Published online Feb 14, 2015. doi: 10.3748/wjg.v21.i6.2000
Peer-review started: May 19, 2014
First decision: June 10, 2014
Revised: June 28, 2014
Accepted: July 29, 2014
Article in press: July 30, 2014
Published online: February 14, 2015
Processing time: 268 Days and 18.7 Hours
Bile duct stones are a serious and the third most common complication of the biliary system that can occur following liver transplantation. The incidence rate of bile duct stones after liver transplantation is 1.8%-18%. The management of biliary stones is usually performed with endoscopic techniques; however, the technique may prove to be challenging in the treatment of the intrahepatic bile duct stones. We herein report a case of a 40-year-old man with rare, complex bile duct stones that were successfully eliminated with percutaneous interventional techniques. The complex bile duct stones were defined as a large number of bile stones filling the intra- and extrahepatic bile tracts, resulting in a cast formation within the biliary tree. Common complications such as hemobilia and acute pancreatitis were not present during the perioperative period. The follow-up period was 20 mo long. During the postoperative period, the patient maintained normal temperature, and normal total bilirubin and direct bilirubin levels. The patient is now living a high quality life. This case report highlights the safety and efficacy of the percutaneous interventional approach in the removal of complex bile duct stones following liver transplantation.
Core tip: Bile duct stones are a rare, but serious complication that can occur following liver transplantation and can be very difficult to treat with endoscopic techniques. A case is presented involving a 40-year-old man who developed complex bile duct stones following liver transplantation, with a large number of stones filling the intra- and extrahepatic bile tracts and forming a cast in the biliary tree. The patient’s stones were successfully removed using percutaneous interventional techniques, highlighting the safety and efficacy of this approach in the removal of complex bile duct stones following liver transplantation.
- Citation: Zhou CG, Wei BJ, Gao K, Dai DK, Zhai RY. Successful treatment of complex cholangiolithiasis following orthotopic liver transplantation with interventional radiology. World J Gastroenterol 2015; 21(6): 2000-2004
- URL: https://www.wjgnet.com/1007-9327/full/v21/i6/2000.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i6.2000
Liver transplantation is the only effective method for the treatment of terminal-stage chronic liver diseases. However, there is a high incidence of biliary complications following liver transplantation and long-term, repeated therapies, as the biliary epithelium appears to be more susceptible to ischemia than the liver parenchyma[1,2]. Biliary stones, though uncommon, are a serious complication of orthotopic liver transplantation, which, if not properly treated, may result in severe infection of the biliary tract, liver failure, and even graft loss. The incidence of biliary stones in liver transplant patients varies widely from 1.8%-18%[3-5]. Biliary stones are sometimes managed with interventional radiology, surgery or retransplantation, but most commonly treated with endoscopy[6-9]. The disadvantage of endoscopy is a potential for the development of serious complications such as hemobilia and acute pancreatitis. Furthermore, endoscopy is technically more challenging in the treatment of intrahepatic bile stones. Following stone extraction there is a recurrence rate of 17% within a median of six months[10,11].
Percutaneous interventional techniques represent an alternative approach for the treatment of bile duct stones. These techniques provide a safe and effective approach for the treatment of not only extrahepatic, but also intrahepatic, bile stones. Here, we present a case of rare, complex bile duct stones following orthotopic liver transplantation. The bile duct stones were considered complex, as a large number were found within the intra- and extrahepatic bile tracts, forming a cast in the biliary tree. The removal of bile duct stones was performed successfully using percutaneous interventional techniques. This case report provides an alternative option for managing difficult and serious complications following liver transplantation.
In May 2009, a 40-year-old man underwent classic orthotopic liver transplantation for the treatment of end-stage liver disease secondary to hepatocellular carcinoma from liver cirrhosis. The patient’s post-transplantation recovery was uneventful; however, three months after the surgery his skin and sclera gradually became yellow. The primary diagnosis was obstructive jaundice, which was confirmed by magnetic resonance cholangiopancreatography (MRCP) and cholangiography, and treated with percutaneous transhepatic biliary drainage. In August 2011, due to persistent aggravated jaundice, the patient was referred to our section for further treatment.
