Published online Jul 7, 2016. doi: 10.3748/wjg.v22.i25.5837
Peer-review started: March 28, 2016
First decision: May 12, 2016
Revised: June 5, 2016
Accepted: June 15, 2016
Article in press: June 15, 2016
Published online: July 7, 2016
Processing time: 99 Days and 0.8 Hours
AIM: To summarize the available information about injection use and its determinants in the South Asian region.
METHODS: We searched published and unpublished literature on injection safety in South Asia published during 1995-2016 using the keywords “injection”“unsafe injection” and “immunization injection” and combined these with each of the countries and/or their respective states or provinces in South Asia. We used a standardized questionnaire to abstract the following data from the articles: the annual number of injections per capita, the proportion of injections administered with a reused syringe or needle, the distribution of injections with respect to prescribers and providers and determinants of injection use.
RESULTS: Although information is very limited for certain countries (i.e., Bhutan, Maldives and Sri Lanka), healthcare injection use is very common across South Asia, with cross-country rates ranging from 2.4 to 13.6 injections/person/year. Furthermore, recent studies show that 5% to 50% of these injections are provided with reused syringes, thus creating potential to transmission of blood-borne pathogens. Qualified and unqualified practitioners, especially in the private sector, are the major drivers behind injection use, but patients also prefer injections, especially among the rural, poor or uneducated in certain countries. According to available data, Pakistan and India have recently taken steps towards achieving safe injection. Potential interventions include the introduction of reuse prevention devices, and patient-, community- and patient/community and provider-centered interventions to change population and practitioner behavior.
CONCLUSION: Injection use is common in South Asian countries. Multilevel interventions aiming at patients, providers and the healthcare system are needed to reduce injection use and reuse.
Core tip: The reuse of syringes in healthcare has been consistently identified as major route of hepatitis B and C transmission in Pakistan and India. Injection use and reuse is common in Pakistan, India and other South Asian countries. This paper synthesizes literature on injection use, re-use and potential interventions to reduce injection use and reuse to prevent hepatitis C transmission and hence overall disease burden. We also propose a multi-level model to guide further research, interventions and programs to prevent unnecessary injection use and reuse.
- Citation: Janjua NZ, Butt ZA, Mahmood B, Altaf A. Towards safe injection practices for prevention of hepatitis C transmission in South Asia: Challenges and progress. World J Gastroenterol 2016; 22(25): 5837-5852
- URL: https://www.wjgnet.com/1007-9327/full/v22/i25/5837.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i25.5837
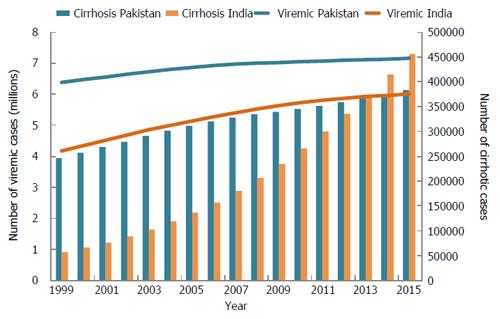
Hepatitis B virus (HBV) and hepatitis C virus (HCV) infections are global health concerns, particularly in South Asian countries where prevalence ranges from 2%-5% and 1.3%-4.8% for HBV and HCV, respectively[1-4]. Pakistan has second highest number of HCV infections in the world. HCV and HBV are associated with increasing morbidity and mortality in these countries. In Pakistan and India in 2015, there were 383301 and 455848 HCV infected people living with cirrhosis and about 16000 and 18000 died of HCV, respectively (Figure 1)[5].
During the early nineties, investigations of clusters of HBV and HCV infections in India and Pakistan revealed the reuse of glass and plastic syringes by unqualified and qualified practitioners as a major factor in occurrence of these outbreaks[6-8]. Later on, detailed investigations of HBV and HCV risk factors in well-planned studies from both countries revealed a consistent association of injections with these infections[9-13]. Based on these studies, reuse of syringes is major contributor to HBV and HCV transmission in India and Pakistan. More than 50% of HCV infections in Pakistan and about 38% of HCV infections in India are attributed to unsafe injections[14,15].
Although use of unsafe and unnecessary injections has long been reported from India[16,17]; unsafe injections as a public health problem became a major concern only after the explosive outbreaks of HBV and HCV in India and Pakistan. Despite the enormity of the problem, the level of concern is not the same in all countries of South Asia, as shown by variations in data availability on injection use and its determinants, and the extent of preventative actions at government levels. However, since countries in South Asia have similar healthcare systems, culture, and people beliefs and behaviors, best practices in countries that have achieved significant progress towards safe injections, may provide valuable lessons to other countries in the region who are just beginning to address this issue.
In this paper we have summarized the situation of injection use in the South Asian region. Specifically we have reviewed the frequency of injection use in populations, reuse of syringes and distribution of injections with respect to prescribers and providers.
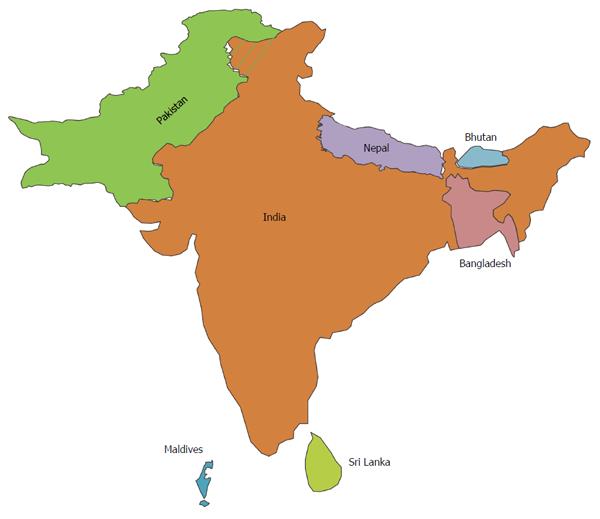
South Asia, which includes Pakistan, India, Bangladesh, Nepal, Sri Lanka, Maldives and Bhutan (Figure 2), is home to about 1.7 billion people. After independence from the British Empire in 1947-1948, these countries had similar health and development indicators, but some did better than others in later decades. From 2005 to 2013, the adult literacy rate ranged from 52.8% in Bhutan to 98.4% in Maldives. Infant mortality ranged from 8.2/1000 live births in Sri Lanka to 69/1000 live births in Pakistan. In terms of overall human development, Sri Lanka is ranked top in the region with a worldwide human development index of 73, while Pakistan is ranked lowest in the region with an index of 147 (Table 1)[18]. The health and development indicators indicate that the overall health status of the population in South Asia is not very impressive, but there are examples of success from Sri Lanka and Kerala in India[19].
| Indicators | Year | Sri Lanka | Maldives | India | Bhutan | Pakistan | Nepal | Bangladesh |
| Total population (millions) | 2014 | 21.4 | 0.4 | 1267.4 | 0.8 | 185.1 | 28.1 | 158.5 |
| GDP per capita (US$) | 2011 | 9426 | 11283 | 5238 | 7167 | 4454 | 2173 | 2853 |
| Population living below $1.25 a day (%) | 2002-2012 | - | 1.5 | 23.6 | 2.4 | 12.7 | 23.7 | 43.3 |
| Adult literacy rate (% ages ≥ 15) | 2005-2013 | 91.2 | 98.4 | 62.8 | 52.8 | 54.7 | 57.4 | 58.8 |
| Public health expenditure (% of GDP) | 2013 | 3.2 | 10.8 | 4.0 | 3.6 | 2.8 | 6.0 | 3.7 |
| Stunting (moderate or severe) (% under age 5) | 2008-2013 | 14.7 | 20.3 | 47.9 | 33.6 | 45.0 | 40.5 | 41.4 |
| Infant Mortality rate per 1000 live births | 2008-2013 | 8.2 | 8.4 | 41.4 | 29.7 | 69.0 | 32.2 | 33.2 |
| Overall human development index | 2015 | 73.0 | 104 | 130 | 132 | 147 | 145 | 142 |
We searched published literature in PubMed from Jan 1, 1995 - Feb 23, 2016 using keywords “injection”, “unsafe injection”“immunization injection” and combined these with each of the countries and/or their respective states or provinces in South Asia. In addition, we also searched the websites of WHO, UNICEF for each country for unpublished reports, including evaluations of the expanded program on immunization (EPI). We contacted researchers in each country for unpublished literature. We also reviewed relevant references cited in identified articles (Table 2).
| Key words | India | Pakistan | Bangladesh | Nepal | Sri Lanka | Maldives | |
| PubMed - Retrieved | Injection and country/state | 189 | 51 | 12 | 14 | 13 | 5 |
| PubMed - selected/relevant | 25 | 25 | 5 | 8 | 0 | 0 | |
| Google Scholar1 | Unsafe injections, injections, country | 3 | 1 (419) | 2 (329) | 1 (242) | 0 (40) | |
| Unsafe injections, injections, country | 2 | 1 | 0 | 0 | |||
| WHO website | 0 | 0 | 0 | 0 | 0 | 0 | |
| PATH | 2 | ||||||
| In country assessments by MoH | 1 | ||||||
| Unpublished reports | 1 | 2 | |||||
| Other circumstantial evidence2 | |||||||
| Risk factors studies suggesting injection use | Risk factors, HBV (HCV), country | 1 | |||||
| Hepatitis B/C | Hepatitis B, Hepatitis C, Country | 19 (38) | 13 (36) | ||||
| Health care utilization | Health care seeking, Health care utilization, Private practice, Country | 15 (32) | 6 (16) | ||||
| (retrieved) | |||||||
| Private practitioners health seeking (retrieved) | Health care seeking, Private practice, Country | 5 (8) | 3 | ||||
| Prescribing practices (retrieved) | Prescription practices, Country | 5 (5) | 1 |
We developed a questionnaire to standardize data abstraction from the articles. Indicators of injection use that were identified and assessed are: the annual number of injections per capita, the proportion of injections administered with a reused syringe or needle, and the distribution of injections with respect to prescribers and providers. We also assessed determinants of injection use.
Annual number of injections per person: To estimate the annual number of injections per person, we selected population based surveys designed for estimating the frequency of injections. These studies yield high quality estimates, although such studies are rare. If estimates from a national or well-designed population based survey using WHO standard methodology over large area of injection use were available, we presumed these to be the best estimates.
Proportion of injection reuse: To estimate the proportion of reuse of syringe or needle for each country, we restricted our selection to standardized observational studies, preferably based on WHO’s tool of injection practices. For each country, we presented the range of the estimates from the studies.
Distribution of injections with respect to prescribers: We reviewed the distribution of injections with respect to prescribers, injection providers and settings.
If no information was available about the annual ratio of injections per capita, proportion reuse or the prescribers for a country, we used circumstantial evidence to infer if there is an injection overuse or safety problem in the country. We used these evidences in the following order, if available: qualitative studies to assess injection practices; studies to describe prevalence and risk factor for HBV, HCV and HIV; and studies of prescription practices and health care seeking.
Healthcare injection: We defined a healthcare injection as a procedure that introduces a substance into the body through a piercing of the skin or mucosal membrane for the purposes of curative or preventive health care, whether administered in a formal healthcare setting (for example, a clinic or hospital) or other settings (such as homes or pharmacies)[20]. Injections of illicit drugs were not considered in this study.
Reuse of injection equipment in the absence of sterilization: We defined reuse of injection equipment in the absence of sterilization as the administration of an injection to a recipient with a syringe or a needle that had been used previously on another person and that was reused in the absence of sterilization. Sterilization means a procedure that kills HBV, HCV and HIV in and on the syringe or needle. In this paper we will refer to reuse of injection equipment in the absence of sterilization simply as “reuse of injection equipment.” Some studies have assessed the unsafe use of injections using other parameters. We have elaborated these parameters while describing these studies.
Injection prescribers and injection providers: A public provider is defined as a health care provider, whether a physician or a dispenser, working in a public sector. A private provider was defined as a health care provider, whether a physician, dispenser or any other primary health care worker, running a clinic/hospital in the private sector[21]. We defined physician as a person with basic medical qualification (MBBS or MD) and a private provider with MBBS was called general practitioner. “Unqualified practitioners” were defined as those with no basic medical qualification (MBBS or MD) and who prescribe medications A prescriber is a person who provides consultation and prescribes injections and drugs while injection provider, also called dispenser in the region, is a persons who dispenses medicine and provides injection.
From PubMed, we were able to retrieve 25 papers on injection safety for India, 25 for Pakistan, 8 for Nepal and 5 for Bangladesh. For the rest of the countries we searched through Google scholar and we found 7 additional articles that provided some evidence about injection use in India, Nepal, Bangladesh and Sri Lanka (Table 2). Table 3 lists the studies and their characteristics that are used in this review.
| Ref. | Study type | Setting | Study base | City/province | n | Sampling | Year | Year |
| conducted | published | |||||||
| India | ||||||||
| Rajasekaran et al[37] | Population survey | Both | 3 areas | Tamil Nadu | 175 | Convenience | 2001 | 2003 |
| IPEN study group[40] | Population survey | Both | Whole country | whole country | 23997 | Cluster sampling | 2002-2003 | 2004 |
| IPEN study group[40] | Patients exit interview and observations | Both | Whole country | whole country | 6015 | Cluster sampling | 2002-2004 | 2004 |
| Murhekar et al[36] | Population survey | Island | Nicobar Island | 210 | Cluster sampling | - | 2004 | |
| Kotwal et al[34] | Population survey | Both | City | Delhi | 150 | Cluster sampling random | 2003 | 2004 |
| Anand et al[38] | Population survey | Rural | 1 village | Haryana State | 1280 | Systematic sampling | - | 2001 |
| Lakshman et al[35] | Patients exit interview and observations | Both | 15 miles around a town | Tamil Nadu | 400 | Consecutive patients | - | 2000 |
| Becker et al[66] | Population survey | Both | 1 district | Karnataka | 4949 | Cluster sampling | 2003 | 2005 |
| Kermode et al[67] | Population survey | Urban | 2 cities | New Delhi and Imphal | 200 | Convenience | 2004 | 2006 |
| Kermode et al[41] | Patients and relatives survey | Rural | 2 hospitals | Bihar and Jharkhand | 280 patients, | Systematic sampling, convenience | 2004-2005 | 2006 |
| 120 relatives | ||||||||
| Pandit et al[42] | Population survey | Both | 1 District | Anand | 182 HF1 | Stratified and simple random | 2004 | 2008 |
| 2080 | ||||||||
| Shah et al[68] | Providers interview | Both | 1 district | Gujarat | 251 | Random sampling | 2012-2013 | 2014 |
| Bhargo et al[43] | Providers interview | Urban | 1 district | Gwalior | 30 | Convenience | 2012-2013 | 2014 |
| Garapati et al[44] | Providers interview and observation | Both | 1 district | Andhra Pradeh | 300 | Convenience | 2010-2011 | 2014 |
| Bendale et al[69] | Hospital survey | Urban | 1 district | Maharashtra | 20 sites | Random sampling | 2015 | |
| Pakistan | ||||||||
| Raglow et al[22] | Survey of OPD patients | Urban | Patients | Karachi | 198 | Consecutive patients | 1995 | 2001 |
| Janjua et al[23] | Population survey | Both | 2 districts | Sindh | 1150 | Cluster sampling random | 2001 | 2005 |
| Janjua et al[29] | Population survey | Both | 2 districts | Sindh | 1150 | Cluster sampling random | 2001 | 2006 |
| Janjua et al[26] | Patients exit interview and observations | Both | 3 districts | Sindh | 2124 | Random sample of clinics | 2004-2005 | UP |
| Janjua et al[27] | Population survey | Both | Whole country | Whole country | 10023 | Cluster sampling | 2006-2007 | 2014 |
| Yousafzai et al[25] | Provider survey | Urban | City | Karachi | 317 | Convenience | 2006 | 2013 |
| Khan et al[6] | Patients exit interview and observations | Peri-urban | 1 village | Sindh | 203 | consecutive patients | 1995 | 2000 |
| Mantel et al[70]2 | Patients exit interview | Both | 8 districts | 3 provinces | Random sample of clinics | 2002 | UP | |
| PDHS 2012-13[24] | Population survey 15-49 years of age | Both | National | F: 13558 | Cluster sampling random | 2012-2013 | 2014 | |
| M: 3134 | ||||||||
| Bangladesh | ||||||||
| Gibney et al[71] | Risk factor study | Urban | Truck stand | Dhaka | 387 | Cluster sampling random | 1999 | 2001 |
| Shill et al[51] | Provider interviews and facility records | Rural | Primary Health Care Centres | Dhaka | 6 | Convenience sample | 2009 | 2011 |
| Chowdhury et al[50] | Provider interviews, FGD, observations and prescription review | Primary Health Care Centres | National | Prescription: 4320 | Cluster sampling | 2008-09 | 2013 | |
| Injection events: 480 | ||||||||
| Sri Lanka | ||||||||
| Rannan-Eliya et al[59] | Patients exit interview | Both | National | Sri Lanka | 2100 | Random sample of clinics | 2000 | 2003 |
| Nepal | ||||||||
| Gyawali et al[54] | Survey of pharmacies | Urban | City | Pokhara | 54 | Convenience sample | 2012 | 2014 |
| Gyawali et al[52] | Population survey | Both | 1 district | Kaski | 2470 | Stratified sampling | 2012 | 2014 |
Injection use and prescribers: Many studies reported an association between injections and HBV and HCV outbreaks during the 1990s[7,9,10]. This association led to a study of injection use among patients presenting to the Aga Khan University Hospital Community Health Center in 1999, which reported 8 injections per person per year[22]. This study was then followed by a population based survey in two districts of Sindh province in 2001 which reported an annual ratio of 13.6 injections per capita. After excluding the top 2% , the annual ratio was 8.2 per capita[23]. A more recent 2012-13 Pakistan Demographic and Health survey (PDHS), which included a nationally representative sample of men and women ages 15-49 years, reported 5 injections per person per year (women: 5.4 and men: 4.9). However, this survey only included those between 15 and 49 years of age, a group which generally has lower health care needs compared to younger and older population[24] (Table 4).
