | |
| B (6-9) | 7 | 17 | |
| C (6-8) | 8 | 21 | |
| D (6-11) | 5 | 16 | |
| E (7-12) | 2 | 22 | |
| F (10-15) | 3 | 7 | |
| G (5-8) | 3 | 4 | |
| H (3-7) | 1 | 1 | |
| Years of experience, mean ± SD | 9.3 ± 3.9 | 9.4 ± 3.4 | 0.830 |
The following items were compared between the ND and DD groups: years of experience of the endoscopists, patient characteristics (age, gender, history of abdominal surgery, transverse diameter of the largest stone, number of stones), endoscopic procedure [sphincterotomy (EST), papillary balloon dilation (EPBD), papillary large balloon dilation (EPLBD)], treatment outcomes (procedure time; removal of stones by the first endoscopist; procedure success rate by the first endoscopist: removal of stones or endoscopic retrograde biliary drainage; final rate of stone removal; final procedure success rate; complications; and hospitalization after procedure). The outcomes related to the second (or more) endoscopist were included in the study: rate of final stone removal and final procedure success rate. History of abdominal surgery and treatment outcomes (procedure time, removal of stones, procedure success rate) were also compared between the two groups for each of the four endoscopists (A-D) who treated many of the patients in the ND group. The main outcome was a comparison of treatment results to evaluate the work efficiency in the ND and DD groups.
Endoscopic retrograde cholangiopancreatography (ERCP)-related procedures were performed for patients with stable breathing and hemodynamics. Before ERCP, patients were sedated with midazolam under observation of blood pressure and oxygen saturation. However, patients in septic shock were not sedated. Most procedures were performed with a JF 260V endoscope (Olympus, Tokyo, Japan). A Q260J (Olympus) was used for double tract reconstruction in proximal gastrectomy, a PCF-Q260AI or Q260J (Olympus) was used for Billroth II (B-II) procedures, and a PCF-Q260AL (Olympus) was used for Roux-en-Y (R-Y). For R-Y after choledocojejunostomy, the bile duct-jejunum anastomosis was accessed with a SIF-Q260 (Olympus) and a sliding tube. The balloon of the sliding tube was expanded, fixed and placed, and endoscopy with a PCF-PQ260AI (Olympus) was then performed through the sliding tube.
EST was performed using Clever Cut (Olympus). In cases in which it was difficult to cannulate the biliary duct, or for patients with a history of abdominal surgery, an RX needle knife XL (Boston Scientific, Tokyo, Japan) was used. EPBD was performed if the transverse diameter of the largest stone was > 8 mm and bile duct stones were difficult to remove only by EST or if a perivaterian diverticulum was present. A Hurricane RX Biliary Balloon Dilation Catheter (Boston Scientific) was used for EPBD. EPLBD was performed if the transverse diameter of the largest stone was > 12 mm, if many bile duct stones were difficult to remove only by EST or if sufficient EST was difficult because of a parapapillary diverticulum or history of abdominal surgery. A CRE Biliary Balloon Dilation Catheter (Boston Scientific) or a Giga (Century Medical, Tokyo, Japan) was used for EPLBD. A Trapezoid RX basket catheter (Boston Scientific) and a LithoCrush V, FG-V435P (Olympus) were used as tools to crush stones.
Years of experience of endoscopists, patient age, transverse diameter of the largest stone, number of stones, and hospitalization after the procedure were compared by Student’s t tests. The number of procedures performed by each endoscopist in the ND and DD groups, patient gender, history of abdominal surgery, EPLBD, rate of stone removal by the first endoscopist, rate of final stone removal and procedure success rate by the first endoscopist were compared by the χ2 test. Procedure time was compared with the Welch t test. EST, EPBD, complications, final procedure success rate and items for each endoscopist (history of abdominal surgery, removal of stones rate, procedure success rate) were compared by the Fisher exact probability test. The procedure time for each endoscopist was compared by the Mann-Whitney U test. P < 0.05 was considered to be significant. All analyses were performed using Statcel 3 (OMS Edition, Saitama, Japan).
