Published online Feb 21, 2015. doi: 10.3748/wjg.v21.i7.2131
Peer-review started: June 16, 2014
First decision: June 27, 2014
Revised: July 9, 2014
Accepted: August 13, 2014
Article in press: August 18, 2014
Published online: February 21, 2015
Processing time: 240 Days and 5.4 Hours
AIM: To identify risk factors of actual appendiceal perforation when computed tomography (CT) scans suggest nonperforated appendicitis and accordingly determine surgical priority.
METHODS: We collected database of 1362 patients who underwent an appendectomy for acute appendicitis between 2006 and 2013. A single radiologist selected 1236 patients whose CT scans were suggestive of nonperforated appendicitis. Patients were divided into 2 groups: actual nonperforation group and actual perforation group according to intraoperative and pathologic features. Comparison of the 2 groups were made using binary logistic regression.
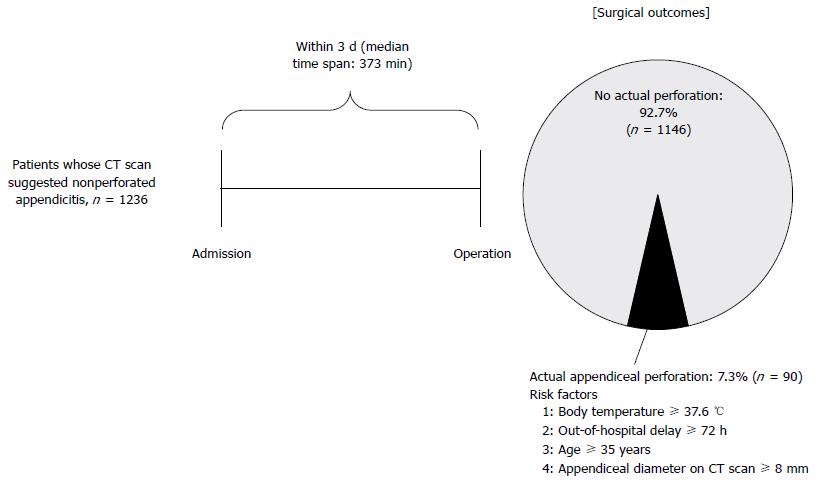
RESULTS: Of 1236 patients, 90 (7.3%) were found to have actual appendiceal perforation. Four risk factors related with actual appendiceal perforation were identified: body temperature ≥ 37.6 °C (HR = 1.912, 95%CI: 1.161-3.149; P = 0.011), out-of-hospital symptom duration ≥ 72 h (HR = 2.454, 95%CI: 1.292-4.662; P = 0.006), age ≥ 35 years (HR = 3.358, 95%CI: 1.968-5.728; P < 0.001), and appendiceal diameter on CT scan ≥ 8 mm (HR = 4.294, 95%CI: 1.034-17.832; P = 0.045). Actual appendiceal perforation group showed longer operation time, later initiation of diet, longer use of parenteral narcotics, longer hospital stay, and higher incidence of postoperative complications (P < 0.05).
CONCLUSION: We proposed here new criteria to select patients with adverse clinical outcomes after appendectomy among the patients with radiologically nonperforated appendicitis. Surgical appendectomy outcomes could be improved by determining the surgical priority according to our criteria.
Core tip: This study analyzed surgical outcomes of 1236 patients whose computed tomography (CT) scans were suggestive of nonperforated appendicitis, and showed in-hospital gross perforation rate was very low (7.3%) and it was predicted by several factors: body temperature ≥ 37.6 °C, out-of-hospital symptom duration ≥ 7 d, age ≥ 35 years, and appendiceal diameter on CT scan ≥ 8 mm. Therefore, determining operative priority based on risk factors of in-hospital perforation is expected to improve surgical outcomes by reducing perforation rates.
- Citation: Lee SC, Park G, Choi BJ, Kim SJ. Determination of surgical priorities in appendicitis based on the probability of undetected appendiceal perforation. World J Gastroenterol 2015; 21(7): 2131-2139
- URL: https://www.wjgnet.com/1007-9327/full/v21/i7/2131.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i7.2131
Appendicitis is the most frequently encountered surgical emergency worldwide, and early appendectomy has been advocated as the therapeutic gold standard to avoid complications. Patients with appendicitis present to the hospital at any time of day or night. However, appendectomies are not performed evenly at all times. A report indicated that although 41% of patients visited the emergency room between 11 PM and 8 AM, only 6% of operations were performed during that period, showing inconsistent durations between the patient visit and operative timing[1]. Besides the hospital visiting hour, appendectomy timing is inconsistently determined by various factors. Therefore, guidelines for the optimal timing of appendicitis are necessary.
The incidence of appendiceal perforation has been reported to range from 17% to 32%[2-6]. Appendiceal perforation dramatically increases morbidity in terms of extended treatment with antibiotics, greater risk of complications, and longer hospital stays[3,7-9]. Surgical priority of grossly perforated appendicitis is not as high as imminent perforation because gross contamination has already occurred. However, cases of microperforated or nonperforated appendicitis should be treated promptly according to the surgical priority, which should be determined based on the risk of gross perforation.
Abdominal computed tomography (CT) scan is widely used for predicting both the presence of appendicitis and its perforation. However, in a study, CT was found to have a low sensitivity (62%) in predicting appendiceal perforation[10]. This could mean that a considerable number of patients with perforated appendicitis could be incorrectly diagnosed radiologically as nonperforated. However, these patients require prompt operation because they are at the risk of progression to gross contamination.
In this study, of the patients with radiologically nonperforated appendicitis, we selected patients with actual perforation evidenced by the operative and pathologic features. We then showed here these patients manifested adverse clinical outcomes. Finally, we intended to determine risk factors that could be useful in predicting actual perforation based on the clinical criteria in patients whose CT scans suggested nonperforated appendicitis.
This study was a retrospective analysis of patients who underwent operations for acute appendicitis at the Department of Surgery of Daejeon St. Mary’s Hospital, the Catholic University of Korea, between January 2006 and December 2013. Daejeon St. Mary’s Hospital is a teaching community hospital with residents on call and supervised by attending surgeons. The study was approved by the ethics committee of Daejeon St. Mary’s Hospital, the Catholic University of Korea (IRB code: DC13RISI0004). The data were gathered from the electronic medical records.
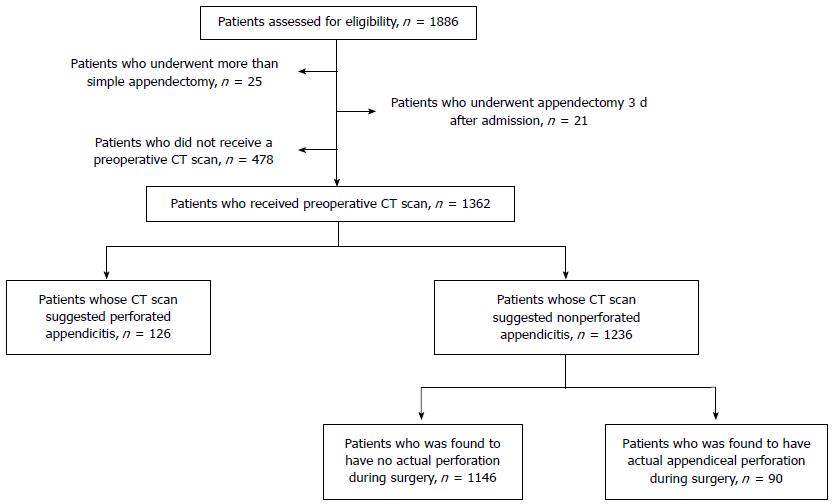
Patients who underwent appendectomy with the impression of nonperforated appendicitis based on preoperative CT scan were the object of our study (Figure 1). During the aforementioned period, 1886 patients underwent operations for appendicitis treatment. Of these, we first excluded the patients who underwent procedures other than simple appendectomy, such as resection of a part of small or large intestine (n = 25). We then excluded patients who underwent appendectomy ≥ 3 d after initial presentation (n = 21). In addition, we excluded patients who did not receive a preoperative CT scan (n = 478). Consequently, 1362 patients remained who received CT scan and thereafter underwent appendectomy. The following step was to differentiate between nonperforated and perforated appendicitis based on the preoperative CT scans. We used an evidence-based definition of perforated appendicitis after a thorough review of the literature; the CT feature of appendiceal perforation was defined as the presence of a hole in the appendix or a fecalith in the abdomen[10,11]. CT images were re-evaluated by one radiologist (G. Park) with ≥ 10 years of experience in abdominal imaging. To avoid selection bias, the radiologist was not given information about the patient’s final diagnosis. The radiologist was provided the CT images in a random sequence created by Picture Archiving and Communication System software (PACS, Maroview, Infinitt, Seoul, Korea) in stack mode. After re-evaluation of CT images, 1236 patients were selected whose CT scan did not suggest a appendiceal perforation. We then divided this patient population into 2 groups: patients with actual appendiceal perforation and those without actual perforation (control group) according to the intraoperative and pathologic features. Thereafter, we investigated whether there were differences in clinical, radiological, and pathologic characteristics between both groups.
Actual appendiceal perforation was defined (1) when an appendicolith was detected outside the appendix; (2) when pus or abscess fluid was evidenced around appendix with disruption of appendiceal wall continuity in the initial operative field without manipulation; or (3) when pus or abscess fluid was evidenced around appendix during surgery and the pathologic diagnosis indicated gangrenous appendicitis or periappendiceal abscess.
Out-of-hospital delay was defined as the time interval between development of initial symptom and the visit to hospital. Time to incision was defined as the time interval between arrival to the hospital and the performance of surgical incision. Comorbidities were assessed with the Charlson comorbidity index[12]. Postoperative complications were classified as described by Clavien[13]. whereby grade 1 represents deviation from the normal postoperative course without the need of pharmacological or any other intervention; grade 2 represents the requirement of pharmacological treatment; grade 3 represents surgical, endoscopic, or radiological intervention; and grade 4 represents a life-threatening complication requiring intensive care unit management. Of the postoperative complications, renal dysfunction was defined as postoperative serum creatinine ≥ 1.5 mg/dL in patients who had normal renal function preoperatively. Hepatitis was defined as postoperative serum ALT (alanine transaminase) ≥ 50 IU/L in patients who showed normal preoperative liver function. Hyperamylasemia was defined as postoperative serum amylase ≥ 160 IU/L in patients whose levels were within the normal range preoperatively.
The initial series of this study included patients who had undergone open appendectomy. Soon after, laparoscopic appendectomy with three ports became the norm in the treatment of acute appendicitis. Thereafter, we introduced the single-port laparoscopic surgery (SPLS) for appendectomy in March 2009. Since then, the SPLS replaced the conventional 3-port procedure. The umbilicus was the most typically used incision site, and a vertical incision with a length ranging from 1.5-2.5 cm was most often used. We frequently used commercially ready-made single ports, such as the OCTO port (Dalim Medical Co., Korea) and the Glove port (Sejong Medical Co., Korea). Peritoneal irrigation with copious amounts of saline was performed under direct visualization in all the procedures, and Jackson-Pratt drains were used as needed.
We implemented a standardized perioperative protocol. For all patients with appendicitis, the initial step at the emergency department includes prompt intravenous hydration using crystalloid fluids and intravenous antibiotics (cefotetan 1.0 g). Because cefotetan is administered according to a 24-h dosing schedule, it was administered at the emergency department and not at a specific time before the incision. Thereafter, starting on the first postoperative day, intravenous cefotetan (usually 1.0 g, maximum dose 2.0 g) was usually administered for 1 to 2 d, or longer if needed. All patients with appendiceal perforation received intravenous metronidazole 50 mg/kg coadministration (maximum dose 2 g). Antibiotic change or dosage adjustments were considered when there was no improvement of the clinical parameters, such as body temperature or leukocyte count. All Patients were allowed a clear liquid diet upon returning to the ward, and the diet was advanced as tolerated. Patients received intravenous ketorolac 0.1 mg/kg as needed for pain. Patients were discharged when tolerating a regular diet. At discharge, oral antibiotics (cefaclor or cefcapene) were prescribed for a 3-d period only to the patients with perforated appendicitis.
Numeric data were presented as mean and standard deviation or as median and range. Continuous variables were analyzed using the independent t-test, whereas proportions were compared using Pearson’s χ2 test or Fisher’s exact test, as appropriate. For variables with a non-normal distribution, Wilcoxon rank sum tests were utilized to examine differences in central tendency. Binary logistic regression was used to assess the risk of in-hospital perforation while controlling for other independent variables. All P values were 2-tailed. Statistical analysis was performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL). Statistical significance was accepted for P values < 0.05.
Of the total 1236 patients whose CT scans suggested nonperforated appendicitis, 1146 (92.7%) were proven to have nonperforated appendicitis and 90 (7.3%) were proven to have actual perforated appendicitis. There were 612 men and 624 women. The median patient age was 37 (range, 15-93) years. The median body mass index was 22.6 (15.1-44.1) kg/m2. Median time to incision was 373 (48-4285) min. There were differences between the mean and median values of time-to-incision to some extent. While the mean time-to-incision was 534 ± 498 min, the median time-to-incision was 373 (48-4285) min. These results could be attributed to the small number of patients who were operated with a long delay, which translated into a deviation of the mean values to the right. Overall, there were 6 (0.5%) open appendectomies, 932 (75.4%) multiport laparoscopic appendectomies, and 298 (24.1%) single-port laparoscopic appendectomies.
Table 1 shows the comparison of patient demographic and baseline characteristics between the two groups. We found that both groups had differences in age, body temperature, serum neutrophil fraction, and appendiceal diameter on CT scan. Patients with actual appendiceal perforation were older (> 35 years of age, 80% vs 53.1%, P < 0.001) and had a body temperature > 37.7 ºC (28.9% vs 15.8%, P < 0.05), neutrophil fraction > 65% (88.9% vs 79.7%, P < 0.05), and appendiceal diameter > 8 mm (97.8% vs 88.7%, P < 0.05). Both groups were similar with respect to sex, body mass index, comorbidity, and out-of-hospital delay. We were also unable to identify a significant difference in time-to-incision [534.6 ± 498.9 min (nonperforation group) vs 521.2 ± 487.4 min (actual perforation group), not significant].
| All patients(n = 1236) | No actual appendiceal perforation(n = 1146) | Actual appendiceal perforation(n = 90) | P value | |
| Age (yr) | < 0.001 | |||
| 15-35 | 556 (45.0) | 538 (46.9) | 18 (20.0) | |
| 35-65 | 515 (41.7) | 471 (41.1) | 44 (48.9) | |
| ≥ 65 | 165 (13.3) | 137 (12.0) | 28 (31.1) | |
| Sex | 0.125 | |||
| Men | 612 (49.5) | 560 (91.5) | 586 (93.9) | |
| Women | 624 (50.5) | 52 (8.5) | 38 (6.1) | |
| Body-mass index (kg/m2) | 0.186 | |||
| < 20 | 255 (20.6) | 239 (20.9) | 16 (17.8) | |
| 20-25 | 673 (54.4) | 627 (54.7) | 46 (51.1) | |
| ≥ 25 | 308 (25.0) | 280 (24.4) | 28 (31.1) | |
| Comorbidity | 0.097 | |||
| Charlson index = 0 | 1142 (92.4) | 1063 (92.8) | 79 (87.8) | |
| Charlson index > 0 | 94 (7.6) | 83 (7.2) | 11 (12.2) | |
| Out-of-hospital delay1 | 0.118 | |||
| < 72 h | 874 (70.7) | 817 (71.3) | 57 (63.3) | |
| ≥ 72 h | 362 (29.3) | 329 (28.7) | 33 (36.7) | |
| Body temperature (°C) | 0.003 | |||
| < 37.6 | 1029 (83.3) | 965 (84.2) | 64 (71.1) | |
| ≥ 37.6 | 207 (16.7) | 181 (15.8) | 26 (28.9) | |
| Presenting symptom | 0.640 | |||
| Abdominal pain | 1209 (97.8) | 1121 (97.8) | 88 (97.8) | |
| Nausea, vomiting | 14 (1.1) | 13 (1.2) | 1 (1.1) | |
| Fever/chill | 12 (1.0) | 12 (1.0) | 0 (0.0) | |
| Indigestion | 1 (0.1) | 0 (0.0) | 1 (1.1) | |
| Lab. findings, median (range) | ||||