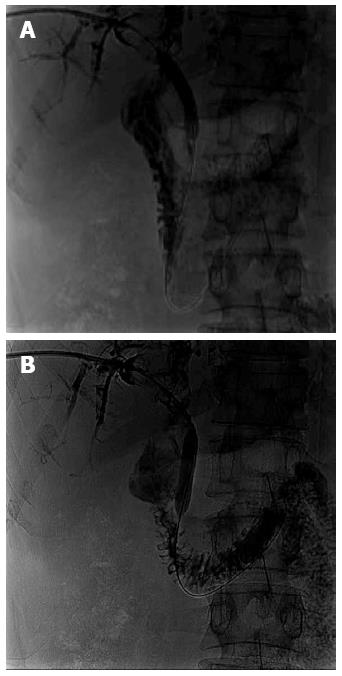
The patient’s medical history showed presence of both hepatitis B and liver cirrhosis. The laboratory examination revealed: total bilirubin, 140 μmol/L (normal, 3.4-20.5 μmol/L); direct bilirubin, 125 μmol/L (normal, 0-6.8 μmol/L); alkaline phosphatase, 152 U/L (normal, 50-136 U/L); gamma-glutamyl transpeptidase, 77 U/L (normal, 5-85 U/L); hepatitis B surface antigen, negative; alpha-fetoprotein, 2.5 ng/mL (normal, 0-13.6 ng/L); and normal total cholesterol and triglyceride levels. The MRCP showed presence of a large number of bile duct stones in the intra- and extrahepatic bile ducts with a mild dilation of the intrahepatic bile duct. Percutaneous transhepatic cholangiography (PTC) showed molding of the intra- and extrahepatic bile ducts into a duct cast by the stones (Figure 1).
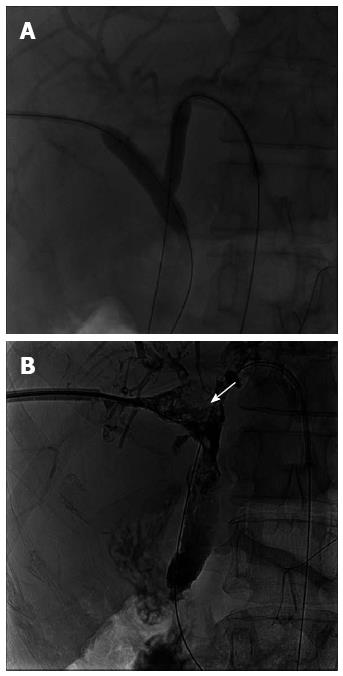
Informed consent was obtained from the patient prior to the interventional procedures. The first procedure was carried out on September 20, 2011. First, a hydrophilic, coated guidewire was used to traverse the stenosis section of the biliary anastomotic stricture entering into the jejunum. Second, an 8 mm × 40 mm balloon catheter (ATB5-35-40-8-4.0; COOK Inc., Bloomington, IN, United States) was placed over the guidewire at the extrahepatic bile duct. Consequently, the extrahepatic bile duct stones were crushed from the proximal to distal bile duct using the inflated balloon catheter (Figure 2). Finally, a biliary tunnel was formed in the biliary cast, and the stone fragments were flushed with a 12 F biliary drainage tube. The procedure was carried out two more times afterwards. The inflated balloon catheter was used to push some of the bigger fragments to the duodenum via balloon sphincteroplasty. On December 5, 2011, a double balloon catheter technique was used for efficient elimination of the intrahepatic bile stones and left side percutaneous transhepatic biliary drainage was performed. Balloon catheters [8 mm × 40 mm and 10 mm × 40 mm (ATB5-35-40-10-4.0; COOK Inc.)] were placed in the left- and right-side bile ducts and simultaneously inflated in order to crush the intrahepatic bile stones. On December 28, 2011, a basket extractor (Nitinol Tipless Stone Extractor, NTSE-030115-UDH-MB; COOK Inc.) was used to cut some of the large residual stones (Figure 3).
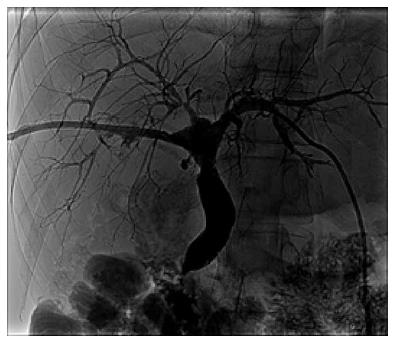
Four months after the percutaneous transhepatic biliary drainage, PTC showed no presence of bile duct stones in either the intra- or extrahepatic or bile ducts. The intrahepatic bile duct was not dilated while the extrahepatic bile duct was mildly dilated (Figure 4). Hence, the left-side drainage tube was removed on April 16, 2012 while the right-side drainage tube was removed on May 23, 2012. All of the procedures were free from complications. The follow-up period was 20 mo (until February 2014). During the postoperative period, the patient maintained normal body temperature, as well as normal levels of total and direct bilirubin. The patient is now able to live a normal life.
Orthotopic liver transplantation is currently the standard therapy for end-stage liver diseases. Despite great improvements in organ preservation, immunosuppression, and surgical techniques, biliary complications (BCs), including non-anastomotic and anastomotic strictures, stone formation, and bile leaks, remain a common source of morbidity. Consequently, patients may undergo long-term and repeated therapies including percutaneous, endoscopic, and surgical procedures. BCs may also increase liver retransplantation rates and influence graft and patient survival rates. The overall incidence of BCs after orthotopic liver transplantation is between 5% and 25%[6]. Although the underlying reasons for the bile stone formation are unknown, some research indicates that anastomotic strictures, bacterial infections, ischemia, elevated total cholesterol, and triglyceride levels could predispose a patient to the formation of biliary stones or sludge[5,6,12].
This case report presents a rare occurrence of complex bile stones following orthotopic liver transplantation and their successful elimination using the percutaneous interventional technique. The case presented a serious situation in which both the intra- and extrahepatic bile ducts were filled with a large number of stones, making their removal by endoscopy difficult. Hence, a series of percutaneous interventional techniques were used in the treatment of the patient. The extrahepatic bile duct stones were crushed with the inflated balloon catheter, and the stone fragments were flushed by a drainage tube. Some of the large stone fragments were pushed into the duodenum via balloon sphincteroplasty. The intrahepatic bile stones were eliminated with the double-balloon catheter technique and a basket extractor was used to cut the large residual stones. The biliary drainage tube was reserved, and ursodeoxycholic acid was administrated to promote biliary excretion and avoid biliary tract infection. Four months later, the bile stones were completely eliminated, and normal liver function was recovered with no perioperative complications. The patient had no clinical symptoms, and the laboratory examinations were normal at the last check-up. The patient is now living a high quality of life.
In conclusion, the percutaneous interventional technique provides a safe and effective treatment of bile stones following orthotopic liver transplantation without commonly associated complications, such as hemobilia or acute pancreatitis. The case presented here demonstrates that the percutaneous interventional technique is especially suitable for the removal of complex bile stones, which are otherwise difficult to treat endoscopically.
A 40-year-old male patient with a history of orthotopic liver transplantation presented with aggravated jaundice.
A large number of bile duct stones filled both the intra- and extrahepatic bile ducts with mild dilation of the intrahepatic bile duct.
Anastomotic stenosis, common bile duct stone, and malignant obstructive jaundice.
Total bilirubin, 140 μmol/L; direct bilirubin, 125 μmol/L; alpha-fetoprotein, 2.5 ng/mL.
Magnetic resonance cholangiopancreatography showed a large number of bile duct stones in the intra- and extrahepatic bile ducts with an associated mild dilation of the intrahepatic bile duct.
The patient was treated with a series of percutaneous interventional procedures.
An endoscopy is commonly used in the management of biliary stones; however, endoscopy may be technically challenging in the treatment of the intrahepatic bile stones.
Complex bile duct stones are defined as a large number of bile stones within the intra- and extrahepatic bile tracts forming a cast in the biliary tree.
This case report emphasizes the safety and efficacy of the percutaneous interventional approach in the removal of complex bile duct stones following liver transplantation.
This article applies a percutaneous interventional technique in the elimination of complex bile duct stones following orthotopic liver transplantation.
| 1. | Noack K, Bronk SF, Kato A, Gores GJ. The greater vulnerability of bile duct cells to reoxygenation injury than to anoxia. Implications for the pathogenesis of biliary strictures after liver transplantation. Transplantation. 1993;56:495-500. [PubMed] |
| 2. | Seehofer D, Eurich D, Veltzke-Schlieker W, Neuhaus P. Biliary complications after liver transplantation: old problems and new challenges. Am J Transplant. 2013;13:253-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 230] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 3. | Yu ZY, Zhang M, Qin YS, Zhou XP, Cai MY, Yu SF, Ke QH, Zheng SS. Risk factors of choledocholithiasis formation after liver transplantation. Hepatobiliary Pancreat Dis Int. 2013;12:215-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Cillo U, Burra P, Norberto L, D’Amico D. Bile duct stones and casts after liver transplantation: Different entities but similar prevention strategy? Liver Transpl. 2008;14:1400-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Spier BJ, Pfau PR, Lorenze KR, Knechtle SJ, Said A. Risk factors and outcomes in post-liver transplantation bile duct stones and casts: A case-control study. Liver Transpl. 2008;14:1461-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol. 2011;34:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 7. | Verdonk RC, Buis CI, Porte RJ, Haagsma EB. Biliary complications after liver transplantation: a review. Scand J Gastroenterol Suppl. 2006;89-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 136] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Arain MA, Attam R, Freeman ML. Advances in endoscopic management of biliary tract complications after liver transplantation. Liver Transpl. 2013;19:482-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Attam R, Freeman ML. Endoscopic papillary large balloon dilation for large common bile duct stones. J Hepatobiliary Pancreat Surg. 2009;16:618-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Thuluvath PJ, Pfau PR, Kimmey MB, Ginsberg GG. Biliary complications after liver transplantation: the role of endoscopy. Endoscopy. 2005;37:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 154] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Chahal P, Baron TH, Poterucha JJ, Rosen CB. Endoscopic retrograde cholangiography in post-orthotopic liver transplant population with Roux-en-Y biliary reconstruction. Liver Transpl. 2007;13:1168-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol. 2008;14:493-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Higuera-de la Tijera MF S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN