Published online Mar 28, 2016. doi: 10.3748/wjg.v22.i12.3502
Peer-review started: November 13, 2015
First decision: November 27, 2015
Revised: December 9, 2015
Accepted: December 30, 2015
Article in press: December 30, 2015
Published online: March 28, 2016
Processing time: 131 Days and 8.6 Hours
Cholesterol crystal embolization (CCE) is a rare systemic embolism caused by formation of cholesterol crystals from atherosclerotic plaques. CCE usually occurs during vascular manipulation, such as vascular surgery or endovascular catheter manipulation, or due to anticoagulation or thrombolytic therapy. We report a rare case of intestinal obstruction caused by spontaneous CCE. An 81-year-old man with a history of hypertension was admitted for complaints of abdominal pain, bloating, and anorexia persisting for 4 mo. An abdominal computed tomography revealed intestinal ileus. His symptoms were immediately relieved by an ileus tube insertion, and he was discharged 6 d later. However, these symptoms immediately reappeared and persisted, and partial resection of the small intestine was performed. A histopathological examination indicated that small intestine obstruction was caused by CCE. At the 12-mo follow-up, the patient showed no evidence of CCE recurrence. Thus, in cases of intestinal obstruction, CCE should also be considered.
Core tip: Cholesterol crystal embolization (CCE) is a rare systemic embolism caused by formation of cholesterol crystals from atherosclerotic plaques. This case report details a rare case that was not only a spontaneous occurrence but also caused a focal intestinal lesion. CCE usually carries a serious prognosis, but this case had a good prognosis.
- Citation: Azuma S, Ikenouchi M, Akamatsu T, Seta T, Urai S, Uenoyama Y, Yamashita Y. Ileus caused by cholesterol crystal embolization: A case report. World J Gastroenterol 2016; 22(12): 3502-3505
- URL: https://www.wjgnet.com/1007-9327/full/v22/i12/3502.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i12.3502
Cholesterol crystal embolization (CCE) is a rare systemic embolism caused by occlusion of the peripheral arteries by cholesterol crystals from atherosclerotic plaques and may show multiorgan involvement, leading to renal failure, cutaneous manifestations, and gastrointestinal disease. CCE is usually an iatrogenic event occurring either after vascular surgery or endovascular catheter manipulations, or in the course of anticoagulation or thrombolytic therapy. Here, we report a rare case of intestinal obstruction caused by CCE in the absence of any causative medication. To our knowledge, this is the first reported case of single intestinal obstruction caused by CCE.
An 81-year-old man with a clinical history of hypertension, benign prostatic hyperplasia, pulmonary tuberculosis, and an oropharyngeal benign tumor was admitted to the hospital for complaints of abdominal pain, bloating, and anorexia persisting for the past 4 mo. Physical examination revealed severe abdominal distension. Chemical laboratory examination showed a slightly elevated white blood cell count (9100/μL; normal, 4000-7000/μL), a high serum creatinine level (1.21 mg/dL; normal, 0.60-1.10 mg/dL), and a low eosinophil value (1.3%; normal, 2.0%-4.0%). An abdominal computed tomography scan revealed focal thickening of the wall of the small intestine, intestinal dilatation of the oral intestine, and intraperitoneal lymphadenopathy (Figure 1). We diagnosed his condition as small intestinal obstruction and prioritized conservative treatment. We promptly inserted an ileus tube, owing to which, the abdominal symptoms alleviated rapidly. Contrast-enhanced imaging of the ileus tube showed that the tube had advanced beyond the lesion site on the third day of admission, and therefore, the patient was discharged on the sixth day of admission. However, his symptoms reappeared immediately after discharge, and he was readmitted to the hospital. An abdominal computed tomography scan at this point revealed focal thickening of the wall of the small intestine, similar to that seen earlier.
