Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2169
Peer-review started: June 24, 2014
First decision: August 6, 2014
Revised: September 8, 2014
Accepted: November 18, 2014
Article in press: November 19, 2014
Published online: February 21, 2015
Processing time: 233 Days and 0 Hours
AIM: To investigate clinical features, treatment strategies and outcomes of patients with hepatolithiasis (HL) undergoing surgical treatment, using a new clinical classification.
METHODS: Sixty-eight HL patients were hospitalized and treated surgically from August 2011 to December 2012 and they were classified into four HL types according to pathological evolution of the disease. These four HL types included type I primary type (defined as no previous biliary tract surgery), type II inflammatory type (with previous biliary tract surgery and cholangitis), type III mass-forming type (HL complicated by hepatic mass-forming lesion), and type IV terminal type (with secondary biliary cirrhosis and resultant portal hypertension). The perioperative data including general information, imaging data, postoperative complications, and immediate and final stone clearance rate were obtained and analyzed.
RESULTS: In all 68 patients, the proportion of HL type I-IV was 50% (34/68), 36.8% (25/68), 10.3% (7/68) and 2.8% (2/68), respectively. Abdominal pain was the main clinical manifestation in type I (88.2%), fever was predominant in type II (52.0%), the malignancy rate in type III was high (71.4%), and portal hypertension and spleen enlargement were common in type IV (2/2, 100.0%). Liver resection rate for types I-III was 79.4%, 72.0% and 71.4%, respectively. The overall incidence of postoperative complications was 23.5% (16/68). There were no perioperative deaths. The average length of hospital stay was 12.7 ± 7.3 d. Immediate and final stone clearance rate was 73.5% (50/68) and 89.7% (61/68), respectively. Fifty-nine of 68 patients (86.8%) were followed- up for > 1 year after surgery, and 96.6% of these patients (57/59) had a good quality of life according to a criterion recommended for postoperative evaluation of quality of life.
CONCLUSION: The pathological evolution-based clinical classification of HL has a role in optimizing treatment strategy, and patients can benefit from this classification when it is used properly.
Core tip: Hepatolithiasis (HL) is a complicated disease to treat and has few conveniently used clinical classifications. In this study, a new clinical classification for HL based on pathological evolution was introduced, which included HL types I-IV based on with (type II) or without (type I) previous biliary tract surgery, with mass-forming lesion (type III) or secondary biliary cirrhosis with portal hypertension (type IV). It is safely and conveniently used in our hospitals and patients can benefit from this classification when it is used properly.
- Citation: Liu FB, Yu XJ, Wang GB, Zhao YJ, Xie K, Huang F, Cheng JM, Wu XR, Liang CJ, Geng XP. Preliminary study of a new pathological evolution-based clinical hepatolithiasis classification. World J Gastroenterol 2015; 21(7): 2169-2177
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2169.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2169
Hepatolithiasis (HL) refers to calculi formed in the proximal part of the junction of the left and right hepatic duct within the liver. Following the formation of calculi in the biliary tract of the liver, they can obstruct the biliary tract, resulting in infection and associated liver parenchymal damage[1]. In the early stage of the disease, biliary dilation and expansion of liver parenchyma can occur; in the following stages, the wall of the bile duct becomes thickened, due to surrounding abnormally proliferated fibrous tissue and accompanying infiltrated chronic inflammatory cells[2-4]. Eventually, atrophy and failure of corresponding liver segments occur, with concurrent liver abscess and malignancy in some patients due to these accumulated changes, and secondary biliary cirrhosis and portal hypertension syndrome also occur in a few cases[5-8]. Specific clinical symptoms of HL can present in patients with respective clinicopathological changes, and patients at different pathological stages can present to doctors for treatment, therefore, we classified patients with HL into four different types based on clinical manifestations at specific pathological stages: type I primary type, type II inflammatory type, type III mass-forming type, and type IV terminal type[9].
The current study applied this clinical classification to 68 patients with HL, and their clinical features and treatment strategies were analyzed to establish an optimal treatment strategy for each type to reduce residual stones and relapse, and improve therapeutic efficacy.
According to the classification, 68 cases of HL were sorted into four types: type I primary type, type II inflammatory type, type III mass-forming type and type IV terminal type. The same team of surgeons from the Hepato-Pancreato-Biliary Surgery Department of the 1st and 2nd Affiliated Hospital of Anhui Medical University performed surgery on these patients from August 2011 to December 2012. Basic information, preoperative laboratory test results, imaging data, distribution of stones, type of surgery, immediate and final stone clearance rate, postoperative complications, and therapeutic efficacy in the short-term were obtained.