| WBC count (× 103/mm3) | 12.0 (1.9-28.7) | 11.9(1.9-28.4) | 13.8 (4.3-28.7) | 0.128 |
| Platelet count (× 103/mm3) | 222 (82-587) | 223 (82-857) | 215 (93-503) | 0.102 |
| Neutrophil fraction | 0.038 | |||
| < 65% | 244 (19.7) | 234 (20.4) | 10 (11.1) | |
| ≥ 65% | 992 (80.3) | 912 (79.6) | 80 (88.9) | |
| Appendix diameter (CT scan) | 0.004 | |||
| < 8 mm | 131 (10.6) | 129 (11.3) | 2 (2.2) | |
| ≥ 8 mm | 1105 (89.4) | 1017 (88.7) | 88 (97.8) | |
| Presence of appendicolith (CT scan) | 0.502 | |||
| No | 1086 (87.9) | 1009 (88.0) | 77 (85.6) | |
| Yes | 150 (12.1) | 137 (12.0) | 13 (14.4) | |
| Time-to-incision (min)2 | 0.860 | |||
| mean ± SD | 534 ± 498 | 535 ± 499 | 521 ± 487 | |
| Median (range) | 373 (48-4285) | 373 (48-4285) | 362 (70-3194) | |
To identify independent factors related with actual appendiceal perforation, consequent multivariate analysis was performed using preoperative variables (Table 2). By multivariate analysis, we identified independent factors related with actual appendiceal perforation, including body temperature (< 37.6 °C vs≥ 37.6 °C), out-of-hospital delay (< 72 h vs≥ 72 h), age (< 35 years vs≥ 35 years), and appendiceal diameter (< 8 mm vs≥ 8 mm). Using these 4 risk factors related with actual appendiceal perforation, we further stratified patients into 3 groups: low-risk (risk factor: 0-1), intermediate-risk (risk factors: 2), and high-risk group (risk factors: 3-4) (Table 3). The probability of actual appendiceal perforation increased 4.8 times in the intermediate-risk group and 10.7 times in the high-risk group compared to the control group (low-risk group).
| Hazard ratio | 95%CI | P value | |
| Body temperature (°C) | 0.011 | ||
| < 37.6 (standard) | 1 | ||
| ≥ 37.6 | 1.912 | 1.161-3.149 | |
| Out-of-hospital delay (h) | 0.006 | ||
| < 72 (standard) | 1 | ||
| ≥ 72 | 2.454 | 1.292-4.662 | |
| Age (yr) | < 0.001 | ||
| < 35 (standard) | 1 | ||
| ≥ 35 | 3.358 | 1.968-5.728 | |
| Appendiceal diameter on CT scan(mm) | 0.045 | ||
| < 8 (standard) | 1 | ||
| ≥ 8 | 4.294 | 1.034-17.832 |
| Groups | No. of risk factors1 | Ratio of patients with perforation vs total population | Hazard ratio of perforation | 95%CI | P value |
| Control group | 0-1 | 1 | |||
| Intermediate risk group | 2 | 52/581 (9.0%) | 4.8 | 2.416-9.563 | < 0.001 |
| High risk group | 3-4 | 28/156 (17.9%) | 10.7 | 5.064-22.596 | < 0.001 |
To determine the effects of actual appendiceal perforation in patients whose initial CT scans suggested nonperforated appendicitis, intraoperative and postoperative variables were compared (Table 4). There were no differences in operative methods between both groups. However, the actual perforation group had a longer operation time (71.2 ± 30.1 min vs 61.1 ± 24.4 min, P < 0.001) and higher incidence of drain insertion (23.3% vs 9.2%, P < 0.001). Furthermore, the actual perforation group had delayed postoperative recovery, which was evidenced by a later initiation of free oral fluids, solid diet, longer use of parenteral narcotics, and longer hospital stay (P < 0.05). However, readmission rates were comparable between the two groups.