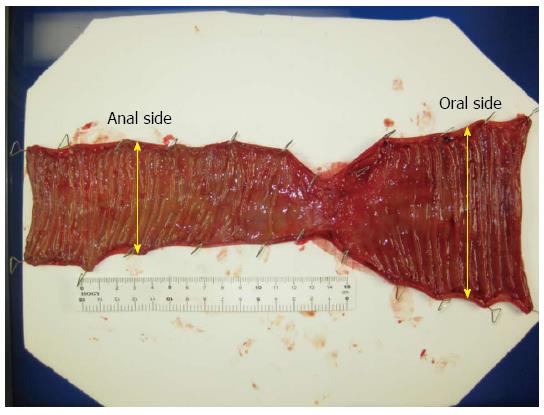
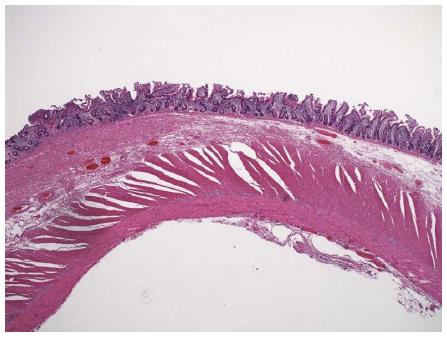
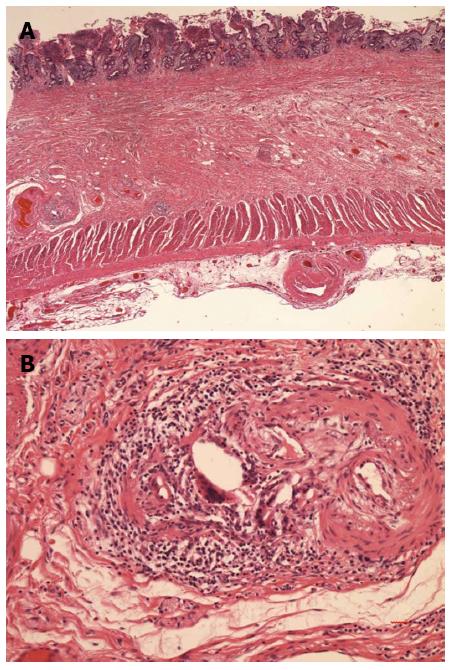
A double-balloon endoscopy of the small intestine was considered at this point; however, it was not performed owing to the presence of severe abdominal bloating. Ultimately, surgery was performed considering the possibility of small intestine cancer. Laparotomy showed a 5-6 cm tumor that had formed at a distance of 220 cm from the Treitz ligament and 180 cm from the terminal ileum. The small intestine has a 1.5-fold bigger lumen on the oral side than on the anal side. The tumor was resected from both the oral and anus sides to ensure a margin of 10 cm. We performed the vertical incision at the mesenteric contralateral anal side of the small intestine and the end-to-end anastomosis. On naked-eye observation of the sample, a narrowing of the intestinal tract caliber of 5-6 cm was observed, and the intestinal wall was found to be slightly thickened (Figure 2). Histologically, we found thickened portions in the wall, muscle plate thickening, fat reduction, fibrosis, and cholesterol clefts, all of which indicated that needle-like cholesterol thrombi were present in the small arteries of the lumen (Figure 3). Further, giant cells were observed in the vicinity, which could have developed due to a foreign-body reaction (Figure 4).
There was no relapse after surgery, and the patient was discharged 8 d later. Up to the last follow-up at the 12 mo after discharge, the patient showed no recurrence.
CCE was first reported by Peter Ludvig Panum in 1862 and is a rare systemic embolism caused by cholesterol crystals from atherosclerotic plaques. CCE may manifest as a systemic disease, characterized by constitutional symptoms (fever, myalgia, and anemia) and clinical signs due to single or multiorgan involvement (renal failure, gastrointestinal ischemia, central nervous system infarcts, or retinal disturbances)[1]. The risk factors are male sex, age > 60 years, diabetes mellitus, hypertension, atherosclerotic vascular disease, and ischemic nephropathy[2]. Approximately 80% of the cases of CCE reported thus far have occurred because of catheter manipulation and anticoagulation therapy[3]. The present patient had no history of endovascular catheter manipulation, anticoagulation, or thrombolytic therapy, and his symptoms were caused by an embolism. The symptoms could vary according the amount and range of embolization, from acute symptoms caused by arterial embolization to chronic symptoms caused by foreign body reaction to cholesterol crystals. There is no established treatment for CCE[3]. In addition, high-pressure therapy, low-density cholesterol apheresis, steroids, and plasma exchange have been reported as causes of CCE. According to Scolari et al[4] following the kidneys and skin, the digestive system is most susceptible to CCE.