There were no significant differences regarding the number of treatments performed by each endoscopist or in the years of experience between the ND and DD groups (Table 1). The frequency of ERCP did not differ significantly between the groups. There were also no significant differences in patient characteristics regarding age, gender, history of abdominal surgery (ND 7: Billroth II 4, R-Y 3; DD 18: double tract reconstruction 1, Billroth I 3, Billroth II 6, R-Y 7, duodenoduodenostomy for annular pancreas 1), transverse diameter of the largest stone, and number of stones between the two groups (Table 2).
| ND Group | DD Group | P value | |
| (n = 34) | (n = 99) | ||
| Age (yr), mean ± SD | 73.1 ± 13.0 | 72.4 ± 14.3 | 0.801 |
| Gender (M/W) | 21/13 | 59/40 | 0.824 |
| History of abdominal surgery, n (%) | 7 (20.6) | 18 (18.2) | 0.757 |
| Double tract reconstruction, n | 1 | ||
| Billroth I | 3 | ||
| Billroth II | 4 | 6 | |
| Roux-en-Y | 3 | 7 | |
| Duodenoduodenostomy | 1 | ||
| Transverse diameter of the largest stone (mm), mean ± SD | 10.6 ± 4.6 | 10.3 ± 4.9 | 0.735 |
| Number of stones, mean ± SD | 2.8 ± 4.0 | 2.8 ± 3.6 | 1.0 |
Among the treatment procedures, the rates of EST and EPBD did not differ significantly between the groups, but EPLBD was performed more frequently in the ND group [47.1% (16/34) vs 19.2% (19/99)] (Table 3). Regarding outcomes, there were no significant differences in the rate of stone removal and procedure success rate, complications (ND: pancreatitis 1; DD: pancreatitis 6, duodenal bleeding 1, decreased blood pressure 1, hypoxia 2), or hospitalization after the procedure (Table 4). However, the procedure time was significantly longer in the ND group (71.5 ± 44.7 vs 54.2 ± 28.8).
| ND Group | DD Group | P value | |
| (n = 34) | (n = 99) | ||
| EST | 32 (94.1) | 83 (83.8) | 0.107 |
| EPBD | 0 (0) | 6 (6.1) | 0.163 |
| EPLBD | 16 (47.1) | 19 (19.2) | 0.001 |
| ND Group | DD Group | P value | |
| (n = 34) | (n = 99) | ||
| Procedure time (min), mean ± SD | 71.5 ± 44.7 | 54.2 ± 28.8 | 0.043 |
| Rate of stone removal by first endoscopist | 13 (38.2) | 52 (52.5) | 0.150 |
| Procedure success rate by first endoscopist | 18 (52.9) | 57 (57.6) | 0.638 |
| Rate of final stone removal | 24 (70.6) | 66 (66.7) | 0.67 |
| Final procedure success rate | 33 (97.1) | 90 (90.9) | 0.22 |
| Complications | 1 (2.9) | 11 (11.1) | 0.136 |
| Pancreatitis | 1 | 6 | |
| Duodenal bleeding | 2 | ||
| Decreased blood pressure | 1 | ||
| Hypoxia | 2 | ||
| Hospitalization after procedure (d), mean ± SD | 7.1 ± 7.6 | 6.6 ± 6.6 | 0.715 |
For each of the four endoscopists A-D, there were no significant differences in patient history of abdominal surgery, rate of stone removal, and procedure success rate. However, the procedure time for endoscopist D was significantly longer in the ND group (Table 5).
| ND Group | DD Group | P value | |
| Endoscopist A | |||
| n | 5 | 11 | |
| Procedure time (min), median ± SD | 90.0 ± 80.8 | 90.0 ± 39.7 | 0.910 |
| Rate of stone removal | 3 (60.0) | 6 (54.5) | 0.635 |
| Procedure success rate | 5 (100) | 9 (81.8) | 0.458 |
| Endoscopist B | |||
| n | 7 | 17 | |
| Procedure time (min), median ± SD | 40.0 ± 20.4 | 50.0 ± 26.0 | 0.589 |
| Rate of stone removal | 5 (71.4) | 11 (64.7) | 0.572 |
| Procedure success rate | 5 (71.4) | 12 (70.6) | 0.607 |
| Endoscopist C | |||
| n | 8 | 21 | |
| Procedure time (min), median ± SD | 75.0 ± 39.6 | 50.0 ± 27.1 | 0.113 |
| Rate of stone removal | 3 (37.5) | 7 (33.3) | 0.745 |
| Procedure success rate | 4 (50.0) | 10 (47.6) | 0.617 |
| Endoscopist D | |||
| n | 5 | 16 | |
| Procedure time (min), median ± SD | 60 ± 31.5 | 40 ± 14.7 | 0.017 |
| Rate of stone removal | 1 (20) | 8 (50) | 0.258 |
| Procedure success rate | 1 (20) | 10 (62.5) | 0.126 |
In this report, we examined the influence of ND on endoscopic therapy for bile duct stones. The rate of EPLBD and the procedure time were significantly greater for endoscopists after ND. The procedure time was also longer in the ND group for one endoscopist.
Although more EPLBD procedures were performed in the ND group, the patients who met the criteria for EPLBD described in the Materials and Methods were not significantly different between the ND group and the DD group according to the results of χ2 tests (Table 6). Fewer EPLBD procedures were performed in the DD group for several reasons. However, it has been shown that EPLBD shortens the procedure by allowing easier removal of stones or at least does not extend the procedure time[14,15]. Based on these earlier reports, we suggest that EPLBD did not contribute to the longer procedure time in the ND group.
| ND Group | DD Group | P value | |
| (n = 34) | (n = 99) | ||
| Patients with EPLBD indication, n (%) | 20 (58.8) | 44 (44.4) | 0.15 |
| Patients in whom EPLBD was performed (shown in Table 3) | 16 | 19 | |
| Reasons for not performing EPLBD | |||
| AOSC | 1 | 5 | |
| Narrow lower bile duct | 1 | 1 | |
| Biliary stricture | 1 | 0 | |
| Minor bleeding of Vater’s papilla | 1 | 0 | |
| No insurance coverage for EPLBD | 0 | 5 | |
| 96 years old and performance status 3 | 0 | 1 | |
| Gallstone pancreatitis | 0 | 3 | |
| Antithrombotic drug therapy | 0 | 4 | |
| Difficulty identifying the biliary anastomotic region | 0 | 2 | |
| Smaller stones on visual inspection | 0 | 2 | |
| Difficulty identifying the Vater papilla | 0 | 1 | |
| Double tract reconstruction | 0 | 1 |
The cause of the longer procedure time for endoscopists after ND might be the influence of sleep deprivation or lower sleep quality on work efficiency. The attention, vigilance, and driving tasks of residents during heavy night call rotations were equivalent to those for residents with a 0.04 to 0.05 g % blood alcohol concentration during a light call rotation[16]. Sanches et al[17] also found that the psychomotor performance of young doctors on night shifts was lower than that of young doctors who were not assigned night work. Thus, ND may influence the procedure time of endoscopic therapy for bile duct stones.
In this study, there was no significant difference in complications between procedures performed by endoscopists who had and had not been on prior ND, but an extended procedure time has been reported to be a risk factor for post-ERCP pancreatitis[18,19]. In addition, Pan et al[20] found that a cannulation challenge to the common bile duct within 10 min gave the best results in trials by trainees. Therefore, if a procedure is slow by an endoscopist working after ND, it might be advisable to change the endoscopist.
There are several limitations to this study, including its retrospective design and the small number of cases of ERCP for bile duct stones at a single institution. We perform 400 ERCP procedures each year. However, in this study, we only included patients treated by endoscopists who had been on ND and performed the initial endoscopic therapy for bile duct stones. This resulted in a small number of eligible subjects. However, restricting the endoscopic procedures to the treatment of bile duct stones allowed for a more precise evaluation of the influence of ND compared to previous studies that considered the effect of ND on multiple types of surgery[8-12]. Secondly, we did not measure the exact sleep time of the endoscopists. However, night shifts and on-call duty have been found to influence circadian rhythm and worsen quality of sleep[21,22]. A difference in bedding also influences quality of sleep[23-26], and, therefore, ND itself is likely to influence quality of sleep. Thirdly, we were unable to compare the number of biliary duct cannulation challenges between the two groups to evaluate the direct influence of ND on the endoscopic procedure due to a lack of precise records. A further study of the number of biliary duct cannulations is desirable.
Within these limitations, we conclude that the procedure time for endoscopic therapy for bile duct stones is increased by the influence of ND. Substitution of an endoscopist after ND might be advisable to shorten the procedure.
We thank all the staff of the Department of Endoscopy of Fukushima Medical University Hospital, the Department of Gastroenterology and Rheumatology of Fukushima Medical University, and the gastroenterology ward of Fukushima Medical University Hospital. We also thank PALABRA and American Journal Experts for English proofreading services.
Concentration was affected by sleep deprivation. Recently, sleep deprivation or night duty (ND) was reported to influence several medical activities. However, the relationship between endoscopic therapy and sleep deprivation or ND was uncertain.
Endoscopic therapy for bile duct stones requires much concentration. In Japan, many endoscopists perform endoscopic therapy after ND. This study clarified the influence of ND on endoscopic therapy for bile duct stones.
There have been no reports about the influence of ND on endoscopic therapy. In this report, ND the previous day influenced the procedure time for endoscopic therapy for bile duct stones.
This study suggested that ND the previous day influenced the procedure time of endoscopic therapy for bile duct stones. According to this result, if the first endoscopist who was on ND the previous day experiences difficulty in the endoscopic procedure, it is advisable to change endoscopists earlier.
ERCP: endoscopic procedure that contrasts biliary duct and pancreatic duct using X-ray equipment; EST: endoscopic procedure that incises the papilla of Vater; EPBD: endoscopic procedure that dilates the biliary exit to remove the stones; EPLBD: endoscopic procedure that dilates the biliary exit using a large balloon catheter to remove large stones or many stones.
This study is innovative, and the conclusion is instructive and practical for endoscopic management of bile duct stones.
| 1. | Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep. 1996;19:318-326. [PubMed] |
| 2. | Chee MW, Choo WC. Functional imaging of working memory after 24 hr of total sleep deprivation. J Neurosci. 2004;24:4560-4567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 318] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 3. | Chee MW, Chuah LY, Venkatraman V, Chan WY, Philip P, Dinges DF. Functional imaging of working memory following normal sleep and after 24 and 35 h of sleep deprivation: Correlations of fronto-parietal activation with performance. Neuroimage. 2006;31:419-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 191] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 4. | Chee MW, Tan JC, Zheng H, Parimal S, Weissman DH, Zagorodnov V, Dinges DF. Lapsing during sleep deprivation is associated with distributed changes in brain activation. J Neurosci. 2008;28:5519-5528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 207] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 5. | Lim J, Tan JC, Parimal S, Dinges DF, Chee MW. Sleep deprivation impairs object-selective attention: a view from the ventral visual cortex. PLoS One. 2010;5:e9087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 6. | Chee MW, Tan JC, Parimal S, Zagorodnov V. Sleep deprivation and its effects on object-selective attention. Neuroimage. 2010;49:1903-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Kong D, Soon CS, Chee MW. Reduced visual processing capacity in sleep deprived persons. Neuroimage. 2011;55:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Ellman PI, Law MG, Tache-Leon C, Reece TB, Maxey TS, Peeler BB, Kern JA, Tribble CG, Kron IL. Sleep deprivation does not affect operative results in cardiac surgery. Ann Thorac Surg. 2004;78:906-911; discussion 906-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Chu MW, Stitt LW, Fox SA, Kiaii B, Quantz M, Guo L, Myers ML, Hewitt J, Novick RJ. Prospective evaluation of consultant surgeon sleep deprivation and outcomes in more than 4000 consecutive cardiac surgical procedures. Arch Surg. 2011;146:1080-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 10. | Sharpe JP, Weinberg JA, Magnotti LJ, Nouer SS, Yoo W, Zarzaur BL, Cullinan DR, Hendrick LE, Fabian TC, Croce MA. Outcomes of operations performed by attending surgeons after overnight trauma shifts. J Am Coll Surg. 2013;216:791-797; discussion 797-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Govindarajan A, Urbach DR, Kumar M, Li Q, Murray BJ, Juurlink D, Kennedy E, Gagliardi A, Sutradhar R, Baxter NN. Outcomes of Daytime Procedures Performed by Attending Surgeons after Night Work. N Engl J Med. 2015;373:845-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, Yu T, Yoon CS, Williams DH, Wien MF. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302:1565-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 181] [Article Influence: 10.6] [Reference Citation Analysis (1)] |
| 13. | Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838-1848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1174] [Cited by in RCA: 1127] [Article Influence: 51.2] [Reference Citation Analysis (0)] |
| 14. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 109] [Article Influence: 6.4] [Reference Citation Analysis (2)] |
| 15. | Kim HG, Cheon YK, Cho YD, Moon JH, Park DH, Lee TH, Choi HJ, Park SH, Lee JS, Lee MS. Small sphincterotomy combined with endoscopic papillary large balloon dilation versus sphincterotomy. World J Gastroenterol. 2009;15:4298-4304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 74] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294:1025-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 260] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 17. | Sanches I, Teixeira F, dos Santos JM, Ferreira AJ. Effects of Acute Sleep Deprivation Resulting from Night Shift Work on Young Doctors. Acta Med Port. 2015;28:457-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Uchino R, Isayama H, Tsujino T, Sasahira N, Ito Y, Matsubara S, Takahara N, Arizumi T, Toda N, Mohri D. Results of the Tokyo trial of prevention of post-ERCP pancreatitis with risperidone-2: a multicenter, randomized, placebo-controlled, double-blind clinical trial. Gastrointest Endosc. 2013;78:842-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Swahn F, Nilsson M, Arnelo U, Löhr M, Persson G, Enochsson L. Rendezvous cannulation technique reduces post-ERCP pancreatitis: a prospective nationwide study of 12,718 ERCP procedures. Am J Gastroenterol. 2013;108:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 20. | Pan Y, Zhao L, Leung J, Zhang R, Luo H, Wang X, Liu Z, Wan B, Tao Q, Yao S. Appropriate time for selective biliary cannulation by trainees during ERCP--a randomized trial. Endoscopy. 2015;47:688-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 21. | Lin YH, Ho YC, Lin SH, Yeh YH, Liu CY, Kuo TB, Yang CC, Yang AC. On-call duty effects on sleep-state physiological stability in male medical interns. PLoS One. 2013;8:e65072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Kim JY, Chae CH, Kim YO, Son JS, Kim JH, Kim CW, Park HO, Lee JH, Kwon SI. The relationship between quality of sleep and night shift rotation interval. Ann Occup Environ Med. 2015;27:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 23. | Jacobson BH, Wallace TJ, Smith DB, Kolb T. Grouped comparisons of sleep quality for new and personal bedding systems. Appl Ergon. 2008;39:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Jacobson BH, Boolani A, Smith DB. Changes in back pain, sleep quality, and perceived stress after introduction of new bedding systems. J Chiropr Med. 2009;8:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Shen L, Chen YX, Guo Y, Zhong S, Fang F, Zhao J, Hu TY. Research on the relationship between the structural properties of bedding layer in spring mattress and sleep quality. Work. 2012;41 Suppl 1:1268-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Jeon MY, Jeong H, Lee S, Choi W, Park JH, Tak SJ, Choi DH, Yim J. Improving the quality of sleep with an optimal pillow: a randomized, comparative study. Tohoku J Exp Med. 2014;233:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Sinha N, Wan SJ, Wang WX S- Editor: Yu J L- Editor: A E- Editor: Zhang FF