| All patients(n = 1236) | No actual appendiceal perforation(n = 1146) | Actual appendiceal perforation(n = 90) | P value | |
| Surgical technique | 0.111 | |||
| Open appendectomy | 6 (0.5) | 5 (0.5) | 1 (1.1) | |
| Lap. appendectomy | ||||
| Multiport | 930 (75.3) | 857 (74.8) | 73 (81.1) | |
| Single-port | 299 (24.2) | 283 (24.7) | 16 (17.8) | |
| Operation time (min) | < 0.001 | |||
| Mean ± SD | 61.8 ± 25.0 | 61.1 ± 24.4 | 71.2 ± 30.1 | |
| Median (range) | 55 (15-230) | 55.0 (15-230) | 65.0 (35-200) | |
| Drain insertion | < 0.001 | |||
| No | 1110 (89.8) | 1041 (90.8) | 69 (76.7) | |
| Yes | 126 (10.2) | 105 (9.2) | 21 (23.3) | |
| Duration prior free oral fluids | 0.001 | |||
| Mean ± SD | 1.3 ± 0.7 | 1.2 ± 0.6 | 1.6 ± 0.6 | |
| Median (range) | 1 (1-7) | 1 (1-7) | 1 (1-6) | |
| Duration prior soft diet | < 0.001 | |||
| Mean ± SD | 1.5 ± 0.9 | 1.47 ± 0.9 | 1.92 ± 1.1 | |
| Median (range) | 1 (1-8) | 1 (1-8) | 2 (1-8) | |
| Dosage of analgesics | 0.054 | |||
| Mean ± SD | 1.58 ± 3.8 | 1.48 ± 3.5 | 2.83 ± 6.5 | |
| Median (range) | 1 (0-70) | 1 (0-70) | 1 (0-50) | |
| Analgesics duration, median (d) | 0.007 | |||
| Mean ± SD | 0.77 ± 1.8 | 0.72 ± 1.7 | 1.4 ± 2.2 | |
| Median (range) | 0.0 (0-42) | 0.0 (0-42) | 1 (0-15) | |
| Postoperative complications | ||||
| Severe complications (grade 3-4) | 16 (1.3) | 14 (1.2) | 7 (7.8) | < 0.001 |
| Total complications | 94 (7.6) | 113 (9.9) | 20 (22.2) | 0.014 |
| Postoperative hospital stay (d) | < 0.001 | |||
| Mean ± SD | 4.02 ± 2.3 | 3.92 ± 2.3 | 5.2 ± 2.9 | |
| Median (range) | 4 (1-48) | 3 (1-48) | 4 (2-17) | |
| Readmissions | 0.714 | |||
| No | 1210 (97.9) | 1122 (97.9) | 88 (97.8) | |
| Yes | 26 (2.1) | 24 (2.1) | 2 (2.2) |
We then classified postoperative complications according to Clavien’s proposal (Table 5). The actual perforation group had higher incidence of grade 2 (14.4% vs 8.2%, P = 0.051), grade 3 (7.8% vs 1.2%, P < 0.001), and total number of complications (22.2% vs 9.9%, P < 0.05). The difference in the complication rates was more marked for grade 3 complications. Grade 3 complications were observed in 1.2% of patients in the control group and 7.8% in the actual perforation group. We experienced 21 reoperations in this study: 14 and 7 in the control and actual perforation groups, respectively. All grade 3 complications in both groups resulted in reoperation, possibly owing to our propensity to adopt a more rapid and definitive management; therefore, the actual perforation group also had a significantly higher reoperation rate (P < 0.001). Regardless of perforation, intra-abdominal abscess (n = 14) was the leading cause of reoperation, and intestinal obstruction (n = 6) was the second.
| No actual appendiceal perforation (n = 1146) | Actual appendiceal perforation (n = 90) | P value | |
| Grade 1, n (%) | 5 (0.8) | 0 (0.0) | 1.000 |
| Renal dysfunction | 1 | 0 | |
| Hepatitis | 1 | 0 | |
| Hyperamylasemia | 3 | 0 | |
| Grade 2, n (%) | 94 (8.2) | 13 (14.4) | 0.051 |
| Wound infection | 72 | 8 | |
| Urinary retention | 11 | 1 | |
| Delayed gastric emptying | 6 | 2 | |
| Pneumonia | 2 | 0 | |
| Pleural effusion | 2 | 2 | |
| Renal dysfunction | 1 | 0 | |
| Grade 3, n (%) | 14 (1.2) | 7 (7.8) | |
| Intra-abdominal abscess | 9 | 5 | |
| Intestinal obstruction (ileus) | 4 | 2 | |
| Intra-abdominal hemorrhage | 1 | 0 | |
| Severe complications (grade 3-4), n (%) | 14 (1.2) | 7 (7.8) | < 0.001 |
| Total complications, n (%) | 113 (9.9) | 20 (22.2) | 0.014 |
Although the presence of appendiceal perforation has a considerable effect on the prognosis of appendicitis, the diagnostic yield of appendiceal perforation by abdominal CT is considerably low. A previous study reported that CT had a sensitivity of 62% and specificity of 81% in predicting appendiceal perforation[10]. In the present study, 7.3% (90/1236) of patients with nonperforated appendicitis on CT images were found to have an actual perforation. Importantly, the patients in the actual perforation group definitely showed adverse clinical outcomes. Therefore, a prompt surgical intervention could improve surgical outcomes among such a patient population (Figure 2).
