Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2249
Peer-review started: July 8, 2014
First decision: August 6, 2014
Revised: August 29, 2014
Accepted: October 14, 2014
Article in press: October 15, 2014
Published online: February 21, 2015
Processing time: 218 Days and 5.9 Hours
A pancreatic pseudocyst (PPC) is a collection of pancreatic fluid enclosed by a non-epithelialized, fibrous or granulomatous wall. Endoscopic pancreatic pseudocyst drainage (PPD) has been widely used clinically to treat PPCs. The success and complications of endoscopic PPD are comparable with surgical interventions. Stent displacement is a rare complication after endoscopic PPD. Almost all the complications of endoscopic PPD have been managed surgically, and there is rare report involving the endoscopic treatment of intraperitoneal stent displacement. We report here a case of stent displacement after endoscopic ultrasound- and fluoroscopy-guided PPD in a 41-year-old female patient with a PPC in the tail of the pancreas. The endoscopic treatment was successfully performed to remove the displaced stent. The clinical course of the patient was unremarkable. The cyst had significantly reduced and disappeared by 12 wk. We found that both endoscopic ultrasound and fluoroscopy should be used during endoscopic PPD to avoid stent displacement. The displaced stent can be successfully treated by endoscopic removal.
Core tip: Almost all the complications of endoscopic pancreatic pseudocyst drainage have been managed surgically, and there is rare report involving the endoscopic treatment of intraperitoneal stent displacement. This case report not only presents a possible cause of stent displacement during endoscopic ultrasound-pancreatic pseudocyst drainage, but also discusses a novel method of endoscopic stent removal.
- Citation: Wang GX, Liu X, Wang S, Ge N, Guo JT, Liu W, Sun SY. Stent displacement in endoscopic pancreatic pseudocyst drainage and endoscopic management. World J Gastroenterol 2015; 21(7): 2249-2253
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2249.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2249
A pancreatic pseudocyst (PPC) is a collection of pancreatic fluid enclosed by a non-epithelialized, fibrous or granulomatous wall. PPCs are likely to develop within 20%-40% of patients with chronic pancreatitis[1]. When PPCs persist > 6 wk[2,3] and/or are associated with clinical symptoms, surgical, percutaneous, or endoscopic pancreatic pseudocyst drainage (PPD) should be performed[4-6]. Over the past two decades, endoscopic ultrasound (EUS) has become an essential tool for the diagnosis and therapy of PPCs and EUS-guided PPD (EUS-PPD) has been widely used clinically. EUS-PPD can be performed using the transmural placement of a stent. The success and complications of EUS-PPD are comparable with or better than the results reported from surgical interventions[5,7]. Stent displacement is a rare complication after endoscopic PPD. The morbidity of stent displacement is approximately 4% according to a previous report[8]. Almost all of the endoscopic PPD complications have been managed surgically, and reports involving the endoscopic treatment of intraperitoneal stent displacement are rare. We report a case in which the stent displacement was resolved by endoscopic treatment in a 41-year-old female patient with a PPC in the tail of the pancreas.
A 41-year-old non-alcoholic woman who had chronic pancreatitis for two years was admitted to the hospital with a complaint of intermittent painful swelling in the epigastrium that had been present for 12 d. The physical examination during the patient’s check-up showed epigastric pain and active bowel sounds. No masses were evident during abdominal palpation. Blood samples taken at the time of admission showed: hemoglobin, 11.7 g/dL; total leukocyte count, 4000; platelet count, 149000; lipase level, 180; fasting blood glucose, 14.63 × 109/L; total bilirubin, 20.9 × 109/L; and direct bilirubin, 9.9 × 109/L. The amylase, carcinoembryonic antigen, carbohydrate antigen (CA) 125, and CA 19-9 levels, and liver and kidney function tests were within the normal range.
