Published online Jan 14, 2016. doi: 10.3748/wjg.v22.i2.718
Peer-review started: May 20, 2015
First decision: August 26, 2015
Revised: September 18, 2015
Accepted: November 9, 2015
Article in press: November 9, 2015
Published online: January 14, 2016
Processing time: 232 Days and 19 Hours
Relatively little is known about the oncologic safety of laparoscopic surgery for advanced rectal cancer. Recently, large randomized clinical trials showed that laparoscopic surgery was not inferior to open surgery, as evidenced by survival and local control rates. However, patients with T4 tumors were excluded from these trials. Technological advances in the instrumentation and techniques used by laparoscopic surgery have increased the use of laparoscopic surgery for advanced rectal cancer. High-definition, illuminated, and magnified images obtained by laparoscopy may enable more precise laparoscopic surgery than open techniques, even during extended surgery for T4 or locally recurrent rectal cancer. To date, the quality of evidence regarding the usefulness of laparoscopy for extended surgery beyond total mesorectal excision has been low because most studies have been uncontrolled series, with small sample sizes, and long-term data are lacking. Nevertheless, laparoscopic extended surgery for rectal cancer, when performed by specialized laparoscopic colorectal surgeons, has been reported safe in selected patients, with significant advantages, including a clear visual field and less blood loss. This review summarizes current knowledge on laparoscopic extended surgery beyond total mesorectal excision for primary or locally recurrent rectal cancer.
Core tip: Relatively little is known about the efficacy and safety of laparoscopic extended surgery beyond total mesorectal excision for primary or locally recurrent rectal cancer. However, some experienced surgeons have reported the usefulness of laparoscopic surgery for such challenging cases. This review summarizes current knowledge on laparoscopic extended surgery beyond total mesorectal excision.
- Citation: Akiyoshi T. Technical feasibility of laparoscopic extended surgery beyond total mesorectal excision for primary or recurrent rectal cancer. World J Gastroenterol 2016; 22(2): 718-726
- URL: https://www.wjgnet.com/1007-9327/full/v22/i2/718.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i2.718
Since its initial description[1], laparoscopic colon resection has become widely accepted as a minimally invasive procedure, with oncologic outcomes equivalent to those of open surgery. Moreover, laparoscopic surgery was found to have several advantages over open surgery, including reduced blood loss, earlier recovery of bowel movement, and shorter hospital stay[2-5]. Despite its widespread acceptance for colon cancer, laparoscopic rectal cancer surgery is still considered investigational, primarily because rectal cancer surgery is more technically demanding, being confined to the narrow bony pelvis. Moreover, the long-term oncologic outcomes after laparoscopic rectal cancer surgery remain unclear due to the lack of high-quality randomized controlled trials (RCTs). However, high-definition, illuminated, and magnified images of the pelvis obtained in patients undergoing laparoscopy are often superior to the images obtained in patients undergoing open surgery. The technological advances in instrumentation, advances in surgical techniques, and increased surgeon experience with laparoscopic rectal cancer surgery have made laparoscopy more precise and easier to perform, not only for total mesorectal excision (TME) but for more extended surgery beyond TME. This review summarizes current evidence about laparoscopic TME for advanced rectal cancer, as well as evaluating developments in laparoscopic surgery extended beyond TME.
Although many studies have reported that laparoscopic TME is feasible for advanced rectal cancer[6-10], this review focuses on three large multicenter RCTs: the United Kingdom Medical Research Council conventional vs laparoscopic assisted surgery in colorectal cancer (MRC CLASICC), the comparison of open vs laparoscopic surgery for mid and low rectal cancer after neoadjuvant chemoradiotherapy (COREAN), and the colorectal cancer laparoscopic or open resection (COLOR II).
The MRC CLASICC trial was the first multicenter large RCT to test laparoscopic surgery in patients with colorectal cancer[4]. Between 1996 and 2002, 794 patients were randomized 2:1 to laparoscopic or open surgery, including 381 rectal cancer patients, 253 who underwent laparoscopic and 128 who underwent open surgery. Although the rate of positive circumferential resection margin was higher in patients who underwent laparoscopic than conventional anterior resection (12% vs 6%)[4], the 3- and 5-year overall survival (OS), disease-free survival (DFS), and local recurrence (LR) rates were similar in the two groups[5,11]. Long-term follow-up over 10 years confirmed that laparoscopic surgery should be the treatment option for patients with rectal cancer because these patients benefited from earlier functional recovery with similar long-term outcomes[12]. Interestingly, early survival tended to be improved in patients who underwent laparoscopic surgery. One of the criticisms of the CLASICC trial was that it involved surgeons who were first learning the laparoscopic technique, as evidenced by the high conversion rate to open surgery (34%)[4].
The next multicenter RCT was the COREAN trial, in which 340 patients with cT3N0-2 mid or low rectal cancer ≤ 9 cm from the anal verge who received neoadjuvant chemoradiotherapy were randomized 1:1 to laparoscopic or open surgery between 2006 and 2009[13]. Laparoscopic surgery was associated with reduced blood loss (200 mL vs 217.5 mL), earlier recovery of bowel movement, and lower morphine use, but also with longer operative time (245 min vs 197 min). Positive circumferential resection margin (2.9% vs 4.1%), macroscopic quality of the TME specimen, number of retrieved lymph nodes (17 vs 18), and postoperative complication (21.2% vs 23.5%) did not differ significantly in the two groups. Notably, only two patients (1.2%) were converted to open surgery, a much lower rate than in the CLASICC trial. This low conversion rate may have been due to the performance of surgery by seven specialized surgeons at three hospitals. Later, laparoscopic surgery was shown to be non-inferior oncologically to open surgery, as determined by their 3-year OS (91.7% vs 90.4%), DFS (79.2% vs 72.5%), and LR (2.6% vs 4.9%) rates[14].
The COLOR II trial is the largest such RCT performed to date, in which 1103 patients with rectal cancer ≤ 15 cm from the anal verge who were treated at 30 centers and hospitals in 8 countries, were randomized 2:1 to laparoscopic or open surgery between 2004 and 2010[14]. Of the 1044 available patients, 699 were randomized to laparoscopic and 345 to open surgery, with similar proportions of these patients receiving preoperative radiotherapy (59% vs 58%). Laparoscopic surgery was associated with significantly reduced blood loss (200 mL vs 400 mL), earlier recovery of bowel movement (2.0 d vs 3.0 d) and shorter hospital stay (8.0 d vs 9.0 d), although it was also significantly associated with longer operative time (240 min vs 188 min), than open surgery. Positive circumferential resection margin (< 2 mm) (10% vs 10%), mean tumor distance to the distal resection margin (3.0 cm vs 3.0 cm), macroscopic completeness of the TME specimen (88% vs 92%), and perioperative morbidity (40% vs 37%) did not differ significantly. The conversion rate was 16%, lower than in the CLASICC trial but higher than in the COREAN trial. Importantly, the percentage of patients with lower rectal cancers ≤ 5 cm from the anal verge and positive circumferential resection margins was significantly lower with laparoscopic than with open surgery (9% vs 22%). This lower rate may have been due to better visualization of the lower pelvic cavity by the laparoscope, providing a well illuminated and magnified image deep in the pelvis and making it easier to perform precise dissection. Long-term survival outcomes in this trial were recently reported, with laparoscopic and open surgery resulting in similar 3-year OS (86.7% vs 83.6%), DFS (74.8% vs 70.8%), and LR (5.0% vs 5.0%) rates[15]. Interestingly, the lower rate of positive circumferential resection margin after laparoscopic surgery for lower rectal cancer was associated with a lower LR rate (4.4% vs 11.7%).
Analysis of the MRC CLASICC trial showed that intraoperative conversions were more likely in rectal cancer patients and in patients having tumors with greater local spread[16]. Patients with cT4 tumors were excluded from the COREAN trial because laparoscopic surgery may be oncologically unsafe for patients with these lesions[13]. The COLOR II trial excluded not only patients with cT4 tumors, but those with cT3 tumors ≤ 2 mm from the endopelvic fascia[14]. A large ongoing RCT in the United States, the American College of Surgeons Oncology Group (ACOSOG)-Z6051 trial, comparing laparoscopic with open surgery for rectal cancers ≤ 12 cm from the anal verge following 5FU based neoadjuvant chemotherapy/radiation therapy, has also excluded patients with T4 tumors[17].
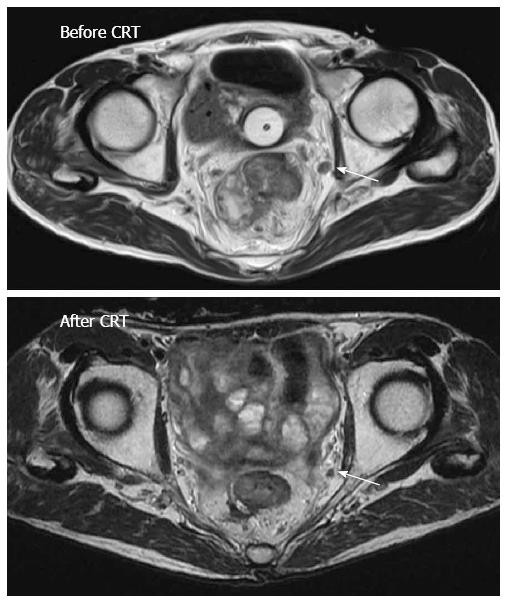
Lateral pelvic lymph node (LPLN) metastasis has been reported in approximately 15%-20% of Japanese patients with advanced low rectal cancer below the peritoneal reflection[18-20]. The Japanese Society for Cancer of the Colon and Rectum guidelines for the treatment of colorectal cancer recommend LPLN dissection (LPLD) for T3/T4 low rectal cancers below the peritoneal reflection[21]. Although LPLD is frequently performed in Japan, it is regarded as futile in western countries because LPLN metastasis is considered not amenable to surgical cure, with preoperative chemoradiotherapy considered the treatment of choice[22]. A recent study, however, showed that preoperative chemoradiotherapy alone could not eradicate LPLN metastases[23], and that LPLN recurrence is common after TME without LPLD following chemoradiotherapy[24]. Therefore, LPLD is considered useful for selected patients with clinically suspected LPLN metastasis, even after preoperative chemoradiotherapy (Figure 1).
