Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2206
Peer-review started: March 27, 2014
First decision: April 15, 2014
Revised: May 31, 2014
Accepted: September 12, 2014
Article in press: September 16, 2014
Published online: February 21, 2015
Processing time: 321 Days and 10.9 Hours
Due to the anatomical peculiarity of the appendix, diagnosis of tumors arising from this area can be challenging by clinicoradiologic means. We report a case of a rare primary appendiceal signet ring carcinoma with an uncommon presentation. An 86-year-old woman was admitted to our hospital with subacute epigastric pain. Computed tomography demonstrated bowel wall thickening with fat stranding in the ileocecal region. The leading diagnostic consideration was inflammatory bowel disease. Upon colonoscopy, a swollen, distorted ileocecal valve was identified. The remaining colon was otherwise unremarkable. Extensive biopsy sampling of the ileocecal region and colon was performed. A lymphangitic signet ring carcinoma within the ileocecal region was diagnosed on biopsy; there was no dysplasia or carcinoma of the remaining biopsies. By cytomorphology and immunoprofile, a lymphangitic signet ring carcinoma of appendiceal origin was the primary consideration, further confirmed upon subsequent laparotomy. This case represents an unusual pattern of appendiceal tumor spread with localized, lymphangitic involvement, creating a milieu which closely simulates Crohn’s disease on imaging modalities.
Core tip: Appendiceal signet ring carcinoma (ASRC) is rare and can be confused with other pathologic processes. This aggressive tumor progresses rapidly with frequent extra-appendiceal spread at the time of diagnosis. It’s clinical and radiologic manifestations are non-discrete and can present as ascities, an ovarian mass or appendicitis. The basis of the paper is to address the peculiar and evasive nature of this tumor. Herein we report a case of ASRC, presenting as confined lymphangitic spread within the illeocecal region, clinically mimicking Crohn’s disease.
- Citation: Murdock T, Lim N, Zenali M. Lymphangitic spread from the appendiceal adenocarcinoma to the ileocecal valve, mimicking Crohn’s disease. World J Gastroenterol 2015; 21(7): 2206-2209
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2206.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2206
According to the National Cancer Institute’s surveillance epidemiology and end-results data from 1973 to 2001, signet ring carcinoma has been the least prevalent of the appendiceal tumors at 4%[1,2]. It does however, portend a poor prognosis, with an overall five year survival of 18%[1,2]. Pre-operative diagnosis of this tumor is invariably difficult because it usually lacks specific clinicoradiologic signs and can be confused with an inflammatory process. At time of diagnosis, there is a high probability of extensive tumor spread beyond the appendiceal wall[3,4].
In this report, we present a case of appendiceal signet ring carcinoma (ASRC) in an 86 year old woman. On computed tomography (CT) there was bowel wall thickening and fat stranding involving the ileocecal region and on colonoscopy a swollen ileocecal valve, mimicking features of inflammatory bowel disease (IBD). Upon extensive histologic evaluation of colon biopsies, an ileocecal region-confined lymphangitic tumor consistent with ASCR was identified.
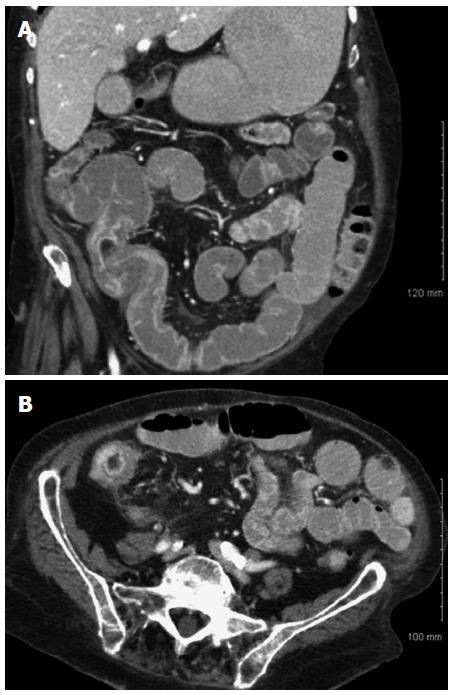
An 86 year-old female was admitted to our hospital with subacute epigastric pain; she had altered bowel habits for several months. Her medical history included atrial fibrillation, diabetes and hypertension. Physical examination was unrevealing. Routine laboratory results were within normal limits. CT imaging showed long segment bowel wall thickening with fat stranding at the ileocecal region (Figure 1). Upon further work up, on colonoscopy, a swollen, distorted ileocecal valve was identified that could not be further intubated (Figure 2). Multiple biopsies of the ileocecal region as well as extensive sampling of the remainder of the colon were performed.
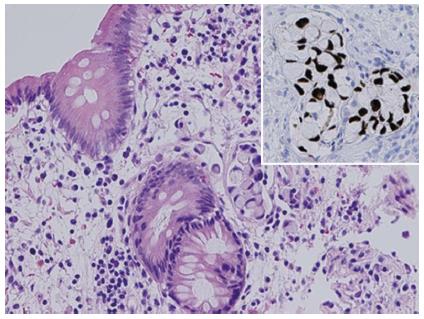
Histologically, the biopsy series contained a lymphangitic signet ring cell neoplasm confined to the ileocecal valve region (Figure 3, HE section). There was no stromal involvement by tumor. The remaining colonic biopsies were free of carcinoma or dysplasia. There was no evidence of IBD. The tumor was positive for CDX-2 (Figure 3, inset) and CK20. It was focally positive for CK7 and was negative for estrogen and progesterone receptors. In view of morphology, immunoprofile and confined lymphangitic nature, the primary consideration included signet ring carcinoma from appendiceal origin. The patient was subsequently scheduled for surgical exploration and possible resection. Upon laparotomy, a large, fixed mass was identified in the right retroperitoneum involving an enlarged, highly distorted appendix with encasement of the ileocecal region. The tumor was deemed non-resectable, and an ileocolic bypass was performed.
After discussions with the oncology team, and given the patient’s age, comorbidities and Eastern Cooperative Oncology Group (ECOG) performance status grade 2, palliative chemotherapy was initiated. The regimen consisted of folinic acid, fluorouracil, and oxaliplatin (FOLFOX), which was given concomitantly with warfarin because of her history of atrial fibrillation. A soft tissue hematoma ensued leading to discontinuation of warfarin therapy and resolution of the hematoma. The patient then suffered an embolic stroke five months following her diagnosis of signet ring carcinoma. After a four month chemotherapy hiatus, FOLFOX was re-initiated at a 25% dose. The patient has now undergone two additional rounds of chemotherapy (5 rounds total), and her ECOG performance status has remained at grade 2, 12 months after the diagnosis.
The various components of the ileocecal area (cecum, appendix, ileocecal valve, terminal ileum) are in close proximity to one another; therefore, pathology may involve more than one anatomic area, creating a diagnostic dilemma[5]. The intimate associations and anatomical peculiarity of the organ contribute to non-specific and even misleading presentations of an appendiceal neoplasm.
Non-neuroendocrine appendiceal malignancies are rare, representing less than 0.5% of all gastrointestinal malignancies[6]. Most mucinous carcinomas of the appendix tend to be identified incidentally, and many are advanced at the time of diagnosis[7]. The narrow diameter of appendix prompts luminal occlusion by the tumor, possible perforation with superimposed appendicitis and increased risk of extension and metastasis by the neoplastic cells[7,8].
On presentation, imaging of a primary appendiceal malignancy may resemble a more common regional disease, including IBD, ischemia or appendicitis[3,4]. Numerous disease processes can also alter the ileocecal imaging and create bowel wall thickening. On imaging, evaluation of various parameters including degree and extent of thickening, pattern of enhancement, presence or absence of fat stranding and associated features including nodal status, can aid in this distinction[5].
On CT imaging, neoplastic processes are more likely associated with wall thickening greater than 3 cm, short segment involvement, and/or an abrupt transition point. In contrary, more commonly identified with IBD are wall thickening less than 2 cm, a longer segment involvement, and/or a smooth transition to normal bowel[9].
Heterogeneous (mixed) attenuation is usually associated with ischemia and necrosis and seen in poorly differentiated gastrointestinal tumors. Heterogeneous-stratified attenuation in IBD is commonly represented by the double halo sign (an inner low-attenuation ring surrounded by an outer higher attenuation ring)[5]. Fat stranding is more commonly associated with inflammatory conditions while asymmetrical/eccentric wall thickening is associated with malignant processes[9]. Of note, IBD and signet ring carcinoma may not be mutually exclusive. In one study, circumferential thickening of the colorectal wall and the presence of free-fluid effusion were correlated with signet ring carcinoma arising in association with IBD[10].
There is a paucity of literature describing the CT findings in primary ASRC. In one case report, CT findings of ASRC included diffuse omental thickening and mild thickening of the appendix, with no obvious mass[6]. Mucinous adenocarcinomas and ASRC are significantly more likely to have tumor extension beyond the colon or metastases at the time of diagnosis, as compared to other primary appendiceal malignancies. Extension to adjacent organs/metastasis can be identified in greater than 70% of patients with ASCR at presentation[2,8,9].
Systemic chemotherapy is a viable treatment option for patients with ASRC. Although optimal medical therapy for ASRC remains unclear, many patients receive a 5-FU-based combination chemotherapy. In a small subset of patients where possible, complete cytoreductive surgery is beneficial. Achieving a complete cytoreduction score of 0 is associated with improved refractory-free and overall survival[11].
In summary, lymphatic-space metastases, from radiographically-obscure carcinoma of appendiceal origin, can closely mimic inflammatory conditions. Familiarity with the vague presentation of the disease, in parallel with the conglomerate of radiologic features, colonoscopy findings and ultimately tissue sampling, can lead to the correct diagnosis. When achievable, in patients with ASRC complete cytoreductive surgery is associated with increased survival.
We thank Sean Reynolds, MD for his help with the computed tomography images.
An 86-year-old woman with subacute epigastric pain and altered bowel habits for several months.
Physical exam and laboratory tests were unrevealing; however, computed tomography demonstrated bowel wall thickening and fat stranding of the ileocecal area, and colonoscopy revealed a distorted, swollen ileocecal valve.
Based on computed tomography, colonoscopy and the demographics of the patient, inflammatory bowel disease, inflammatory/infectious growth and carcinoma were amongst the differential diagnoses.
Laboratory tests were within normal limits at initial presentation.
Computed tomography demonstrated bowel wall thickening and fat stranding in region the ileocecal valve, and colonoscopy demonstrated a swollen, distorted ileocecal valve.
On histologic examination, the ileocecal valve biopsy showed a lymphangitic signet ring cell neoplasm confined within the valve region, which was positive for CDX-2 and CK20. Otherwise, there was no dysplasia or carcinoma arising from the overlying epithelium or evidence of inflammatory bowel disease.
A large, unresectable appendiceal-based tumor mass was present at the time of surgery. The patient underwent palliative ileocolic bypass and five rounds of chemotherapy to date, with folinic acid, 5-fluorouracil and oxaliplatin.
There is a paucity of literature related to primary appendiceal signet ring carcinomas and their clinicoradiologic presentation. There have been rare case reports from appendiceal signet ring carcinoma mimicking inflammatory conditions/appendicitis.
Signet ring carcinomas can present with non-specific radiologic patterns resembling inflammatory processes. Although ruptured appendicitis and inflammatory bowel disease are amongst the plausible differential, particularly in older patients, carcinoma should be suspected. This will lead to further investigation and correct diagnosis, as in the presented.
This article familiarizes the audience with a primary appendiceal carcinoma with an unexpected presentation. Histology was the gold standard in diagnosing malignancy. The diagnostic challenge in the clinical setting often stems from radiographic findings on presentation with features overlapping with inflammatory conditions such as inflammatory bowel disease, ischemia or appendicitis.
| 1. | McGory ML, Maggard MA, Kang H, O’Connell JB, Ko CY. Malignancies of the appendix: beyond case series reports. Dis Colon Rectum. 2005;48:2264-2271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 179] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | McCusker ME, Coté TR, Clegg LX, Sobin LH. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer. 2002;94:3307-3312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 421] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 3. | Fusari M, Sorrentino N, Bottazzi EC, Del Vecchio W, Cozzolino I, Maurea S, Salvatore M, Imbriaco M. Primary signet ring cell carcinoma of the appendix mimicking acute appendicitis. Acta Radiol Short Rep. 2012;1:arsr.2012.120017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Mastoraki A, Papanikolaou IS, Kanakis D, Safioleas P, Sakorafas G, Safioleas M. A case of signet ring carcinoma of the appendix: dilemmas in differential diagnosis and management. J Gastrointest Cancer. 2010;41:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Hoeffel C, Crema MD, Belkacem A, Azizi L, Lewin M, Arrivé L, Tubiana JM. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics. 2006;26:1373-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Bertuzzo VR, Coccolini F, Pinna AD. Peritoneal seeding from appendiceal carcinoma: A case report and review of the literature. World J Gastrointest Surg. 2010;2:265-269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Hashash JG, Nasr JY, Francis F. Education and Imaging. Gastrointestinal: mucinous and signet cell adenocarcinoma of the appendix. J Gastroenterol Hepatol. 2013;28:903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Turaga KK, Pappas SG, Gamblin T. Importance of histologic subtype in the staging of appendiceal tumors. Ann Surg Oncol. 2012;19:1379-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 164] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 9. | Macari M, Balthazar EJ. CT of bowel wall thickening: significance and pitfalls of interpretation. AJR Am J Roentgenol. 2001;176:1105-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 232] [Article Influence: 9.3] [Reference Citation Analysis (1)] |
| 10. | Hristova L, Soyer P, Hoeffel C, Marteau P, Oussalah A, Lavergne-Slove A, Boudiaf M, Dohan A, Laurent V. Colorectal cancer in inflammatory bowel diseases: CT features with pathological correlation. Abdom Imaging. 2013;38:421-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Lieu CH, Lambert LA, Wolff RA, Eng C, Zhang N, Wen S, Rafeeq S, Taggart M, Fournier K, Royal R. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol. 2012;23:652-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Grossi L, Raman M, Schafer KH S- Editor: Gou SX L- Editor: A E- Editor: Liu XM