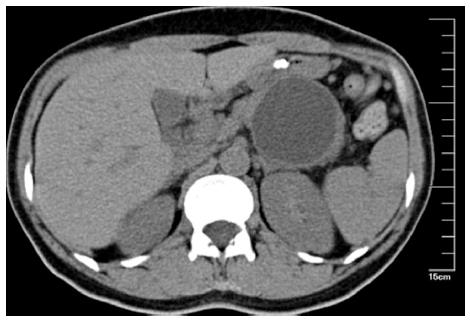
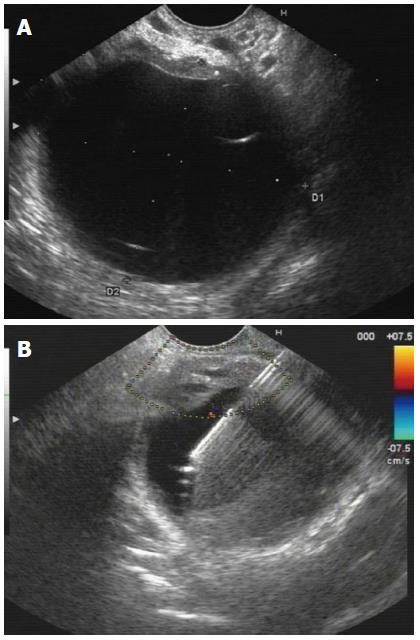
An abdominal contrast CT scan revealed an atrophic pancreatic parenchyma and a well-defined cystic lesion with a diameter of 5.3 cm located in the tail of the pancreas (Figure 1). On EUS, a 4.7 cm × 5.6 cm near-circular unilocular cystic lesion in the tail of the pancreas without continuity to the main pancreatic duct was noted, which was consistent with a pseudocyst (Figure 2A). Fine needle aspiration cytology of the cystic fluid showed no malignant cells. The amylase level was extremely high (22593 U/L). The carcinoembryonic antigen and CA 19-9 concentrations in cyst fluid of the PPC were 64 ng/mL and 35 U/mL, respectively. Based on these findings, we considered the patient to have a symptomatic PPC.
The drainage procedure was carried out with propofol sedation and continuous cardiorespiratory monitoring. Under fluoroscopic and EUS guidance, endoscopic PPD was performed in the lesser curvature of the stomach. Color Doppler ultrasonography was applied to identify the regional vascular structures (Figure 2B). An aspiration needle was inserted into the pseudocyst under EUS guidance.
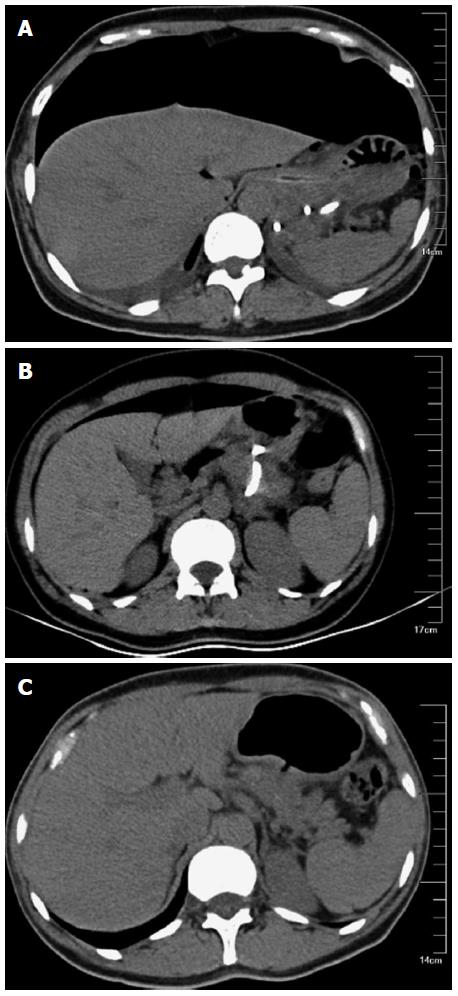
The following steps were guided by fluoroscopy. A guide wire was introduced through the needle and coiled as a quasi-circular shape under fluoroscopy. A cystenterostomy fistula was created using a 10 Fr cystenterostome. The fistula was dilated with a 10 mm balloon. Under fluoroscopic guidance, one 10 Fr double-pigtail plastic stent was placed (Figure 3).
After the procedure, the patient complained of mild abdominal pain. Three days after EUS-guided drainage, the abdominal pain worsened. A bulge was noted on abdominal examination. Localized tenderness in the epigastrium was noted on deep palpation without muscle spasm or rebound tenderness. A CT scan showed that the entire stent had migrated into the lesser peritoneal sac, and there were large amounts of gas in the peritoneal cavity (Figure 4A). A decision was made to remove the stent and perform endoscopic drainage again.
The fistula in the lesser curvature of stomach was seen and dilated using a 10 mm balloon. We advanced the endoscope into the lesser peritoneal sac, and removed the stent with foreign body forceps. A nasobiliary drainage tube was placed in the lesser peritoneal sac via the transgastric fistula. We then performed endoscopic drainage in the posterior wall of the stomach, and placed one 10 Fr double-pigtail plastic stent into the pseudocyst guided by EUS. A nasogastric tube was then placed in the gastric cavity. Peritoneocentesis was performed and the gas in the peritoneal cavity was released.
After 3 d of expectant treatment, the clinical symptoms (abdominal pain and swelling) were resolved. A repeat CT scan of the abdomen 3 d after treatment showed that the cyst had significantly shrunk. The gas in the peritoneal cavity was clearly reduced (Figure 4B). The patient was discharged and a follow-up was conducted by phone and clinic appointment. The PPC disappeared as observed by CT scan 12 wk later (Figure 4C).
Since Grimm first reported EUS-PPD in 1992, EUS-PPD has become the standard procedure for treating symptomatic PPCs[9-13]. During EUS-PPD, EUS can help identify mucinous cystic neoplasms and relative contraindications to endoscopic drainage, such as a distance > 1 cm and normal intervening pancreatic parenchyma[14]. Several authors have directly compared the success and complication rates of endoscopic drainage with surgical therapy and have found them to be comparable[15,16]; however, EUS-PPD has less morbidity, a faster recovery, and is less invasive and expensive than surgery[6,13,17,18].
Previous reports have shown a success rate of > 90% for EUS-PPD in patients with chronic pseudocysts[6,19]. The recurrence rate after EUS-PPD is approximately 4%, and the complication rate is < 16%[20]. In a prospective study with 99 patients, the short-term success rate of EUS-PPD was 93% and the long-term success rate was 84%; complications occurred in 19% of cases[5]. The major complications of EUS-PPD include immediate or delayed infection (0%-8%), bleeding (0%-9%), retroperitoneal perforation (0%-5%), and stent displacement (4.0%-6.5%)[2,5,8,21-24]. In the present case, the guide-wire introduction and stent placement were guided only by fluoroscopy. When introduced through the needle, the guide-wire was coiled in a quasi-circular shape under fluoroscopy, which suggested that the wire remained in the cyst. However, because fluoroscopy only provides a two-dimensional image, the migration vertical to the X-ray might have been overlooked. Thus, the stent displacement may have primarily been due to the lack of EUS imaging during the placement and confirmation of the stent location. Hence, EUS imaging should be monitored from the beginning to the ending of endoscopic PPD.
According to previous reports, almost all stent displacements are managed surgically[25-27]; however, recent advances in therapeutic endoscopy, as well as the development of natural orifices transluminal endoscopic surgery, allow removal of the migrated stents without surgery. There are some case reports involving the endoscopic treatment of stent displacement after EUS-PPD. Mahnken et al[28] reported a case of immediate transgastric repositioning of the dislocated drainage stent with a snaring technique guided by fluoroscopy. Varadarajulu[29] reported a similar case in which a stent was successfully removed using a balloon dilator by fluoroscopic guidance. Chung et al[30] reported the successful endoscopic removal of a migrated double-pigtail stent through a pancreaticoduodenal fistula tract that developed > 6 years after the stent was originally misplaced into the pseudocyst. We report here that endoscopic treatment was successfully performed to remove the migrated stent. The clinical course was unremarkable. The cyst had significantly reduced in size after 3 d, and had disappeared by 12 wk.
In conclusion, both EUS and fluoroscopy should be used during EUS-PPD to avoid stent displacement. The misplaced stent can be successfully treated by endoscopic removal.
A 41-year-old non-alcoholic woman who had chronic pancreatitis for two years presented with intermittent painful swelling in the epigastrium that had been present for 12 d.
Symptomatic pancreatic pseudocyst.
Pancreatic serous cystadenoma; pancreatic mucinous cystadenoma.
Upon admission: hemoglobin, 11.7 g/dL; total leukocyte count, 4000; platelet count, 149000; lipase level, 180; fasting blood glucose, 14.63 × 109/L; total bilirubin, 20.9 × 109/L; and direct bilirubin, 9.9 × 109/L. The amylase, carcinoembryonic antigen, carbohydrate antigen (CA) 125, and CA 19-9 levels, and liver and kidney function tests were within the normal range. The amylase level in cyst fluid of the PPC was 22593 U/L. The carcinoembryonic antigen and CA 19-9 concentrations in cyst fluid were 64 ng/mL and 35 U/mL, respectively.
Computed tomography scan revealed an atrophic pancreatic parenchyma and a well-defined cystic lesion with a diameter of 5.3 cm located in the tail of the pancreas. Endoscopic ultrasound (EUS) showed a 4.7 cm × 5.6 cm near-circular, unilocular cystic lesion in the tail of the pancreas without continuity to the main pancreatic duct.
Fine needle aspiration cytology of the cystic lesion showed no malignant cells.
The patient was treated with endoscopic pancreatic pseudocyst drainage guided by EUS and fluoroscopy.
According to previous reports, almost all stent displacements are managed surgically, however, recent advances in therapeutic endoscopy allow removal of the migrated stents without surgery.
A pancreatic pseudocyst is a collection of pancreatic fluid enclosed by a non-epithelialized, fibrous or granulomatous wall. When pancreatic pseudocysts persist > 6 wk and/or are associated with clinical symptoms, surgical, percutaneous, or endoscopic pancreatic pseudocyst drainage (PPD) should be performed. EUS-guided PPD has been widely used clinically.
This case report presents a possible cause for stent displacement during EUS-guided PPD, and discusses a novel method of stent removal by endoscopy.
The authors describe a case of a patient with an unusual complication of a transgastric stent insertion and subsequent non-surgical management, which is an interesting case report.
| 1. | Usatoff V, Brancatisano R, Williamson RC. Operative treatment of pseudocysts in patients with chronic pancreatitis. Br J Surg. 2000;87:1494-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Samuelson AL, Shah RJ. Endoscopic management of pancreatic pseudocysts. Gastroenterol Clin North Am. 2012;41:47-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Bradley EL, Clements JL, Gonzalez AC. The natural history of pancreatic pseudocysts: a unified concept of management. Am J Surg. 1979;137:135-141. [PubMed] |
| 4. | Pitchumoni CS, Agarwal N. Pancreatic pseudocysts. When and how should drainage be performed? Gastroenterol Clin North Am. 1999;28:615-639. [PubMed] |
| 5. | Kahaleh M, Shami VM, Conaway MR, Tokar J, Rockoff T, De La Rue SA, de Lange E, Bassignani M, Gay S, Adams RB. Endoscopic ultrasound drainage of pancreatic pseudocyst: a prospective comparison with conventional endoscopic drainage. Endoscopy. 2006;38:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 6. | Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009;15:38-47. [PubMed] |
| 7. | Johnson MD, Walsh RM, Henderson JM, Brown N, Ponsky J, Dumot J, Zuccaro G, Vargo J. Surgical versus nonsurgical management of pancreatic pseudocysts. J Clin Gastroenterol. 2009;43:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Fabbri C, Luigiano C, Cennamo V, Polifemo AM, Barresi L, Jovine E, Traina M, D’Imperio N, Tarantino I. Endoscopic ultrasound-guided transmural drainage of infected pancreatic fluid collections with placement of covered self-expanding metal stents: a case series. Endoscopy. 2012;44:429-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Grimm H, Binmoeller KF, Soehendra N. Endosonography-guided drainage of a pancreatic pseudocyst. Gastrointest Endosc. 1992;38:170-171. [PubMed] |
| 10. | Giovannini M. Endoscopic ultrasonography-guided pancreatic drainage. Gastrointest Endosc Clin N Am. 2012;22:221-230, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Kida M, Itoi T. Current status and future perspective of interventional endoscopic ultrasound in Japan. Dig Endosc. 2009;21 Suppl 1:S50-S52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Ng PY, Rasmussen DN, Vilmann P, Hassan H, Gheorman V, Burtea D, Surlin V, Săftoiu A. Endoscopic Ultrasound-guided Drainage of Pancreatic Pseudocysts: Medium-Term Assessment of Outcomes and Complications. Endosc Ultrasound. 2013;2:199-203. [PubMed] |
| 13. | Singla V, Garg PK. Role of diagnostic and therapeutic endoscopic ultrasonography in benign pancreatic diseases. Endosc Ultrasound. 2013;2:134-141. [PubMed] |
| 14. | Ross AS, Kozarek RA. Therapeutic pancreatic endoscopy. Dig Liver Dis. 2010;42:749-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Varadarajulu S, Lopes TL, Wilcox CM, Drelichman ER, Kilgore ML, Christein JD. EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts. Gastrointest Endosc. 2008;68:649-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 16. | Melman L, Azar R, Beddow K, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Edmundowicz S, Jonnalagadda S, Matthews BD. Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystgastrostomy for pancreatic pseudocysts. Surg Endosc. 2009;23:267-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Berzosa M, Maheshwari S, Patel KK, Shaib YH. Single-step endoscopic ultrasonography-guided drainage of peripancreatic fluid collections with a single self-expandable metal stent and standard linear echoendoscope. Endoscopy. 2012;44:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Rotman SR, Kahaleh M. Pancreatic fluid collection drainage by endoscopic ultrasound: new perspectives. Endosc Ultrasound. 2012;1:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Norton ID, Clain JE, Wiersema MJ, DiMagno EP, Petersen BT, Gostout CJ. Utility of endoscopic ultrasonography in endoscopic drainage of pancreatic pseudocysts in selected patients. Mayo Clin Proc. 2001;76:794-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Libera ED, Siqueira ES, Morais M, Rohr MR, Brant CQ, Ardengh JC, Ferrari AP. Pancreatic pseudocysts transpapillary and transmural drainage. HPB Surg. 2000;11:333-338. [PubMed] |
| 21. | Hookey LC, Debroux S, Delhaye M, Arvanitakis M, Le Moine O, Devière J. Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Gastrointest Endosc. 2006;63:635-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 230] [Article Influence: 11.5] [Reference Citation Analysis (1)] |
| 22. | Cahen D, Rauws E, Fockens P, Weverling G, Huibregtse K, Bruno M. Endoscopic drainage of pancreatic pseudocysts: long-term outcome and procedural factors associated with safe and successful treatment. Endoscopy. 2005;37:977-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Weckman L, Kylänpää ML, Puolakkainen P, Halttunen J. Endoscopic treatment of pancreatic pseudocysts. Surg Endosc. 2006;20:603-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Giovannini M, Bories E, Téllez-Ávila FI. Endoscopic Ultrasound-guided Bilio-pancreatic Drainage. Endosc Ultrasound. 2012;1:119-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Henriksen FW, Hancke S. Percutaneous cystogastrostomy for chronic pancreatic pseudocyst. Br J Surg. 1994;81:1525-1528. [PubMed] |
| 26. | Rasmussen DN, Hassan H, Vilmann P. Only few severe complications after endoscopic ultrasound guided drainage of pancreatic pseudocysts. Dan Med J. 2012;59:A4406. [PubMed] |
| 27. | Rana SS, Bhasin DK, Rao C, Gupta R. Intramural pseudocysts of the upper gastrointestinal tract. Endosc Ultrasound. 2013;2:194-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Mahnken AH, Günther RW, Winograd R. Percutaneous transgastric snaring for repositioning of a dislocated internal drain from a pancreatic pseudocyst. Cardiovasc Intervent Radiol. 2008;31 Suppl 2:S217-S220. [PubMed] |
| 29. | Varadarajulu S. EUS-guided retrieval of a migrated transgastric pancreatic stent. Endoscopy. 2007;39 Suppl 1:E18-E19. [PubMed] |
| 30. | Chung IH, Kim HW, Lee DK. Endoscopic removal of a migrated cystogastrostomy double pigtail stent through a pancreatico-duodenal fistula tract. J Interv Gastroenterol. 2011;1:142. |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Chisthi MM, Friedland S, Leeds JS S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Liu XM