Several studies from Asian countries have reported the short-term outcomes of patients undergoing laparoscopic (including robotic) LPLD for rectal cancer since 2011 (Table 1)[25-32]. The first published retrospective study, involving 34 rectal cancer patients who received neoadjuvant chemoradiotherapy, found that laparoscopic LPLD was technically safe and feasible, although 71% of patients were positive for LPLN metastasis after laparoscopic LPLD[25]. Two other studies reported that > 50% of patients were positive for LPLN metastasis after laparoscopic LPLD[26,27], although other studies have reported lower percentages[28-32]. These differences among studies in the percentage of patients with metastatic LPLN may have been due to differences in indications for LPLD. In Japan, patients not treated with preoperative chemoradiotherapy and without clinically swollen LPLNs frequently receive prophylactic LPLD. Owing to the limited number of patients who underwent laparoscopic LPLD, there are limited objective data showing the superiority of laparoscopic compared with open LPLD or on long-term outcomes after laparoscopic LPLD. However, median blood loss (25-380 mL) reported in the studies of laparoscopic LPLD[25-32] was considerably lower than that (576 mL) reported by JCOG0212[33], in which 351 patients with clinical stage II/III low rectal cancer without LPLN enlargement underwent open TME plus bilateral prophylactic LPLD. Together with the 0% conversion rates reported in studies of laparoscopic LPLD[26,27,30,31], these findings suggest that laparoscopic LPLD is a technically safe and feasible procedure, at least when performed by experienced laparoscopic surgeons specializing in pelvic surgery.
| Study | Year | No. of patients | Preoperative chemoradio-therapy | Median operative time, min (range) | Median blood loss, mL (range) | Median number of retrieved lateral lymph nodes (range) | Percent with positive lateral pelvic lymph nodes | Percent converted to open surgery | Overall morbidity rate |
| Liang et al[25] | 2011 | 34 | 100% | 58 (42-94) for unilateral LPLD | 44 (20-240) for unilateral LPLD | 6 (2-14) | 71% | NR | 21% |
| Konishi et al[26] | 2011 | 14 | 100% | 413 (277-596) | 25 (5-1190) | 23 (14-33)2 | 57% | 0% | 36% |
| Park et al[27] | 2011 | 163 | 56% | 310 (220-510)1 | 188 (50-370)1 | 9 (3-19) | 56% | 0% | 31% |
| Liu et al[28] | 2011 | 68 | NR | 271 (SD 31)1 | 150 (SD 50)1 | 2312 | 7% | NR | 7% |
| Obara et al[29] | 2012 | 12 | 0% | 678 (556-778) | 155 (10-613) | 17 | 8% | NR | NR |
| Bae et al[30] | 2014 | 214 | 86% | 396 (170-581) | 200 (50-700) | 7 (2-23) | 0% | 0% | 29% |
| Furuhata et al[31] | 2014 | 18 | 0% | 604 (473-746)1 | 380 (10-930)1 | 17 (7-27)1 | 28% | 0% | 17% |
| Kagawa et al[32] | 2015 | 505 | 12% | 476 (320-683) | 27 (5-690) | 19 (5-47) | 20% | 0% | 14% |
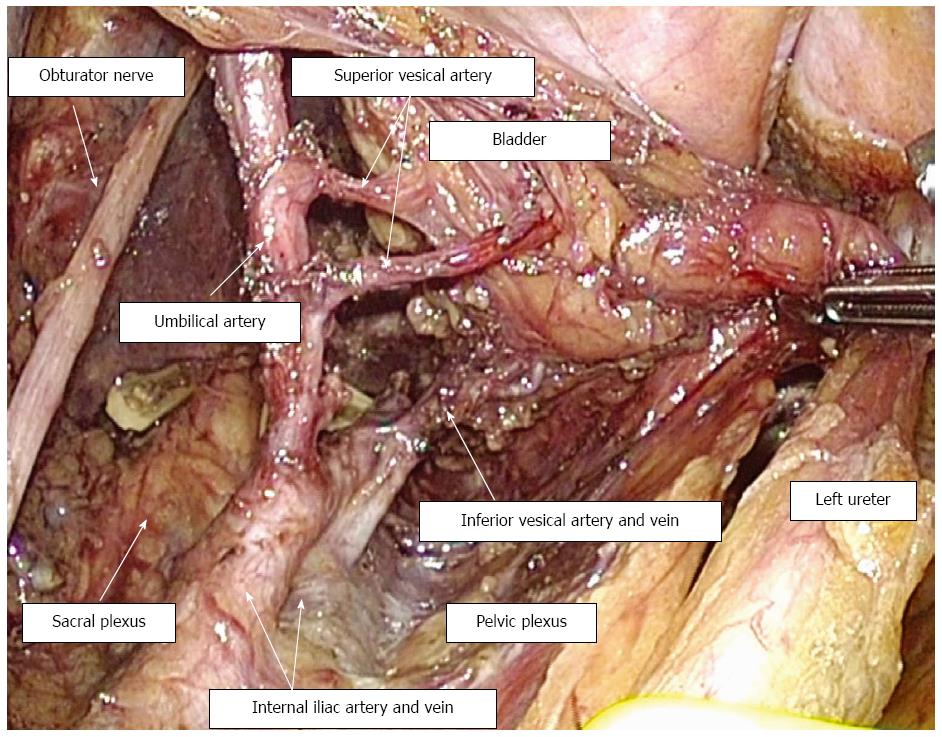
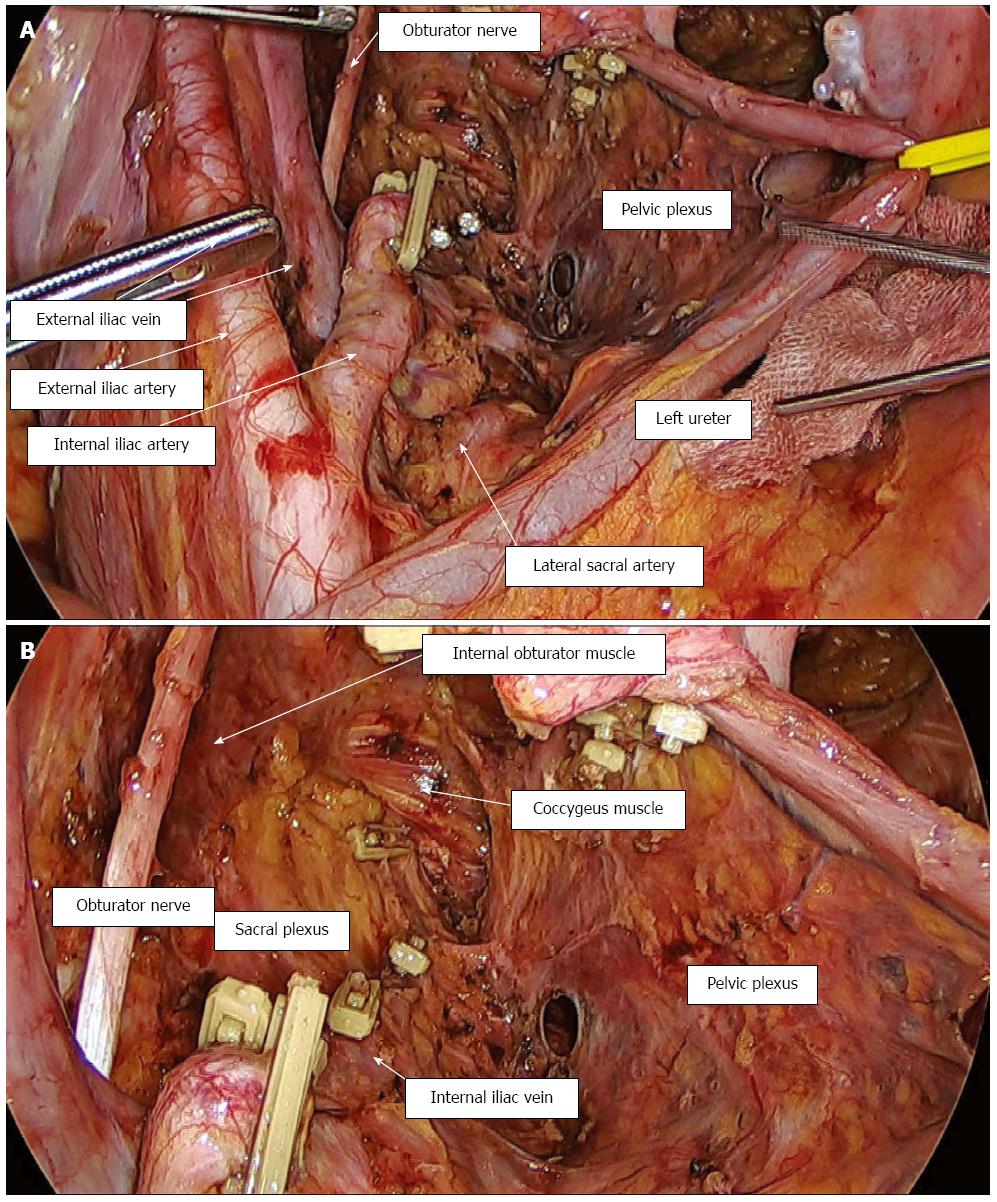
To date, over 100 patients at our institution have undergone laparoscopic LPLD for primary rectal cancer. LPLN metastasis most frequently occurs around the distal internal iliac vessels[18]. Because the operative field of LPLD, especially around these distal internal iliac vessels, is located very deep in the pelvic space, the magnified and illuminated vision provided by laparoscopy is clearer than that of open surgery (Figures 2 and 3). Therefore, laparoscopic LPLD, when performed by surgeons with sufficient knowledge of the lateral pelvic anatomy and sufficient experience with laparoscopic TME, might result in more meticulous dissection with less blood loss than open surgery. Recent high-definition videos of laparoscopic LPLD performed by experts have enhanced the understanding by many Japanese surgeons of the anatomy of the lateral pelvic area.
Robotic LPLD has been reported feasible for rectal cancer[30,32,34]. There are some technical advantages to robotic surgery over conventional laparoscopy, including increased operability of instruments, elimination of tremor, and a 3-dimensional high definition image. Although LPLD is rarely performed by colorectal surgeons in the United States, LPLD is routinely performed by urologists during robotic-assisted cystoprostatectomy[35]. Use of a robotic approach may therefore increase the number of LPLDs performed by multidisciplinary teams in western countries[35].
Few studies to date have focused on laparoscopic surgery for rectal cancer invading adjacent organs. One analysis assessed 39 patients undergoing laparoscopic surgery for colorectal cancer with suspected involvement of another organ, including 12 patients undergoing rectal cancer resection[36]. The conversion and R0 resection rates in these 12 rectal cancer patients were 16% and 75%, respectively. Another study compared outcomes in 38 patients undergoing laparoscopic and 16 undergoing open multivisceral colorectal cancer resection[37]. Of the 22 patients undergoing multivisceral rectal cancer resection, 19 (86%) underwent laparoscopic surgery, with none requiring conversion to open surgery, suggesting that laparoscopic multivisceral resection may be more feasible in patients with rectal than with colon cancer. A study from our institution comparing 60 laparoscopic and 66 open multivisceral colorectal cancer resections found that the conversion and R0 rates in the 21 patients undergoing laparoscopic multivisceral rectal cancer resection were 4.8% and 90%, respectively[38]. Although these studies regarding laparoscopic multivisceral colorectal cancer resection[36-38] did not include patients requiring laparoscopic pelvic exenteration, en bloc partial resection of the vagina, prostate, or pelvic floor muscle can be performed relatively easily under direct vision during the perineal phase of laparoscopic abdominoperineal resection.
Abdominosacral resection is necessary for patients with rectal cancer involving the presacral fascia and sacral bone. Laparoscopic abdominosacral resection for primary rectal cancer was first reported successful in three patients[39]. Sacrectomy was low (below the level of S3/4) in all three patients and was performed after patients were turned to the prone position. A finger placed in the presacral space above the tumor was used as a guide. R0 resections were achieved in all three patients. Laparoscopic abdominosacral resection was also reported successful for primary rectal cancer patients with negative circumferential resection margins[40,41]. Laparoscopic methods may be suitable for abdominosacral resection with low sacrectomy because sacrectomy, which itself has excellent access, can be performed through a posterior approach in the prone position. Although it is necessary to assess the long-term oncological outcomes of laparoscopic multivisceral rectal cancer resection, laparoscopic surgery may be suitable for selected patients with rectal cancers invading adjacent organs.
Surgery for locally recurrent rectal cancer can vary greatly, depending on the site of local recurrence and its relationship to adjacent structures. Moreover, these operations are often technically challenging owing to the strong fibrosis and altered anatomy around the tumor. Although few reports have assessed the usefulness of laparoscopy for locally recurrent rectal cancer, a study of seven patients undergoing laparoscopic salvage surgery for locally recurrent rectal cancer included three patients who underwent anterior resection and one each who underwent abdominoperineal resection, posterior exenteration, and proctocolectomy[42]. Their mean blood loss was 200 mL, and all patients underwent R0 resection. Laparoscopic salvage abdominoperineal resection with en bloc vaginal resection was reported successful for recurrence at an anastomotic site after laparoscopic low anterior resection[43]. A comparison of laparoscopic and open surgery for recurrent or metachronous colorectal cancer included three patients with anastomotic site recurrence and two with LPLN recurrence undergoing laparoscopic surgery[44]. Although the two patients with LPLN recurrence were converted to open surgery, mainly due to widespread adhesions and ambiguous tissue planes around the tumor, all patients undergoing laparoscopic surgery for locally recurrent rectal cancer underwent R0 resection, indicating that laparoscopic surgery was feasible in these patients. A study comparing 13 patients undergoing laparoscopic surgery and 17 undergoing open surgery for locally recurrent rectal cancer at the anastomotic site or LPLNs found that operating time was longer (381 mL vs 241 mL), but blood loss smaller (110 mL vs 450 mL) for laparoscopic surgery[45]. The conversion and R0 resection rates for laparoscopic surgery were 7.7% and 100%, respectively. The percentage of postoperative complications was similar (30.8% vs 23.5%), and gastrointestinal recovery was significantly faster following laparoscopic than open surgery. Although these studies did not include more extended surgery such as total pelvic exenteration (TPE), they suggested that laparoscopic surgery for locally recurrent rectal cancer could be safely performed in selected patients, with significantly reduced blood loss and faster gastrointestinal recovery.
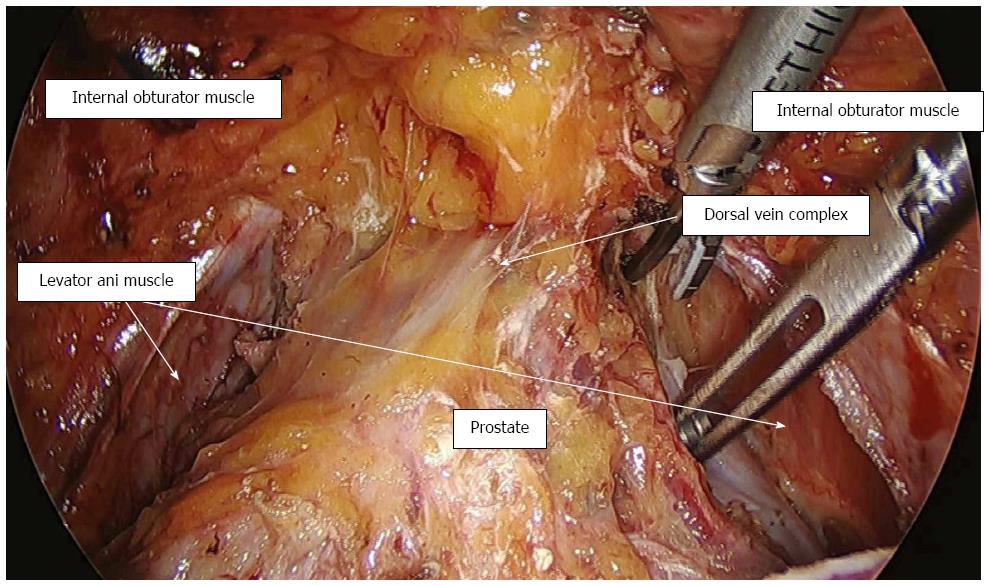
LPLD is considered indispensable for extended surgery “beyond” TME, such as pelvic exenteration, regardless of whether surgery is open or laparoscopic. However, the introduction of laparoscopic LPLD has enabled laparoscopic pelvic exenteration, involving dissection of the lateral pelvic space beyond the layer of the TME. Laparoscopy can be used to dissect the Retzius space and paravesical space with good visualization (Figure 4), with the layer of retro-rectal dissection basically the same as in TME. The first reported successful laparoscopic TPE with en bloc LPLD for primary rectal cancer involved division of the dorsal vein complex under direct vision after changing the patient to a prone position[46]. This was followed by successful laparoscopic TPE for locally recurrent rectal cancer[47]. Laparoscopic pelvic exenteration has the advantages of precise dissection and blood loss < 1000 mL, with a very clear view of the operative field. A recent study compared short-term outcomes of laparoscopic pelvic exenteration (n = 9) with open pelvic exenteration (n = 58) for pelvic malignancies, which included 13 patients with malignancies other than primary or locally recurrent rectal cancer[48]. The dorsal vein complex was clipped and divided using bipolar soft-coagulation of a VIO system. Intraoperative blood loss was significantly lower in patients who underwent laparoscopic than open pelvic exenteration (830 mL vs 2769 mL), although the operative time (935 min vs 883 min) and R0 resection rate (77.8% vs 75.9%) were similar. Importantly, overall rates of any complication (66.7% vs 89.7%) and major complications (0% vs 32.8%) were lower in the laparoscopic surgery group, although differences were not significant. In another case series, three patients underwent robotic pelvic exenteration for primary rectal cancer, including one who underwent en bloc resection of the prostate with a coloanal anastomosis and robotically performed vesico-urethral anastomosis[49]. Because laparoscopic vesico-urethral anastomosis is technically demanding, a robotic system might be especially useful for pelvic exenteration requiring vesico-urethral anastomosis.
Improvements in instrumentation have yielded high-definition laparoscopic images of the pelvic cavity, enhancing knowledge of the precise pelvic anatomy beyond the TME. These advances have enabled laparoscopic extended surgery for rectal cancer to be performed safely by specialized laparoscopic surgeons who can use the oncologically safe outer layer beyond the TME. However, additional studies are necessary to evaluate the long-term oncologic safety of laparoscopic extended surgery beyond the TME.
| 1. | Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144-150. [PubMed] |
| 2. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2541] [Article Influence: 115.5] [Reference Citation Analysis (0)] |
| 3. | Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 965] [Cited by in RCA: 1076] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 4. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2325] [Article Influence: 110.7] [Reference Citation Analysis (0)] |
| 5. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1121] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 6. | Denost Q, Adam JP, Pontallier A, Celerier B, Laurent C, Rullier E. Laparoscopic total mesorectal excision with coloanal anastomosis for rectal cancer. Ann Surg. 2015;261:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Lujan J, Valero G, Biondo S, Espin E, Parrilla P, Ortiz H. Laparoscopic versus open surgery for rectal cancer: results of a prospective multicentre analysis of 4,970 patients. Surg Endosc. 2013;27:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD. Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg. 2011;212:844-854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Penninckx F, Kartheuser A, Van de Stadt J, Pattyn P, Mansvelt B, Bertrand C, Van Eycken E, Jegou D, Fieuws S. Outcome following laparoscopic and open total mesorectal excision for rectal cancer. Br J Surg. 2013;100:1368-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (3)] |
| 10. | Kuroyanagi H, Akiyoshi T, Oya M, Fujimoto Y, Ueno M, Yamaguchi T, Muto T. Laparoscopic-assisted anterior resection with double-stapling technique anastomosis: safe and feasible for lower rectal cancer? Surg Endosc. 2009;23:2197-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 830] [Cited by in RCA: 748] [Article Influence: 46.8] [Reference Citation Analysis (2)] |
| 12. | Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 505] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 13. | Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010;11:637-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 687] [Cited by in RCA: 768] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 14. | van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1030] [Cited by in RCA: 1249] [Article Influence: 96.1] [Reference Citation Analysis (1)] |
| 15. | Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372:1324-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 864] [Cited by in RCA: 962] [Article Influence: 87.5] [Reference Citation Analysis (0)] |
| 16. | Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J, Brown JM. Patient factors influencing conversion from laparoscopically assisted to open surgery for colorectal cancer. Br J Surg. 2008;95:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Nandakumar G, Fleshman JW. Laparoscopy for rectal cancer. Surg Oncol Clin N Am. 2010;19:793-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Akiyoshi T, Watanabe T, Miyata S, Kotake K, Muto T, Sugihara K. Results of a Japanese nationwide multi-institutional study on lateral pelvic lymph node metastasis in low rectal cancer: is it regional or distant disease? Ann Surg. 2012;255:1129-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 223] [Article Influence: 15.9] [Reference Citation Analysis (1)] |
| 19. | Sugihara K, Kobayashi H, Kato T, Mori T, Mochizuki H, Kameoka S, Shirouzu K, Muto T. Indication and benefit of pelvic sidewall dissection for rectal cancer. Dis Colon Rectum. 2006;49:1663-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 344] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 20. | Ueno M, Oya M, Azekura K, Yamaguchi T, Muto T. Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg. 2005;92:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 264] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 21. | Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H. Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015;20:207-239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 451] [Cited by in RCA: 498] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 22. | Moran B. Exploring the limits in low rectal cancer. Lancet Oncol. 2012;13:565-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Unno T, Kano A, Kuroyanagi H. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 219] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 24. | Kim MJ, Kim TH, Kim DY, Kim SY, Baek JY, Chang HJ, Park SC, Park JW, Oh JH. Can chemoradiation allow for omission of lateral pelvic node dissection for locally advanced rectal cancer? J Surg Oncol. 2015;111:459-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 123] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 25. | Liang JT. Technical feasibility of laparoscopic lateral pelvic lymph node dissection for patients with low rectal cancer after concurrent chemoradiation therapy. Ann Surg Oncol. 2011;18:153-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 26. | Konishi T, Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Akiyoshi T, Yoshimatsu H, Watanabe T, Yamaguchi T, Muto T. Multimedia article. Lateral lymph node dissection with preoperative chemoradiation for locally advanced lower rectal cancer through a laparoscopic approach. Surg Endosc. 2011;25:2358-2359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 27. | Park JS, Choi GS, Lim KH, Jang YS, Kim HJ, Park SY, Jun SH. Laparoscopic extended lateral pelvic node dissection following total mesorectal excision for advanced rectal cancer: initial clinical experience. Surg Endosc. 2011;25:3322-3329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Liu T, Zhang C, Yu P, Chen J, Zeng D, Gan L, Lv W, Liu L, Yan X. Laparoscopic radical correction combined with extensive lymphadenectomy and pelvic autonomic nerve preservation for mid-to-low rectal cancer. Clin Colorectal Cancer. 2011;10:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Obara S, Koyama F, Nakagawa T, Nakamura S, Ueda T, Nishigori N, Inoue T, Kawasaki K, Nakamoto T, Fujii H. Laparoscopic lateral pelvic lymph node dissection for lower rectal cancer: initial clinical experiences with prophylactic dissection. Gan To Kagaku Ryoho. 2012;39:2173-2175. [PubMed] |
| 30. | Bae SU, Saklani AP, Hur H, Min BS, Baik SH, Lee KY, Kim NK. Robotic and laparoscopic pelvic lymph node dissection for rectal cancer: short-term outcomes of 21 consecutive series. Ann Surg Treat Res. 2014;86:76-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Furuhata T, Okita K, Nishidate T, Ito T, Yamaguchi H, Ueki T, Akizuki E, Meguro M, Ogawa T, Kukita K. Clinical feasibility of laparoscopic lateral pelvic lymph node dissection following total mesorectal excision for advanced rectal cancer. Surg Today. 2015;45:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 32. | Kagawa H, Kinugasa Y, Shiomi A, Yamaguchi T, Tsukamoto S, Tomioka H, Yamakawa Y, Sato S. Robotic-assisted lateral lymph node dissection for lower rectal cancer: short-term outcomes in 50 consecutive patients. Surg Endosc. 2015;29:995-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 33. | Fujita S, Akasu T, Mizusawa J, Saito N, Kinugasa Y, Kanemitsu Y, Ohue M, Fujii S, Shiozawa M, Yamaguchi T. Postoperative morbidity and mortality after mesorectal excision with and without lateral lymph node dissection for clinical stage II or stage III lower rectal cancer (JCOG0212): results from a multicentre, randomised controlled, non-inferiority trial. Lancet Oncol. 2012;13:616-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 273] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 34. | Park JA, Choi GS, Park JS, Park SY. Initial clinical experience with robotic lateral pelvic lymph node dissection for advanced rectal cancer. J Korean Soc Coloproctol. 2012;28:265-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Kasten KR, Joseph JV, Francone TD. Robotic-assisted abdominoperineal resection with obturator lymph node dissection: a multidisciplinary approach. Dis Colon Rectum. 2014;57:1329-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Bretagnol F, Dedieu A, Zappa M, Guedj N, Ferron M, Panis Y. T4 colorectal cancer: is laparoscopic resection contraindicated? Colorectal Dis. 2011;13:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Kim KY, Hwang DW, Park YK, Lee HS. A single surgeon’s experience with 54 consecutive cases of multivisceral resection for locally advanced primary colorectal cancer: can the laparoscopic approach be performed safely? Surg Endosc. 2012;26:493-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 38. | Nagasue Y, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Nagasaki T, Nagata J, Mukai T. Laparoscopic versus open multivisceral resection for primary colorectal cancer: comparison of perioperative outcomes. J Gastrointest Surg. 2013;17:1299-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Williams GL, Gonsalves S, Bandyopadhyay D, Sagar PM. Laparoscopic abdominosacral composite resection for locally advanced primary rectal cancer. Tech Coloproctol. 2008;12:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Lengyel J, Sagar PM, Morrison C, Gonsalves S, Lee P, Phillips N. Multimedia article. Laparoscopic abdominosacral composite resection. Dis Colon Rectum. 2009;52:1662-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 41. | Nagasaki T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Yamaguchi T. Laparoscopic abdominosacral resection for locally advanced primary rectal cancer after treatment with mFOLFOX6 plus bevacizumab, followed by preoperative chemoradiotherapy. Asian J Endosc Surg. 2014;7:52-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Lu AG, Wang ML, Hu WG, Li JW, Zang L, Mao ZH, Dong F, Feng B, Ma JJ, Zong YP. [Experience of laparoscopic salvage surgery for locally recurrent rectal cancer]. Zhonghua Waike Zazhi. 2006;44:597-599. [PubMed] |
| 43. | Kim SH, Neve RS, Joh YG. Multimedia article. Relaparoscopy for salvage surgery in anastomotic recurrence of rectal cancer: feasible and safe. Dis Colon Rectum. 2008;51:1712-1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 44. | Park SY, Choi GS, Jun SH, Park JS, Kim HJ. Laparoscopic salvage surgery for recurrent and metachronous colorectal cancer: 15 years’ experience in a single center. Surg Endosc. 2011;25:3551-3558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 45. | Nagasaki T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Yamaguchi T. Laparoscopic salvage surgery for locally recurrent rectal cancer. J Gastrointest Surg. 2014;18:1319-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Mukai T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Ikeda A, Yamaguchi T. Laparoscopic total pelvic exenteration with en bloc lateral lymph node dissection after neoadjuvant chemoradiotherapy for advanced primary rectal cancer. Asian J Endosc Surg. 2013;6:314-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Akiyoshi T, Nagasaki T, Ueno M. Laparoscopic Total Pelvic Exenteration for Locally Recurrent Rectal Cancer. Ann Surg Oncol. 2015;22:3896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Uehara K, Nakamura H, Yoshino Y, Arimoto A, Kato T, Yokoyama Y, Ebata T, Nagino M. Initial experience of laparoscopic pelvic exenteration and comparison with conventional open surgery. Surg Endosc. 2015;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 49. | Shin JW, Kim J, Kwak JM, Hara M, Cheon J, Kang SH, Kang SG, Stevenson AR, Coughlin G, Kim SH. First report: Robotic pelvic exenteration for locally advanced rectal cancer. Colorectal Dis. 2014;16:O9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Contul RB, Ruiz MG, Santoro GA S- Editor: Gong ZM L- Editor: A E- Editor: Liu XM