Published online Sep 28, 2016. doi: 10.3748/wjg.v22.i36.8242
Peer-review started: March 12, 2016
First decision: April 14, 2016
Revised: April 20, 2016
Accepted: June 13, 2016
Article in press: June 13, 2016
Published online: September 28, 2016
Processing time: 198 Days and 16.2 Hours
The present report describes a rare case of a tumor composed of early gastric cancer and a duodenal neuroendocrine tumor (NET). A 78-year-old woman underwent esophagogastroduodenoscopy at a local institution for screening of the upper gastrointestinal tract which revealed a protruded tumor through the pyloric ring from the pyloric antrum. The tumor was too large to treat at the facility; consequently, she was referred to our hospital for further management. Esophagogastroduodenoscopy with tumor biopsy of the lesion revealed the diagnosis of early gastric cancer. Endoscopic submucosal dissection was performed with sufficient free margins in both vertical and horizontal directions. Histopathological findings showed NET confined to the submucosal layer and covered by well-differentiated adenocarcinoma. Immunohistochemical stainings showed that the two lesions existed continuously. While the possibility of a collision cancer was considered, it was suggested that the two lesions existed continuously. Finally, the tumor was diagnosed as gastric cancer composed of duodenal NET G1, with a lymphatic invasion of NET component.
Core tip: Although there are some reports of endoscopic resection performed to duodenal neuroendocrine tumor (NET), no reports have been published on the treatment of duodenal NET composed of early gastric cancer treated by endoscopic submucosal dissection (ESD). A 78-year-old woman underwent esophagogastroduodenoscopy and revealed a protruded tumor through the pyloric ring from the pyloric antrum. ESD was performed and finally the tumor was diagnosed as gastric cancer composed of duodenal NET G1, with a lymphatic invasion of NET component. We report the first case of early gastric cancer accompanied by duodenal NET, which was resected by ESD.
- Citation: Kaneko H, Miyake A, Ishii Y, Sue S, Miwa H, Sasaki T, Tamura T, Kondo M, Maeda S. Case of a tumor comprising gastric cancer and duodenal neuroendocrine tumor. World J Gastroenterol 2016; 22(36): 8242-8246
- URL: https://www.wjgnet.com/1007-9327/full/v22/i36/8242.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i36.8242
Endoscopic submucosal dissection (ESD) is widely performed for gastric cancer, and is also used for other cancers, such as esophagus, colon, rectum. The use of ESD for treatment for superficial non-ampullary duodenal epithelial tumors is also increasing[1].
Duodenal neuroendocrine tumor (NET) is a rarely encountered tumor, with fewer cases reported than those for gastric and rectal carcinoid tumors, and its natural history has not yet been well defined[2]. Although there are some reports of endoscopic resection, no reports have been published on the treatment of duodenal NET composed of early gastric cancer treated by ESD. We here report the first case of early gastric cancer accompanied by duodenal NET resected by ESD.
A 78-year-old woman presented to a local institution with nausea and right hypochondrial pain. Careful examination led to the diagnosis of gallstones and common bile duct stones. Esophagogastroduodenoscopy (EGD) screening of the upper gastrointestinal tract was performed before surgery to remove the gallstones and a protruded tumor through the pyloric ring from the pyloric antrum was found. Although biopsy specimen from the lesion was diagnosed as an adenoma, the tumor was too large to treat at the facility. The patient was referred to our hospital for further management of the gastric tumor. She had no specific medical history except hypertension and dyslipidemia.
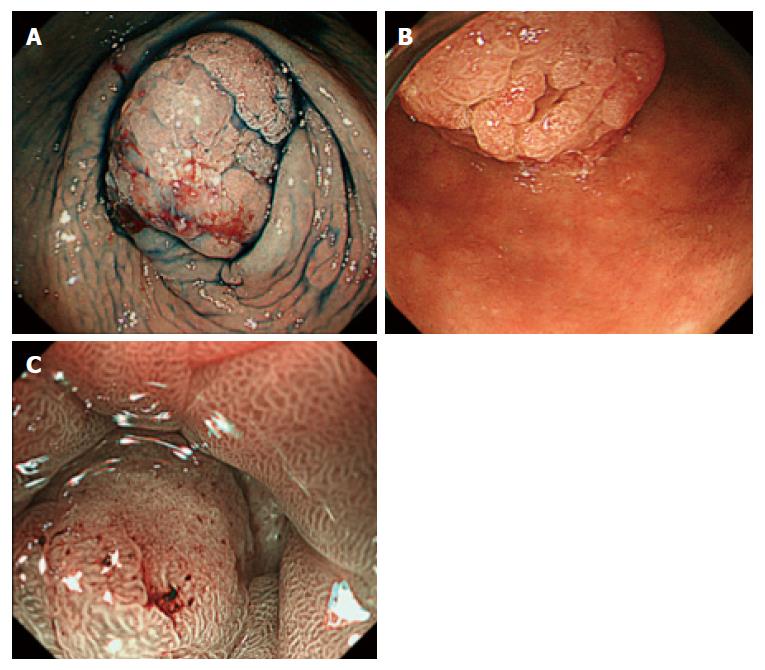
No abnormalities were found on physical examination, including vital signs, and routine laboratory analyses. Serum levels of tumor markers such as carcinoembryonic antigen and carbohydrate antigen 19-9 were 2.9 ng/mL and 9 U/mL, respectively. Computed tomography of the abdomen revealed no mass in the gastrointestinal tract and no lymph node swelling or metastasis. EGD revealed a protruded tumor with a diameter of approximately 20 mm over the bulb from the pylorus antrum (Figure 1A and B). Magnifying endoscopy with narrow-band imaging showed irregularities in the structures and vessels of the tumor, which led to the suspicion of early gastric cancer (Figure 1C). Biopsy from the gastric portion of the tumor revealed well-differentiated adenocarcinoma. We were unable to investigate the whole tumor because it occupied and existed beyond the pyloric ring; however, there were no obvious signs suggesting submucosal tumor invasion. Although the tumor extended to the duodenum, the major part of the tumor was from the stomach. Finally, the diagnosis was early gastric cancer, and ESD was recommended.
The tumor was resected in a single fashion by the ESD technique, using a GIF-Q260J instrument (Olympus, Tokyo, Japan) with a transparent hood (MAJ-1989-11302; Olympus) attached to the tip of the gastroscope, a dual knife (Olympus), and an insulated tipped knife 2 (Olympus). An electrosurgical current generator (VIO200; ERBE, Tubingen, Germany) was used for the ESD. The tumor was resected with no complications, such as perforation or delayed bleeding. As a result, the patient was discharged on postoperative day 5.
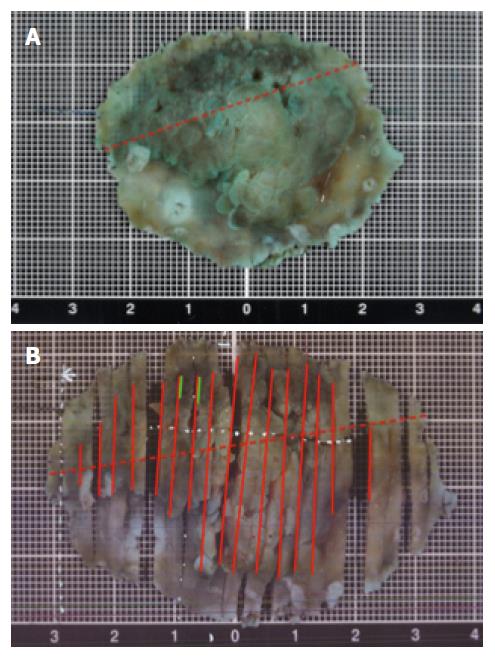
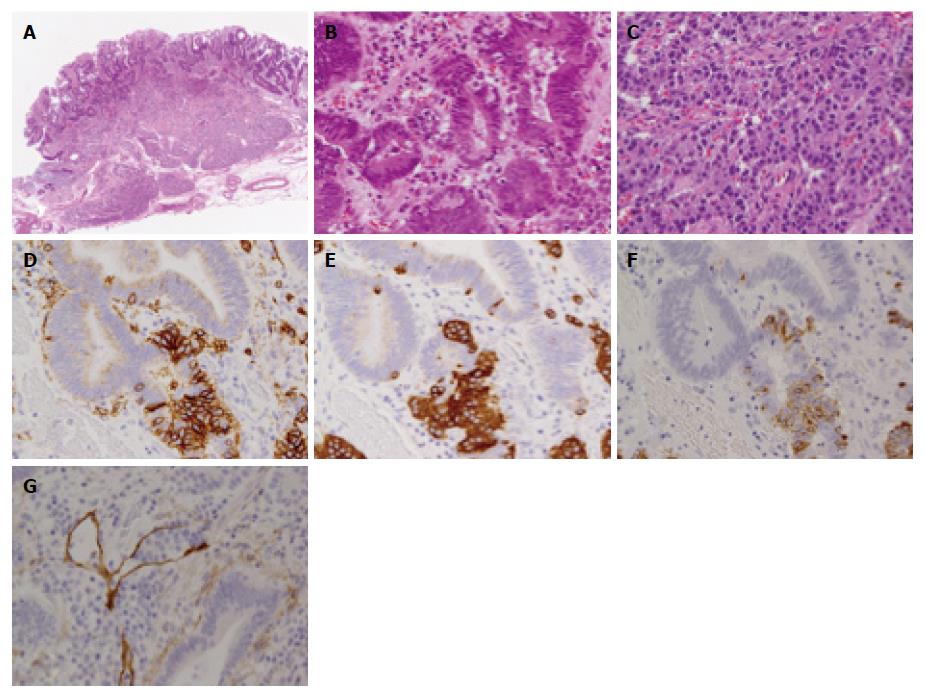
Figure 2 shows a macroscopic view of the resected specimen. The resected mucosa and the tumor measured 54 mm × 40 mm and 38 mm × 32 mm, respectively. The histopathology results showed the resected specimen had sufficient free margins in both vertical and horizontal directions, but the tumor consisted of two components: The first part with irregular atypical epithelium, which formed a tubular and papillary structure confined to the mucosal layer, was a well differentiated adenocarcinoma, and the second part was located near the edge of duodenum side of the specimen and showed a mass composed of nests of small uniform tumor cells, which is typical of NET (Figure 3A-C). These cells were positive for CD56 (Figure 3D), synaptophysin (Figure 3E), and chromogranin A (Figure 3F), and the Ki-67 labeling index was less than 1%. According to the WHO 2010 classification, obvious nuclear fission images were not admitted and finally the NET was diagnosed as G1[3]. The NET cells were detected from the mucosal layer over the submucosa, but no infiltration of the muscle layer was recognized.
The adenocarcinoma cells and the NET cells were in contact. Although migration images were not detected, both component cells had mixed in some parts and formed a tumor duct. Immunohistochemical staining also showed NET cells coexisting with adenocarcinoma cells (Figure 3E and F). No venous invasion was revealed by Elastica van Gieson staining, however, lymphatic invasion of NET component was seen with D2-40 staining (Figure 3G).
The patient was sufficiently explained about the results of the histopathological examination and the risk of lymph node metastasis; she refused additional operation and opted for careful observation. Therefore, close follow-up has been scheduled.
Since Oberndorfer proposed the term “carcinoid” in 1907, the origins of NET of the gastrointestinal tract, as well as the malignancy of these tumors, have been attracting the attention of clinicians[3]. NETs are quite rare and almost 55% of NETs occur in the gastrointestinal tract[2]. In Japan, NET occurs more frequently in the rectum and the stomach followed by the duodenum, and primary NET of the duodenum may occur in less than 5% of all cases[2,4].
Although there were some reports about gastric collision tumor composed of epithelial and nonepithelial malignant neoplasm, Morishita et al[5] reported that a simultaneous incidence of adenocarcinoma and malignant lymphoma was the most frequent finding and cases of gastric collision tumor composed of adenocarcinoma and NET were rare.
Previously, Kato et al[6] reported a case of duodenal adenocarcinoma with neuroendocrine features in a 67-year-old woman with acromegaly and thyroid papillary adenocarcinoma. Wen et al[7] reported a case of duodenal bulb adenocarcinoma with neuroendocrine features in a 63-year-old woman, which was treated by endoscopic mucosal resection. They stated that duodenal adenocarcinoma with neuroendocrine features is extremely rare[7], and as per our review of the published literature, our report is likely the first instance of the gastric adenocarcinoma with duodenal NET resected by endoscopic treatment.
In this report, after ESD, we detected a tiny mass composed of nests of small uniform tumor cells that were typical of NET. The possible reasons the diagnosis of NET was overlooked before ESD are as follows: first, the whole tumor was located over the pylorus and its relatively large size made it difficult to observe the whole tumor precisely; and second, the NET component surface was covered with adenocarcinoma, which was also a protruded lesion.
Collision tumors are thought to arise from morphologically different neighboring neoplasms that do not intermingle[8], but usually, it is not easy to morphologically distinguish a collision-type from a composite-type tumor[9]. It was difficult to determine whether the tumor was collision or composite-type in our patient as well: the immunohistochemical staining showed that the two lesions coexisted, suggesting a composite-type tumor, but the NET clinically presented in the duodenal part.
It was also difficult to distinguish histologically whether the adenocarcinoma derived from the stomach or duodenum as the ESD specimen did not include the muscle layer and it was impossible to detect the pyloric sphincter as a surgical specimen. Most of the tumor was present in the stomach and remainder gastric mucosa was atrophic, allowing the adenocarcinoma derived from the gastric epithelium to be diagnosed as not from duodenum. The NET was present in the end of the duodenal side of the specimen, and it was evident that the NET existed intraduodenally from the comparison marking dots of endoscopic findings and the analyte. We therefore judged clinically that the NET was from the duodenal epithelium (Figure 2).
Surgical treatment may have been one treatment options, but as the tumor was diagnosed as early gastric cancer which had adaptation for ESD, surgery could be excessively invasive to the patient.
By the popularization of ESD, there have been some reports on cancer accompanied by submucosal tumor or NET[5,8,9]. However, the coexistence of gastric NET and adenocarcinoma are rare, because gastric neuroendocrine tumors represent less than 1% of all gastric neoplasms[8,10]. There have been no previous reports on endoscopic resection of gastric adenocarcinoma with duodenal NET; hence, we considered this case to be extremely rare.
We report the first case of early gastric cancer accompanied by duodenal NET, which was resected by ESD.
We thank all medical staff and technicians of Yokohama City University Graduate School of Medicine.
A 78-year-old woman with medical history of hypertension and dyslipidemia presented with a protruded gastric tumor through the pyloric ring from the pyloric antrum.
Magnifying endoscopy with narrow-band imaging showed irregularities in the structures and vessels of the tumor, which the biopsy specimen led to the diagnosis of early gastric cancer.
Gastric cancer with submucosal tumor invasion or duodenum cancer.
All labs were within normal lomits.
Computed tomography showed no remarkable metastasis.
A well differentiated adenocarcinoma composed of nests of small uniform tumor cells, which is typical of neuroendocrine tumor (NET).
Endoscopic submucosal dissection.
Although there were some reports about gastric collision tumor composed of epithelial and nonepithelial malignant neoplasm, malignant lymphoma was the most frequent finding and cases of gastric collision tumor composed of adenocarcinoma, and NET were rare. Duodenal adenocarcinoma with neuroendocrine features is also extremely rare and there were no previous report on endoscopic resection of gastric adenocarcinoma with duodenal NET.
NET is derived from enterochromaffin cells throughout the gastrointestinal (GI), pancreas and bronchopulmonary systems. The most common sites for primary GI carcinoid tumors in Japan are the rectum, stomach, and duodenum.
Although we experienced an extremely rare case coincidentally, especially in the case of protruded tumor, the possibilities of collision tumor should be bear in mind.
In this paper the authors describe a duodenal neuroendocrine tumor resected by endoscopic submucosal dissection. This is a rare condition and manuscript is well written.
| 1. | Kakushima N, Kanemoto H, Tanaka M, Takizawa K, Ono H. Treatment for superficial non-ampullary duodenal epithelial tumors. World J Gastroenterol. 2014;20:12501-12508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Matsumoto S, Miyatani H, Yoshida Y, Nokubi M. Duodenal carcinoid tumors: 5 cases treated by endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1152-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Yamaguchi T, Fujimori T, Tomita S, Ichikawa K, Mitomi H, Ohno K, Shida Y, Kato H. Clinical validation of the gastrointestinal NET grading system: Ki67 index criteria of the WHO 2010 classification is appropriate to predict metastasis or recurrence. Diagn Pathol. 2013;8:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Soga J. Early-stage carcinoids of the gastrointestinal tract: an analysis of 1914 reported cases. Cancer. 2005;103:1587-1595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 222] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 5. | Morishita Y, Sugitani M, Sheikh A, Nemoto N, Fujii M, Takayama T. Collision tumor of the stomach: a rare case of an adenocarcinoma and carcinoid tumor. Arch Pathol Lab Med. 2005;129:407-409. [PubMed] |
| 6. | Kato K, Takeshita Y, Misu H, Ishikura K, Kakinoki K, Sawada-Kitamura S, Kaneko S, Takamura T. Duodenal adenocarcinoma with neuroendocrine features in a patient with acromegaly and thyroid papillary adenocarcinoma: a unique combination of endocrine neoplasia. Endocr J. 2012;59:791-796. [PubMed] |
| 7. | Wen MY, Wang Y, Meng XY, Xie HP. Endoscopic mucosal resection of duodenal bulb adenocarcinoma with neuroendocrine features: An extremely rare case report. World J Gastroenterol. 2015;21:7608-7612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Kadowaki Y, Nishimura T, Komoto S, Yuasa T, Tamura R, Okamoto T, Ishido N. Gastroduodenal intussusception caused by a gastric collision tumor consisting of adenocarcinoma and neuroendocrine carcinoma. Case Rep Gastroenterol. 2014;8:89-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Kim B, Huh JH, Kim Y, Chung MJ, Park JY, Song SY, Park SW. Duodenal adenocarcinoma following a neuroendocrine tumor in the duodenum. Korean J Intern Med. 2014;29:96-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Lee HH, Jung CK, Jung ES, Song KY, Jeon HM, Park CH. Mixed exocrine and endocrine carcinoma in the stomach: a case report. J Gastric Cancer. 2011;11:122-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Pavlovic M, Treaba DO S- Editor: Qi Y L- Editor: A E- Editor: Wang CH