Published online Feb 28, 2015. doi: 10.3748/wjg.v21.i8.2546
Peer-review started: January 29, 2014
First decision: February 14, 2014
Revised: March 15, 2014
Accepted: April 23, 2014
Article in press: May 23, 2014
Published online: February 28, 2015
Processing time: 396 Days and 23 Hours
The number of bariatric operations, as well as the incidence of perioperative complications, has risen sharply in the past ten years. Perioperative acute portal vein thrombosis is an infrequent and potentially severe postoperative complication that has not yet been reported after biliopancreatic diversion (BPD). Three cases are presented of portal vein thrombosis that occurred following BPD treatment for morbid obesity and type 2 diabetes. The thromboses were detected by abdominal ultrasound and computed tomography with intravenous contrast. The portomesenteric venous thromboses in all three cases presented as unexpected abdominal pain several days after discharge from the hospital. The complications occurred despite adequate perioperative prophylaxis and progressed to bowel gangrene in the diabetic patients only. These cases demonstrate the occurrence of this rare type of complication, which may be observed by physicians that do not routinely treat bariatric patients. Awareness of this surgical complication will allow for early diagnosis and prompt initiation of adequate therapy.
Core tip: As the number of bariatric operations has risen sharply in the past ten years, severe postoperative complications are likely to occur more frequently. Perioperative acute portal vein thrombosis is one such potential complication that has not yet been reported after biliopancreatic diversion. The first reported cases of portal vein thrombosis following laparoscopic biliopancreatic diversion are described, which occurred early in the postoperative period despite adequate perioperative prophylaxis. An early diagnosis made by abdominal ultrasound and computed tomography will allow for prompt initiation of adequate therapy.
- Citation: Cesaretti M, Elghadban H, Scopinaro N, Papadia FS. Portomesenteric venous thrombosis: An early postoperative complication after laparoscopic biliopancreatic diversion. World J Gastroenterol 2015; 21(8): 2546-2549
- URL: https://www.wjgnet.com/1007-9327/full/v21/i8/2546.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i8.2546
Obesity has become a worldwide epidemic affecting up to 25% of the population in developed countries[1,2]. The National Institutes of Health have concluded that surgical therapy offers the best long-term chance of successfully treating morbid obesity for most patients[3]. Indeed, the number of bariatric operations has risen sharply in the past ten years, with 66339 procedures performed between 2005 and 2007 in 235 American Bariatric and Metabolic Centers of Excellence alone[4]. The incidence of complications after bariatric surgery varies greatly, but can be as high as 7%[5]. Furthermore, there is a clear trend towards early postoperative hospital discharge. Therefore, physicians unaccustomed to treating bariatric patients will increasingly be confronted with and required to treat patients with postoperative complications[6]. Biliopancreatic diversion (BPD) is one such surgical procedure that can present complications to the treating primary physician. Although acute portomesenteric vein thrombosis (PMVT) is an infrequent and potentially severe postoperative complication[7], it is a possible cause of unexplained and unexpected abdominal pain in the immediate postoperative period. Three cases are presented of patients who underwent BPD that presented with signs of perioperative PMVT.
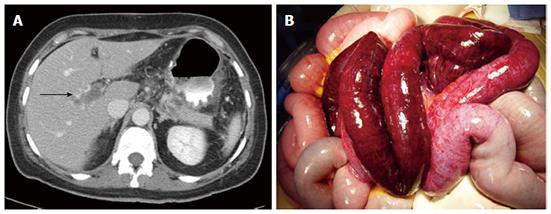
A 51-year-old female with a body mass index (BMI) of 28.4 kg/m2 underwent standard laparoscopic BPD in a pilot study evaluating the effect of BPD on type 2 diabetes mellitus. Preoperative laboratory findings were unremarkable, except for a high glycated hemoglobin level of 8%. Routine thromboprophylaxis in the form of 6000 IU of low molecular weight heparin (LMWH) was initiated immediately after admission and elastic stockings were applied intraoperatively. Laparoscopic BPD was performed without remarkable events. In the immediate postoperative period, routine prophylactic anticoagulation was continued and ambulation was encouraged. The patient was discharged on the fifth postoperative day. Three days later the patient was admitted to a local emergency hospital because of abdominal pain. She was given analgesics and discharged. Two days later she again returned to the hospital presenting with frank signs of an acute abdomen. A computed tomography (CT) scan showed extensive PMVT. The patient was admitted for surgery, upon which gangrene of the biliopancreatic limb was found, necessitating resection and anastomosis 70 cm caudal to the ligament of Treitz, in the absence of internal herniation. Two days later the patient’s condition deteriorated and relaparotomy with re-resection and exteriorization was performed. She was transferred to our unit where Doppler ultrasound (US) and contrast enhanced CT scans were repeated, confirming the continued presence of PMVT (Figure 1). The patient was administered a heparin infusion throughout her hospitalization and recanalization was performed uneventfully one month later. Pre-discharge Doppler US and CT scans showed complete patency of the superior mesenteric and portal veins without portal cavernoma formation. The patient was prescribed fondaparinux and discharged from the hospital.
A diabetic 68-year-old male with a BMI of 35.4 kg/m2 was admitted to our hospital for bariatric surgery. Routine thromboprophylaxis in the form of 6000 IU of LMWH was initiated immediately after admission. The patient underwent a standard laparoscopic BPD without remarkable events and elastic stockings were applied intraoperatively. In the immediate postoperative period, routine prophylactic anticoagulation was continued and early ambulation was encouraged. The patient was discharged on the fifth postoperative day. Ten days later the patient was readmitted to the hospital because of abdominal pain. On evaluation, the patient presented with frank signs of an acute abdomen and shock. A CT scan showed dilatation of small intestinal loops and PMVT. Examination revealed gangrene of the biliopancreatic limb with no signs of ischemia of the alimentary limb. No internal hernia was found. Subtotal jejunal resection along the biliopancreatic limb was performed with exteriorization of the bowel ends. The patient was administered a heparin infusion throughout his hospitalization, with uneventful recanalization performed three months later. Pre-discharge Doppler US and CT scans showed complete patency of the superior mesenteric and portal veins.
A 22-year-old non-diabetic male with a BMI of 45.4 kg/m2 was admitted to our hospital for bariatric surgery. Routine thromboprophylaxis in the form of 6000 IU of LMWH was initiated immediately after admission. There was no family or personal history of coagulation disorders. Preoperative laboratory findings were unremarkable. The patient underwent a standard laparoscopic BPD without remarkable events and elastic stockings were applied intraoperatively. In the immediate postoperative period, routine prophylactic anticoagulation was continued and early ambulation was encouraged. The patient was discharged from the hospital on the fifth postoperative day. Ten days later, he was admitted to a local hospital for abdominal pain. PMVT was observed on Doppler US and CT scans, and the patient was transferred to our unit. A full blood investigation was initiated, including D-dimer and coagulation factor assays, which showed an undiscovered heterozygous mutation in coagulation factor II. Anticoagulation with LMWH was started immediately. There were no signs of intestinal ischemia and no surgery was necessary. The patient was prescribed fondaparinux and discharged from the hospital. A follow-up US showed minimal recanalization of the portal vein.
The increased prevalence of obesity in the United States and Europe is associated with a dramatic increase in the number of gastrointestinal operations that are performed to treat the condition. Although the results and complications of BPD, after nearly 30 years of clinical use, are well known by bariatric surgeons, there have been no reports of PMVT after BPD. PMVT has been well documented since 1868, though its prevalence is rare[8,9] and is usually associated with cirrhosis, liver transplantation, malignancies, inflammatory disorders, hypercoagulable states and variable physiologic derangements. Although there is a low incidence, a prospective study on patients undergoing splenectomy by Ikeda et al[10] revealed that PMVT occurred at a significantly higher rate with laparoscopy versus open surgery, at 55% and 19%, respectively.
A variety of factors result from laparoscopic procedures, including pneumoperitoneum-induced hemodynamic changes, hypercapnia-induced mesenteric vasoconstriction and coagulation impairment, which may contribute to the development of PMVT. A report by Takagi showed that portal venous trunk diameter and blood flow were significantly decreased during laparoscopy with intraperitoneal pressure elevation above 10 mmHg[11]. The majority of splanchnic vein thromboses developed within the widely accepted insufflation pressures of 12 to 15 mmHg, and elevation of intraperitoneal pressure to 7 and 14 mmHg reduced mean portal blood flow by 37% and 53%, respectively. However, the elevated portal venous pressures that occur during laparoscopy normalize after abdominal desufflation[12].
It has been reported that laparoscopy potentially causes a prothrombotic state[13]. In addition, the patient’s position during laparoscopy (such as a prolonged reverse Trendelenburg position that may be necessary for various procedures) may exacerbate portal venous stasis, as has been observed in experimental models[14,15]. In support of this, we have not observed any case of PMVT after open BPD, suggesting that laparoscopy has a role in the pathogenesis of thrombus formation. In the cases presented here, PMVT occurred despite adequate perioperative prophylaxis, and progressed to bowel gangrene in the diabetic patients. It is possible that D-dimer assays and pelvic-abdominal US may serve as an indicator of ongoing thrombosis in the immediate postoperative period, and are therefore advised for monitoring diabetic patients undergoing laparoscopic procedures.
Acute postoperative PMVT is a rare but life-threatening complication that can occur after laparoscopic BPD. Early recognition is of paramount importance to prevent the progression into bowel infarction. In addition to early laparoscopic exploration, abdominal US and CT with intravenous contrast could be very useful diagnostic tools. Treatment should include full anticoagulation, which is effective and safe, and resection and exteriorization are also advised. Further investigations are needed to determine why PMVT occurs only in the biliopancreatic limb and to identify additional methods that can be used for early detection.
Three cases are presented of unexpected abdominal pain following laparoscopic biliopancreatic diversion for treatment of morbid obesity and type 2 diabetes.
Frank acute abdomen.
Internal hernia, anastomotic leakages, biliary peritonitis, mesenteric artery ischemia.
Unremarkable full blood examination in two patients, and identification of a heterozygous mutation in coagulation factor II in one patient.
Abdominal ultrasound and computed tomography imaging showed extensive portomesenteric venous thrombosis (PMVT) in the three patients, along with dilatation of small intestinal loops in one patient.
Gangrene of the biliopancreatic limb is reported upon surgery in two cases.
Surgery and anticoagulation with low molecular weight heparin for the patient with heterozygous mutation of coagulation factor II.
Acute postoperative PMVT is a rare complication of surgery. Clinical presentation and blood tests are often unspecific. Imaging is a very useful diagnostic tool.
In biliopancreatic diversion, approximately two-thirds of the stomach is removed and the remaining portion is reconnected to the ileum bypassing almost nine feet of this digestive organ. Cholecystectomy is also performed.
This report represents the first case of acute PMVT as a postoperative complication after biliopancreatic diversion; acute abdominal pain after bariatric surgery (especially laparoscopy) should be investigated early for a prompt diagnosis and treatment.
This report of three cases provides important guidance to clinicians for the prevention and treatment of PMVT after laparoscopic biliopancreatic diversion.
| 1. | Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6297] [Cited by in RCA: 5895] [Article Influence: 294.8] [Reference Citation Analysis (0)] |
| 2. | Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1817] [Cited by in RCA: 1685] [Article Influence: 80.2] [Reference Citation Analysis (0)] |
| 3. | NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115:956-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1172] [Cited by in RCA: 1025] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 4. | Pratt GM, Learn CA, Hughes GD, Clark BL, Warthen M, Pories W. Demographics and outcomes at American Society for Metabolic and Bariatric Surgery Centers of Excellence. Surg Endosc. 2009;23:795-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Birkmeyer NJ, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010;304:435-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 320] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 6. | Edwards ED, Jacob BP, Gagner M, Pomp A. Presentation and management of common post-weight loss surgery problems in the emergency department. Ann Emerg Med. 2006;47:160-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | James AW, Rabl C, Westphalen AC, Fogarty PF, Posselt AM, Campos GM. Portomesenteric venous thrombosis after laparoscopic surgery: a systematic literature review. Arch Surg. 2009;144:520-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 8. | Webster GJ, Burroughs AK, Riordan SM. Review article: portal vein thrombosis -- new insights into aetiology and management. Aliment Pharmacol Ther. 2005;21:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 117] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Sobhonslidsuk A, Reddy KR. Portal vein thrombosis: a concise review. Am J Gastroenterol. 2002;97:535-541. [PubMed] |
| 10. | Ikeda M, Sekimoto M, Takiguchi S, Kubota M, Ikenaga M, Yamamoto H, Fujiwara Y, Ohue M, Yasuda T, Imamura H. High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg. 2005;241:208-216. [PubMed] |
| 11. | Takagi S. Hepatic and portal vein blood flow during carbon dioxide pneumoperitoneum for laparoscopic hepatectomy. Surg Endosc. 1998;12:427-431. [PubMed] |
| 12. | Rhee RY, Gloviczki P. Mesenteric venous thrombosis. Surg Clin North Am. 1997;77:327-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 112] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Poultsides GA, Lewis WC, Feld R, Walters DL, Cherry DA, Ruby ST. Portal vein thrombosis after laparoscopic colectomy: thrombolytic therapy via the superior mesenteric vein. Am Surg. 2005;71:856-860. [PubMed] |
| 14. | Gutt CN, Schmedt CG, Schmandra T, Heupel O, Schemmer P, Büchler MW. Insufflation profile and body position influence portal venous blood flow during pneumoperitoneum. Surg Endosc. 2003;17:1951-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Junghans T, Böhm B, Gründel K, Schwenk W, Müller JM. Does pneumoperitoneum with different gases, body positions, and intraperitoneal pressures influence renal and hepatic blood flow? Surgery. 1997;121:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Qin JM S- Editor: Gou SX L- Editor: A E- Editor: Ma S