| Ref. | Annual ratio of injections per capita | Received an injection | Therapeutic | Injection reuse byinterview7 | Injection reuse byobserving | Overall unsafe |
| India | ||||||
| Rajasekaran et al[37] | 2.4 | 60.6%1 | 87% | 64.6% | ||
| IPEN study group[40] | 2.91-5.8 | 27.1%1/44.1%3 | 82.5% | 31.6% | 62.9% | |
| Murhekar et al[36] | 3 | 21.9%1 | 91% | 6.5% | ||
| Kotwal et al[34] | 5.1 | 45.6%1 | 71.2% | 56.5% | 77.5% | |
| Anand et al[38] | 2.45 | 35%4 | 40%-100% | 45% | ||
| Lakshman et al[35] | 89%3 | 100% | 73%-99% | 99% | ||
| Becker et al[66] | 3.5 | 67.7%6 | ||||
| Kermode et al[67] | 8.6 | 15%2 | 68% | 31% | ||
| Kermode et al[41] | 43%2 (Patients) | 100% | 7.6% | |||
| 13.3%1 (Relatives) | ||||||
| Pandit NB | 0.2 | 21.6%6 | 77% | |||
| Shah et al[68] | 64.1% | |||||
| Bhargo et al[43] | 76.7% | |||||
| Garapati et al[44] | 0.72 | 14.3% | ||||
| Pakistan | ||||||
| Raglow et al[22] | 8.4 | 51%5 | 100% | 48% | 16% | |
| Janjua et al[23] | 13.6 | 68%1 | 94% | 46% | ||
| Janjua et al[26] | 74%1 | |||||
| Janjua et al[23] | 55%3 | 47% | ||||
| Janjua et al[27] | 51%6 | 4% | ||||
| Yousafzai et al[25] | 87% | |||||
| Khan et al[6] | 81%3 | 90% | 94% | |||
| Mantel et al[70] | 12% | 65% | ||||
| PDHS 2012-13[24] | F:5.4/M:4.9 | F:61%/M: 53%6 | F:15%/M:10% | |||
| Bangladesh | ||||||
| Gibney et al[71] | 39.7%6 | 100% | ||||
| Shill et al[51] | 4.88 | |||||
| Chowdhury et al[50] | 77.7% | 15.5% | ||||
| Sri Lanka | ||||||
| Rannan-Eliya et al[59] | 3%3 | |||||
| Nepal | ||||||
| Gyawali et al[54] | ||||||
| Gyawali et al[52] | 2.37 | 10.4%1 | 97.1% |
A national survey conducted in 2007-08 to assess HBV and HCV prevalence found that 48% respondents received < 5, 22% received 5-10 and 6% received > 10 intramuscular injections. However, this study may have underestimated injections as it only inquired about intramuscular injections[4].
In a Sindh survey, 96% injections were provided for therapeutic purposes, the majority (63.1%) of which were given at the private general practitioners (GP) clinics by dispensers (75%) who were often not qualified, a finding corroborated by another recent study[23,25]. A study of injection use at clinics of GPs, public health care facilities and unqualified practitioners in 2004-2005, selected randomly from three districts in Sindh province, indicated that 95.6% (95%CI: 93.9%-97.2%) of the administered injections were unnecessary[26]. In summary, a large number of injections are administered in Pakistan, with the majority being unnecessary and occurring in the private sector.
Safety of injection equipment: A study in a peri-urban community in Karachi conducted in 1995 reported that 94% of the 54 observed injections were provided with reused injection equipment[6]. In a population based survey in Sindh province, only 54% (454/1150) of the respondents had been injected with newly opened injection equipment[23]. A study at the public and private sector in three districts of Sindh province revealed that 59.3% (677/1153) of injections are provided with a new syringe opened in front of a patient[23] (Table 4). The PDHS 2006-07 (women only) and 2012-2013 (both men and women) inquired about injection with newly opened syringes. In the 2012-2013 PDHS, 85% of women and 90% of men reported receiving an injection with a newly opened syringe. There were marked geographic differences in injections with new syringes ranging from 68% and 58% in Baluchistan province to 90% and 96% in Punjab among women and men, respectively[24]. Similar results were reported in the 2006-2007 PDHS[27]. In a national HBV and HCV survey, 49% of injections were provided with re-used syringes[4]. These data suggest some improvements in injection reuse in Pakistan, but still there is substantial reuse happening in Pakistan, calling for multilevel interventions.
Determinants of injection use: Injection use occurs because of preference of injections by both prescribers and patients (Table 5). A qualitative study for determinants of injection use in Sindh province reported that the practitioners take the initiative for injection prescription. However, some patients believe that disease can only be cured by injections. Quick relief, referred to as early relief from the disease was reported as the main reason for patients to prefer injections. Daily wage earners were concerned about loss of their working day and practitioners gave them assurance that injection could quickly relieve their symptoms allowing them to go back to work the next morning[28]. These results have been substantiated by an epidemiological study that quantified the beliefs of the general population in two districts of Sindh province regarding injection use. The study revealed that the majority of subjects (80.6%) were not aware of the risk associated with injection use. Multivariable logistic regression analysis for factors associated with receiving an injection revealed that those living in rural areas who believe “injections act faster than oral drugs and symptoms are quickly relieved” were 15 times more likely to receive injection than those living in urban areas without this belief. Those who live in urban areas and believe in the quick action of injections were 2.5 times more likely to receive injections than those who did not believe in quick action of injections. Similarly those who believed that a disease can only be cured by injections were 2.2 times more likely to receive injections[29]. In a recent analysis, poor knowledge about blood borne pathogens was associated with receiving injections with used syringes[27].
| Ref. | Prescribed by GP | Prescribed by unqualified practitioner | Provided at private clinic | Provider dispenser | Patient prefers Injection | Practitioner prefers injection | Practitioner says patient demand it |
| India | |||||||
| Rajasekaran et al[37] | 59% | 37.6% | 40% | 87.2% | |||
| IPEN study group[40] | 42.6% | 57.5% | 77%1/34%2 | 93.5% | 10.2% | 70.6%3 | 88.6% |
| Murhekar et al[36] | 50.8% | 54.8% | |||||
| Kotwal et al[34] | 13.8% | 58.8% | 30% | ||||
| Anand et al[38] | 18% | ||||||
| Lakshman et al[35] | 65% | ||||||
| Kermode et al[67] | 8% | 35% | |||||
| Kermode et al[41] | 55% (patients) | 24.8% (patients) | 7.7% (patients) | 9.3% (relatives) | |||
| Pandit et al[42] | 57% | 55% | 17% | ||||
| Garapati et al[44] | 48.7% | ||||||
| Bendale et al[69] | 8.16% | 35% | 65% | ||||
| Pakistan | |||||||
| Raglow et al[22] | 94% | 94% | |||||
| Janjua et al[23] | 63% | 28% | 69% | 76% | 16% | ||
| Janjua et al[26] | 63% | 28% | 63% | 32% | |||
| Janjua et al[23] | |||||||
| Janjua et al[27] | 52% | 16% | |||||
| Yousafzai et al[25] | 7.9% | 8.8% | 71% | ||||
| Khan et al[6] | 44% | ||||||
| Bangladesh | |||||||
| Gibney et al[71] | |||||||
| Shill et al[51] | 50% | ||||||
| Sri Lanka | |||||||
| Rannan-Eliya et al[59] | |||||||
| Nepal | |||||||
| Gyawali et al[54] | 92.6% | ||||||
| Gyawali et al[52] | 12.6% | 21.4% | 5% |
The relative contribution of prescribers in injection overuse is greater than that of the population inclination for injections. Patient exit interviews in a cross-sectional study at public and private clinics in three districts of Sindh province revealed that 60% of the 2124 patients surveyed left the choice for type of medication to the practitioner while 22.5% demanded injections in the current visit[26]. Another study in the community showed that of the 815 who remembered their last injection, 32% demanded injections at their contact with a health care provider while 62.2% left the choice of prescription to the prescribers[29]. An exit interview study of patients in a peri-urban community of Karachi reported that 40% prefer injections if told oral and injectable drugs are equally effective[6]. A high proportion (28%) of injections are prescribed by unqualified practitioners as documented by two studies in Pakistan[23,29]. Hence, although some patients demand injections, these studies consistently report that providers’ decision to administer injection is major driving force for injection overuse in Pakistan. Economic incentives of the practitioners have been reported to play a role in injection overuse since practitioners earn more if they provide injections. In such circumstances, the use of reuse prevention devices (RUP) such as autodisable (AD) syringes could prevent the injection equipment reuse[23].
An assessment of a simple health education program through community outreach about the risks associated with unnecessary and unsafe injections in Hafizabad (a town where an earlier study of injections and HCV infections were conducted) found that the use of new syringes increased from 24% in 1994 to 59% in 1998; however, the number of injections stayed the same[30]. Since injection prescribers are major drivers behind injection overuse, addressing their behaviors including behaviors of unqualified practitioners is also needed[31].
Another study at GP clinics in Karachi that used interactional group discussion (IGD) methodology, involving patients and prescribers discussing their choice for medication, resulted in: reduction in injection use by 33% from a baseline of 84%; an increase in the use of new syringes from 77 % to 92% in the intervention group; and dropped from 74% to 67% in control group[32]. The implementation of such intervention on a larger scale in national programs needs to be assessed.
A study conducted in 2011 in Sindh province assessed the community based interventions focusing on messages in large gatherings and discussions with key community influencers including teachers and religious leaders (Imams) along with messages on safe injection use in media. The study showed an increase in HBV and HCV knowledge and report of injection with new syringe from 15% to 29%[33].
In August 2004, the Ministry of Health Pakistan, Aga Khan University, the World Health Organization’s local office and UNICEF organized a first national workshop/meeting to devise a national policy on injection safety in Pakistan. The workshop produced the National Policy on Injection Safety draft that highlighted the need for: population and provider behavior change, adequate supplies of injection devices, switching to reuse prevention injection devices and safe disposal of sharp waste. The syringe manufacturing industry has shown an interest in manufacturing Re-Use Prevention (RUP) injection devices for therapeutic injection to prevent reuse. Immunization injections in the EPI are already provided with AD syringes. Two manufacturers had shown an interest in supplying AD and RUP syringes for immunization and medical injections, but due to lack of progress on policy and legislation, this did not materialize.
In 2005, the government in Pakistan launched the National Program for Hepatitis B and C Prevention, with injection safety being one of its major components. The program included communication and behavior change and construction of incinerators throughout the country for disposal of syringes. However, there is still a need to develop and test methodologically sound interventions based on theories of behavior change to achieve reduction in injection use and reuse of injection equipment. Overall, two types of interventions, one focusing on providers and patients in small groups and the other focusing on the community as a whole, showed improvement in injection safety.
Injection use, prescribers and providers: Since the 1980’s, there has been an awareness of injection overuse in India[16,17]. During the 1990s, the medical/public health community became more concerned with the emergence of HIV/AIDS and the occurrence of injection associated outbreaks of HBV and HCV in many parts of India[8,11,12]. Since then, many injection use studies have been reported from various parts of India (Table 3)[34-39]. In India, the receipt of injections per person per year ranged from 0.2 to 8.6 injections (Table 4). In 2002-2003, a national assessment of injection practices was conducted using a population survey utilizing cluster sampling. The study involved interviews at home, observation at clinics and exit interviews of patients. The results revealed that each person received between 2.8 (based on 3 mo recall) to 5.8 (based on past 2 wk recall) injections per year with a higher number (9.5) for those ≤ 1 year of age. Overall, 17% injections were provided for vaccination purposes. At public facilities 68.0% of injections were for vaccination purposes compared to 31.9% in the private sector. The proportion of injections for vaccination is higher in India than other countries including Pakistan. Injections are provided by unqualified health workers (helper/trainee/assistant, yet-to- qualify) to qualified practitioners. Infacility survey, 44% of patients at private clinics and 38% of public clinics received an injection. A higher proportion of patients received injections at non-formal prescriber clinics (58%) and Indigenous Medicine clinics (53%). In the private sector, unqualified helpers/assistants provided most of the injections compared to health workers or nurses in the public sector. Public facilities prescribed 34% of all injections for fever, diarrhea or cough while 49.5% of private facilities provided injections for these complaints. However, most of these injections are not required as these conditions can be treated with oral drugs[40].
Private practitioners are more likely to provide injections as compared to public practitioners. Data from other studies suggest that injections are prescribed by a variety of practitioners ranging from unqualified dispensers who learned injection administration while working at a clinic to a qualified medical practitioner (MBBS)[34-38,41-43].
Safety of injection equipment: The national assessment of injection safety in 2002-2003, described above, found that glass syringes are still being used although less common (27.2%)[40]. Overall, 32% of the injections provided could potentially transmit blood borne pathogens and 62.9% were considered unsafe. The highest proportion of unsafe injections were reported from immunization clinics (74.0%) followed by government (68.7%) and private health care facilities (59.9%)[40]. Other studies have reported varying proportion of unsafe injections (Table 4).
Determinants of injections: The majority of the injections were administered by private practitioners driven by economic benefits. Qualitative data from the National assessment suggest that injections are prescribed for money, for quick relief, and to maintain credibility among patients. Studies have consistently reported that prescribers, rather than patients, make the decision for injection most of the time (> 50%)[40], though more patients in rural areas (43.1%-47.8%) have shown preference for injections as compared to those in cities (19.4%) (Table 5)[37]. In a study from Car Nicobar Island, 54.8% of participants preferred injection for treatment of a fever while only 36.2% preferred oral medication[36]. In summary, practitioners reported that injections are provided because patients demand/prefer them while in reality only small numbers of patients prefer injections[40,44]. This common phenomenon of cognitive dissonance has also been reported from other parts of the world[45].
Progress towards promoting safe injection practices: India took a giant leap towards promoting safe injection practices once the injection problem was recognized at a high political level[46]. The Indian Medical Association (IMA) and the Indian Academy of Pediatrics (IAP) issued injection safety policies and endorsed the use of safe injections by its members in 2004[47]. IMA started a national project in which about 400 leaders of the IMA from five regions of the India were trained in injection safety issues in workshops with the expectation that they would address the issues at the local level among practitioners. IMA organized a special session in its national conference and distributed a CD of safe injection practices among 1500 participants. Andhra Pradesh state IMA took the lead and started a pilot project with Program for Appropriate Technologies in Health (PATH) to educate members at its local branches about injection safety. A “Model Injection Center” was developed by PATH in collaboration with Niloufer Hospital attached to Osmania Medical College, Hyderabad, to educate the medical community about the safe administration of injections[48]. In 2014, the National Centre for Disease Control issued guidelines on safe and appropriate use injections in medical practice[49].
A national assessment of injection practices 2003-2004 in India showed that 48% of the injections were provided with glass syringes in immunization programs, where the sterility of syringes is always uncertain. The government decided to switch to AD syringes that prevent reuse. This is a big step towards ensuring safety of immunization injection, however immunization injections are a fraction of all provided injections and most of the injections are provided in the private sector.
Local and international manufacturers of syringes have started producing immunization and therapeutic RUP at an affordable price. With the implementation of the South Asia Free Trade Agreement, these syringes will be available to people in other countries in South Asia at the same low price (5 US Cents).
However, this is just the beginning of a journey towards safe injections for India. Strategies need to be developed for making injections safer in the private sector, and to encourage behavior change of prescribers, providers and the population.
Injection use, prescribers and providers: We found two published articles on injection practices from Bangladesh. Chowdhury et al[50], conducted a study in 2008-09 at 24 primary health care centers (PHC) across Bangladesh and included three components: (1) a retrospective review of prescriptions; (2) systematic observation of PHCs facilities, injection providers, waste handlers, and injection administering events; and (3) six focus group discussions (FGDs) with prescribers and 38 in-depth interviews with doctors, nurses, and waste handlers on injection safety practices. In this study, 78% of 3354 prescriptions included at least one injection. The most commonly provided injections included antibiotics (78.3%), IV fluids (38.6%), analgesics/pain killers (29.4%), vitamins (26.7%), and anti-histamines (18.5%). About 85% of 480 observed injections were provided with new syringes and new needles. Reuse of syringes was higher in Sylhet (25%). Qualitative data revealed that decisions for injection prescriptions were influenced by: prescribers’ belief in efficacy of injections compared to oral medication; perception of the seriousness of the disease; quest to prove superiority over other doctors by using high-cost “powerful medications”; and the perception that patients want injection because patients do not consider prescriptions without injection as good as injections, and patients desire quick relief[50].
Shill et al[51] conducted a retrospective review of prescriptions at six primary health care units in Dhaka in 2009. This study found that about 60% of prescriptions included an injection. Major reasons for injection prescriptions by prescribers included seriousness of illness, patient’s demand, belief in injection efficacy, and injection prescription by an assistant in absence of physician.
The above mentioned studies reported high injection use in facilities, but did not report on population level injection frequency and distribution by public and private sector which is important for planning interventions to reduce injection use and re-use. Studies are needed to estimate the annual ratio of injections which could be accomplished by including questions on injection use in demographic and health survey similar to Pakistan.
Data on injection use in Nepal has been reported recently. A population based study including a cross-sectional survey (2470 people from 600 households) and FGDs with those who reported receiving injections was conducted in 2012 in Western Nepal[52]. In this study, 10% of individuals received an injection during the last three months, and annual ratio of injection per capita was 2.37. About 3% of injections were provided for vaccination. Of the respondents who recalled their last injection, 77%, received their injection from a formal health provider (physicians, nurses or other trained healthcare worker) while 21% received injections from a medical dispenser. Of all injections, 95% were provided with a new single use syringe taken from a sealed packet. In this study, 79% of 714 respondent preferred oral drugs for fever, 5% preferred injection and 16% had no preference (Table 5). Data from this study suggest that injection use in this part of Nepal is low and most injections are provided with new syringes and population does not prefer injection. However, these data are in contrast to an earlier qualitative study conducted in 2000 in seven districts of Nepal’s central region. This earlier study included FGDs, secret shoppers interaction and in-depth interviews with consumers and providers[53]. The study indicates that injection use is common, as reported by both consumers and providers; however the exact magnitude is not known. Most of the injections are unnecessary, provided for weakness, pain, fever and flu and include multivitamin (7 of 50 observations), painkillers and antibiotics. Various types of practitioners prescribe injections ranging from those unqualified with no formal schooling at all to qualified physicians; most are administered by the unqualified practitioners. The majority of injections are provided at pharmacies and “medical shops” but also at homes, and grocery stores. The use of glass syringe has declined and disposable syringes are used most of the time, but reuse of these syringes is common. Reusing a syringe is more often done by unqualified practitioners and for poor and less educated people. Reuse of syringes has been reported consistently from observations, in-depth interviews and focus group discussions.
In most of the interactions with practitioners, patients did not request injection; practitioners made the decision for the medication especially for poor and less educated patients. However, at the same time many practitioners refused injections to secret shoppers. However, during in-depth interviews providers reported that patients, especially the less educated, demand injections and that is why they provide injections. Most of the patients think that it is better to use oral drugs and use injections for serious conditions but some also believe that injections are fast acting and more efficacious then oral drugs. However, most consumers believe that children should be treated with injections. Most consumers are aware of the risks associated with injections, like injection abscesses and even death either because of their own experience or that of family or friends.
An assessment of pharmacy and injection practices at pharmacies in Western Nepal revealed that 91% pharmacies dispensed and administered injections. About half of these pharmacies reported dumping sharp waste into municipal waste[54].
In summary, there is wide variation in injection use in Nepal. There is need to collect data on injection use from all regions of Nepal using standardized methodology to inform programs.
No published or unpublished report was available to describe the magnitude of injection use in Sri Lanka. The prevalence of HBV and HCV is low in Sri Lanka, although recent estimates from large, well designed studies are not available[55,56].The private sector played a negligible role in provision of health care until 1977 when the government allowed private practice physicians. Recently there has been growth of the private sector that is now providing about 45% of the outpatient care[57]. This is much less than the 80% provided by the private sector in India and Pakistan. There have been some reports of malpractice of physicians in the private sector in terms of over prescription of drugs[58]. A national survey was conducted in 2000 to assess the size of the primary care private sector and the quality of their practice by the Institute of Policy Studies[59]. The study included clinics run by full time private practitioners and excluded private practice of government physicians (a substantial proportion) and traditional and unqualified practitioners. The study reported that the private practitioners provide about 15% of outpatient care in Sri Lanka. Assessment of prescriptions revealed that: no medication was prescribed in 14% of cases, the mean number of items prescribed per consultation was 2.7, and only 3% of the prescriptions contained an injection. The authors concluded that the quality of care is comparable to that provided by GPs in Australia[59].
The available evidence suggests that injection use is not very common in Sri Lanka. There are many plausible explanations for this. A large proportion of those in private practice have post graduate qualifications in family medicine. All of the practitioners receive their initial training and many years of post-internship practical experience in the public sector where rational prescription is a norm. Moreover, the literacy level of the population is also very high.
We were not able to find any published or unpublished reports that relate to injection safety in these countries.
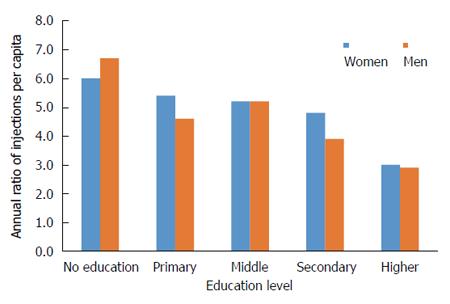
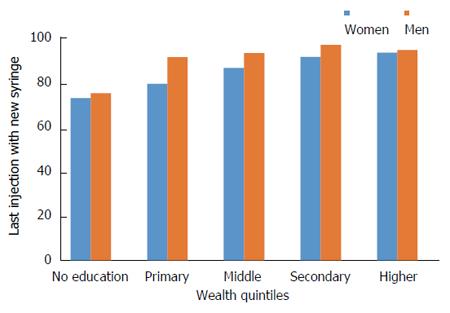
Limited data on socioeconomic disparities in injection use was available. In the 2012-13 PDHS, men and women in rural areas reported receiving more injections compared to those in urban areas of Pakistan (women: 5.8 vs 4.7; men: 5.2 vs 4.2)[24]. A similar finding of higher injection use in rural areas has been reported from Indian[40]. PDHS also reported a decreasing trend in number of injections received with increasing education level, with the number of injections being about twice as high among those with no formal schooling compared to those with higher education for both men and women (Figure 3). There was no clear relationship between wealth and injection use, however, injection with a new syringe increased with an increase in wealth of the patient for both men and women (Figure 4)[24,27]. Other data from both India and Pakistan support that people in rural areas, with low education level and those in lower quintiles of wealth are more likely to receive low quality health care including injections with use syringes[34,60].
This is the first paper to summarize evidence on injection use in South Asia. Overall, injection use is very common in South Asia with variation across countries (2.4-13.6 injections/person per year) with a varying proportion of injections being unsafe in recent studies (5%-50%). In this regard, Sri Lanka is an exception where limited available reports suggest that very few injections are used. Studies to assess injection use are not available from Maldives and Bhutan. Injections are provided in formal and informal sectors, more so in the private than the public sector. Practitioners are the major driving force behind injection overuse, although patients from different parts of South Asia also prefer injections as a form of therapy. Countries for which ample injection use data is available (India and Pakistan), have taken major steps towards promotion of safe injection practices. Hence the availability of data about unsafe injections plays an important role in mobilizing political will to reduce unsafe injection practices. The paucity of information in the region from rest of the countries demands an immediate assessment of injection safety to inform optimal response.
Available evidence suggests some major similarities in injection use patterns across countries. Injection use is high and most of the curative injections are provided in the private sector and prescribed by a variety of prescribers that include unqualified as well as qualified practitioners. Similarly, injection providers range from qualified health workers to unqualified providers, with the latter being more common in the private sector. Reuse of injection equipment or unsafe injections are also more common in the private sector. Mostly prescribers make the decision for injections although there is demand for injections from consumers as well. Consumer demand varies from one place to another within a country as well as between countries.
In Pakistan, Nepal, and India, the poor and uneducated are more likely to be prescribed injections which are prone to be unsafe if they are being provided at an unqualified practitioner’s clinic, especially in rural areas[22,23,34]. Practitioners state that poor and uneducated people demand more injections, but in most cases the decision about injections is made by a practitioner not the consumer. Very few patients demand injections and the poor are less likely to do so because of the power differential. Choice of the practitioner made by the economically disadvantaged and uneducated patients may put them at a higher risk of unsafe and unnecessary injections. For example, in Pakistan those in the lowest income bracket were more likely to seek care from unqualified practitioners[60] and in India those with income < 5000 rupees were more likely to receive injections from informal health care workers[34]. Other reasons could be that poor and uneducated are not aware of the risks associated with injections or the reuse of syringes and are more concerned about getting better quickly and returning to work soon so as not to lose their wages[6,23,27,28,34,37,51]. In Pakistan, knowledge of bloodborne pathogens increased incrementally with education level and injection administration with new syringes increased with this increase in knowledge. Furthermore, 70% of those who had no formal education and lacked knowledge on transmission of HCV with reused syringes received injections with a new syringe, while 94% of those who had some education and knowledge on HCV transmission with reused syringes received injections with a new syringe[27]. Thus, higher education level, wealth and knowledge are all associated with higher percentage of injections with a new syringe. Higher education level and socioeconomic status also provide empowerment and increases self-efficacy, enabling the patient to negotiate quality of care. Thus, large scale interventions on knowledge and awareness related to oral and injectable medication efficacy and harms associated with injections may reduce injection use and reuse among the general population with higher education and socioeconomic status. Mass awareness campaigns using low cost health education material on injection safety and information dissemination through community meetings and mosques etc., has been shown to reduce the reuse and overuse of injections[30,33].
People with low education levels and wealth are less empowered and there is a greater power differential with their healthcare provider. Thus, this segment of population has lower self-efficacy to negotiate care quality and injection prescription. Interventions to improve self-efficacy to negotiate injection prescription could be successful in reducing injection use and reuse. Tools to help in initiating discussions on different types of medications could be useful in this regards. Support structures to change overall prescription environment by empowerment of community and community expectation of safe injection practices from prescribers and providers could aid in the overall injection prescription negotiation and reducing injection use. Community education and involvement has been successful in increasing knowledge levels and injections with new syringes in rural area of Pakistan[33].
The discrepancy between patients’ preference for injections and prescribers’ beliefs that patients demand it is present in all the countries for which data is available. This gap is greater in urban than rural areas where a larger proportion of patients have shown preference for injections. A behavior change intervention - Interactional Group Discussion (IGD) - to convince prescribers that patients do not systematically prefer injectable medications has been successful in reducing injection use and reuse in Indonesia, Pakistan and India[32,45,61]. Hence, behavior change among practitioners and the population can reduce unsafe injection; however, these strategies need to be tested on a large scale in public health programs.
Since there is a concern among practitioners that if they do not provide injections their clients will shift to other practitioners, professional medical associations could play an important role in alleviating this concern. Dialogue and consensus at the local level and endorsement at the national and local levels about appropriate use of injections and counseling of patients about the appropriateness of injection could allay the fear of losing clients and reduce injection use. These activities can have enormous impact over large areas without too much cost. Pilot projects should test the involvement of professional associations and practitioners in improving safety and reducing overall injection use.
A large proportion of injection use occurs in the private sector and many studies have indicated that the role of economic incentives in the reuse and overuse of needles/syringes by practitioners[6,22,23,32]. Structural interventions in the form of re-use prevention (RUP) injection devices can play a major role in reducing reuse of injection devices. However, their use in the private sector can only occur if the price is affordable (similar to or lower than conventional devices) and conventional devices are replaced with RUP injection devices. Partnerships between industry and governments can play a major role in providing these devices at an affordable price and assist with the phase-out of conventional devices from the market. The likely role of government is to establish a policy of RUP injection device use at all health care facilities and to provide incentives to manufacturers in the form of tax subsidies to lower initial cost. In India, industry has already started producing these devices at an affordable price. These ventures have implications for the entire South Asian region especially for smaller countries where establishing a new plant may not be cost effective.
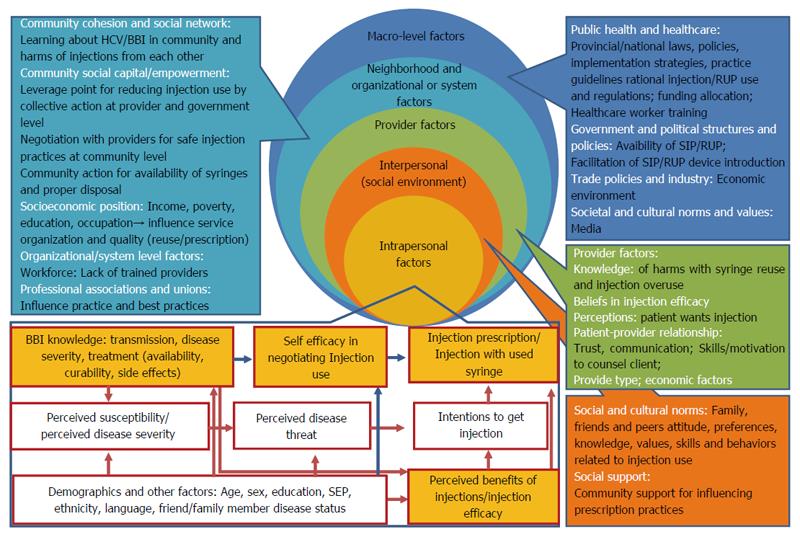
As highlighted above, injection use and safety is a complex issue and requires interventions at multiple levels and settings including individual patients, prescribers/providers, community, health system and broader policy level to have a major impact. We propose a framework based on social ecological model (SEM) and health belief model (HBM) to inform design of interventions targeting various components to promote rational injection use and eliminate reuse[62-64] (Figure 5). In this framework, the HBM is based on the understanding that at the individual level, a patient’s ability to avoid unnecessary and unsafe injections is based on the individual’s perceived susceptibility of getting an HCV/HIV infection, perceived severity, or his/her belief of how serious the consequences of getting this infection can be, the benefits of being able to avoid getting infected, the perceived barriers to being able to avoid unsafe and unnecessary injection, and self-efficacy in his/her abilities to negotiate with the provider to not administer unnecessary or unsafe injection with a used syringe. Self-efficacy is defined as people’s judgments of their capabilities to organize and execute a course of action required to attain designated types of performances[65]. Beliefs and behaviors, BBP knowledge, education, socioeconomic status and ethnicity influence beliefs on efficacy of injections and self-efficacy to negotiate injection prescription with a healthcare provider. Self-efficacy is an important factor for client/patient empowerment for demanding quality of care. To enhance self-efficacy to negotiate injection prescription, beliefs about injection efficacy have to be addressed. The SEM takes into account factors not just at the individual level, but also at interpersonal, community, organizational and policy levels that may impact prevalence of unnecessary or unsafe injection administration. For instance, at the interpersonal level, health care providers’ knowledge on harms related to reuse and rational prescription, beliefs on injection efficacy and patient expectation of an injection, communication skills, economic incentive and power imbalance play a major role in unnecessary injection prescription. Family and friends, and broader community also play a role in creating an environment for promoting injection safety. At the organization and community level, professional associations can influence safety of injections through creating code of conduct and standard of practice by their members at local level as was done in India. Community members together can negotiate and create a demand for safe injection practices. Finally, macro level factors including policies related to promotion and introduction of RUP injection devices, rational prescription guidelines, training of healthcare work force, and economic incentive for reuse prevention and sharp injury prevention devices could provide enabling environment.
In this paper, we included all available literature to synthesize evidence on injection practices in South Asia to provide a comprehensive picture. We did not rate quality of studies for methodological rigour. However, during evidence synthesis we commented on methodological quality and generalizability of studies.
In summary, although information is not available for all countries, injection use is common in South Asia with high levels of reuse of injection equipment and the potential to spread BBPs. Injections are prescribed and provided by qualified and unqualified practitioners mainly in the private sector. Practitioners mostly make decision for injection use although a small percentage of patients also prefer injections. Patient preference varies from one place to another and is higher in rural than urban areas. SEM model proposed above could guide design of multi- pronged interventions including: (1) introduction of RUP devices; (2) behavior change of the population through education, enhancement of self-efficacy of patients and community empowerment to negotiate injection prescription; and (3) behavior change of practitioners through focused IGDs, involvement of community and medical associations in promoting and endorsing safe injection practices.
Knowledge gaps still exist in assessing the magnitude of the problem of injection use in some countries in South Asia which could be bridged by including questions on injection use in demographic and health surveys (DHS). DHS will provide comparable data on injections at the national level to provide a baseline and to assess impact of interventions. Also, there is a need to develop and test new interventions for behavior change, to improve the currently known interventions and to test them in large scale public health programs. The impact of policy and regulation on the supply/availability of injection equipment, and other devices should also be documented. Greater collaboration among stakeholders could enhance achievement of safe injection practices in the region.
Although, hepatitis B and C are global concern, prevalence in South Asian countries is particularly high. Reuse of syringes for healthcare injections have been consistently shown to transmit hepatitis B and C.
This is the first paper to summarize evidence on injection use in South Asia. Overall, injection use is very common in South Asia with variation across countries (2.4-13.6 injections/person per year) with a varying proportion of injections being unsafe in recent studies (5%-50%). Studies to assess injection use are not available from Maldives and Bhutan. Injections are provided in formal and informal sectors, more so in the private than the public sector. Practitioners are the major driving force behind injection overuse, although patients from different parts of South Asia also prefer injections as a form of therapy.
Interventions aimed at patients, providers and health system such as availability of re-use prevention injection devices have shown to reduce the injection re-use and overuse.
Countries for which ample injection use data is available (India and Pakistan), have taken major steps towards promotion of safe injection practices. Hence the availability of data about unsafe injections plays an important role in mobilizing political will to reduce unsafe injection practices. The paucity of information in the region from rest of the countries demands an immediate assessment of injection safety to inform optimal response.
Re-use prevention injection devices are syringes that have mechanical mechanism to prevent reuse after a single use. Social ecological model is a theory-based framework that proposes that individual behaviour is shaped within the context of broader interpersonal, community, organization and policy environment.
To provide a context to readers, reviewers highlighted need for inclusion of data on hepatitis B and C prevalence and association between injection and transmission of hepatitis B virus and hepatitis C virus.
| 1. | Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61:S45-S57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1325] [Cited by in RCA: 1381] [Article Influence: 115.1] [Reference Citation Analysis (0)] |
| 2. | Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1770] [Cited by in RCA: 1854] [Article Influence: 142.6] [Reference Citation Analysis (3)] |
| 3. | Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015;386:1546-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1806] [Cited by in RCA: 2051] [Article Influence: 186.5] [Reference Citation Analysis (4)] |
| 4. | Qureshi H, Bile KM, Jooma R, Alam SE, Afridi HU. Prevalence of hepatitis B and C viral infections in Pakistan: findings of a national survey appealing for effective prevention and control measures. East Mediterr Health J. 2010;16 Suppl:S15-S23. [PubMed] |
| 5. | Razavi H. Polaris Observatory: Hepatitis C disease burden in India and Pakistan. : Centre for Data Analysis 2016; . |
| 6. | Khan AJ, Luby SP, Fikree F, Karim A, Obaid S, Dellawala S, Mirza S, Malik T, Fisher-Hoch S, McCormick JB. Unsafe injections and the transmission of hepatitis B and C in a periurban community in Pakistan. Bull World Health Organ. 2000;78:956-963. [PubMed] |
| 7. | Luby SP, Qamruddin K, Shah AA, Omair A, Pahsa O, Khan AJ, McCormick JB, Hoodbhouy F, Fisher-Hoch S. The relationship between therapeutic injections and high prevalence of hepatitis C infection in Hafizabad, Pakistan. Epidemiol Infect. 1997;119:349-356. [PubMed] |
| 8. | Singh J, Gupta S, Khare S, Bhatia R, Jain DC, Sokhey J. A severe and explosive outbreak of hepatitis B in a rural population in Sirsa district, Haryana, India: unnecessary therapeutic injections were a major risk factor. Epidemiol Infect. 2000;125:693-699. [PubMed] |
| 9. | Bari A, Akhtar S, Rahbar MH, Luby SP. Risk factors for hepatitis C virus infection in male adults in Rawalpindi-Islamabad, Pakistan. Trop Med Int Health. 2001;6:732-738. [PubMed] |
| 10. | Pasha O, Luby SP, Khan AJ, Shah SA, McCormick JB, Fisher-Hoch SP. Household members of hepatitis C virus-infected people in Hafizabad, Pakistan: infection by injections from health care providers. Epidemiol Infect. 1999;123:515-518. [PubMed] |
| 11. | Singh J, Bhatia R, Khare S, Patnaik SK, Biswas S, Lal S, Jain DC, Sokhey J. Community studies on prevalence of HBsAg in two urban populations of southern India. Indian Pediatr. 2000;37:149-152. [PubMed] |
| 12. | Singh J, Bhatia R, Patnaik SK, Khare S, Bora D, Jain DC, Sokhey J. Community studies on hepatitis B in Rajahmundry town of Andhra Pradesh, India, 1997-8: unnecessary therapeutic injections are a major risk factor. Epidemiol Infect. 2000;125:367-375. [PubMed] |
| 13. | Usman HR, Akhtar S, Rahbar MH, Hamid S, Moattar T, Luby SP. Injections in health care settings: a risk factor for acute hepatitis B virus infection in Karachi, Pakistan. Epidemiol Infect. 2003;130:293-300. [PubMed] |
| 14. | Reid S. Estimating the Burden of Disease from Unsafe Injections in India: A Cost-benefit Assessment of the Auto-disable Syringe in a Country with Low Blood-borne Virus Prevalence. Indian J Community Med. 2012;37:89-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Hauri AM, Armstrong GL, Hutin YJ. The global burden of disease attributable to contaminated injections given in health care settings. Int J STD AIDS. 2004;15:7-16. [PubMed] |
| 16. | Wyatt HV. The popularity of injections in the Third World: origins and consequences for poliomyelitis. Soc Sci Med. 1984;19:911-915. [PubMed] |
| 17. | Greenhalgh T. Drug prescription and self-medication in India: an exploratory survey. Soc Sci Med. 1987;25:307-318. [PubMed] |
| 18. | World Bank. World Development Indicators 2015. Washington, DC: World Bank 2015; . |
| 19. | Bhutta ZA, Gupta I, de'Silva H, Manandhar D, Awasthi S, Hossain SM, Salam MA. Maternal and child health: is South Asia ready for change? BMJ. 2004;328:816-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Hutin Y, Hauri A, Chiarello L, Catlin M, Stilwell B, Ghebrehiwet T, Garner J. Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Bull World Health Organ. 2003;81:491-500. [PubMed] |
| 21. | Hanson K, Berman P. Private health care provision in developing countries: a preliminary analysis of levels and composition. Health Policy Plan. 1998;13:195-211. [PubMed] |
| 22. | Raglow GJ, Luby SP, Nabi N. Therapeutic injections in Pakistan: from the patients' perspective. Trop Med Int Health. 2001;6:69-75. [PubMed] |
| 23. | Janjua NZ, Akhtar S, Hutin YJ. Injection use in two districts of Pakistan: implications for disease prevention. Int J Qual Health Care. 2005;17:401-408. [PubMed] |
| 24. | Pakistan Demographic and Health Survey 2012-13. Islamabad: National Institute of Population Studies (NIPS) and Macro International Inc. 2013; 1-366. |
| 25. | Yousafzai MT, Nisar N, Kakakhel MF, Qadri MH, Khalil R, Hazara SM. Injection practices among practitioners in private medical clinics of Karachi, Pakistan. East Mediterr Health J. 2013;19:570-575. [PubMed] |
| 26. | Janjua NZ, Akhtar S, Hutin YJ. Economic burden of unnecessary Injections in Pakistan. Proceedings of the AIDS 2006 - XVI International AIDS Conference; 2006 August 13, 2006; Toronto, Canada. Geneva: International AIDS Society 2006; TUPE0504. |
| 27. | Janjua NZ, Mahmood B, Imran Khan M. Does knowledge about bloodborne pathogens influence the reuse of medical injection syringes among women in Pakistan? J Infect Public Health. 2014;7:345-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Altaf A, Fatmi Z, Ajmal A, Hussain T, Qahir H, Agboatwalla M. Determinants of therapeutic injection overuse among communities in Sindh, Pakistan. J Ayub Med Coll Abbottabad. 2004;16:35-38. [PubMed] |
| 29. | Janjua NZ, Hutin YJ, Akhtar S, Ahmad K. Population beliefs about the efficacy of injections in Pakistan's Sindh province. Public Health. 2006;120:824-833. |
| 30. | Luby S, Hoodbhoy F, Jan A, Shah A, Hutin Y. Long-term improvement in unsafe injection practices following community intervention. Int J Infect Dis. 2005;9:52-59. [PubMed] |
| 31. | Ahmad K, Raza SA, Janjua NZ, Bin Hamza H, Khan MI. Interventions for improvement in unsafe injection practices in Pakistan. Int J Infect Dis. 2005;9:232-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Agboatwalla M, Hutin Y, Luby S, Mussarat A. A pilot intervention to improve injection practices in the informal private sector in Karachi, Pakistan. Abstract #AC 112. 2004;. |
| 33. | Altaf A, Shah SA, Shaikh K, Constable FM, Khamassi S. Lessons learned from a community based intervention to improve injection safety in Pakistan. BMC Res Notes. 2013;6:159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Kotwal A, Priya R, Thakur R, Gupta V, Kotwal J, Seth T. Injection practices in a metropolis of North India: perceptions, determinants and issues of safety. Indian J Med Sci. 2004;58:334-344. [PubMed] |
| 35. | Lakshman M, Nichter M. Contamination of medicine injection paraphernalia used by registered medical practitioners in south India: an ethnographic study. Soc Sci Med. 2000;51:11-28. [PubMed] |
| 36. | Murhekar MV, Murhekar KM, Arankalle VA, Sehgal SC. Epidemiology of hepatitis B infection among the Nicobarese--a mongoloid tribe of the Andaman and Nicobar Islands, India. Epidemiol Infect. 2002;128:465-471. [PubMed] |
| 37. | Rajasekaran M, Sivagnanam G, Thirumalaikolundusubramainan P, Namasivayam K, Ravindranath C. Injection practices in southern part of India. Public Health. 2003;117:208-213. [PubMed] |
| 38. | Anand K, Pandav CS, Kapoor SK. Injection use in a village in north India. Natl Med J India. 2001;14:143-144. [PubMed] |
| 39. | Kaipilyawar SB, Rao RG. Injection safety for immunisation--Andhra Pradesh experience. J Indian Med Assoc. 2005;103:222-225. [PubMed] |
| 40. | IPEN Study Group. Injection practices in India. WHO South-East Asia Journal of Public Health. 2012;1:189-200. |
| 41. | Kermode M, Muani V. Injection practices in the formal & amp; informal healthcare sectors in rural north India. Indian J Med Res. 2006;124:513-520. [PubMed] |
| 42. | Pandit NB, Choudhary SK. Unsafe injection practices in Gujarat, India. Singapore Med J. 2008;49:936-939. [PubMed] |
| 43. | Bhargo L, Tiwari R, Jain S, Yuwane P, Rajpoot MB, Tiwari S. A study to assess injection practices at different levels of health care facilities in district Gwalior, MP, India. Int Res Med Sci. 2014;2:1020-1025. |
| 44. | Garapati S, Peethala S. Assessment of knowledge and practices on injection safety among service providers in east Godavari district of Andhra Pradesh. Indian J Community Health. 2014;26:259-263. |
| 45. | Hadiyono JE, Suryawati S, Danu SS, Sunartono B. Interactional group discussion: results of a controlled trial using a behavioral intervention to reduce the use of injections in public health facilities. Soc Sci Med. 1996;42:1177-1183. [PubMed] |
| 46. | Hutin YJ. Acting upon evidence: progress towards the elimination of unsafe injection practices in India. Indian Pediatr. 2005;42:111-115. [PubMed] |
| 47. | Kamath SS. IAP Workshop on Safe Injection Practices: recommendations and IAP plan of action. Indian Pediatr. 2005;42:155-161. [PubMed] |
| 48. | Shankar U, Kanchan R. Model injection centre (MIC). J Indian Med Assoc. 2005;103:226-227. [PubMed] |
| 49. | National Centre for Disease Control. Handbook on safe injection practices New Delhi. India: National Centre for Disease Control (NCDC), Ministry of Health & Family Welfare 2014; . |
| 50. | Chowdhury AK, Roy T, Faroque AB, Bachar SC, Asaduzzaman M, Nasrin N, Akter N, Gazi HR, Lutful Kabir AK, Parvin M. A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health. 2011;11:779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 51. | Shill MC, Fahad MB, Sarker S, Dev S, Rufaka H K, D AK. Injection practices at primary healthcare units in bangladesh: experience at six upazilla health complexes. Australas Med J. 2011;4:26-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 52. | Gyawali S, Rathore DS, Shankar PR, Kumar VK, Maskey M, Jha N. Injection practice in Kaski district, Western Nepal: a community perspective. BMC Public Health. 2015;15:435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 53. | Bhattarai M, Wittet S. Perceptions about Injections and Private Sector Injection Practices in Central Nepal. : General Welfare Pratisthan and Gates Children¡¯s Vaccine Program at PATH 2000; . |
| 54. | Gyawali S, Rathore DS, Adhikari K, Shankar PR, K C VK, Basnet S. Pharmacy practice and injection use in community pharmacies in Pokhara city, Western Nepal. BMC Health Serv Res. 2014;14:190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 55. | Gunasekera HA, Sunil-Chandra NP, de Silva HJ. Low community seroprevalence of hepatitis C virus infection in the Gampaha district. Ceylon Med J. 2002;47:122. [PubMed] |
| 56. | Premawardhena AP, Premaratne R, Jayaweera G, Costa S, Chandrasena LG, de Silva HJ. Hepatitis B and C virus markers among new entrant medical students. Ceylon Med J. 1999;44:120-122. [PubMed] |
| 57. | Hsiao WC, Li K. A preliminary assessment of Sri Lanka's health sector and steps forward. : William Hsiao 2000; . |
| 58. | Attanayake N, Siyambalagoda L. An inquiry into the regulation of pharmaceuticals and medical practice in Sri Lanka. HEFP working paper 05/03. London, UK: London School of Hygiene and Tropical Medicine 2003; viii 70. |
| 59. | Rannan-Eliya RP, Jayawardhane P. Private primary care practitioners in Sri Lanka. : Health Policy Research in South Asia 2003; 279. |
| 60. | Janjua NZ, Khan MI, Usman HR, Azam I, Khalil M, Ahmad K. Pattern of health care utilization and determinants of care-seeking from GPs in two districts of Pakistan. Southeast Asian J Trop Med Public Health. 2006;37:1242-1253. [PubMed] |
| 61. | Bhunia R, Hutin Y, Ramkrishnan R, Ghosh PK, Dey S, Murhekar M. Reducing use of injections through interactional group discussions: a randomized controlled trial. Indian Pediatr. 2010;47:409-414. [PubMed] |
| 62. | Bronfenbrenner U. The ecology of human development: Experiments by design and nature. Cambridge, MA: Harvard University Press 1979; . |
| 63. | Janjua NZ, Razaq M, Chandir S, Rozi S, Mahmood B. Poor knowledge--predictor of nonadherence to universal precautions for blood borne pathogens at first level care facilities in Pakistan. BMC Infect Dis. 2007;7:81. [PubMed] |
| 64. | Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. Health behavior and health education: Theory, research, and practice. San Francisco: Jossey-Bass 2008; 465-486. |
| 65. | Bandura A. Self-efficacy. : Wiley Online Library 1994; . |
| 66. | Becker ML, Reza-Paul S, Ramesh B, Washington R, Moses S, Blanchard JF. Association between medical injections and HIV infection in a community-based study in India. AIDS. 2005;19:1334-1336. [PubMed] |
| 67. | Kermode M, Holmes W, Langkham B, Thomas MS, Gifford S. Safer injections, fewer infections: injection safety in rural north India. Trop Med Int Health. 2005;10:423-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 68. | Shah HD, Mangal AD, Solanki HR, Parmar DV. Unsafe injection practices: An occupational hazard for health care providers and a potential threat for community: A detailed study on injection practices of health care providers. IJHAS. 2014;3:28. |
| 69. | Bendale N, Bhatkule P. Assessment of injection safety practices in tertiary institute in Maharashtra, India. Int J Recent Trends Sci Technol. 2015;15:622-625. |
| 70. | Mantel C. Survey on the safety of injections in Pakistan. Assignment report, 17 May 2002. Islamabad: Ministry of Health, Govrnment of Pakistan 2002; . |
| 71. | Gibney L, Saquib N, Metzger J, Choudhury P, Siddiqui M, Hassan M. Human immunodeficiency virus, hepatitis B, C and D in Bangladesh’s trucking industry: prevalence and risk factors. Int J Epidemiol. 2001;30:878-884. [PubMed] |
Manuscript Source: Invited manuscript
Specialty Type: Gastroenterology and Hepatology
Country of Origin: Canada
Peer-Review Report Classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Abenavoli L, Lee HC, Said Z, Waheed Y S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH