Published online Feb 7, 2015. doi: 10.3748/wjg.v21.i5.1670
Peer-review started: June 20, 2014
First decision: July 21, 2014
Revised: August 5, 2014
Accepted: September 19, 2014
Article in press: September 19, 2014
Published online: February 7, 2015
Processing time: 236 Days and 0.3 Hours
A 34-year-old woman presented at our hospital with abdominal distention due to overeating. Acute gastric dilatation was diagnosed. The patient was hospitalized, and nasogastric decompression was initiated. On hospitalization day 3, she developed shock, and her respiratory state deteriorated, requiring intubation and mechanical ventilation. Nasogastric decompression contributed to the improvement in her clinical condition. She was discharged 3 mo after admission. During outpatient follow-up, her dietary intake decreased, and her body weight gradually decreased by 14 kg. An upper gastrointestinal series and endoscopy revealed pyloric stenosis; therefore, we performed gastrojejunostomy 18 mo after her initial admission. The patient was discharged from the hospital with no postoperative complications. Gastric necrosis and perforation due to overeating-induced gastric dilatation are life-threatening conditions. Surgical intervention may be required if delayed pyloric stenosis occurs after conservative treatment. We report a case of pyloric stenosis due to overeating-induced gastric dilatation treated by gastrojejunostomy 18 mo after the initial presentation.
Core tip: Acute gastric dilatation due to overeating may be life-threatening if gastric necrosis or perforation occurs. Therefore, emergency surgery is performed in most cases. This is the first report of a patient who underwent surgery more than a year after initial treatment. The number of patients with eating disorders, such as bulimia, has recently increased. For this reason in particular, physicians should be aware of acute gastric dilatation due to overeating.
- Citation: Kimura A, Masuda N, Haga N, Ito T, Otsuka K, Takita J, Satomura H, Kumakura Y, Kato H, Kuwano H. Gastrojejunostomy for pyloric stenosis after acute gastric dilatation due to overeating. World J Gastroenterol 2015; 21(5): 1670-1674
- URL: https://www.wjgnet.com/1007-9327/full/v21/i5/1670.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i5.1670
Although gastric necrosis or perforation following gastric dilatation is unusual because of the rich blood supply to the stomach, the occurrence of these conditions may be life-threatening. We report our experience with a patient who underwent gastrojejunostomy for pyloric stenosis after presenting with acute gastric dilatation due to overeating. Furthermore, we discuss the recent literature available on the subject.
A 34-year-old woman ate an overly large meal of curry, rice, and potatoes. She gradually developed abdominal distention for which she sought medical attention. The general physician decided on an expectant approach. However, she presented at our hospital because her symptoms did not improve. This patient had a history of episodes of bulimic binging, but she had failed to self-induce vomiting this time.
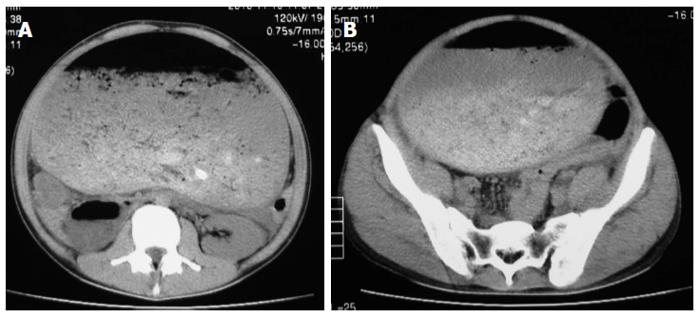
Physical examination at presentation revealed a blood pressure of 117/68 mmHg, a pulse rate of 100 beats/min, and a body temperature of 36.7 °C. Her abdomen was distended, but there were no signs of peritoneal irritation. The significant laboratory test results were as follows: white blood cell count, 16700 cells/μL; C-reactive protein, 2.33 mg/dL; amylase, 1190 IU/L; serum creatinine phosphokinase, 4007 IU/L; blood urea nitrogen (BUN), 15.2 mg/dL; and creatinine, 2.33 mg/dL. Abdominal computed tomography scans revealed a massive dilation of the stomach reaching the pelvis but with no ascites or free air (Figure 1). We made a diagnosis of acute gastric dilatation due to overeating without gastric perforation or necrosis.
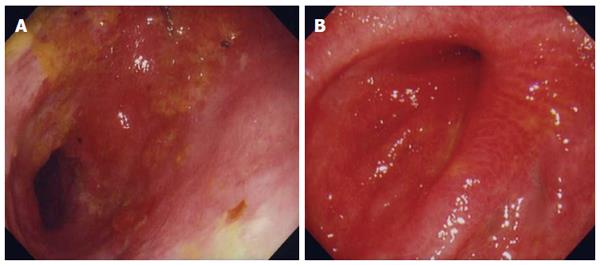
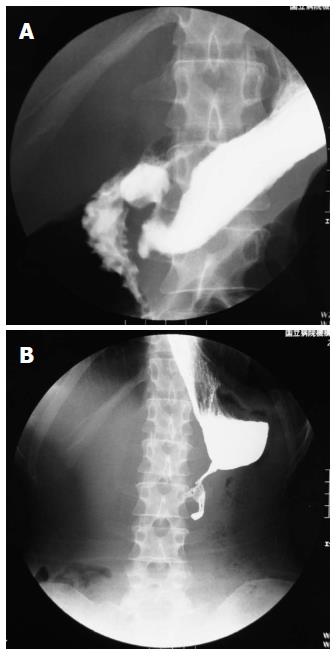
A nasogastric tube was inserted, and decompression and irrigation were initiated. On post-hospitalization day 3, the patient developed shock, and her respiratory state worsened. We then performed intubation and initiated mechanical ventilation. The inferior vena cava and diaphragm were compressed by her remarkably distended stomach. Further, decreased venous return and ventilatory impairment aggravated her condition. Although we considered emergency surgery, her general condition promptly improved after fluid resuscitation and respiratory care. Therefore, we continued conservative treatment. Seven days after intubation, we performed a tracheotomy. Her respiratory state gradually improved, and she was extubated 3 wk after intubation. The abdominal distention gradually improved by decompression. Thereafter, upper gastrointestinal (UGI) endoscopy and an UGI series were performed. The UGI endoscopy showed mucosal deciduation at the pyloric antrum (Figure 2A), but the UGI series showed no leakage and good passage of the contrast medium (Figure 3A). Thus, there was no evidence of pyloric stenosis. Tube feeding was initiated on hospitalization day 30 and continued until she was able to eat rice gruel. Three months after admission, she was discharged from our hospital.
While our patient was followed-up as an outpatient, her dietary intake gradually decreased. Although we recommended surgical treatment for her several times during the course of an outpatient, she rejected surgical treatment. Ultimately, she lost 14 kg from her original weight on admission. At present, her height and weight are 160 cm and 40 kg, respectively. However, because the UGI series and endoscopy revealed pyloric stenosis (Figures 2B and 3B), we performed Roux-en-Y gastrojejunostomy 18 mo after the first admission, with her consent. The postoperative course was uneventful, and she was discharged from our hospital 3 wk after surgery. The passage of contrast medium during the postoperative UGI series indicated that the anastomosis was accurate (Figure 4). At two years after surgery, the patient had gained 20 kg.
Acute gastric dilatation is a medical condition in which the stomach becomes progressively hypotonic and overstretched despite the absence of mechanical obstruction[1]. This condition can be caused by overeating, postoperative ileus, child birth, chronic debilitating affection, central nervous system damage, severe infection, and trauma[2]. Among these causes, acute gastric dilatation due to overeating is more common in females with underlying eating disorders, such as anorexia nervosa[3]. The rich collateral blood flow of the stomach generally protects the gastric wall from ischemia; gastric necrosis or perforation following gastric dilatation is unusual. However, a remarkable increase in the intragastric pressure by massive gastric dilatation can decrease the intramural blood flow, resulting in possible gastric necrosis or perforation[4]. Immediate nasogastric decompression and sufficient fluid resuscitation are necessary for the treatment of acute gastric dilatation[5]. These procedures can decrease the intragastric pressure and reduce the risk of necrosis and perforation; therefore, they should be implemented as early as possible. If gastric necrosis or perforation is suspected or if draining the gastric contents is difficult, immediate surgical intervention is required. Resection of the necrotic portion of the stomach is required in some cases, and total gastrectomy is required in others.
In our case, the pyloric stenosis progressed more than a year after initial treatment. The partial necrosis of the gastric wall may have been caused by acute gastric dilatation because the serum creatinine-phosphokinase level increased at onset. We promptly performed nasogastric decompression, which may have prevented complete gastric necrosis and perforation. Because of the increase in the intragastric pressure caused by massive gastric dilatation, the intramural blood flow decreased, resulting in partial necrosis of the gastric mucosa and muscle scarring due to fibrosis. Together, these regenerative processes can lead to pyloric stenosis. In this case, acute gastric dilatation occurred only once. However, the dilatation of the stomach was severe, and it took approximately one month to drain the gastric contents completely. Therefore, delayed pyloric stenosis might have occurred.
From a literature search of the PubMed database between l966 and 2013, in addition to our patient, we retrieved 25 cases of acute gastric dilatation due to overeating (Table 1). The mean age of these patients was 22.7 (range, 4-48) years, indicating a greater frequency among young patients. There were more female patients than males (n = 20 and 5 patients, respectively, with the gender of one patient being unknown). Eighteen patients had underlying eating disorders, such as anorexia or bulimia nervosa. Sixteen patients underwent laparotomy, three of whom underwent total gastrectomy. In contrast, eight patients were treated by nasogastric decompression alone. Eleven patients underwent emergency surgery: three within several hours and one within several days. In most cases, emergency or semi-emergency surgery was performed. To the best of our knowledge, our patient was the first to undergo surgery more than a year after initial treatment. According to our literature search, six patients died despite immediate treatment, including surgical intervention. Despite the many reports of young patients, some patients died shortly after surgery or the onset of symptoms. Therefore, gastric perforation following acute gastric dilatation may be more severe than usually considered.
| Year | Ref. | Age (yr) | Sex | Underlying disease | Duration to surgery | Treatment | Outcome |
| 2000 | Nakao et al[5] | 17 | F | Anorexia nervosa | 8 h | Proximal gastrectomy | Alive |
| 2006 | Barada et al[6] | 24 | F | Anorexia nervosa | NA | Nasogastric tube decompression | Alive |
| 2011 | Kim et al[7] | 26 | F | Eating disorder | NA | Nasogastric tube decompression | Dead |
| 1987 | Abdu et al[8] | 14 | F | None | Emergency | Partial gastrectomy | Alive |
| 1987 | Abdu et al[8] | 17 | F | Eating disorder | Emergency | Total gastrectomy | Dead |
| 1987 | Deret et al[9] | 48 | F | Schizophrenia | 5 h | Total gastrectomy | Alive |
| 1990 | Trott et al[10] | 17 | F | Bulimia nervosa | Emergency | Gastric tube decompression (by laparotomy) | Alive |
| 1992 | Beiles et al[11] | 24 | F | Bulimia nervosa | Emergency | Partial gastrectomy | Alive |
| 1995 | Adson et al[12] | 35 | F | Eating disorder | 2 d | Nasogastric tube decompression (with appendectomy) | Alive |
| 1995 | Adson et al[12] | 30 | F | Bulimia nervosa | NA | Nasogastric tube decompression | Alive |
| 1996 | Willeke et al[13] | 19 | F | Anorexia nervosa | Emergency | Partial gastrectomy | Alive |
| 1998 | Seligmann et al[14] | 31 | F | Bulimia nervosa | NA | Nasogastric tube decompression | Alive |
| 2000 | Qin et al[15] | 12 | F | None | NA | Oral gastric tube decompression | Dead |
| 2000 | Qin et al[15] | 4 | F | None | Emergency | Partial gastrectomy | Alive |
| 2002 | Holtkamp et al[16] | 16 | M | Anorexia nervosa | 8 h | Aspiration of stomach contents (by laparotomy) | Alive |
| 2003 | Turan et al[17] | 18 | M | Mental retardation | Emergency | Total gastrectomy | Dead |
| 2004 | Sinicina et al[18] | 19 | M | Anorexia nervosa | NA | None | Dead |
| 2004 | Mathevon et al[19] | 25 | F | Anorexia nervosa | NA | Nasogastric tube decompression | Alive |
| 2005 | Luncă et al[20] | 22 | M | Mental retardation | NA | Nasogastric tube decompression | Alive |
| 2006 | Gyurkovics et al[21] | 22 | F | Eating disorder | Emergency | Gastrostomy | Dead |
| 2009 | Kashyap et al[22] | 36 | F | Eating disorder | Emergency | Gastrotomy | Alive |
| 2010 | García Salido et al[23] | 16 | Unknown | Anorexia nervosa | NA | Nasogastric tube decompression | Alive |
| 2011 | Hohenauer et al[24] | 21 | F | Psychosis | NA | Nasogastric tube decompression | Alive |
| 2012 | Mishima et al[25] | 12 | M | None | Emergency | Partial gastrectomy | Alive |
| 2012 | Franco-López et al[26] | 31 | F | Bulimia nervosa | Emergency | Gastrotomy | Alive |
| 2012 | Our case | 34 | F | Bulimia nervosa | 1.5 yr | Gastrojejunostomy | Alive |
In conclusion, although acute gastric dilatation due to overeating is rare, physicians should be aware of its potential complications, such as gastric necrosis or perforation. Moreover, if conservative treatment is preferred over surgery, physicians should be aware of the possibility of delayed pyloric stenosis.
A 34-year-old woman developed abdominal distention due to overeating.
The abdomen was distended, but there were no signs of peritoneal irritation.
Gastric perforation, Ascites, Gastric dilatation.
White blood cell count, 16700 cells/μL; C-reactive protein, 2.33 mg/dL; amylase, 1190 IU/L; serum creatinine phosphokinase, 4007 IU/L; blood urea nitrogen, 15.2 mg/dL; and creatinine, 2.33 mg/dL. The results of her liver function tests were within normal limits.
Abdominal computed tomography scans revealed a massively dilated stomach reaching the pelvis without ascites or free air.
Initially, conservative treatment by nasogastric decompression was performed, and Roux-en-Y gastrojejunostomy was performed for delayed pyloric stenosis 18 mo after the first admission.
Twenty-five cases of acute gastric dilatation due to overeating were retrieved from a literature search of the PubMed database of cases between l966 and 2013.
Acute gastric dilatation is a medical condition in which the stomach becomes progressively hypotonic and overstretched, despite the absence of mechanical obstruction.
This study not only presents the importance of immediate treatment for acute gastric dilatation but also describes the possibility of delayed pyloric stenosis after conservative treatment.
The article demonstrated a high mortality rate when performing emergency surgery for acute gastric dilatation due to overeating. Gastrojejunostomy is an interesting option in this situation.
| 1. | Hiraga M, Ono F, Omura N, Sato M, Yamamura A. A case of gastric necrosis and perforation due to overeating-induced gastric dilatation: A case report. J Jpn Surg Assoc. 2012;73:1933-1937. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Kaneda T, Miyazawa H, Kobayashi T, Shimizu N, Katayama M, Sato T. A case of acute gastric dilatation occurring after bulimia while on a diet. J Tokyo Med Univ. 1996;54:66-68. |
| 3. | Natsume S, Terasaki M, Goto Y, Kurumiya Y, Shingu Y. A case of gastric necrosis. J Abdom Emerg Med. 2003;23:1075-1078. |
| 4. | Usuda M, Koizumi M, Kouda H, Nakahara C, Ueki H, Shibazaki S. Gastric necrosis caused by acute gastric dilatation after an episode of bulimia - A case report. Jpn J Gastroenterol Surg. 1998;31:2346-2349. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Nakao A, Isozaki H, Iwagaki H, Kanagawa T, Takakura N, Tanaka N. Gastric perforation caused by a bulimic attack in an anorexia nervosa patient: report of a case. Surg Today. 2000;30:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Barada KA, Azar CR, Al-Kutoubi AO, Harb RS, Hazimeh YM, Abbas JS, Khani MK, Al-Amin HA. Massive gastric dilatation after a single binge in an anorectic woman. Int J Eat Disord. 2006;39:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Kim HH, Park SJ, Park MI, Moon W. Acute gastric dilatation and acute pancreatitis in a patient with an eating disorder: solving a chicken and egg situation. Intern Med. 2011;50:571-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Abdu RA, Garritano D, Culver O. Acute gastric necrosis in anorexia nervosa and bulimia. Two case reports. Arch Surg. 1987;122:830-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Deret C, Leborgne J, Rochedreux A, Jonet D, Heloury Y, Hepner Y. [Gastric fundus necrosis following acute gastric dilatation]. J Chir (Paris). 1987;124:609-611. [PubMed] |
| 10. | Trott GE, Elliger T, Kerscher P, Nissen G. [Acute abdomen in anorexia nervosa. A case report]. Fortschr Med. 1990;108:525-526. [PubMed] |
| 11. | Beiles CB, Rogers G, Upjohn J, Wise AG. Gastric dilatation and necrosis in bulimia: a case report. Australas Radiol. 1992;36:75-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Adson DE, Mitchell JE, Trenkner SW. The superior mesenteric artery syndrome and acute gastric dilatation in eating disorders: a report of two cases and a review of the literature. Int J Eat Disord. 1997;21:103-114. [PubMed] |
| 13. | Willeke F, Riedl S, von Herbay A, Schmidt H, Hoffmann V, Stern J. [Decompensated acute gastric dilatation caused by a bulimic attack in anorexia nervosa]. Dtsch Med Wochenschr. 1996;121:1220-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Seligmann C, Liehr RM, Schwarz A. Massive gastric dilatation after a bulimic excess. Med J Aust. 1998;169:503. [PubMed] |
| 15. | Qin H, Yao H, Zhang J. Gastric rupture caused by acute gastric distention in non-neonatal children: clinical analysis of 3 cases. Chin Med J (Engl). 2000;113:1147-1149. [PubMed] |
| 16. | Holtkamp K, Mogharrebi R, Hanisch C, Schumpelick V, Herpertz-Dahlmann B. Gastric dilatation in a girl with former obesity and atypical anorexia nervosa. Int J Eat Disord. 2002;32:372-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Turan M, Sen M, Canbay E, Karadayi K, Yildiz E. Gastric necrosis and perforation caused by acute gastric dilatation: report of a case. Surg Today. 2003;33:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Sinicina I, Pankratz H, Büttner A, Mall G. Death due to neurogenic shock following gastric rupture in an anorexia nervosa patient. Forensic Sci Int. 2005;155:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Mathevon T, Rougier C, Ducher E, Pic D, Garcier JM, Schmidt J. [Acute abdominal dilatation, a serious complication in the case of anorexia nervosa]. Presse Med. 2004;33:601-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Luncă S, Rikkers A, Stănescu A. Acute massive gastric dilatation: severe ischemia and gastric necrosis without perforation. Rom J Gastroenterol. 2005;14:279-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Gyurkovics E, Tihanyi B, Szijarto A, Kaliszky P, Temesi V, Hedvig SA, Kupcsulik P. Fatal outcome from extreme acute gastric dilation after an eating binge. Int J Eat Disord. 2006;39:602-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Kashyap AS, Chopra D, Anand KP, Arora S, Kashyap S. Acute gastric dilatation. Emerg Med J. 2009;26:326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | García Salido A, Martínez de Azagra A, de la Torre Espí M, Pérez Suárez E, López Neyra A, Cañedo Villarroya E. [Acute gastric dilation due to food gorging: Could be a life-threatening emergency]. An Pediatr (Barc). 2010;73:148-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Hohenauer P, Dünser MW. Massive gastric distension. Wien Klin Wochenschr. 2011;123:592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Mishima T, Kohara N, Tajima Y, Maeda J, Inoue K, Ohno T, Kitasato A, Watanabe T, Irie J, Adachi T. Gastric rupture with necrosis following acute gastric dilatation: report of a case. Surg Today. 2012;42:997-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Franco-López Á, Badillo S, Contreras J. [Acute gastric dilatation in a bulimic patient; systemic efects]. Nutr Hosp. 2012;27:1364-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: de Moura EGH, Sinha R S- Editor: Qi Y L- Editor: A E- Editor: Ma S