Doppler ultrasound (US), computed tomography (CT) and magnetic resonance imaging were jointly used to assess the distribution and range of stones, expansion or stricture of bile ducts, condition of the bile duct tree, atrophy of liver lobes/segments, fibrosis, mass-forming property of the lesions, and complications of cirrhosis. For patients with cirrhosis, barium meal examination of the esophagus was performed to establish the degree of esophageal varicose veins and secondary portal hypertension. Nutritional risk assessment and evaluation of liver function grade and reserve were carried out routinely for each patient.
A detailed surgical plan was formed based on preoperative evaluation and the main considerations included how to remove as many stones as possible, whether liver lobe resection was needed, and how to select the method of biliary drainage. Indications for liver lobe resection included: Bile duct stones located within one liver lobe and the presence of atrophy or fibrosis; multiple liver abscesses secondary to bile duct infection; and mass-forming lesions with suspicion of malignancy. Precise surgery was performed with the assistance of BiClamp forceps, titanium clamps and a high-frequency electric knife, with or without occlusion of the first hepatic hilar region[10]. Choledochoscopy was performed in all patients to help determine the distribution of bile duct stones, directly extract them, with the assistance of a stone basket when needed, and evaluate the function of the sphincter of Oddi (SO) in the lower part of the common bile duct. Grading criteria for the SO function were as follows: normal: SO radiates through the center or looks bean-shaped with normal rhythmic contractions and the choledochoscope cannot enter the duodenum; SO laxity (SOL): the choledochoscope directly enters the duodenum and the duodenal mucosa can be seen from the common bile duct[11]. Based on SO grading and whether stones were removed completely, the method of biliary drainage was chosen individually: external T tube drainage was chosen for normal SO without residual stones, and cholangioenterostomy was chosen for SOL without residual stones. If residual stones could not be prevented, cholangioenterostomy and T tube drainage were performed at the same time[12]. Choledochoscopy was performed again after hepatic lobe resection to check whether there were residual stones and to assess the immediate stone clearance rate. Bile acid was collected and sent for bacterial culture and drug sensitivity testing in all patients.
Fast-track postoperative rehabilitation: Patients were given gastric acid secretion inhibitors and broad-spectrum antibiotics immediately after and a liquid diet 48 h after surgery; the antibiotics were adjusted if necessary according to the bile acid culture results; liver function tests were monitored at 1, 3 and 7 d after surgery; and short-term surgical complications were treated in a timely manner.
Follow-up: All patients were followed-up by regular visits from 4 to 6 wk after discharge, clinical symptoms and signs were checked, liver function was monitored, and anatomical structure of the liver was examined using US, CT or magnetic resonance cholangiopancreatography (MRCP). Immediate stone clearance was defined as complete depletion of stones during the operation. Final stone clearance was defined as removal of residual stones after the operation using a stone basket under choledochoscopy or holmium laser. Postoperative residual stones were defined as remaining stones that could not be removed by any method, and were confirmed by US, CT or MRCP 3 mo postoperatively[7,13,14]. Postoperative quality of life was divided into three types based on the criteria used in our hospitals: patients are asymptomatic and can return to normal work after surgery, graded as excellent; patients have occasional abdominal pain and discomfort, but they can continue normal work and life, graded as good; patients with recurrent cholangitis, residual intrahepatic bile duct stones or relapse, or cancer forming, graded as poor. All the information mentioned above was kept in the Hengkang medical follow-up system to ensure integrity of the follow-up information.
All clinical data were entered into SPSS version 10.01 statistical software. The student’s t-test was used for measurement data and the χ2 test was used for categorical data. P < 0.05 was defined as statistically significant.
We studied 68 patients (48 female and 20 male, with a male to female ratio of 0.42:1) and an average age of 50.5 ± 10.8 years. Forty-nine patients (72.1%) had Child class A liver function and 19 (27.9%) had Child class B function. The four types of HL based on our new classification were 34 type I (50.0%), 25 type II (36.8%), seven type III (10.3%) and two type IV (2.9%).
According to whether the liver lobes were removed jointly, operations were divided into simple cholangiotomy (16 cases: 7 type I, 7 type II, 1 type III, and 1 type IV) and cholangiotomy combined with partial hepatectomy (52 cases: 27 type I, 18 type II, 6 type III, 1 type IV). Biliary drainage was divided into external T-tube drainage (48 cases: 29 type I, 12 type II, 6 type III, 1 type IV) and cholangioenterostomy (20 cases: 5 type I, 13 type II, 1 type III, and 1 type IV) (Table 1).
| Primary | Inflammatory | Mass-forming | Terminal | Total | Percentage | |
| Biliary tract exploration + external T tube drainage | 7 | 4 | 1 | 1 | 13 | 19.1% |
| Biliary tract exploration + cholangioenterostomy | 0 | 3 | 0 | 0 | 3 | 4.4% |
| Partial liver resection + external T tube drainage | 22 | 8 | 5 | 0 | 35 | 51.5% |
| Partial liver resection + cholangioenterostomy | 5 | 10 | 1 | 1 | 17 | 25.0% |
| Total | 34 | 25 | 7 | 2 | 68 |
Fiberoptic choledochoscopy was performed in all patients. Five patients had past cholangioenterostomy; two of them received end-to-end anastomosis (SO not retained), and three received end-to-side anastomosis (SO retained). The SO function in 66 cases was assessed by choledochoscopy and SOL was found in 18 cases (27.3%). Complete stone clearance was confirmed in 50 cases by choledochoscopy during the operation and total immediate stone clearance rate was 73.5%, including 26 (76.5%) type I cases, 19 (76%) type II cases, four (57.1%) type III cases, and one (50%) type IV case (Table 2). The difference between the immediate stone clearance rates in the four types was not significant (P = 0.623). In 18 cases, residual stones were completely removed by repeated stone removal (1-4 times) by choledochoscopy in 11 cases, and the final stone clearance rate was 89.7% (61/68). The final stone clearance rate for types I-IV was 91.2% (31 cases), 92.0% (23 cases), 71.4% (5 cases), and 100% (2 cases), respectively, which did not differ significantly among the four types (P = 0.104) (Table 1). There were 40 cases of immediate stone removal among 52 patients with cholangiotomy combined with partial hepatectomy, with an immediate stone clearance rate of 76.9%. There were 10 cases of immediate stone removal in 16 patients with simple cholangiotomy, with an immediate stone clearance rate of 62.5%. Immediate stone clearance rate between the two groups did not differ significantly (P = 0.332) (Table 3).
| Primary | Inflammatory | Mass-forming | Terminal | Total | |
| Immediate case | 26 (76.5) | 19 (76.0) | 4 (57.1) | 1 (50.0) | 50 (73.5) |
| Final case | 31 (91.2) | 23 (92.0) | 5 (71.4) | 2 (100) | 61 (89.7) |
| Total cases | Clearance cases | Clearance rate | P value | |
| Liver resection | 52 | 40 | 76.9% | 0.332 |
| Non-liver resection | 16 | 10 | 62.5% |
The average operating time was 236.8 ± 65.24 min. Bacterial culture of bile was performed in 58 cases and 45 (77.6%) were positive; 35 (60.3%) for Gram-negative bacteria and 12 (20.7%) for Gram-positive bacteria. The three most common bacteria cultured in bile were Escherichia coli (19 cases), Enterococcus faecium (5 cases) and Enterococcus faecalis (5 cases). Postoperative complications occurred in 16 cases (23.5%), including seven cases of bile leakage (10.3%, cured by puncture drainage), six cases (8.8%) of pulmonary infection, four cases (5.9%) of incisional wound infection, two cases (2.9%) of postoperative intraperitoneal hemorrhage, and one case (1.5%) of bleeding complicated by adhesive intestinal obstruction (cured by enterodialysis), in which all post-operative complications were eventually cured and no perioperative deaths occurred. The average length of hospital stay after surgery was 12.7 ± 7.3 d.
Fifty-nine of 68 patients (86.8%) were followed up for an average 16.4 ± 4.3 mo. In five cholangiocarcinoma cases (type III), three patients died and two survived, but did not relapse during follow-up. Satisfactory postoperative quality of life was reported in 54/59 patients (91.5%), including 95.6% for type I, 96.6% for type II, 57.1% for type III, and 100% for type IV.
Surgery remains the main treatment option for HL and the principle is to remove lesions, extract stones, remedy strictures, free drainage, relieve cholestasis, restore the biliary tract to normal physiological function, and cure disease[15-19]. HL is complicated, therefore, an appropriate and personalized treatment strategy should be devised for each specific case, with considerations including number and distribution of stones, location and degree of stricture, expansion of biliary tract, pathological change, and functional status of the liver, as well as the overall condition of the patients. For each specific case, evaluation of the distribution of stones and liver function and a definite surgical plan are preferred preoperatively. Accurate surgery, complete removal of the diseased liver lobe including atrophy and stones, and selecting the appropriate method of bile tract drainage based on SO function are favored during the operation. Good patient management, reduction of complications, close follow-up, and dietary advice to reduce relapse and improve therapeutic efficacy are encouraged postoperatively[15].
HL can be divided into cholesterol and pigment type according to the chemical composition of the stones, and the latter can be further divided into black and brown pigment types. Due to differences in stone composition caused by diet between eastern and western patients, HL is also divided into western type (cholesterol and black pigment type) and Asian type (brown pigment type)[20]. Other classifications of HL have a greater focus on stone distribution or biliary stricture and expansion[18,21-23]. The Biliary Study Group of the Chinese Medical Association proposed one HL classification scheme in 2007 based on location of stones and lesion extent, which resulted in type I (focal type): stones limited to one lobe or segment; and type II (diffuse type): stones distributed within both liver lobes. Type II was further divided into four subtypes: type IIa without fibrosis and atrophy; type IIb with regional fibrosis and atrophy; type IIc with widespread fibrosis, secondary biliary cirrhosis, and portal hypertension; and type IId with stones outside the biliary tract[15]. This classification is considered to be comprehensive and widely accepted by hepatobiliary surgeons, but it is too complicated to implement when it is used to guide clinical treatment and compare therapeutic efficacy.
We propose our HL classification which combines biliary tract surgery history and clinical and pathological changes at the onset of disease, including: type I (primary type): (1) no previous surgery; (2) type II (inflammatory type): one or more previous biliary tract operations and recurrent cholangitis; (3) type III (mass-forming type): multiple intrahepatic stones accompanied by a mass-forming lesion, regardless of whether benign or malignant; and (4) and type IV (terminal type): multiple intrahepatic stones accompanied by secondary biliary cirrhosis, portal hypertension, splenomegaly, hypersplenism, portal vein spongiform degeneration or schistosomiasis hepatic cirrhosis[9]. We summarized the clinical data of 68 patients with HL based on our classification scheme and found the following: Type I (primary type): 34 of 68 cases (52.9%). The main clinical manifestation was abdominal pain (30 cases), Child class A liver function was found in 27 cases (79.4%). Liver lobectomy combined with external T tube drainage was performed in 27 cases (79.4%) including 18 cases of left lateral hepatectomy (66.7%). Lung infections were commonly seen postoperatively (3/5). Type II (inflammatory type): 25 cases. The main clinical manifestation was fever in 13 cases (52.0%), liver resection was performed in 18 cases (72%), and cholangioenterostomy was performed in 13 cases (52%). Bile leakage was the main postoperative complication in four of eight cases, and 22 of 23 cases (95.7%) were bile culture positive. Type III (mass-forming type): seven cases. There were five cases of cholangiocarcinoma. Laboratory tests showed increased CA19-9 and predominantly Child class B liver function in three of seven cases. Treatment included liver resection (5/7) and external T-tube drainage (6/7). Postoperative hospital stay and duration of drainage tube use were longer. The bile culture positive rate was high (85.7%, 6/7 cases). Type IV (terminal type): only two cases. Imaging data indicated cirrhosis, portal hypertension, and spleen enlargement. Laboratory tests showed poor liver function, prothrombin time extension and surgical treatment options were limited.
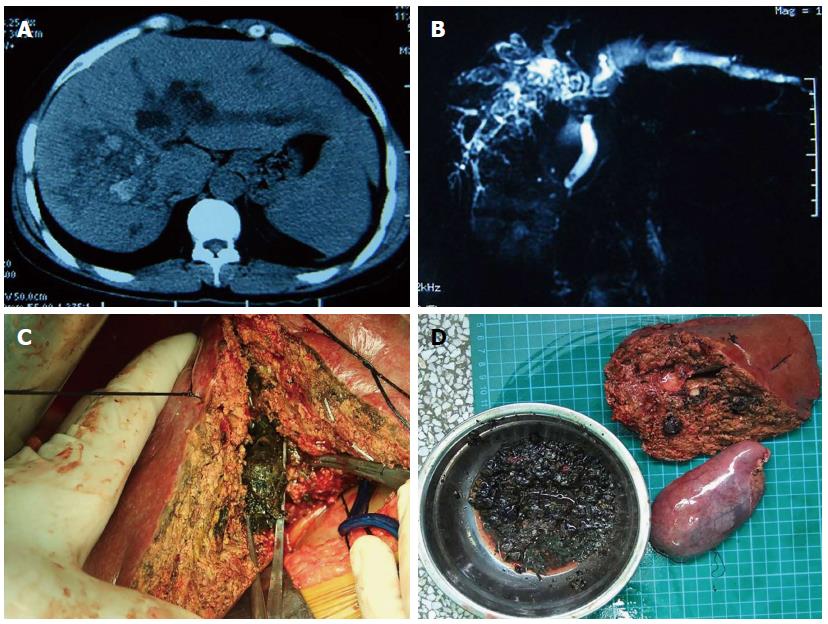
Each type of HL based on our classification was found to have specific clinical features. Primary type (type I) exhibited multiple intrahepatic stones with or without gallstones, with no previous biliary tract surgery. Primary intrahepatic biliary tract stones occurred in most cases due to biliary tract roundworm or abnormal metabolism and secretion of bile and its abnormal composition. A few cases showed abnormal biliary tract anatomy. Patients with this type of HL often exhibited no typical symptoms and no severe biliary infection. A large number of intrahepatic biliary tract stones were often found at first diagnosis with fewer extrahepatic biliary tract and gallbladder stones. Therefore, these patients normally had reasonable liver function and partial hepatectomy combined with cholecystectomy was the main surgical procedure (Figure 1). There were 27 cases of partial hepatectomy and 29 cases of external T tube drainage among 34 cases of primary type HL.
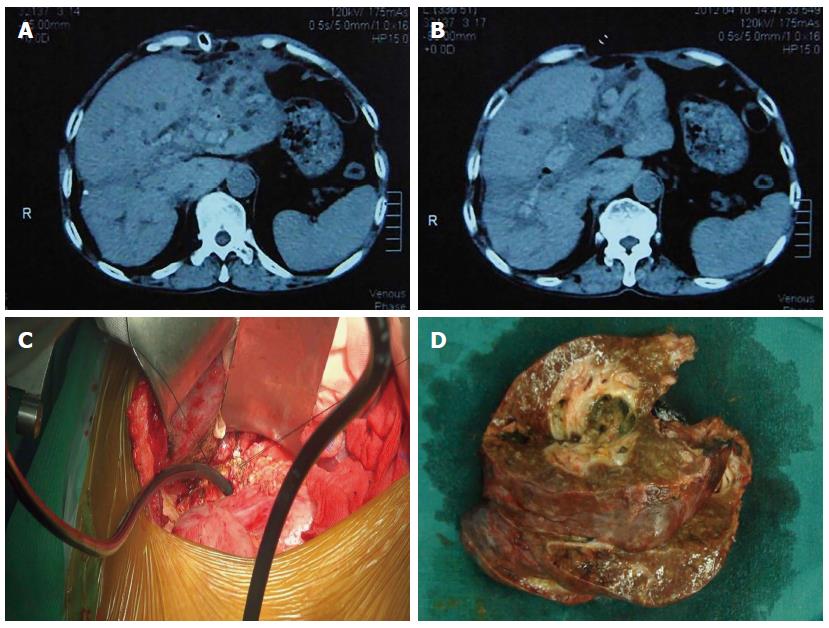
Inflammation type (type II) patients often had previous biliary tract surgery to remove stones from outside the liver. However, prior surgery often caused injury to the OS or biliary tract, or was performed incorrectly with cholangioenterostomy, followed by the formation of multiple intrahepatic stones with recurrent cholangitis. Imaging data often showed different degrees of intrahepatic biliary tract expansion and gas formation. Some patients had frequent and severe cholangioenterostomy reflux due to previous cholangioenterostomy and primary or secondary SOL. Patients with this type of HL can undergo partial liver resection combined with cholangioenterostomy. However, attention needs to be paid to the different degree of stricture or short bridge loop due to previous cholangioenterostomy, or abandoned improper cholangioenterostomy such as choledochoduodenostomy, bile-duct and jejunal side-to-side anastomosis or bile-duct and jejunal end-to-side anastomosis. In such cases, the stricture or anastomotic stoma may need to be removed to regenerate functional cholangioenterostomy. PTCD (percutaneous transhepatic cholangio drainage) or ENBD (endoscopic nasobiliary drainage) can be used to control cholangitis until the disease is stabilized for further surgical stone removal (in accordance with the principles of injury control). Emergency laparotomy should be avoided when severe cholangitis occurs (Figure 2). In 25 patients with type II HL, partial hepatectomy was performed in 17 cases (68%) and cholangioenterostomy was performed in 13 (52%).
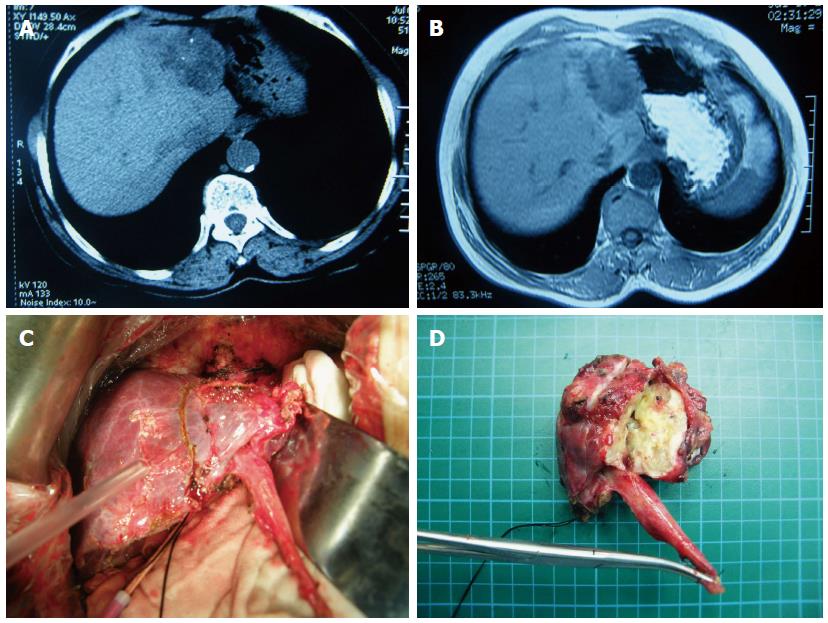
Mass-forming type of HL (type III) was confirmed by imaging showing intrahepatic biliary stones with single or multiple lesions, and lesions in the liver including inflammatory lesions, abscesses and tumors. Abscesses in HL should be cut or punctured for drainage. Inflammatory masses, especially those deep in the liver, can also be cured by drainage and anti-infective therapy. If the lesion is confirmed to be a malignant tumor, surgery can only be performed when the tumor is contained in the resected liver segments. In seven patients with type III HL, there were five cases of cholangiocarcinoma (Figure 3) and these patients received partial hepatectomy. There were two cases of inflammatory masses; one received partial hepatectomy and the other mass incision and abscess drainage.
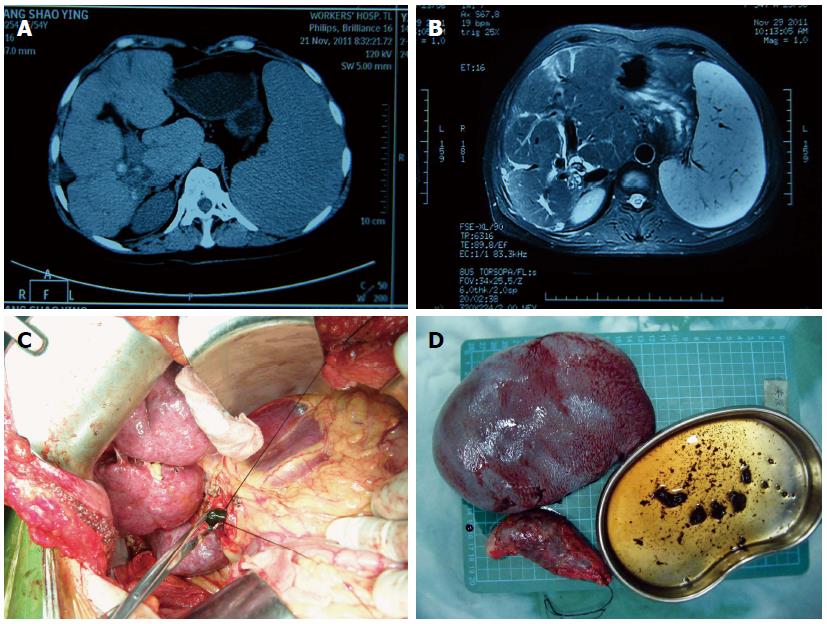
Terminal type (type IV) HL exhibited multiple intrahepatic stones complicated by liver cirrhosis, portal hypertension, hypersplenism and portal vein spongy degeneration or schistosomiasis cirrhosis. Patients often had a history of repeated biliary tract surgery both inside and outside the liver, stone recurrence, residual stones, upper digestive tract bleeding, and biliary cirrhosis in the late stage. Imaging indicated cirrhosis, reduced liver volume, liver deformation, and spleen enlargement. Laboratory tests showed liver dysfunction, prothrombin time extension, and elevated bilirubin level. Some patients were complicated by portal vein spongy degeneration or schistosomiasis cirrhosis, repeated ascites, lower limb edema, and malnutrition. Such patients had poor prognosis and treatment was difficult, with liver transplantation being the last option. Due to the limited number of cases in this study, only two cases belonged to this type; one of which received splenectomy, followed by selective secondary surgery to improve liver function, and the other received splenectomy plus biliary tract incision to remove stones (Figure 4).
Appropriate treatment for HL is complex and the patients are often from poor families and have undergone repeated surgery, with high expectation for complete removal of stones and elimination of relapse. Thus, careful planning is needed based on comprehensive preoperative evaluation and precise liver surgery rather than an exploratory operation. Precise liver surgery for HL is different from that for liver cancer. It involves limited liver resection to excise as much as possible of the fibrotic or atrophic liver parenchyma and as little as possible of normal liver tissue, with margins close to the lesions, to ensure better residual liver function. In precise liver surgery, the first hepatic hilum can be blocked repeatedly for removal of lesions and stones. Choledochoscopy can be performed before and after liver resection to distinguish and confirm stone distribution, remove stones with the assistance of a stone basket, and to assess OS function to choose the appropriate biliary drainage method. The choledochoscope can enter level II of the biliary tract or level III or above when it is dilated, and it can directly visualize mucosal lesions of the biliary tract, and the size, number and shape of the stones, biliary tract stricture and its location. It can also remove stones repeatedly, assess immediate stone clearance rate, and help reduce surgical complications. A high immediate stone clearance rate in the liver resection and non-liver resection groups indicated precise judgment of the indication for partial liver resection. In the non-liver resection group, the stones were located within level II of the biliary tract and were removed using choledochoscopy only, and there was no indication for partial liver resection. A high immediate stone clearance rate and final stone clearance rate in the four types of HL based on our classification indicated that our current surgical strategy was rational and a similar therapeutic effect could be achieved despite the different clinical features.
In summary, we proposed a clinical classification method for HL that took account surgical history, clinical and imaging features, and the pathological evolutionary process of HL. Each type of HL within our classification scheme has a preferential treatment option, but the therapeutic effect was similar, indicating that the classification is scientific, reasonable, clinically applicable, and useful for optimal treatment selection. However, the number of cases in this study was limited, and long-term follow-up was lacking. This classification needs to be improved to guide clinical therapy and improve the therapeutic effect, in combination with other classification schemes such as that proposed by The Biliary Study Group of the Chinese Medical Association. In addition to classification, clinical practice requires careful evaluation of stone distribution, liver function and preoperative planning. Meticulous handling is desired to ensure complete removal of stones and lesions and free drainage. Good management is required after the operation to reduce complications and prevent stone recurrence. Precise liver resection requires a combination of surgical effectiveness and safety to benefit patients as much as possible[24,25].
Hepatolithiasis (HL) can cause many problems in patients including biliary tract dilation, biliary tract infection, and associated liver parenchymal damage including chronic inflammation and cirrhosis. The current management strategies are to remove lesions, extract stones, remedy strictures, free drainage, relieve cholestasis, restore the biliary tract to normal physiological function, and cure disease when possible, based on an appropriate classification, however, the outcomes of HL patients are still unsatisfactory.
Many HL classifications are currently used in clinical practice, however, not many are useful. The current research hotspot is to improve therapeutic efficacy by proposing new classifications.
In order to develop an HL classification, we introduced a novel classification for HL based on pathological changes, which included type I primary type (defined as no previous biliary tract surgery), type II inflammatory type (previous biliary tract surgery and cholangitis), type III mass-forming type (HL complicated by hepatic mass-forming lesion), and type IV terminal type (with secondary biliary cirrhosis and resultant portal hypertension).
The initial study results suggest that the pathological evolution-based classification for HL could be a potentially useful clinical classification in the future.
HL is a disease in which calculi form in the biliary tract within the liver, and can cause many problems, including biliary tract dilation, biliary tract infection, chronic inflammation, and liver cirrhosis.
Hepatolithiasis is a very complex and difficult disease to treat. This paper introduced a new clinical classification based on pathological evolution in order to get a useful guideline to different hepatolithiasis. It is valuable for hepatolithiasis research and treatment.
| 1. | Sakpal SV, Babel N, Chamberlain RS. Surgical management of hepatolithiasis. HPB (Oxford). 2009;11:194-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (5)] |
| 2. | Jarufe N, Figueroa E, Muñoz C, Moisan F, Varas J, Valbuena JR, Bambs C, Martínez J, Pimentel F. Anatomic hepatectomy as a definitive treatment for hepatolithiasis: a cohort study. HPB (Oxford). 2012;14:604-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Lai EC, Ngai TC, Yang GP, Li MK. Laparoscopic approach of surgical treatment for primary hepatolithiasis: a cohort study. Am J Surg. 2010;199:716-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Lilly JR, Karrer FM. Contemporary surgery of biliary atresia. Pediatr Clin North Am. 1985;32:1233-1246. [PubMed] |
| 5. | Bai XL, Chen YW, Zhang Q, Ye LY, Xu YL, Wang L, Cao CH, Gao SL, Khoodoruth MA, Ramjaun BZ. Acute iatrogenic Budd-Chiari syndrome following hepatectomy for hepatolithiasis: a report of two cases. World J Gastroenterol. 2013;19:5763-5768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Chen DW, Tung-Ping Poon R, Liu CL, Fan ST, Wong J. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 95] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Fang CH, Liu J, Fan YF, Yang J, Xiang N, Zeng N. Outcomes of hepatectomy for hepatolithiasis based on 3-dimensional reconstruction technique. J Am Coll Surg. 2013;217:280-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Jiang H, Wu H, Xu YL, Wang JZ, Zeng Y. An appraisal of anatomical and limited hepatectomy for regional hepatolithiasis. HPB Surg. 2010;2010:791625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Geng XP. The problem of surgical management in hepatolithiasis and treatment strategy. Gandan Waike Zazhi. 2002;10:2. [DOI] [Full Text] |
| 10. | Zhao HC, Geng XP, Liu FB, Wang Guobing, Zhao YJ, Zhang ZG. Clinical application of ERBE Biclamp forceps assisted liver resection. Zhonghua Gandan Waike Zazhi. 2011;17:4. [DOI] [Full Text] |
| 11. | Liang TB, Liu Y, Bai XL, Yu J, Chen W. Sphincter of Oddi laxity: an important factor in hepatolithiasis. World J Gastroenterol. 2010;16:1014-1018. [PubMed] |
| 12. | Liu FB, W GB, Luo YZ, Zhao YJ, Chen JM, Xie K, Mao CK, Geng XP. Clinical efficacy of precision liver surgery in the management of hepatolithiasis. Zhonghua Xiaohua Waike Zazhi. 2013;21:2. [DOI] [Full Text] |
| 13. | Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007;31:479-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (2)] |
| 14. | Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T, Tanaka S, Kubo S. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009;198:199-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 15. | Biliary surgery group of surgery branch of the Chinese Medical Association. The guideline of diagnosis and treatment of hepatolithiasis. Zhonghua Xiaohua Waike Zazhi. 2007;6:5. [DOI] [Full Text] |
| 16. | Suzuki Y, Mori T, Yokoyama M, Nakazato T, Abe N, Nakanuma Y, Tsubouchi H, Sugiyama M. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014;21:617-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (2)] |
| 17. | Shah OJ, Robbani I, Shah P, Zargar SA, Javaid G, Yattoo GN, Shah A, Mustafa F. Left-sided hepatic resection for hepatolithiasis: a longitudinal study of 110 patients. HPB (Oxford). 2012;14:764-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Tsunoda T, Tsuchiya R, Harada N, Yoshino R, Noda T, Izawa K, Yamaguchi T, Yamamoto K. Long-term results of surgical treatment for intrahepatic stones. Jpn J Surg. 1985;15:455-462. [PubMed] |
| 19. | Tsuyuguchi T, Miyakawa K, Sugiyama H, Sakai Y, Nishikawa T, Sakamoto D, Nakamura M, Yasui S, Mikata R, Yokosuka O. Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy. J Hepatobiliary Pancreat Sci. 2014;21:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Ti TK, Wong CW, Yuen R, Karunanithy R. The chemical composition of gallstones: its relevance to surgeons in Southeast Asia. Ann Acad Med Singapore. 1996;25:255-258. [PubMed] |
| 21. | Nakayama F. Intrahepatic calculi: a special problem in East Asia. World J Surg. 1982;6:802-804. [PubMed] |
| 22. | Nakayama F. [Hepatolithiasis. Classification of hepatolithiasis and its statistical distribution in Japan]. Nihon Rinsho. 1987;45:1560-1563. [PubMed] |
| 23. | Matsumoto Y, Fujii H, Yoshioka M, Sekikawa T, Wada T, Yamamoto M, Eguchi H, Sugahara K. Biliary strictures as a cause of primary intrahepatic bile duct stones. World J Surg. 1986;10:867-875. [PubMed] |
| 24. | Qian NS, Liao YH, Cai SW, Raut V, Dong JH. Comprehensive application of modern technologies in precise liver resection. Hepatobiliary Pancreat Dis Int. 2013;12:244-250. [PubMed] |
| 25. | Sato F, Igami T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, Nagino M. A study of the right intersectional plane (right portal scissura) of the liver based on virtual left hepatic trisectionectomy. World J Surg. 2014;38:3181-3185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Otegbayo JA, Xu Z S- Editor: Ma YJ L- Editor: Webster JR E- Editor: Wang CH