In our study, we attempted to find independent factors that could be useful in discriminating between actual nonperforation and actual perforation in patients diagnosed with nonperforation radiologically. Time-to-incision did not affect the perforation, which suggests a low possibility of in-hospital perforation. Notably, we found four independent factors that can be useful to determine the presence of appendiceal perforation: body temperature ≥ 37.6 °C, out-of-hospital symptom duration ≥ 72 h, age ≥ 35 years, and appendiceal diameter on CT scan ≥ 8 mm. Based on the number of these risk factors, we were able to classify the patients into 3 groups: low-risk (risk factor: 0-1), intermediate risk (risk factors: 2), and high-risk (risk factors: 3-4) groups. The high-risk group had 10.7 times higher probability of actual perforation than the low-risk group.
There have been a number of controversies over the appropriate timing of appendectomy for acute appendicitis. Proponents of prompt appendectomy emphasize the time dependency of pathologic grade and complication rates[14-18]. Ditillo et al[19] reported in an analysis of 1081 patients with acute appendicitis that the risk of developing advanced pathology and complications increased with time-to-treatment, favoring prompt appendectomy. In contrast, Kearney et al[4] reported that the stage of appendicitis was affected by out-of-hospital delay, but not by in-hospital delay. These differences may be attributed to variations in study design, patient characteristics, and inclusion/exclusion criteria. Therefore, further clarification of the optimal operation timing is required. Our results do not fully support either timing; rather, we support prompt appendectomy for the selected patients who have high-risk factors for actual perforation.
Appendicitis is largely initiated by the luminal obstruction by inspissated stool (fecalith or appendicolith) or lymphoid hyperplasia[20]. Luminal obstruction promotes bacterial overgrowth and increases mucus secretion, leading to intraluminal distention and wall pressure elevation. Subsequently, blood and lymphatic flow are impaired, and mucosal ischemia follows. These events collectively lead to the progression of inflammation, such as gangrene and perforation. In our study, patients with actual perforation showed longer operation time, delayed initiation of postoperative diet, longer and higher doses of postoperative analgesics, higher incidences of postoperative complications, and a longer hospital stay. Therefore, performing appendectomy before its perforation is crucial in the treatment of appendicitis.
In conclusion, our study showed that actual appendiceal perforation occurred in 7.3% (90/1236) of the patients whose CT scans suggested nonperforated appendicitis. The actual perforation group showed inferior clinical outcomes. These patients require prompt operation because they are at the risk of progression to gross contamination. We detected four independent factors that can predict perforated appendicitis even though the CT scans of the patients suggest nonperforated appendicitis: body temperature ≥ 37.6 °C, out-of-hospital symptom duration ≥ 72 h, age ≥ 35 years, and appendiceal diameter on CT scan ≥ 8 mm. We think that surgical outcomes of appendectomy could be improved by following our guidelines for the determination of surgical priority based on the sum of the risk factors.
Although the presence of appendiceal perforation has a considerable effect on the prognosis of appendicitis, the diagnostic yield of appendiceal perforation by abdominal computed tomography (CT) is considerably low. Therefore, clinicians frequently encounter patients have perforated appendicitis in the operation room, even though their preoperative CT scans suggested nonperforated appendicitis.
Appendiceal perforation is an event provoking appendicitis progression from a local disease to an extensive or systemic disease. Therefore, it should be clearly characterized. To prevent or promptly manage it, the identification of risk factors related with appendiceal perforation is particularly important.
To improve the accuracy of CT scans in predicting perforated appendicitis, several CT features favoring perforated appendicitis have been proposed. However, improving predictability of perforated appendicitis using clinical manifestations has not been attempted. The authors herein proposed new criteria to select patients with adverse clinical outcomes after appendectomy among the patients with radiologically nonperforated appendicitis.
The authors have developed novel and simple criteria to predict actual perforated appendicitis in patients whose CT scans suggested nonperforated appendicitis: body temperature ≥ 37.6 °C, out-of-hospital symptom duration ≥ 72 h, age ≥ 35 years, and appendiceal diameter on CT scan ≥ 8 mm. The authors were able to classify the patients into 3 groups based on the number of risk factors: low-risk (risk factor: 0-1), intermediate risk (risk factors: 2), and high-risk (risk factors: 3-4) groups. The high-risk group had 10.7 times higher probability of actual appendiceal perforation than the low-risk group. The authors criteria could be particularly advantageous in the determination of surgical priority or when encountered with indeterminate CT features for appendiceal perforation.
This is a good paper, with a very good and rigorous design, with clear definitions of variables and interesting information obtained from an absolutely correct statistical analysis, bi and multivariate. Leaving apart minor corrections that may be easily remedied, it is born from a weak hypothesis and perhaps it must be otherwise designed and conceived. Information obtained from this design must be utilized as it is really interesting, and only a few reports have given such a good approximation to risk factors of perforated appendicitis in the presence of a normal CT.
| 1. | Yardeni D, Hirschl RB, Drongowski RA, Teitelbaum DH, Geiger JD, Coran AG. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004;39:464-469; discussion 464-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg. 1997;174:723-726; discussion 723-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, Steele SR, Symons RG, Thirlby R. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008;248:557-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 155] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Kearney D, Cahill RA, O’Brien E, Kirwan WO, Redmond HP. Influence of delays on perforation risk in adults with acute appendicitis. Dis Colon Rectum. 2008;51:1823-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Pittman-Waller VA, Myers JG, Stewart RM, Dent DL, Page CP, Gray GA, Pruitt BA, Root HD. Appendicitis: why so complicated? Analysis of 5755 consecutive appendectomies. Am Surg. 2000;66:548-554. [PubMed] |
| 6. | Sleem R, Fisher S, Gestring M, Cheng J, Sangosanya A, Stassen N, Bankey P. Perforated appendicitis: is early laparoscopic appendectomy appropriate? Surgery. 2009;146:731-737; discussion 737-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Eldar S, Nash E, Sabo E, Matter I, Kunin J, Mogilner JG, Abrahamson J. Delay of surgery in acute appendicitis. Am J Surg. 1997;173:194-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 114] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Fahim F, Shirjeel S. A comparison between presenatation time and delay in surgery in simple and advanced appendicitis. J Ayub Med Coll Abbottabad. 2005;17:37-39. [PubMed] |
| 9. | Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults. A prospective study. Ann Surg. 1995;221:278-281. [PubMed] |
| 10. | Fraser JD, Aguayo P, Sharp SW, Snyder CL, Rivard DC, Cully BE, Sharp RJ, Ostlie DJ, St Peter SD. Accuracy of computed tomography in predicting appendiceal perforation. J Pediatr Surg. 2010;45:231-234; discussion 234-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | St Peter SD, Sharp SW, Holcomb GW, Ostlie DJ. An evidence-based definition for perforated appendicitis derived from a prospective randomized trial. J Pediatr Surg. 2008;43:2242-2245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 185] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 12. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [PubMed] |
| 13. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [PubMed] |
| 14. | Paulsamy S, Sivakumar R, Balasubramaniam V, Arumugasamy K, Nagarajan N. Fire Control - A Conservation Tool for certain Medical Plants in Grass Hills Ecosystem, The Western Ghats. Anc Sci Life. 2001;20:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Bickell NA, Aufses AH, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg. 2006;202:401-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 223] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 16. | Busch M, Gutzwiller FS, Aellig S, Kuettel R, Metzger U, Zingg U. In-hospital delay increases the risk of perforation in adults with appendicitis. World J Surg. 2011;35:1626-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Krebs DL, Denton K. Toward a more pragmatic approach to morality: a critical evaluation of Kohlberg’s model. Psychol Rev. 2005;112:629-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 190] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 18. | Udgiri N, Curras E, Kella VK, Nagpal K, Cosgrove J. Appendicitis, is it an emergency? Am Surg. 2011;77:898-901. [PubMed] |
| 19. | Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann surg. 2006;244:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 190] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 20. | Prystowsky JB, Pugh CM, Nagle AP. Current problems in surgery. Appendicitis. Curr Probl Surg. 2005;42:688-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Aranda-Narvaez JM S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN