Published online Oct 21, 2016. doi: 10.3748/wjg.v22.i39.8849
Peer-review started: April 4, 2016
First decision: May 12, 2016
Revised: May 26, 2016
Accepted: July 20, 2016
Article in press: July 20, 2016
Published online: October 21, 2016
Processing time: 199 Days and 2.5 Hours
We present a unique case of crowned dens syndrome (CDS) that developed after endoscopic retrograde cholangiopancreatography (ERCP) in a patient who presented with fever and neck pain. Administration of non-steroidal anti-inflammatory drugs was extremely effective for relieving fever and neck pain, and in the improvement of inflammatory markers. To the best of our knowledge, this is the first case report of CDS caused by an ERCP procedure. In a patient with fever and neck pain after an ERCP procedure, CDS should be considered in the differential diagnosis.
Core tip: There are numerous differential diagnoses for patients with fever after an endoscopic retrograde cholangiopancreatography (ERCP). A careful evaluation of medical history and a physical examination provide clues to making a definitive diagnosis. Retrograde cholangitis is a well-known complication of ERCP; additionally, pseudogout is known to develop after severe illnesses or surgery. This case report describes a patient with pseudogout of the neck, which is also known as crowned dens syndrome (CDS). CDS should be considered in a patient with fever and neck pain after an ERCP procedure.
- Citation: Nakano H, Nakahara K, Michikawa Y, Suetani K, Morita R, Matsumoto N, Itoh F. Crowned dens syndrome developed after an endoscopic retrograde cholangiopancreatography procedure. World J Gastroenterol 2016; 22(39): 8849-8852
- URL: https://www.wjgnet.com/1007-9327/full/v22/i39/8849.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i39.8849
endoscopic retrograde cholangiopancreatography (ERCP) is an established technique for the removal of common bile duct stones in patients with cholangitis. It is well known that there are several complications that arise after ERCP, such as hemorrhage, gastrointestinal perforation, pancreatitis, and ascending cholangitis. Additionally, fever and neck pain are frequently encountered in clinical settings.
Crowned dens syndrome (CDS) is characterized by neck pain and fever, computed tomography (CT) findings of periodontoid calcification, and a clinical entity of pseudogout. Pseudogout is characterized by the involvement of large joints that most commonly affects knees and wrists. Radiographs demonstrate chondrocalcinosis within articular joints. Aspiration of joint fluid shows calcium pyrophosphate crystals in the joint space. The etiology of pseudogout still remains unclear; however, an excessive mechanical load on cervical motion may be a factor that triggers CDS. Here, we present a case of CDS in a patient who developed stiff neck pain after an ERCP procedure. We propose that CDS might be caused by the patient lying in the prone position in ERCP, as the patient is restricted of cervical rotation movements.
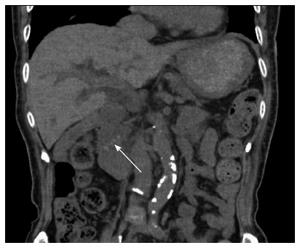
An 87-year-old woman with a past medical history of diabetes mellitus and hypertension presented to our hospital complaining of frequent vomiting and jaundice. She took anti-hypertensives and oral glycemic control medications. On arrival, she was alert and had stable vital signs, except for a low grade fever of 37.2 °C. Physical examination showed jaundice without epigastric tenderness, and Murphy’s sign. Laboratory tests showed a marked elevation of inflammatory markers and hepatobiliary enzymes, which showed the following lab values: WBC 11100/μL, CRP 14.27 mg/dL, procalcitonin 1.56 μg/L, AST 356 IU/L, ALT 174 IU/L, ALP 836 IU/L, γ-GTP 240IU/L, LDH 327 IU/L, and a total bilirubin of 5.7 mg/dL. Uric acid of 3.3 g/dL was within normal limits. Abdominal computed tomography (CT) revealed multiple stones in the bile duct (Figure 1). The patient was diagnosed with choledocholithiases and acute cholangitis with moderate severity[1], and emergency endoscopic stone removal with endoscopic sphincterotomy (EST) was performed on the day of admission (Figure 2), after which her symptoms resolved. We perform ERCP following sedation with hydroxyzine pamoate and pentazocine as premedication, and midazolam is administered intravenously. Additional midazolam is given in incremental doses during the procedure as needed.
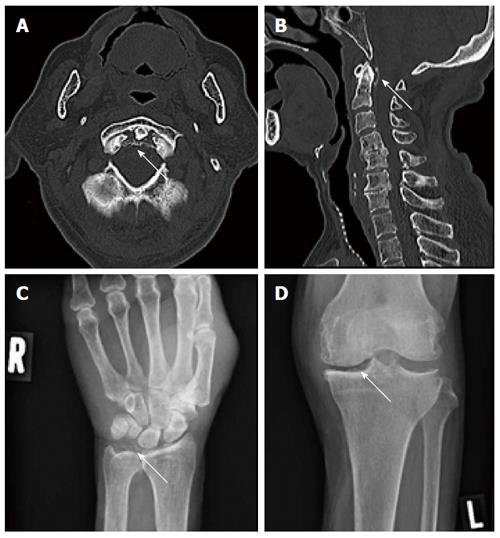
On day 2 after the ERCP procedure, her temperature rose to 38 °C without any elevation of serum biliary enzymes. As we suspected retrograde cholangitis, we continued to administer antibiotics; however, her temperature remained at 37-38 °C. On day 4, she complained of neck pain, right wrist pain, and left knee pain. The patient did not exhibit confusion or convulsion. In particular, neck pain was of moderate to severe intensity and was aggravated by the rotation of the head. Both neck stiffness and jolt accentuation of headaches was positive. Although serum biliary enzymes decreased after the ERCP procedure, laboratory tests showed a marked elevation of inflammatory markers. Based on her physical examination, the differential diagnosis was meningitis, retropharyngeal abscess, infective spondylitis, polymyalgia rheumatica, Lemierre’s syndrome, and CDS. Two sets of blood cultures were obtained to rule out bacteremia, and the results were later shown to be negative. A head CT revealed no space-occupying lesions; however, there was a sharply defined periodontoid calcification on the patient’s cervical CT (Figure 3A and B), which confirmed a diagnosis of CDS. In addition, radiographs of the wrist and knee showed crystal deposits in the joint spaces, which are consistent with a diagnosis of pseudogout (Figure 3C and D). She has never experienced nuchal pain or other joint pain before. Based on this diagnosis, treatment with the non-steroidal anti-inflammatory drug loxoprofen (180 mg per day) was started, and her fever and neck, wrist, and knee pain dramatically improved. Inflammatory markers on laboratory tests showed a marked improvement after administration of loxoprofen. She was discharged on the 14th day after admission.
CDS is a clinico-radiographic entity characterized by an acute onset of neck pain, fever, nuchal rigidity, jolt accentuation of headaches, general signs of inflammation, and a periodontoid calcification on cervical CT images[2]. In the present case, despite the removal of the bile duct stones, the patient presented with persisting fever, neck pain, a significant restriction of neck rotation and elevation of serum inflammatory markers. Crystal deposits on CT are mainly composed of calcium pyrophosphate dehydrate crystals. Because of its rarity and lack of awareness, CDS is sometimes misdiagnosed as meningitis, spondylitis, bone metastasis, or polymyalgia rheumatica[3]. As CDS is recognized to be a subtype of pseudogout, plain radiographs of other joints, such as the knees and wrists, even though there are no specific symptoms, might be helpful in detecting calcification in the articular cartilage. Laboratory tests are helpful to diagnose CDS, as elevation of CRP and the erythrocyte sedimentation rate caused by an inflammatory reaction is common.
The pathogenesis of CDS involves the phagocytosis of crystals by inflammatory cells, which initiates a sequence of inflammatory responses in articular joints[4]. However, what triggers inflammation is still unclear. The development of CDS after the onset of myocardial or cerebral ischemia has been reported[5], which indicates that severe illnesses may trigger an inflammatory response. No previous reports have indicated that ERCP may be a trigger for CDS. We hypothesize that there are two causative factors for the onset of CDS: systemic inflammation caused by cholangitis or head rotation with the patient in the prone position during ERCP. These factors could trigger CDS in elderly adults with periodontoid calcification, inducing a local inflammatory response in joint spaces.
We have seen three similar cases of CDS that developed after an ERCP procedure. The precise clinical manifestations of three CDS cases are showed on Table 1. All patients were febrile and over 80 years old with acute cholangitis. Interestingly, the onset of CDS after ERCP and total procedure time of ERCP differed in each case. We need to accumulate more cases whether these factors are associated with the onset of CDS.
| No. | Age | Sex | Day | Fever | Site | Time(min) | WBC(μL) | CRP(mg/dL) | Treatment |
| 1 | 82 | Male | day 16 | 39.2 °C | Neck | 65 | 4800 | 0.10 | NSAIDs |
| 2 | 85 | Female | day 1 | 38.6 °C | Neck, Ankle | 30 | 11500 | 4.93 | NSAIDs |
| 3 | 83 | Male | day 3 | 38.0 °C | Neck | 22 | 7800 | 2.12 | NSAIDs |
According to our patients diagnosed with CDS, all of them have never experienced nuchal pain nor diagnosed with pseudogout. Whether long session of ERCP with restricted head movement attributes to the onset of CDS is still unknown. In order to warn for endoscopist about the possibility of CDS, endoscopist should be cautious for the patient’s position during ERCP if they have frequent episode of neck pain or have history of cervical spondylitis before.
In summary, CDS should be considered in the differential diagnosis when elderly patients are placed in the prone position with the head rotated during an ERCP and subsequently complain of neck pain and fever after.
A 87-year-old female presented with fever and neck pain, who was diagnosed with Crowned dens syndrome (CDS) after an endoscopic retrograde cholangiopancreatography (ERCP) that was detected with a careful physical examination and radiographic findings.
The neck computed tomography (CT) scan performed after the onset of fever and neck pain revealed a sharply defined periodontoid calcification, which was compatible with neck pseudogout, namely CDS.
The authors performed complete physical examination (PE) when she complained of fever and neck pain. Based on PE, the differential diagnosis was meningitis, retropharyngeal abscess, infective spondylitis, polymyalgia rheumatica, Lemierre’s syndrome and CDS.
Inflammatory marker including white blood cells and C-reactive protein was gradually elevated, though hepato-biliary enzyme is decreasing after ERCP.
Head to neck CT was a key diagnostic tool to make a definitive diagnosis. Neck CT revealed a sharply periodontoid calcification.
NSAID with Loxoprofen 180 mg per day was extremely effective to relieve her symptoms, namely fever and neck pain.
CDS is characterized by neck pain and fever, CT findings of periodontoid calcification, and a clinical entity of pseudogout which is largely affected by the large joints such as knees and wrists.
Clinicians need to know that CDS is not rare disease entity, but is easily to be missed when not in clinician’s mind. If elderly patients, who are under an endoscopic procedure with head rotating, are complaining of fever and neck pain, CDS is one of the differential diagnosis. Focusing on patient’s physical examination on knees and wrists whether there are inflammatory findings is extremely important. If you suspect this disease, cervical CT scan or affected joint X-ray will help you to make a definitive diagnosis.
Arthrocentesis is a diagnostic intervention of pseudogout. The authors regard patient’s clinical symptoms based on history, physical examination and radiographic findings as pseudogout. Another important differential diagnosis of joint pain, especially presenting with mono-arthralgia, is a septic arthritis. If you judge patient’s complaint as not-typical symptoms, arthrocentesis is needed to be performed in order to differentiate septic arthritis or pseudogout.
| 1. | Miura F, Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yoshida M, Mayumi T. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Bouvet JP, le Parc JM, Michalski B, Benlahrache C, Auquier L. Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthritis Rheum. 1985;28:1417-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 122] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Aouba A, Vuillemin-Bodaghi V, Mutschler C, De Bandt M. Crowned dens syndrome misdiagnosed as polymyalgia rheumatica, giant cell arteritis, meningitis or spondylitis: an analysis of eight cases. Rheumatology (Oxford). 2004;43:1508-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 95] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Constantin A, Marin F, Bon E, Fedele M, Lagarrigue B, Bouteiller G. Calcification of the transverse ligament of the atlas in chondrocalcinosis: computed tomography study. Ann Rheum Dis. 1996;55:137-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Takakuni M, Nakamura M, Suenaga T. Pseudogout as a complication of stroke. Clin Neurol. 2008;48:563-567. |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Lai KH, Kayaalp C, Tantau A, Yan SL S- Editor: Qi Y L- Editor: A E- Editor: Wang CH