Published online Oct 14, 2015. doi: 10.3748/wjg.v21.i38.10824
Peer-review started: April 9, 2015
First decision: June 23, 2015
Revised: July 8, 2015
Accepted: September 14, 2015
Article in press: September 14, 2015
Published online: October 14, 2015
Processing time: 188 Days and 7.7 Hours
As surgical techniques continue to move towards less invasive techniques, single incision laparoscopic surgery (SILS), a hybrid between traditional multiport laparoscopy and natural orifice transluminal endoscopic surgery, was introduced to further the enhanced outcomes of multiport laparoscopy. The safety and feasibility of SILS for both benign and malignant colorectal disease has been proven. SILS provides the potential for improved cosmesis, postoperative pain, recovery time, and quality of life at the drawback of higher technical skill required. In this article, we review the history, describe the available technology and techniques, and evaluate the benefits and limitations of SILS for colorectal surgery in the published literature.
Core tip: As surgical techniques continue to move towards less invasive techniques, single incision laparoscopic surgery (SILS) is a valuable platform with distinct advantages and comparable or better outcomes than other minimally invasive platforms. The safety and feasibility of SILS for both benign and malignant colorectal disease has been proven, and this review of the history, current state, available technology, limitations to widespread use, and their solutions will be a valuable addition to the published literature. It will draw attention to the benefits and potentially increase use of the platform and minimally invasive surgery as a whole.
- Citation: Madhoun N, Keller DS, Haas EM. Review of single incision laparoscopic surgery in colorectal surgery. World J Gastroenterol 2015; 21(38): 10824-10829
- URL: https://www.wjgnet.com/1007-9327/full/v21/i38/10824.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i38.10824
Since the first laparoscopic colectomy was described in 1991, minimally invasive colorectal surgery has continued to grow[1]. The expanding use of laparoscopy has been the greatest technical and clinical advance in the field of colorectal surgery. Laparoscopic colorectal surgery has been proven to improve patient outcomes, including faster return of gastrointestinal function, less postoperative pain, shorter length of stay, lower complication and readmission rates, and lower total healthcare utilization compared to open surgery[1-14]. Despite proven benefits, use of laparoscopy is estimated at only 50% of all colorectal procedures, 20% of colon cancer, and 10% of rectal cancer procedures in the United States[15,16]. Thus, there is room to increase utilization and the benefits. In addition, there is the continued drive towards reduced port and “scarless” surgery, and great efforts have been made to minimize surgical trauma, improving cosmesis and surgery-related pain and morbidity. Techniques, such as natural orifice transluminal endoscopic surgery (NOTES) and single-incision laparoscopy surgery (SILS) have been developed to reach the goals. NOTES is still in the experimental stages, but SILS is ready for incorporation into routine practice and currently regarded as the next major advance in the progression of minimally invasive surgical approaches feasible in generalized use[17,18].
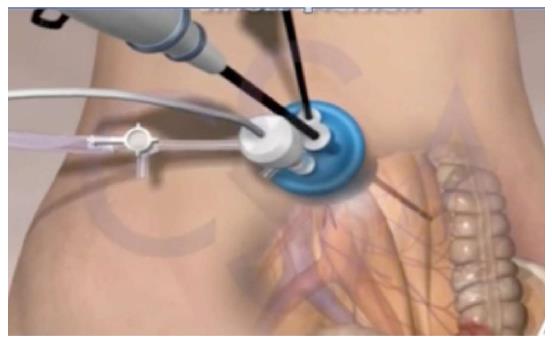
SILS was developed to further the outcomes of multiport laparoscopy. The SILS technique was first reported for colorectal surgery in 2008, when both Remzi et al[19] and Bucher et al[20] reported use for right colectomy. Since that time, multiple studies have proven SILS is safe and feasible for the full array of benign and malignant colorectal disease, and its applications continue to grow[21-35]. SILS is currently regarded as the next major advance in the progression of minimally invasive surgical approaches to colorectal disease suitable for generalized use[17] (Figure 1).
Most SILS procedures enter the peritoneum at the umbilicus, creating a “hidden” incision and allowing the fascial incision to be lengthened without extending the overlying skin incision[36]. If a stoma is planned, the ostomy site may be used for access, allowing “scarless” surgery[23,37,38].
For access, there are several commercially produced SILS ports, as well as a homemade glove port. The most common ports are the SILS™ Port (Covidien, Mansfield, Massachusetts, United States), the GelPOINT® platform (Applied Medical, Rancho Santa Margarita, CA, United States), and the TriPort or QuadPort (Olympus Medical, Center Valley, PA, United States). All devices have three or more working channels in the single port to introduce the laparoscopic instruments and a camera into the operative field through a solitary incision. The single incision helps reduce fascial defects, abdominal wall trauma, and their associated postoperative pain and hernia risk[39-41]. Each port is introduced through a 2-4 cm skin and fascial incision, and has costs and benefits. The SILS™ Port (Covidien, Mansfield, MA, United States) is pliable elastomeric foam that creates a seal with the skin to maintain pneumoperitoneum, offers enhanced mobility, and allows the surgeon to interchange 5-mm and 12-mm ports. However, the SILSTM port is limited to 3 trocars and has no wound protector for specimen extraction. The GelPOINT® uses a wound protector sleeve inserted into the peritoneum and GelSeal® cap that trocars are inserted into per surgeon preference. The port offers a low internal profile, which may help accommodate various abdominal wall sizes, and the sleeve offers protection during specimen extraction from tumor seeding and superficial wound infections[42,43]. The GelPOINT® has a larger profile on the abdominal wall, and may lose pneumoperitoneum with extreme torque. The TriPort and QuadPort channels have three or four instrument channels, respectively, a similar to the GelPOINT®, and a lower external profile. However, the assembly, insertion, and extracorporealization are reported more difficult than other platforms. The glove port uses a sterile, non-latex glove secured to a small wound protector, with the glove’s fingers used for instrument and camera access. This approach is simple, inexpensive, and easily reproducible, but there is a poor seal and lack of rigidity provided from the finger ports compared to commercially available devices[35,44-47].
Standard laparoscopic tools are commonly used with SILS, but straight, curved, and articulating instruments are available. Straight instruments offer rigidity, but when working in a parallel, fixed space, there can be collisions between the working ports and the camera. Curved instruments were introduced to remedy collisions, but they cannot be passed through conventional, straight trocars. Articulating instruments were designed to overcome the lack of triangulation, as they articulate at the tip, rotating 360° around the instrument axis. However, there is a loss of rigidity and tactile feedback with the flexible tools[48-50]. It is generally agreed upon that straight laparoscopic instruments are preferred and the curved or articulating instruments are not required or commonly used in practice.
In all clinical and quality metrics, SILS has comparable outcomes to traditional laparoscopy[34,39]. Studies have proven SILS is feasible and safe for benign and malignant colorectal disease[22,28-30,32,33]. From early reports, SILS had similar postoperative outcomes, including complication, intraoperative conversion, and readmission rates[39]. Oncologic outcomes, including the feasibility of R0 resection, specimen length, number of lymph nodes harvested, and proximal and distal margins were comparable to multiport laparoscopy[51-54]. SILS has been shown safe and feasible specifically in rectal resections[29]. Initial studies reported an increased operative time with SILS, but failed to take into account the learning curve and need for experience[52,55]. The operative time decreases with accumulating experience, with a learning curve defined between 30 to 36 cases[56].
SILS has distinct benefits over traditional laparoscopic surgery. Using a single port with multiple incorporated working channels, SILS has reduced the number of incisions and tissue trauma required for surgery, improved cosmesis, and lowered the rate of port-site related complications and incisional hernias[39-41,57] (Figure 2). Reduced perioperative pain is another reported advantage of SILS over traditional multiport laparoscopy, with the reduction in pain translating to lower pain scores and opioid use from the immediate post-operative period up to post-operative day 2[39,41]. SILS has also shown a significantly shorter length of stay (LOS); studies have demonstrated LOS more than 1 d shorter for SILS compared to multiport laparoscopy[28,39]. A recent meta-analysis reviewing 14 studies comparing SILS to traditional multiport laparoscopy concluded SILS had lower blood loss, decreased blood transfusion requirement, shorter time to flatus, shorter hospital stay, and smaller incision[51].
The use of SILS introduced several new technical challenges, which may limit widespread use of the platform[58]. The ergonomic and technical requirements of SILS are distinct from those used in conventional multiport laparoscopy, initially adding difficulty even for experienced laparoscopic surgeons[59,60]. The technical challenges are further amplified in colorectal procedures, where there is the need to work in more than one quadrant[58,61]. First, there is the challenge from the in-line orientation of the working trocars through the single access port causes the visual axis to become more in-line, with camera movement resulting in inadvertent movement of the adjacent instrument[17,62]. Working through a small single incision with multiple parallel, instruments competing for the same space at the fulcrum of the entry port decreases the range of motion and external working space, increasing instrument collisions[28,58,63]. These collisions are experienced both intra-corporeally, creating difficulty maintaining pneumoperitoneum, and extra-corporeally, complicating the role of the assistant holding the camera[28]. This forces the surgeon to operate with crossed hands to acclimate[17,62]. The proximity of the trocars at a fixed position, restricted freedom, and clashing of the instruments is contradictory to the traditional teaching of triangulation in laparoscopy[64]. These problems in exposure and “crowding” add to the difficulty in the SILS technique and can result in restricted visualization, inadequate dissection and mobilization, and the potential for inadvertent injury[55,65].
With increasing operator experience, these ergonomic and technical challenges can be readily overcome. Technical instruments and procedural adaptations have been developed to help work through these challenges. To improve surgeon efficiency and decrease collisions, it has also been recommended to keep the laparoscope away from the surgeon’s hands, such as with a flexible-tipped or bariatric-length laparoscope[24,28,66,67]. Articulating or curved instruments can be used to help recreate triangulation familiar with multiport laparoscopy[58]. For assistance in pelvic and multi-quadrant cases, a SILS +1 technique has been developed and validated[65]. With SILS +1, the single access device is introduced through a Pfannenstiel incision and an additional 5-mm port is placed through the umbilicus for the laparoscopic camera, allowing access to more than one abdominal quadrant and minimizing “sword fighting” between the surgeon and the camera holder[65]. To become proficient at SILS, one idea is to become proficient at reduced port laparoscopy - using 3 ports; then the transition to SILS will be more natural.
Despite evidence supporting the use and proven benefits, SILS has not been widely adopted. The main reason cited is the ergonomic demands and additional time, costs, and skills required, especially in early cases[55,59,64,68]. Surgeon experience can overcome the technical and ergonomic challenges, and specialized instruments and platforms have been developed to help ascend the learning curve[17,62].
The technology was also advocated for surgeons experienced with laparoscopy and minimally invasive techniques, and results described in the published literature are achieved by skilled laparoscopic surgeons beyond the learning curve performing the procedures[32,34,69,70]. In addition, published experience has centered on non-obese patients[23,66,70-74]. To increase utilization of this minimally invasive technique, its feasibility in different patient populations must be explored[72]. The learning curve to achieve competence with this technology has been defined, and there are no increased complications or negative outcomes reported during the early phases of the learning curve[56,72]. Therefore, increasing use of SILS for patient benefits and increased overall use of minimally invasive colorectal surgery is encouraged.
As the field of colorectal surgery has emphasized moving towards less invasive techniques, single incision laparoscopic surgery, a hybrid between traditional multiport laparoscopy and NOTES, is the natural evolution in minimally invasive surgery. SILS offers distinct benefits over traditional multiport laparoscopy, but widespread use has been limited from technical, ergonomic, and patient selection challenges. With experience demonstrating the safety and feasibility, and the learning curve for competence defined, increased use of SILS in colorectal surgery is encouraged.
| 1. | Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2606] [Cited by in RCA: 2541] [Article Influence: 115.5] [Reference Citation Analysis (0)] |
| 2. | Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1901] [Cited by in RCA: 1829] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 3. | Delaney CP, Kiran RP, Senagore AJ, Brady K, Fazio VW. Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg. 2003;238:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Schwenk W, Haase O, Neudecker J, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;CD003145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 438] [Article Influence: 20.9] [Reference Citation Analysis (1)] |
| 5. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2325] [Article Influence: 110.7] [Reference Citation Analysis (0)] |
| 6. | Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Hellinger M, Flanagan R, Peters W, Nelson H. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655-662; discussion 662-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 809] [Article Influence: 42.6] [Reference Citation Analysis (3)] |
| 7. | Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg. 2007;142:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 390] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 8. | Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061-3068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1121] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 9. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1710] [Article Influence: 81.4] [Reference Citation Analysis (0)] |
| 10. | Delaney CP, Chang E, Senagore AJ, Broder M. Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg. 2008;247:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 201] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 11. | Delaney CP, Marcello PW, Sonoda T, Wise P, Bauer J, Techner L. Gastrointestinal recovery after laparoscopic colectomy: results of a prospective, observational, multicenter study. Surg Endosc. 2010;24:653-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 830] [Cited by in RCA: 748] [Article Influence: 46.8] [Reference Citation Analysis (2)] |
| 13. | Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 505] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 14. | van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1030] [Cited by in RCA: 1249] [Article Influence: 96.1] [Reference Citation Analysis (1)] |
| 15. | Carmichael JC, Masoomi H, Mills S, Stamos MJ, Nguyen NT. Utilization of laparoscopy in colorectal surgery for cancer at academic medical centers: does site of surgery affect rate of laparoscopy? Am Surg. 2011;77:1300-1304. [PubMed] |
| 16. | Kwon S, Billingham R, Farrokhi E, Florence M, Herzig D, Horvath K, Rogers T, Steele S, Symons R, Thirlby R. Adoption of laparoscopy for elective colorectal resection: a report from the Surgical Care and Outcomes Assessment Program. J Am Coll Surg. 2012;214:909-18.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Cianchi F, Staderini F, Badii B. Single-incision laparoscopic colorectal surgery for cancer: state of art. World J Gastroenterol. 2014;20:6073-6080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Curcillo PG, Podolsky ER, King SA. The road to reduced port surgery: from single big incisions to single small incisions, and beyond. World J Surg. 2011;35:1526-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10:823-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 409] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 20. | Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis. 2008;23:1013-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 348] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 21. | Boni L, Dionigi G, Cassinotti E, Di Giuseppe M, Diurni M, Rausei S, Cantore F, Dionigi R. Single incision laparoscopic right colectomy. Surg Endosc. 2010;24:3233-3236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 92] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 22. | Adair J, Gromski MA, Lim RB, Nagle D. Single-incision laparoscopic right colectomy: experience with 17 consecutive cases and comparison with multiport laparoscopic right colectomy. Dis Colon Rectum. 2010;53:1549-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | Geisler DP, Condon ET, Remzi FH. Single incision laparoscopic total proctocolectomy with ileopouch anal anastomosis. Colorectal Dis. 2010;12:941-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 91] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 24. | Law WL, Fan JK, Poon JT. Single-incision laparoscopic colectomy: early experience. Dis Colon Rectum. 2010;53:284-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Merchant AM, Lin E. Single-incision laparoscopic right hemicolectomy for a colon mass. Dis Colon Rectum. 2009;52:1021-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 93] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 26. | Choi SI, Lee KY, Park SJ, Lee SH. Single port laparoscopic right hemicolectomy with D3 dissection for advanced colon cancer. World J Gastroenterol. 2010;16:275-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 81] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 27. | Ramos-Valadez DI, Patel CB, Ragupathi M, Bartley Pickron T, Haas EM. Single-incision laparoscopic right hemicolectomy: safety and feasibility in a series of consecutive cases. Surg Endosc. 2010;24:2613-2616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 28. | Papaconstantinou HT, Sharp N, Thomas JS. Single-incision laparoscopic right colectomy: a case-matched comparison with standard laparoscopic and hand-assisted laparoscopic techniques. J Am Coll Surg. 2011;213:72-80; discussion 80-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 29. | Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 127] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 30. | Chen WT, Chang SC, Chiang HC, Lo WY, Jeng LB, Wu C, Ke TW. Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc. 2011;25:1887-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 113] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 31. | Rijcken E, Mennigen R, Argyris I, Senninger N, Bruewer M. Single-incision laparoscopic surgery for ileocolic resection in Crohn’s disease. Dis Colon Rectum. 2012;55:140-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC, Delaney CP. Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg. 2012;255:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 33. | Huscher CG, Mingoli A, Sgarzini G, Mereu A, Binda B, Brachini G, Trombetta S. Standard laparoscopic versus single-incision laparoscopic colectomy for cancer: early results of a randomized prospective study. Am J Surg. 2012;204:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 34. | Makino T, Milsom JW, Lee SW. Feasibility and safety of single-incision laparoscopic colectomy: a systematic review. Ann Surg. 2012;255:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 35. | Moftah M, Nazour F, Cunningham M, Cahill RA. Single port laparoscopic surgery for patients with complex and recurrent Crohn’s disease. J Crohns Colitis. 2014;8:1055-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Keller DS, Ragupathi M, Haas EM. Single Incision Laparoscopic Colon and Rectal Surgery. Clin Colon Rectal Surg. 2015;In press. |
| 37. | Atallah SB, Debeche-Adams T. Incisionless laparoscopic stoma construction using a 12-mm Hassan trocar. Am Surg. 2012;78:E495-E497. [PubMed] |
| 38. | Lopez NE, Peterson CY, Ramamoorthy SL, McLemore EC, Sedrak MF, Lowy AM, Horgan S, Talamini MA, Sicklick JK. Single-incision laparoscopic surgery through an ostomy site: a natural approach by an unnatural orifice. Surg Laparosc Endosc Percutan Tech. 2015;25:74-78. [PubMed] |
| 39. | Vasilakis V, Clark CE, Liasis L, Papaconstantinou HT. Noncosmetic benefits of single-incision laparoscopic sigmoid colectomy for diverticular disease: a case-matched comparison with multiport laparoscopic technique. J Surg Res. 2013;180:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Chambers WM, Bicsak M, Lamparelli M, Dixon AR. Single-incision laparoscopic surgery (SILS) in complex colorectal surgery: a technique offering potential and not just cosmesis. Colorectal Dis. 2011;13:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 116] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 41. | Poon JT, Cheung CW, Fan JK, Lo OS, Law WL. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc. 2012;26:2729-2734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 158] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 42. | Horiuchi T, Tanishima H, Tamagawa K, Matsuura I, Nakai H, Shouno Y, Tsubakihara H, Inoue M, Tabuse K. Randomized, controlled investigation of the anti-infective properties of the Alexis retractor/protector of incision sites. J Trauma. 2007;62:212-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 43. | Reid K, Pockney P, Draganic B, Smith SR. Barrier wound protection decreases surgical site infection in open elective colorectal surgery: a randomized clinical trial. Dis Colon Rectum. 2010;53:1374-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 44. | Day W, Lau P. Novel “glove” access port for single port surgery in right hemicolectomy: a pilot study. Surg Laparosc Endosc Percutan Tech. 2011;21:e145-e147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Livraghi L, Berselli M, Bianchi V, Latham L, Farassino L, Cocozza E. Glove technique in single-port access laparoscopic surgery: results of an initial experience. Minim Invasive Surg. 2012;2012:415430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 46. | Rodicio Miravalles JL, Rodríguez García JI, Llaneza Folgueras A, Avilés García P, González González JJ. [Single port laparoscopic colostomy using the glove technique]. Medicina (B Aires). 2014;74:201-204. [PubMed] |
| 47. | Sirikurnpiboon S. Single-access laparoscopic rectal cancer surgery using the glove technique. Asian J Endosc Surg. 2014;7:206-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6-16. [PubMed] |
| 49. | Saber AA, El-Ghazaly TH. Single-incision transumbilical laparoscopic right hemicolectomy using SILS Port. Am Surg. 2011;77:252-253. [PubMed] |
| 50. | Trakarnsanga A, Akaraviputh T, Wathanaoran P, Phalanusitthepha C, Methasate A, Chinswangwattanakul V. Single-incision laparoscopic colectomy without using special articulating instruments: an initial experience. World J Surg Oncol. 2011;9:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Zhou YM, Wu LP, Zhao YF, Xu DH, Li B. Single-incision versus conventional laparoscopy for colorectal disease: a meta-analysis. Dig Dis Sci. 2012;57:2103-2112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 52. | Daher R, Chouillard E, Panis Y. New trends in colorectal surgery: single port and natural orifice techniques. World J Gastroenterol. 2014;20:18104-18120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | Chew MH, Chang MH, Tan WS, Wong MT, Tang CL. Conventional laparoscopic versus single-incision laparoscopic right hemicolectomy: a case cohort comparison of short-term outcomes in 144 consecutive cases. Surg Endosc. 2013;27:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Fujii S, Watanabe K, Ota M, Watanabe J, Ichikawa Y, Yamagishi S, Tatsumi K, Suwa H, Kunisaki C, Taguri M. Single-incision laparoscopic surgery using colon-lifting technique for colorectal cancer: a matched case-control comparison with standard multiport laparoscopic surgery in terms of short-term results and access instrument cost. Surg Endosc. 2012;26:1403-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 55. | Gaujoux S, Bretagnol F, Ferron M, Panis Y. Single-incision laparoscopic colonic surgery. Colorectal Dis. 2011;13:1066-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 56. | Haas EM, Nieto J, Ragupathi M, Aminian A, Patel CB. Critical appraisal of learning curve for single incision laparoscopic right colectomy. Surg Endosc. 2013;27:4499-4503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 57. | Bulut O, Nielsen CB, Jespersen N. Single-port access laparoscopic surgery for rectal cancer: initial experience with 10 cases. Dis Colon Rectum. 2011;54:803-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 58. | Fung AK, Aly EH. Systematic review of single-incision laparoscopic colonic surgery. Br J Surg. 2012;99:1353-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 59. | Pucher PH, Sodergren MH, Singh P, Darzi A, Parakseva P. Have we learned from lessons of the past? A systematic review of training for single incision laparoscopic surgery. Surg Endosc. 2013;27:1478-1484. [PubMed] |
| 60. | Islam A, Castellvi AO, Tesfay ST, Castellvi AD, Wright AS, Scott DJ. Early surgeon impressions and technical difficulty associated with laparoendoscopic single-site surgery: a Society of American Gastrointestinal and Endoscopic Surgeons Learning Center study. Surg Endosc. 2011;25:2597-2603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 61. | Chew MH, Wong MT, Lim BY, Ng KH, Eu KW. Evaluation of current devices in single-incision laparoscopic colorectal surgery: a preliminary experience in 32 consecutive cases. World J Surg. 2011;35:873-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 62. | Dhumane PW, Diana M, Leroy J, Marescaux J. Minimally invasive single-site surgery for the digestive system: A technological review. J Minim Access Surg. 2011;7:40-51. [PubMed] |
| 63. | Gandhi DP, Ragupathi M, Patel CB, Ramos-Valadez DI, Pickron TB, Haas EM. Single-incision versus hand-assisted laparoscopic colectomy: a case-matched series. J Gastrointest Surg. 2010;14:1875-1880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 64. | Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). J Gastrointest Surg. 2009;13:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 156] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 65. | Ragupathi M, Ramos-Valadez DI, Yaakovian MD, Haas EM. Single-incision laparoscopic colectomy: a novel approach through a Pfannenstiel incision. Tech Coloproctol. 2011;15:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 66. | Rieger NA, Lam FF. Single-incision laparoscopically assisted colectomy using standard laparoscopic instrumentation. Surg Endosc. 2010;24:888-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 67. | Waters JA, Chihara R, Moreno J, Robb BW, Wiebke EA, George VV. Laparoscopic colectomy: does the learning curve extend beyond colorectal surgery fellowship? JSLS. 2010;14:325-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 68. | Champagne BJ, Lee EC, Leblanc F, Stein SL, Delaney CP. Single-incision vs straight laparoscopic segmental colectomy: a case-controlled study. Dis Colon Rectum. 2011;54:183-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 69. | Bemelman WA, van Hogezand RA, Meijerink WJ, Griffioen G, Ringers J. Laparoscopic-assisted bowel resections in inflammatory bowel disease: state of the art. Neth J Med. 1998;53:S39-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 70. | Geisler D, Garrett T. Single incision laparoscopic colorectal surgery: a single surgeon experience of 102 consecutive cases. Tech Coloproctol. 2011;15:397-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 71. | Bucher P, Pugin F, Morel P. Transumbilical single incision laparoscopic sigmoidectomy for benign disease. Colorectal Dis. 2010;12:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 72. | Miller S, Causey MW, Damle A, Maykel J, Steele S. Single-incision laparoscopic colectomy: training the next generation. Surg Endosc. 2013;27:1784-1790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 73. | Remzi FH, Kirat HT, Geisler DP. Laparoscopic single-port colectomy for sigmoid cancer. Tech Coloproctol. 2010;14:253-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 74. | Ross H, Steele S, Whiteford M, Lee S, Albert M, Mutch M, Rivadeneira D, Marcello P. Early multi-institution experience with single-incision laparoscopic colectomy. Dis Colon Rectum. 2011;54:187-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Bandyopadhyay SK, Karabicak I, McArdle A S- Editor: Yu J L- Editor: A E- Editor: Ma S