With respect to lesions in the gastrointestinal tract, lesions occur most frequently the large intestine, followed by the small intestine, and finally the stomach[5]. The characteristics of the lesions vary in terms of redness, erosion, ulcer, stricture, obstruction, and symptoms caused such as abdominal pain, diarrhea, and gastrointestinal bleeding[6,7]. Such lesions may also lead to perforation by intestinal ischemia[8]. In our case, the patient was not under any type of treatment including anti-thrombotic therapy and vascular catheterization. Since the arteriosclerosis was very pronounced, it may have been a risk factor, along with hypertension, for CCE. The lesion was confined to one area of the small intestine, and atherosclerosis was observed in the large blood vessels in the vicinity. Thus, the cholesterol emboli could have led to vessel occlusion. Embolism caused by cholesterol crystals differs from thrombosis in that the former does not usually completely occlude the vessel. Since an embolism caused gradual ischemic changes, it may have caused advanced fibrosis, which could further lead to intestinal stenosis. Although this condition has a poor prognosis[9], at present, the current patient is healthy without recurrence.
In conclusion, intestinal obstruction caused by spontaneous CCE is very rare. Although CCE usually has a serious prognosis, this patient is presently healthy without recurrence. In cases of unexplained intestinal obstruction, it may be useful to think of CCE as a potential differential diagnosis.
An 81-year-old man with a clinical history of hypertension, benign prostatic hyperplasia, pulmonary tuberculosis, and an oropharyngeal benign tumor complained abdominal pain, bloating, and anorexia.
Physical examination revealed severe abdominal distension.
Intestinal obstruction, ascites, peritonitis, Intra-abdominal tumor.
Inflammatory response and renal dysfunction were showed.
An abdominal computed tomography revealed focal thickening of the wall of the small intestine, intestinal dilatation of the oral intestine, and intraperitoneal lymphadenopathy.
Cholesterol clefts in small intestine.
Complete surgical excision of lesion.
Cholesterol crystal embolization (CCE) is a rare systemic embolism caused by occlusion of the peripheral arteries by cholesterol crystals from atherosclerotic plaques.
CCE is a rare systemic embolism caused by formation of cholesterol crystals from atherosclerotic plaques. Cases were confined to the gastrointestinal tract is little.
Although the main cause of intestinal obstruction is adhesion or tumor, in cases of unexplained intestinal obstruction, it may be useful to think of CCE as a potential differential diagnosis.
In their work, the Authors describe a rare case of intestinal obstruction caused by spontaneous CCE. This rare form of systemic embolism may attract the attention of the readers. The work is well written with a good iconography.
| 1. | Panniello G, Fenizi G, Amicarelli V, Sanguedolce F, Carosi I, Bisceglia M. Spontaneous cutaneous cholesterol crystal embolism with focal clinical symptomatology: report of a case in an unusual location with secondary histological changes reminiscent of atypical decubital fibroplasia. Am J Dermatopathol. 2011;33:726-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Desai M, Ram R, Prayaga A, Dakshinamurty KV. Cholesterol crystal embolization (CCE): Improvement of renal function with high-dose corticosteroid treatment. Saudi J Kidney Dis Transpl. 2011;22:327-330. [PubMed] |
| 3. | Higo S, Hirama A, Ueda K, Mii A, Kaneko T, Utsumi K, Iino Y, Katayama Y. A patient with idiopathic cholesterol crystal embolization: effectiveness of early detection and treatment. J Nippon Med Sch. 2011;78:252-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Scolari F, Bracchi M, Valzorio B, Movilli E, Costantino E, Savoldi S, Zorat S, Bonardelli S, Tardanico R, Maiorca R. Cholesterol atheromatous embolism: an increasingly recognized cause of acute renal failure. Nephrol Dial Transplant. 1996;11:1607-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Moolenaar W, Lamers CB. Cholesterol crystal embolisation to the alimentary tract. Gut. 1996;38:196-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Venturelli C, Jeannin G, Sottini L, Dallera N, Scolari F. Cholesterol crystal embolism (atheroembolism). Heart Int. 2006;2:155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Paraf F, Jacquot C, Bloch F, de Montpréville V, Bruneval P. Cholesterol crystal embolization demonstrated on GI biopsy. Am J Gastroenterol. 2001;96:3301-3304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Mori H, Kobara H, Kobayashi M, Muramatsu A, Nomura T, Yachida T, Izuishi K, Suzuki Y, Gong J, Masaki T. Rectal perforation from cholesterol embolization syndrome. Endoscopy. 2010;42 Suppl 2:E352-E353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Masuda J, Tanigawa T, Nakamori S, Sawai T, Murata T, Ishikawa E, Yamada N, Nakamura M, Ito M. Use of corticosteroids in the treatment of cholesterol crystal embolism after cardiac catheterization: a report of four Japanese cases. Intern Med. 2013;52:993-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Cho YS, Sijens PE, Zippi M S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN