Published online Oct 14, 2016. doi: 10.3748/wjg.v22.i38.8605
Peer-review started: June 28, 2016
First decision: July 29, 2016
Revised: August 26, 2016
Accepted: September 12, 2016
Article in press: September 12, 2016
Published online: October 14, 2016
Processing time: 106 Days and 22.8 Hours
To determine whether contrast-enhanced ultrasonography (CEUS) as the first-line method is more cost-effective in evaluating incidentally discovered focal liver lesions (FLLs) than is computed tomography (CT) and magnetic resonance imaging (MRI).
Between 2010 and 2015, our prospective study enrolled 459 patients with incidentally found FLLs. The biological nature of FLLs was assessed by CEUS in all patients. CT or MRI examinations were added in unclear cases. The sensitivity and specificity of CEUS were calculated. The total costs of CEUS examinations and of the added examinations performed in inconclusive cases were calculated. Afterwards, the theoretical expenses for evaluating incidentally discovered FLLs using CT or MRI as the first-line method were calculated. The results were compared.
The total cost of the diagnostic process using CEUS for all enrolled patients with FLLs was 75884 USD. When the expenses for additional CT and MRI examinations performed in inconclusive cases were added, the total cost was 90540 US dollar (USD). If all patients had been examined by CT or MR as the first-line method, the costs would have been 78897 USD or 384235 USD, respectively. The difference between the cost of CT and CEUS was 3013 USD (4%) and that between MRI and CEUS was 308352 USD (406.3%). We correctly described 97.06% of benign or malignant lesions, with 96.99% sensitivity and 97.09% specificity. Positive predictive value was 94.16% and negative predictive value was 98.52%. In cases with 4 and more lesions, malignancy is significantly more frequent and inconclusive findings significantly less frequent (P < 0.001).
While the costs of CEUS and CT in evaluating FLLs are comparable, CEUS examination is far more cost-effective in comparison to MRI.
Core tip: Diagnosing focal liver lesions (FLLs) is a part of everyday practice, and therefore the cost-effectiveness of their diagnosis is important. Our study compared the costs of contrast-enhanced ultrasonography (CEUS), computed tomography (CT) and magnetic resonance imaging (MRI) in assessing the biological nature of FLL. We have proven significant savings when using CEUS instead of MRI. The costs of CEUS and CT examinations can be considered comparable. There exist additional parameters which influence the efficacy of individual modalities.
- Citation: Smajerova M, Petrasova H, Little J, Ovesna P, Andrasina T, Valek V, Nemcova E, Miklosova B. Contrast-enhanced ultrasonography in the evaluation of incidental focal liver lesions: A cost-effectiveness analysis. World J Gastroenterol 2016; 22(38): 8605-8614
- URL: https://www.wjgnet.com/1007-9327/full/v22/i38/8605.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i38.8605
Incidental discovery of focal liver lesions (FLLs) occurs very commonly in everyday practice. Although the majority of these lesions are benign[1], non-contrast ultrasound cannot be counted upon reliably to distinguish between benign and malignant lesions. Therefore, the new ACG clinical guideline: the diagnosis and management of focal liver lesions[2] has been published and recommends further investigation of these lesions using CT or MRI. Contrast-enhanced ultrasound (CEUS) constitutes an alternative option for further evaluating FLLs. European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) published guidelines and recommendations for application of CEUS in 2004[3]. These guidelines were revised in cooperation with the World Federation of Societies for Ultrasound in Medicine and Biology (WFUMB)[4,5] in 2008 and 2012.
CEUS is an ultrasound technique whereby a special intravenous contrast agent is administered. There are several registered products on the market worldwide: Definity (Lantheus Medical Imaging), Lumason (Bracco Diagnostics), Optison (GE Healthcare), SonoVue® (Bracco Diagnostics), and Sonazoid (GE Healthcare)[6]. SonoVue®) is the only product currently registered in the Czech Republic. This contrast agent is based on gas microbubbles of size 1-10 μm, stabilized by a phospholipid shell[7]. It is a strictly intravenous contrast agent enabling detailed evaluation of tissue perfusion in real time.
CEUS is not a time-consuming method and, unlike CT or MRI examinations, it can be performed in one session along with non-contrast ultrasound immediately upon finding a lesion. It benefits patients inasmuch as they are, in most cases, immediately informed of their diagnoses and are spared the stress of waiting for another examination. It is advantageous for the doctors, as well, because they can respond more flexibly and quickly to their findings. Considering how common liver lesions are, the cost of their diagnosis is also important.
The aim of this study was to assess the economic aspect and efficacy of CEUS in evaluating the biological nature of incidentally found FLLs in comparison with other standard modalities, namely CT or MRI.
Between January 2010 and December 2015, CEUS of the liver was performed 3638 times in our department. Patients enrolled in the study were diagnosed with one or more FLLs incidentally discovered: (1) by abdominal ultrasound performed for another reason (abdominal pain, diarrhoea, vomitus, dyspepsia, anaemia, etc.); (2) during a staging ultrasound for a newly diagnosed malignancy; or (3) during a follow-up ultrasound in patients with an oncological disease (colorectal cancer, breast cancer, renal carcinoma, etc.).
Exclusion criteria were (1) FLL previously known and being followed up for some time; (2) solitary lesions ≤ 1 cm with typical appearance of haemangioma or cyst in patients without a history of malignancy (no follow-up is needed according to the guidelines)[2]; (3) lesions found by another diagnostic imaging modality (CT, MRI) with an inconclusive result; (4) untargeted CEUS performed for the purpose of finding malignant lesions in the liver changed by cirrhosis or with heterogeneous appearance; (5) assessment of response to treatment of malignant FLL (i.e., after radiofrequency ablation); and (6) CEUS results not confirmed by other diagnostic imaging modality or by ultrasound scan in 6 mo time or later.
The majority of health care payments in the Czech Republic are made by health care insurers, which are private or state-owned companies. The insurers are regulated by Act No. 48/1997 Coll. (known as the Public Health Care Insurance Act)[8]. There is a specific point value (issued annually as a Regulation of the Ministry of Health)[9-15] for every medical examination or treatment. The same regulation also announces the Czech crown (CZK) value of a point for the next year. In addition to the system of state regulation, every provider of health care (such as hospitals and general practitioners, among others) may negotiate slightly different conditions with all health insurers.
It is important also to note that some medical examinations are provided only by specialized departments. In our study, we disregarded possible differences which could ensue from negotiations with the various health care insurers and thus used the standard prices as issued by the Ministry of Health.
The presented costs are final (covering the costs of work by medical staff and consumption of material), and the providers of health care receive no other payments from either insurers or patients. The final prices of the examinations for each year are presented in Table 1.
| Modality | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Average |
| Non-contrast ultrasound | 31.89 | 37.98 | 37.98 | 38.09 | 38.31 | 38.42 | 37.11 |
| Contrast-enhanced US | 165.02 | 171.82 | 164.19 | 164.3 | 164.51 | 164.61 | 165.74 |
| CT | 139.14 | 142.99 | 132.52 | 133.12 | 133.22 | 130.62 | 135.27 |
| MRI | 856.79 | 850.51 | 825.08 | 793.17 | 763.98 | 778.23 | 811.29 |
Upon discovering an FLL, a non-contrast ultrasound scan was made to assess its presence, number, size, and appearance in B mode. The cost of this examination also is a part of that for an FLL diagnosis. When calculating the total cost of CT and MRI strategies, the price of the non-contrast ultrasound scan also was included.
The price of a non-contrast abdominal ultrasound scan varied from 31.89 to 38.42 USD, depending on the year such examination was performed.
When an FLL was incidentally discovered by non-contrast ultrasound scan during office hours, CEUS was subsequently performed by the same radiologist. That radiologist would not have been specialized in liver imaging. The radiologists performing the US and CEUS were either certified radiologists (5-15 years of experience), or residents (9 mo to 5 years of practice) under the supervision of a certified radiologist present at the US department. Consultation with another radiologist present at the US department was possible and common. A senior radiologist (9-14 years of experience) specialized in liver imaging was available for consultation in unclear cases.
The ultrasound machines used were Ultrasound System iU22 Vision (Philips, the Netherlands) and Ultrasound System EPIQ 7 (Philips, the Netherlands). When an FLL was found incidentally during a non-contrast ultrasound scan, an intravenous application of 1.5-4.8 mL (median 2.5 mL) of the contrast agent SonoVue® (Bracco, Italy) followed. The contrast-enhanced examination was performed in side by side mode (B mode and contrast mode in one picture) and lasted at least 3 min. Lesions were assessed and classified in accordance with the literature[5].
The cost of CEUS ranged between 164.19 USD and 171.82 USD, depending upon the year. The price of the non-contrast ultrasound examination and of the contrast agent was already included into those figures.
CT examination was performed on a Brilliance 64 scanner (Philips, the Netherlands). Non-contrast scans were followed by contrast-enhanced CT according to a specific protocol for liver lesion evaluation which calls for administering 100-125 mL (median 125 mL) of an intravenous contrast agent in proportion to the patient’s body weight. In our hospital, Iomeron 350 (Bracco, Germany) is mostly used.
The cost of CT was 130.62-142.99 USD, depending upon the year, including the cost of the contrast agent.
MRI of the liver was performed in supine position on an Achieva 1.5T MR system (Philips, the Netherlands) and using a SENSE SL Torso coil. Non-contrast images were first obtained and there followed intravenous application of the contrast agent Primovist 0.25 mmol/mL (Bayer, Germany). The amount of contrast medium applied depended on the weight of the patient and was in the range 15-20 mL (median 15 mL; once opened the ampoule cannot be reused).
The price of MRI consists of the sum of the component procedures: basic sequences for liver evaluation, diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ACD) maps, contrast-enhanced MRI. The price for 2 × 10 mL of Primovist is then added. The total cost of an MRI examination was in the range 763.98-856.79 USD, varying by year.
In accordance with the literature[5], the number, size, and biological nature (malignant, benign, indeterminate) of each FLL were evaluated with CEUS. When possible, benign lesions were subclassified as haemangioma, focal nodular hyperplasia, pseudolesion, focal steatosis, cyst, abscess, or haematoma). A χ2 test was used to evaluate the relationship between the number and biological nature of the lesions.
The sensitivity and specificity of CEUS for our department were calculated.
The total cost of CEUS examinations of all patients was calculated. We then worked out what the expenses would have been if the biological nature of the FLL had been assessed by CT or MRI as the first-line method in all patients. The price of the non-contrast ultrasound scan was added. The expenses were subsequently compared to establish theoretical savings or losses.
It is especially important for managing the patient to establish the biological nature of a lesion, meaning to determine if it is malignant or benign. Neither CEUS nor CT nor MRI is always reliable in defining the final diagnosis. Those cases in which the findings of CEUS were not clear formed the group “inconclusive”. In these patients, further investigation was essential, either using another diagnostic imaging modality (CE-CT or CE-MRI) or with repeated ultrasonography scans. The cost of such additional examinations increased the expenses for diagnosing FLLs in cases of inconclusive CEUS findings. When CEUS results were conclusive, the expenses corresponded to the price of CEUS.
Given the sensitivity and specificity of CEUS in our study and considering data already published from other studies[16-20], we regarded the reliability of CEUS, CT, and MRI to be comparable. Therefore, the cost-minimization analysis was conducted.
In calculating the cost-effectiveness of CEUS, we counted the expenses for groups of patients in individual years and then the total sum for the period as a whole. We based our calculations on the prices of examinations mentioned above.
We established the costs for individual years and then for the period as a whole. All expenses are stated in USD, although all were paid in CZK. The average exchange rate for the period from 1 January 2010 through 31 December 2015 was used in the cost calculations, meaning 1 USD = 20.21 CZK[21].
The statistical methods of this study were reviewed by Petra Ovesna from the Institute of Biostatistics and Analyses, Masaryk University, Brno, Czech Republic.
The study included 459 patients, 212 (46.2%) of which were men and 247 (53.8%) of which were women. Ages ranged from 21 to 93 years (mean 63.4 years). Together, they accounted for 1335 FLLs discovered incidentally by non-contrast ultrasound. Benign lesions were discovered in 271 (59.1%) patients and malignant lesions in 137 patients (29.8%). In 51 (11.1%) patients (Figure 1), the CEUS result was inconclusive. All lesions were further evaluated with another diagnostic imaging modality or followed up with ultrasound. The findings during individual years are given in Table 2.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Total | |
| Total sum | 38 | 53 | 73 | 85 | 124 | 86 | 459 |
| Benign | 16 | 27 | 45 | 50 | 72 | 61 | 271 |
| Malignant | 15 | 21 | 19 | 27 | 39 | 16 | 137 |
| Inconclusive | 7 | 5 | 9 | 8 | 13 | 9 | 51 |
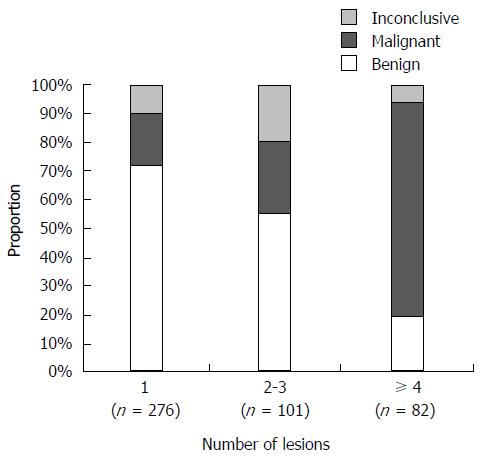
One lesion was found in 276 (60.1%) patients, 2 to 3 lesions in 101 (22%) patients, and 4 or more lesions in 82 (17.9%) patients.
As illustrated in Figure 2, it is clear from our results that in cases with 4 and more lesions malignancy is significantly more frequently seen and the proportion of inconclusive findings is significantly less (P < 0.001).
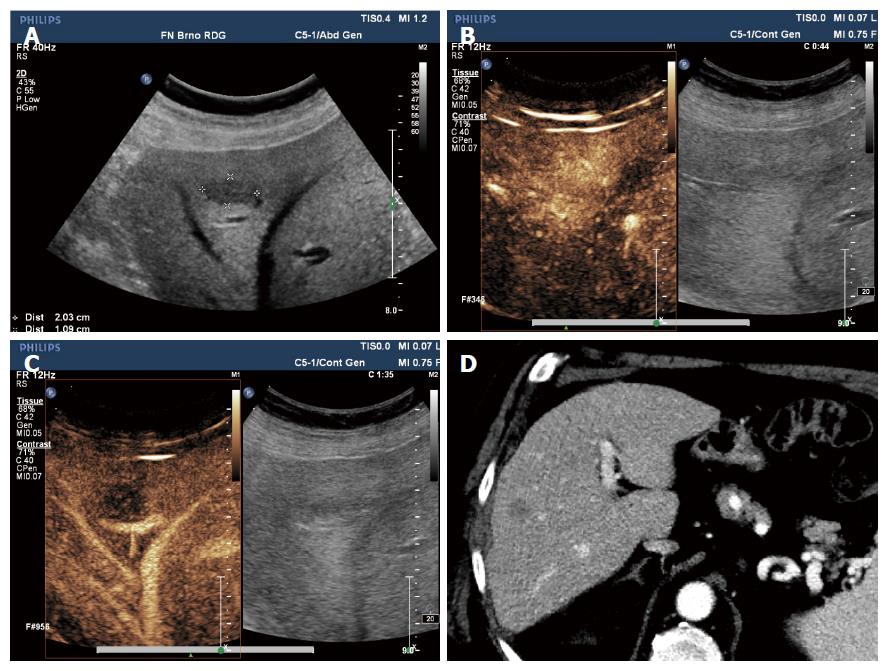
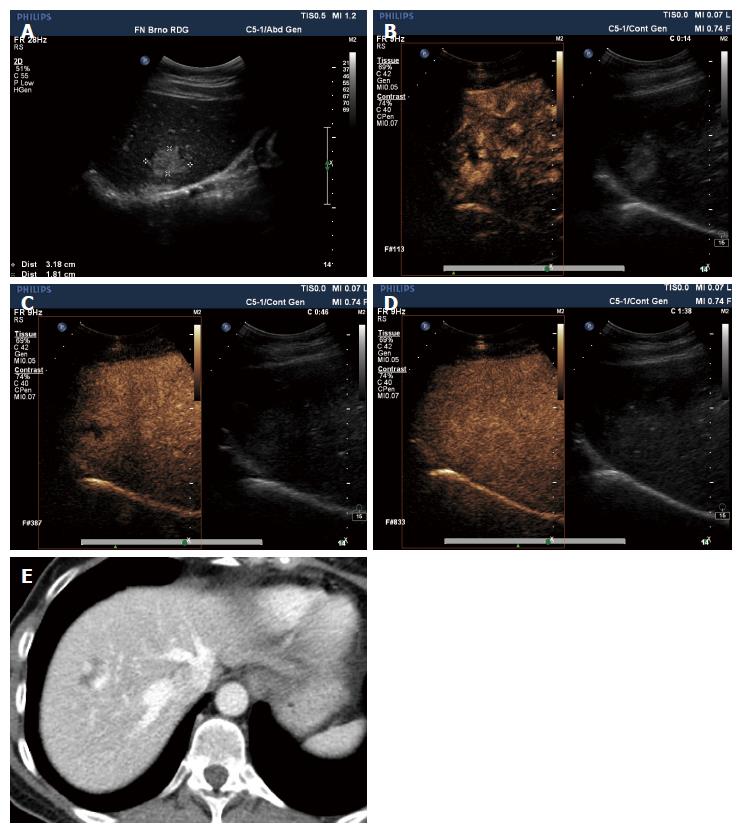
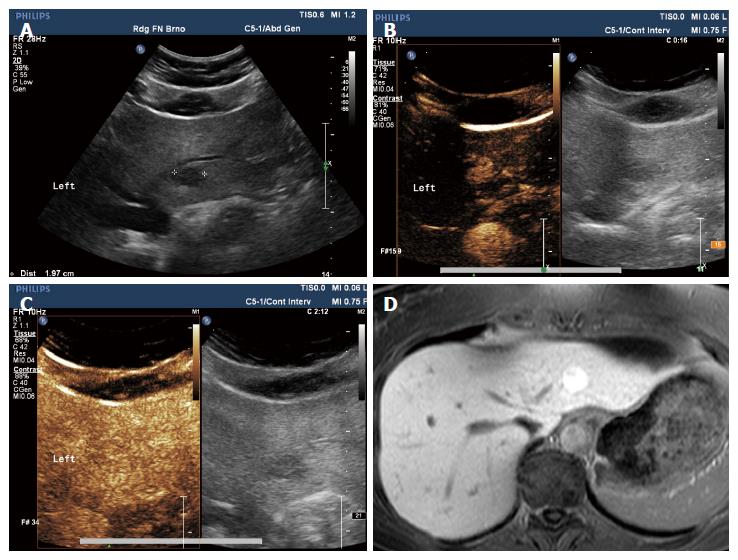
Of benign lesions, there were 136 (58.2%) haemangiomas (Figure 3), 23 (7.7%) focal nodular hyperplasia (Figure 4), 58 (24%) pseudolesions, 16 (3.1%) focal steatoses, 16 (4.01%) cysts, 6 (0.5%) liquid collections, and 5 other findings (haematoma, postoperative changes, dysplastic nodule in cirrhotic liver). In 26 (6.6%) patients, the lesions were not further subclassified but the nature of those lesions was described as benign. In 13 patients, two types of lesions occurred.
To be able to calculate the specificity and sensitivity of CEUS in our study, the findings had to be verified by another diagnostic imaging modality which is considered a gold standard or to be unchanged over an extended period of time. Lesions were subsequently evaluated by CT or MRI (either performed as a follow-up examination or as an assessment of a response to treatment) or they were observed by ultrasound for longer than 6 mo or verified by histology.
We described 97.06% of benign or malignant lesions correctly with 96.99% sensitivity and 97.09% specificity. Positive predictive value was 94.16% and negative predictive value was 98.52%.
The cost of CEUS for the 459 enrolled patients with incidentally found FLLs was 75884 USD, thus averaging 165.3 USD per patient.
In 51 patients with inconclusive CEUS findings, the costs were increased by additional CT or MRI examination or ultrasonography follow-up (CT was performed in 33 patients, MRI in 10 patients, and ultrasound follow-up in 8 patients; Table 3). The total cost of additional examinations was 14657 USD.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Total | |
| Total | 38 | 53 | 73 | 85 | 124 | 86 | 459 |
| Methods used for examining inconclusive findings | |||||||
| Ultrasound follow-up | 1 | 3 | 1 | 2 | 1 | 8 | |
| CT | 4 | 4 | 6 | 6 | 9 | 4 | 33 |
| MRI | 3 | 1 | 2 | 4 | 10 |
The total cost of diagnosing FLLs while pursuing a CEUS strategy was therefore 90540 USD, averaging 197.3 USD per patient.
Theoretically, if all FLLs incidentally found by non-contrast ultrasound scans would have been evaluated with CT, the expenses for 459 patients would have been 78897 USD for the whole period, meaning 171.9 USD per patient.
In case of using MRI after the initial non-contrast ultrasound scan, the cost for 459 patients would have been 384235 USD, meaning 837.1 USD per patient.
Inconclusive findings could be expected even when using CT or MRI, and such patients would have to be examined further (using MRI after CT, PET/CT, biopsy, CT or MRI follow-up). That would increase the total cost of these strategies. Considering that similar sensitivity and specificity are described in the literature for CEUS and CT[16-23], a similar incidence of inconclusive results could be expected. We could find no relevant data as to how many such results may occur, however, and therefore the cost of possible additional examinations could not be added.
Over the period of the study, the difference in total cost between CT and CEUS was 3013 USD (4%; i.e., 6.6 USD per patient) and between MRI and CEUS it was 308352 USD (406.3%; i.e., 471.8 USD per patient). Those also are the sums we hypothetically saved using CEUS as the method of choice instead of CT or MRI in evaluating the biological nature of incidentally found FLLs.
If the costs of further investigating inconclusive CEUS findings were included, then examination with CT would be less costly by 11643 USD (12.9%) for the period (i.e., by 25.4 USD per patient). Evaluation with MRI would be still more costly by 293695 USD (324.4%) for the period (i.e., 639.9 USD per patient). The prices for CT and MRI examinations do not include expenses for further evaluating possible inconclusive findings.
Table 4 summarizes the prices of individual examinations for the individual years and for the period as a whole.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Total | Total per patient | |
| CEUS | ||||||||
| Examination | 6271 | 9107 | 11986 | 13965 | 20399 | 14156 | 75884 | 165.3 |
| Additional examination | 3350 | 800 | 1251 | 1935 | 3302 | 4020 | 14657 | 287.4 |
| Total | 9621 | 9906 | 13237 | 15900 | 23700 | 18176 | 90540 | 197.3 |
| CT | ||||||||
| Examination | 6499 | 9591 | 12447 | 14553 | 21269 | 14537 | 78897 | 171.9 |
| MRI | ||||||||
| Examination | 33770 | 47090 | 63004 | 70657 | 99483 | 70232 | 384235 | 837.1 |
Savings and losses for individual diagnostic strategies are summarized in Table 5.
| Difference in USD | Difference per patient in USD | Difference (%) | |
| CT | |||
| CEUS vs CT | -3013 | -6.6 | -4.0 |
| CEUS + additional vs CT | 11643 | 25.4 | 12.9 |
| MRI | |||
| CEUS vs MRI | -308352 | -671.8 | -406.3 |
| CEUS + additional vs MRI | -293695 | -639.9 | -324.4 |
The nature of all lesions of the patients enrolled in the study was evaluated by CEUS and subsequently verified. The nature of 97.06% of lesions was correctly determined by CEUS, with sensitivity 96.99% and specificity 97.09%.
Our results were comparable to those from other studies in other countries which pursued this topic[22-26]. The high sensitivity and specificity in our group may be attributed to the option to consult a specialized senior radiologist and to quantify the perfusion.
By comparison, a large German multicentre study (the DEGUM study)[22] evaluated 1349 patients with liver lesions. Malignant and benign lesions were correctly differentiated in 95.7% of patients with sensitivity 95.8% and specificity 83.1%.
In a French multicentre study[23], 874 patients with 1034 FLLs were examined and CEUS results were compared to gold standard methods (CE-CT, CE-MR, or liver biopsy). In this case, 73% of benign and malignant FLLs were correctly evaluated, with sensitivity 79% and specificity 88%.
Finally, another German study[24] observed 317 patients, 89% of which were correctly diagnosed by CEUS, with sensitivity 90% and specificity 99%.
A number of other studies also address specificity and sensitivity of CEUS[27-30]. With regard to cost effectiveness, several published studies have reported significant savings when using CEUS[31-34].
An Italian multicentre prospective study[31] evaluated 485 patients with 575 lesions. Two diagnostic algorithms were compared: a standard approach (after finding a liver lesion with non-contrast ultrasound, CT or MR follows) at a total cost of 134576 EUR for diagnosing the nature of lesions and a new strategy (non-contrast ultrasound immediately followed by CEUS) at a cost of 55674 EUR. Using CEUS resulted in savings of 78902 EUR (i.e., 162 EUR per patient).
A German study[32] also compared the economic aspect of using CEUS and CT in evaluating incidentally found FLLs. It concluded that CEUS was the more cost-effective method for all scenarios in which CEUS examinations were performed at specialized centres. The price for CEUS ranged between 122.18 and 184.53 EUR, and the price for multi-phase CT was 223.19 EUR. With approximately 40000 incidentally found FLLs in Germany per year, systematic implementation of CEUS would result in savings of around 4 million EUR/year. The cost of CEUS examination would be significantly higher, however, if performed also at non-specialized centres, where the price for one CEUS examination could average 407.87 EUR[32].
The data from a French multicentre study[33] assessed the costs of evaluating 149 liver lesions. The final savings were 128.5 EUR per lesion when using CEUS.
Finally, another Italian study[34] evaluated 398 patients with benign FLLs between 2002 and 2005. The cost of one CEUS examination was 101.51 EUR and that of CT was 211.48 EUR. The final cost saving was 47055 EUR when using CEUS as the first-line diagnostic imaging modality after non-contrast ultrasound.
In our prospective study, the difference between the total costs of CEUS and CT, at just 3013 USD (i.e., + 4%) for the entire period, was relatively small compared to those from studies published previously. Adding in the cost for further investigation of inconclusive CEUS findings would bring that difference to 11643 USD (i.e., +12.9%).
The high price of the contrast agent for CEUS in the Czech Republic increases the overall cost of a CEUS examination (average 165.74 USD) compared to the price of CT (average 135.27 USD) and contributes to the relatively small savings in comparison with other studies.
The difference between the cost of CEUS and MRI was significant even in our study, at 308352 USD (i.e. 406.3%). Adding in the cost for further investigation of inconclusive CEUS findings, that difference would have been 293695 USD (i.e., +324.4%).
The hypothetical cost of diagnosing FLLs with CT and MRI does not include the expenses for further evaluation of inconclusive findings, which would certainly arise. Such patients would have to be followed up or examined using another diagnostic modality (MRI, PET/CT, biopsy or surgery, including the costs of hospitalization and possible complications). Accordingly, the total cost of these diagnostic scenarios would have increased and the cost-effectiveness of CEUS would have been even more pronounced. Unfortunately, we could find no published data which would indicate numbers of inconclusive CT and MRI findings in evaluating FLLs. Therefore, we could not include the hypothetical cost of possible additional examinations.
A disadvantage of CT is its necessity for intravenous application of iodinated contrast agent with accompanying risks of its having side effects and causing complications (allergic reaction, anaphylactic shock, etc.). The cost of treating such complications was also not included in the total expenses. These complications are rare, however, and the cost of their treatment would probably not significantly alter the result of this study. In cases of using MRI and CEUS examinations, as we did, these reactions are even rarer.
Additionally, patients with known or suspected allergy to iodinated contrast agent would have to be examined by MRI, which is more expensive. We did not take this into account, but it would certainly further raise the total cost of diagnosis while pursuing a CT strategy.
In the Czech Republic, MRI is still an expensive examination and one that for many patients is poorly accessible due to a small number of available devices and their high workload. Therefore, CEUS is more advantageous not only in terms of cost-efficiency but also of accessibility and usage. Another significant impact of these disadvantages is that CT is used as the second-line examination method after inconclusive CEUS findings rather than MRI.
Important advantages of CEUS are the absence of ionizing radiation, good accessibility, short duration, and its possibility to be conducted immediately after the non-contrast ultrasound scan. Thus, the patient is examined in a single session and need not wait weeks for another examination and diagnosis.
Unfortunately, although health insurance covers CEUS examinations performed in our specialized centre, this is not the case for district hospitals in the Czech Republic.
In conclusion, the expenses for diagnosing FLLs with CEUS are comparable to those of CT. Important advantages of CEUS are the absence of radiation and the speed of diagnosis while maintaining diagnostic accuracy. Moreover, CEUS is significantly more cost-effective in comparison with MRI.
Incidental focal liver lesions are very common in daily practice at US departments. For the further management of a patient it is important to distinguish whether a lesion is benign or malignant. Computed tomography (CT) and magnetic resonance imaging (MRI) and contrast-enhanced ultrasonography (CEUS) are standard methods used for the investigation. Each has its advantages and disadvantages in terms of radiation exposure, availability, side effects, accuracy, price and others. How best to manage these diagnoses and their costs is much discussed today. Therefore, cost-effectiveness analysis of these methods is very pertinent.
Numbers of focal liver lesions and their further investigation have a great financial impact on hospitals. Therefore, this study presents and compares costs of three strategies for evaluating the biological nature of incidentally found focal liver lesions.
This study shows that CEUS, as a first-line method, is significantly more cost-effective in comparison with MRI. Compared to other cost-effectiveness studies, this analysis is directed mainly to the comparative costs of CEUS and CT strategies because of the high price of CEUS contrast agent against the relatively low price of CT examination in the Czech Republic.
This study will enable knowledge regarding economic aspects of investigating focal liver lesions to be used in practice. It shows the advantages of using CEUS as a first-line method.
CEUS: A sonographic method with use of contrast agents containing microbubbles of gas that allow evaluating perfusion of organs and lesions. Cost-effectiveness analysis: A form of economic analysis that compares the relative costs and outcomes (effects) of two or more courses of action.
The authors have performed a very good study. The manuscript is interesting.
| 1. | Little JM, Richardson A, Tait N. Hepatic dystychoma: a five year experience. HPB Surg. 1991;4:291-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Marrero JA, Ahn J, Rajender Reddy K. ACG clinical guideline: the diagnosis and management of focal liver lesions. Am J Gastroenterol. 2014;109:1328-1347; quiz 1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 301] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 3. | Albrecht T, Blomley M, Bolondi L, Claudon M, Correas JM, Cosgrove D, Greiner L, Jäger K, Jong ND, Leen E. Guidelines for the use of contrast agents in ultrasound. January 2004. Ultraschall Med. 2004;25:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 249] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 4. | Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D’Onofrio M. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008;29:28-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 503] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 5. | Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver - update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol. 2013;39:187-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 506] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 6. | International Contrast Ultrasound Society. What is CEUS? Available from: http://www.icus-society.org/about-ceus/what-is-ceus. |
| 7. | Greis C. Technology overview: SonoVue (Bracco, Milan). Eur Radiol. 2004;14 Suppl 8:P11-P15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Public Health Care Insurance Act No. 48/1997 Coll. Available from: http://www.mzcr.cz. |
| 9. | Regulation issued by the Ministry of Health No. 134/1998 Coll. that declares list of medical examinations with point values. Available from: http://www.mzcr.cz/. |
| 10. | Regulation issued by the Ministry of Health No. 471/2009 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits to volume of health care services provided and paid from public health care insurance for year. 2010; Available from: http://www.mzcr.cz/. |
| 11. | Regulation issued by the Ministry of Health No. 396/2010 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits to volume of health care services provided and paid from public health care insurance for year. 2011; Available from: http://www.mzcr.cz/. |
| 12. | Regulation issued by the Ministry of Health No. 425/2011 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits to volume of health care services provided and paid from public health care insurance for year. 2012; Available from: http://www.mzcr.cz/. |
| 13. | Regulation issued by the Ministry of Health No. 475/2012 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits for year. 2013; Available from: http://www.mzcr.cz/. |
| 14. | Regulation issued by the Ministry of Health No. 428/2013 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits for year. 2014; Available from: http://www.mzcr.cz/. |
| 15. | Regulation issued by the Ministry of Health No. 324/2014 Coll. defining point value and health care expenses paid by public health care insurance and regulatory limits. 2015; Available from: http://www.mzcr.cz/. |
| 16. | Halavaara J, Breuer J, Ayuso C, Balzer T, Bellin MF, Blomqvist L, Carter R, Grazioli L, Hammerstingl R, Huppertz A. Liver tumor characterization: comparison between liver-specific gadoxetic acid disodium-enhanced MRI and biphasic CT--a multicenter trial. J Comput Assist Tomogr. 2006;30:345-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 140] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Sporea I, Şirli R. Is Contrast Enhanced Ultrasound (CEUS) ready for use in daily practice for evaluation of focal liver lesions? Med Ultrason. 2014;16:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Seitz K, Strobel D, Bernatik T, Blank W, Friedrich-Rust M, Herbay Av, Dietrich CF, Strunk H, Kratzer W, Schuler A. Contrast-Enhanced Ultrasound (CEUS) for the characterization of focal liver lesions - prospective comparison in clinical practice: CEUS vs. CT (DEGUM multicenter trial). Parts of this manuscript were presented at the Ultrasound Dreiländertreffen 2008, Davos. Ultraschall Med. 2009;30:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (2)] |
| 19. | Seitz K, Bernatik T, Strobel D, Blank W, Friedrich-Rust M, Strunk H, Greis C, Kratzer W, Schuler A. Contrast-enhanced ultrasound (CEUS) for the characterization of focal liver lesions in clinical practice (DEGUM Multicenter Trial): CEUS vs. MRI--a prospective comparison in 269 patients. Ultraschall Med. 2010;31:492-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Wernecke K, Rummeny E, Bongartz G, Vassallo P, Kivelitz D, Wiesmann W, Peters PE, Reers B, Reiser M, Pircher W. Detection of hepatic masses in patients with carcinoma: comparative sensitivities of sonography, CT, and MR imaging. AJR Am J Roentgenol. 1991;157:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 160] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Czech National Bank. Exchange rates USD/CZK. Available from: http://www.kurzy.cz/kurzy-men/kurzy.asp?A=H&KM= USD&D1=01.01.2010&D2=31.12.2015&I=1. |
| 22. | Strobel D, Seitz K, Blank W, Schuler A, Dietrich C, von Herbay A, Friedrich-Rust M, Kunze G, Becker D, Will U. Contrast-enhanced ultrasound for the characterization of focal liver lesions--diagnostic accuracy in clinical practice (DEGUM multicenter trial). Ultraschall Med. 2008;29:499-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 179] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 23. | Tranquart F, Fayault A, Le Gouge A, Giraudeau B, Correas JM, Ladam Marcus V, Manzoni P, Vilgrain V, Aube C, Bellin MF. Role of contrast-enhanced ultrasound in the blinded assessment of focal liver lesions in comparison with MDCT and CEMRI: Results from a multicentre clinical trial. EJC Suppl. 2008;6:9-15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Trillaud H, Bruel JM, Valette PJ, Vilgrain V, Schmutz G, Oyen R, Jakubowski W, Danes J, Valek V, Greis C. Characterization of focal liver lesions with SonoVue-enhanced sonography: international multicenter-study in comparison to CT and MRI. World J Gastroenterol. 2009;15:3748-3756. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 134] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (2)] |
| 25. | von Herbay A, Westendorff J, Gregor M. Contrast-enhanced ultrasound with SonoVue: differentiation between benign and malignant focal liver lesions in 317 patients. J Clin Ultrasound. 2010;38:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Celli N, Gaiani S, Piscaglia F, Zironi G, Camaggi V, Leoni S, Righini R, Bolondi L. Characterization of liver lesions by real-time contrast-enhanced ultrasonography. Eur J Gastroenterol Hepatol. 2007;19:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Nicolau Molina C, Fontanilla Echeveste T, Del Cura Rodríguez JL, Cruz Villalón F, Ripollés González T, Baudet Naveros B, Velasco Marcos MA, Garre Sánchez C, Huertas Arroyo R, Hernández García L. [Usefulness of contrast-enhanced ultrasonography in daily clinical practice: a multicenter study in Spain]. Radiologia. 2010;52:144-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Smajerova M, Petrasova H, Andrasina T, Válek V. Contrast-enhanced ultrasonography in the evaluation of incidental focal liver lesions - a cost-effective study. Ces Radiol. 2015;69:42-47. |
| 29. | Sporea I, Martie A, Bota S, Sirli R, Popescu A, Dănila M. Characterization of focal liver lesions using contrast enhanced ultrasound as a first line method: a large monocentric experience. J Gastrointestin Liver Dis. 2014;23:57-63. [PubMed] |
| 30. | Gomaa AI, Khan SA, Leen EL, Waked I, Taylor-Robinson SD. Diagnosis of hepatocellular carcinoma. World J Gastroenterol. 2009;15:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 31. | Romanini L, Passamonti M, Aiani L, Cabassa P, Raieli G, Montermini I, Martegani A, Grazioli L, Calliada F. Economic assessment of contrast-enhanced ultrasonography for evaluation of focal liver lesions: a multicentre Italian experience. Eur Radiol. 2007;17 Suppl 6:F99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 32. | Giesel FL, Delorme S, Sibbel R, Kauczor HU, Krix M. [Contrast-enhanced ultrasound for the characterization of incidental liver lesions - an economical evaluation in comparison with multi-phase computed tomography]. Ultraschall Med. 2009;30:259-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Tranquart F, Correas JM, Ladam Marcus V, Manzoni P, Vilgrain V, Aube C, Elmaleh A, Chami L, Claudon M, Cuilleron M. [Real-time contrast-enhanced ultrasound in the evaluation of focal liver lesions: diagnostic efficacy and economical issues from a French multicentric study]. J Radiol. 2009;90:109-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 34. | Faccioli N, D’Onofrio M, Comai A, Cugini C. Contrast-enhanced ultrasonography in the characterization of benign focal liver lesions: activity-based cost analysis. Radiol Med. 2007;112:810-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Czech Republic
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Chiow AKH S- Editor: Qi Y L- Editor: A E- Editor: Wang CH