Published online Jul 14, 2015. doi: 10.3748/wjg.v21.i26.8148
Peer-review started: December 3, 2014
First decision: January 8, 2015
Revised: February 6, 2015
Accepted: April 9, 2015
Article in press: April 9, 2015
Published online: July 14, 2015
Processing time: 224 Days and 10.8 Hours
AIM: To examine the correlation between the severity of venous calcifications and the clinical symptoms of phlebosclerotic colitis.
METHODS: This was a retrospective study. The data, including the numbers of episodes of active disease, were collected from the medical records at Taipei Veterans General Hospital and Wei Gong Memorial Hospital in Taiwan between January 2005 and December 2014. All computed tomography images with or without contrast enhancement were obtained using a multiple detector computed tomography scanner. The scanning range reached from the dome of the diaphragm to the pelvis. The severity of calcification at the tributaries of the portal vein was measured using a four-grade scoring system of the calcification of phlebosclerotic colitis. The episodes of active disease were defined as symptoms of fever, abdominal pain, severe constipation, bowel obstruction, vomiting or diarrhea based on a review of the medical records. Spearman’s correlation analysis was used to examine the correlation between the numbers of episodes of active disease and the severity of the calcification of the mesenteric veins.
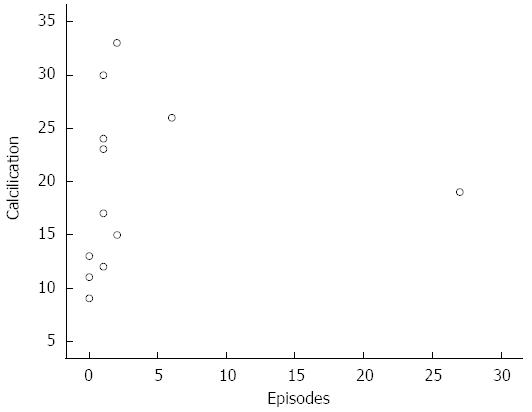
RESULTS: More than 3000 cases were reviewed from 2005 to 2014, and a total of 12 patients from Taipei Veterans General Hospital and Wei Gong Memorial Hospital were enrolled according to our inclusion criteria. Among these 12 patients, the mean age of the six males and the six females was 61.8 ± 11.5 years. All patients exhibited typical imaging characteristics, consisting of threadlike calcifications and colonic wall thickening in the standard radiographs and calcifications along the colonic and mesenteric vessels or associated with colonic wall thickening and adjacent fat stranding in the computed tomography images. The median score of the severity of the venous calcifications was 18 ± 13, and the median number of active disease episodes was 1 ± 1.75. Spearman’s correlation analysis revealed that the number of episodes of active phlebosclerotic colitis disease significantly positively correlated with the severity of the calcification of the mesenteric veins (r = 0.619, P < 0.05).
CONCLUSION: The extent of mesenteric venous calcification is strongly associated with the number of episodes of active disease among patients with phlebosclerotic colitis.
Core tip: Phlebosclerotic colitis, which is almost exclusively observed in the Asian population, is a rare condition of ischemic colitis associated with the sclerosis and calcification of the mesenteric venous wall, resulting in the preferential involvement of the right hemicolon and complications during a relatively chronic clinical course. We reviewed the medical records and examined the correlation between the severity of venous calcifications and the clinical symptoms of phlebosclerotic colitis observed on computed tomography images. According to our findings, the extent of mesenteric venous calcifications strongly positively correlates with the number of episodes of active disease.
- Citation: Yen TS, Liu CA, Chiu NC, Chiou YY, Chou YH, Chang CY. Relationship between severity of venous calcifications and symptoms of phlebosclerotic colitis. World J Gastroenterol 2015; 21(26): 8148-8155
- URL: https://www.wjgnet.com/1007-9327/full/v21/i26/8148.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i26.8148
Ischemic bowel disease is a heterogeneous group of disorders that display a common characteristic of bowel hypoxia caused by alterations in blood flow and is typically evoked by arterial thromboembolic disease[1]. However, disturbed venous return may also result in colitis[2]. Phlebosclerotic colitis, which is almost exclusively observed in the Asian population[3-7], is a rare condition of ischemic colitis associated with the sclerosis and calcification of the mesenteric venous wall. Phlebosclerotic colitis preferentially involves the right hemicolon[8], and its clinical course is relatively chronic[9,10]. The common clinical symptoms caused by phlebosclerotic colitis are nonspecific and include abdominal pain, diarrhea or bloody stool[8]. The severity of venous calcification, which is an imaging finding that is specific to phlebosclerotic colitis[11], based on radiography increases gradually and progresses in the caudal direction[12,13]. Pathological examination may reveal various degrees of occlusion of the affected venous lumen[14]. We therefore hypothesized that the severity of venous calcification positively correlates with clinical symptoms. Thus, the objective of this study was to examine the correlation between the severity of venous calcifications and the number of active episodes involving the clinical symptoms of phlebosclerotic colitis.
This is a retrospective study, and the data were collected from the medical records at Taipei Veterans General Hospital and Wei Gong Memorial Hospital between January 2005 and December 2014. Written informed consent was waived.
We retrospectively reviewed the medical records for patients who fulfilled the following inclusion criteria: (1) at least one complete abdominal computed tomography (CT) examination with or without intravenous contrast medium injection; and (2) calcification at tributaries of the superior mesenteric veins.
All CT images with or without contrast enhancement were obtained using a multiple detector CT scanner. The scanning range reached from the dome of the diaphragm to the pelvis. For dual-phase contrast enhanced CT images, nonionic contrast material was administered intravascularly using an automated injector at a rate of 1.5-2 mL/s during a single breath-hold. The axial and coronal images were reconstructed in 5-mm-thick intervals.
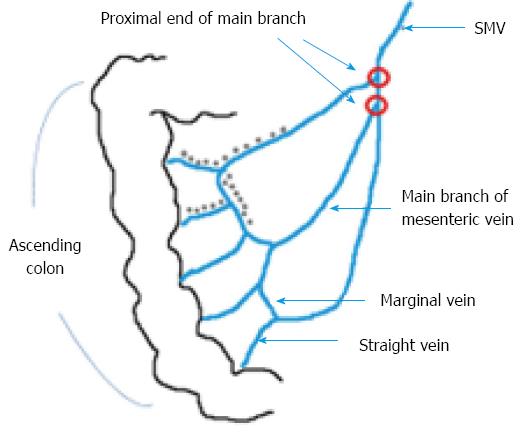
The CT imaging findings were assessed by two radiologists (with 4 and 10 years of clinical experience, respectively). The threshold value for calcification was set at 130 Hounsfield units (HU) according to the typically used value of 130 HU for the Agatston score[15]. For patients who underwent multiple CT scans, the most recent CT scan was evaluated. The severity of calcification at the tributaries of the portal vein was measured using a 4-grade scoring system of the calcification of phlebosclerotic colitis[16] (Table 1; a schematic of the calcification score calculation is depicted in Figure 1).
| Calcifications limited in straight vein of the colon (× 1) |
| Calcifications extended to the paracolic marginal vein (× 2) |
| Calcifications extended to the main branch of mesenteric vein (× 3) |
| The proximal end of the main branch is involved (× 4) |
The episodes of active disease were defined as symptoms of fever, abdominal pain, severe constipation, bowel obstruction, vomiting, and diarrhea based on a review of the medical records.
All data were analyzed using SPSS (Statistical Package for the Social Sciences) version 22.0 software (IBM, Armonk, NY). Descriptive statistics of the distributions of the demographic and clinical characteristics of the patients exhibiting calcification at the tributaries of the portal vein from the continuous data are presented as median values and interquartile ranges, and the statistics from the categorical data are presented as the numbers and frequencies of observations. Spearman’s correlation analysis was used to examine the correlation between the number of active disease episodes and the severity of mesenteric vein calcification. A two-tailed P-value less than 0.05 was considered to indicate a significant correlation between the variables.
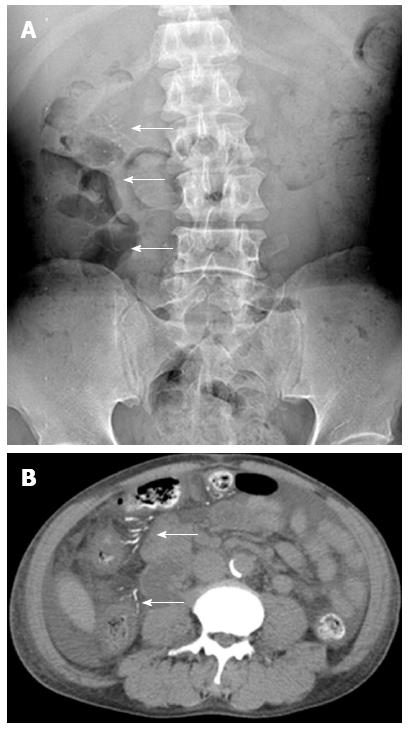
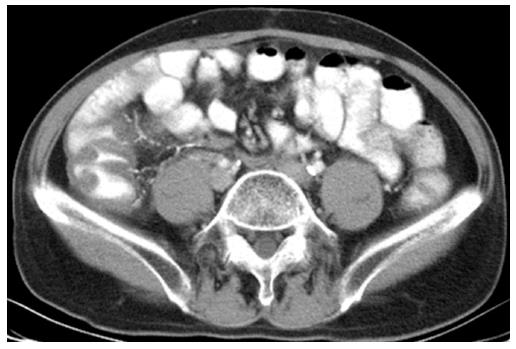
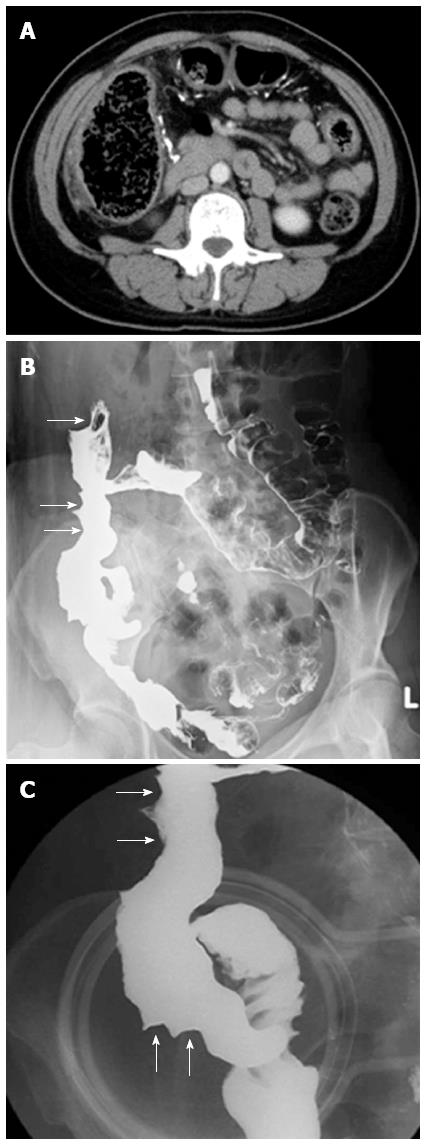
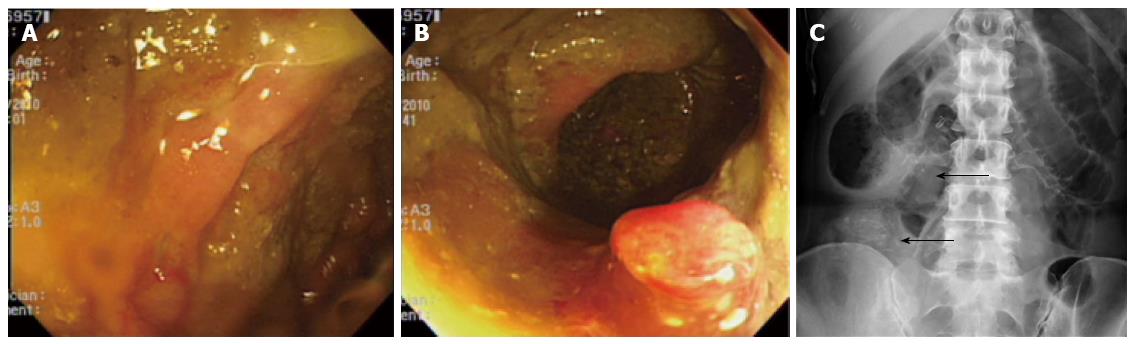
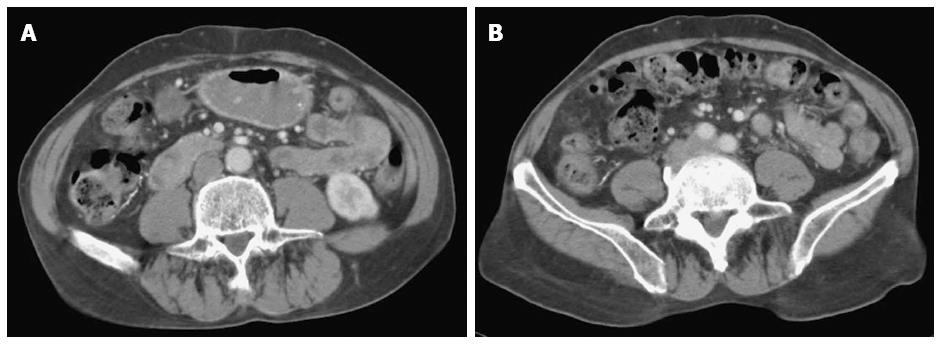
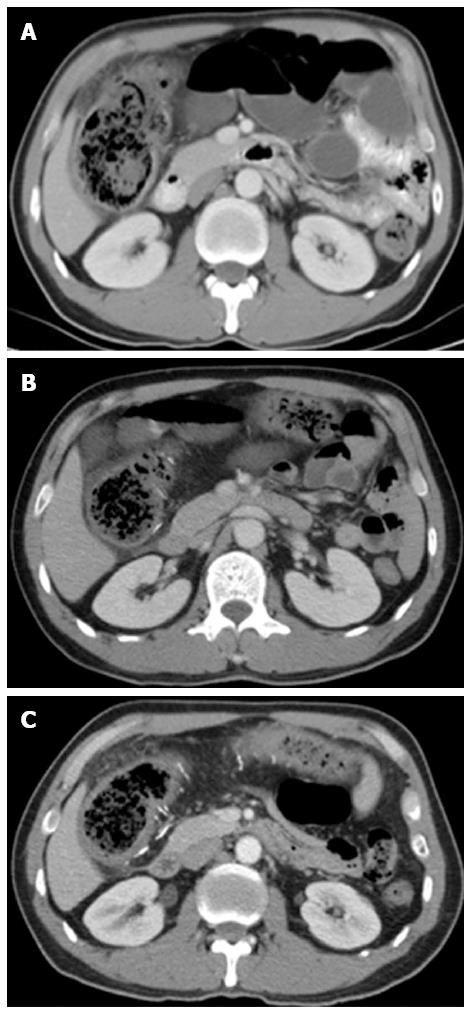
More than 3000 cases were reviewed, and a total of 12 patients were enrolled according to the inclusion criteria. Among these 12 patients, the 6 males and the 6 females had a mean age of 61.8 years, ranging from 49 to 85 years. No patients underwent surgical intervention. Seventy-five percent of the patients exhibited symptoms of phlebosclerotic colitis, and the number of episodes of active disease ranged from 0 to 27 [1 ± 1.75, median ± interquartile range (IQR)] (Table 2). All patients exhibited linear calcification on CT, and the scores for the severity of venous calcification ranged from 9 to 33 (18 ± 13, median ± IQR). Table 3 shows the imaging findings for these patients. Based on the imaging findings, 10 patients displayed threadlike calcifications (Figure 2) on conventional radiographs, eight patients exhibited colonic wall thickening in CT studies (Figure 3), and one patient displayed a typical characteristic, which was thumb-printing appearance, based on barium follow-through study (Figure 4). One patient received a colonoscopic examination, and the findings revealed a typical ischemic change in the ascending colon (Figure 5). Three patients exhibited no apparent symptoms; however, the CT imaging findings of these three asymptomatic patients were bowel wall thickening and fat stranding at the paracolic gutters of the involved colon (Figure 6), which were typical imaging characteristics of this rare disease.
| Characteristics | Case (n = 12) |
| Age (yr), mean ± SD | 61.8 ± 11.5 |
| Sex | |
| Male | 6 (50.0) |
| Female | 6 (50.0) |
| Underlying disease | |
| No | 2 (16.7) |
| HCC | 2 (16.7) |
| Bladder cancer | 1 (8.3) |
| Ampulla Vater cancer | 1 (8.3) |
| ESRD | 6 (50.0) |
| Known episode of active disease | |
| None | 3 (25.0) |
| One | 5 (41.7) |
| Two | 2 (16.7) |
| More than two | 2 (16.7) |
| The score of the severity of venous calcifications (median ± interquartile) | 18.0 ± 13.0 |
| Imaging features | Case (n = 12) |
| Plain-film radiographs of the abdomen (kidney ureter bladder) | |
| Threadlike calcification, | 10 (83.3) |
| Was not performed | 2 (16.7) |
| Abdominal computed tomography | |
| Finding of thickening of colonic wall | |
| Negative | 4 (33.3) |
| Positive | 8 (66.7) |
| Finding of threadlike calcification | |
| Negative | 0 (0.0) |
| Positive | 12 (100.0) |
The dispersion diagram (Figure 7) displays the relationship between the number of active disease episodes and the severity of mesenteric venous calcification. Spearman correlation analysis showed that the number of episodes of active disease significantly correlated with the severity of mesenteric venous calcification (r = 0.619, P < 0.05).
Ischemic colitis is caused by a disturbance in the blood supply and is evoked by arterial thromboembolic disease; however, phlebosclerotic colitis affects regions of the colon displaying aberrant venous drainage into the superior mesenteric vein. The first description of phlebosclerotic colitis was in a Japanese study in 1991[5]. The clinical course of phlebosclerotic colitis is chronic, and its clinical symptoms, such as fever, abdominal pain, severe constipation, bowel obstruction, vomiting, and diarrhea, are attributable to the ischemic change in the colon secondary to the sclerosis of the draining veins. Several additional severe symptoms, such as bowel obstruction, bowel perforation, bloody diarrhea, and abscess formation[17], occur over time. However, the etiology and risk factors for sclerosis in the tributaries of the superior mesenteric vein remain unclear. Six patients with phlebosclerotic colitis in our studies suffered from end-stage renal disease (ESRD), all of whom ingested Chinese herbs for different periods. The incidence of ESRD in Taiwan is the highest in the world, and there is evidence that Chinese herb nephropathy is a significant cause of ESRD in Taiwan[18,19]. Chang[20] indicated that these absorbed substances enter the venous return, potentially damaging veins. Moreover, several studies[20-22] reported that certain substances or toxins from ingested Chinese herbs may contribute to phlebosclerotic colitis. Therefore, we propose that ESRD correlates with phlebosclerotic colitis. The relationship between ESRD and phlebosclerotic colitis requires further investigation. Although Chang[20] reported 5 phlebosclerotic colitis cases with a history of herbal ingestion, the hypothesis that herb ingestion contributes to phlebosclerotic colitis requires further investigation. Regarding the medical history, the laboratory findings, and the family history of the 12 examined patients, no notable etiologies or risk factors were detected.
The clinical diagnosis of phlebosclerotic colitis is typically based on a combination of symptoms and clinical, radiological, and endoscopic findings. The typical findings from a barium enema are the disappearance of the semilunar folds, luminal narrowing and a thumbprint-like appearance[8,11]. On conventional radiographs, threadlike calcification in the right hemicolon is a pathognomonic imaging finding. CT scans are more reliable for detecting mesenteric venous calcification[23] and colonic wall thickening. Several angiographic findings, such as narrowing and irregularity of the marginal arteries with tortuous vasa recta[23] and delayed venous return[14,25] with or without developed collateral veins[25], have been reported.
In the present study, although three patients exhibited no apparent clinical episodes of active disease, their CT imaging findings were typical of this disease (Figure 6). In contrast, patients at the early stage of this disease may exhibit no substantial calcification based on imaging or microscopic examination[26].
One patient in our study experienced the recurrent symptoms of abdominal pain, constipation, nausea and vomiting many times since 2003. The CT examination conducted in 2005 only revealed a dilated ascending colon without calcification at the mesenteric veins. The barium enema performed in 2006 revealed a loss of haustration in the ascending colon, the transverse colon, and the proximal descending colon and a thumbprint-like appearance of the ascending colon. Colitis with unknown etiology was observed. The severity of colonic wall thickening and calcification in the portal vein tributaries increased in serial CT studies performed in 2005, 2009, 2010 and 2012 (Figure 8). However, the diagnosis of phlebosclerotic colitis was initially determined in 2010 according to typical imaging findings and clinical symptoms. The CT examinations of patients with phlebosclerotic colitis may display nonspecific findings, and thus, accurate diagnosis during the early stage of this disease is difficult.
In this study, Spearman’s correlation analysis was used to examine the relationship between the clinical symptoms of phlebosclerotic colitis and the severity of venous calcifications based on the imaging data. The results indicated that more severe mesenteric venous calcification was associated with more numerous clinical symptoms.
The major limitation of this study is the small case number. In addition, because these patients may have experienced mild clinical symptoms[26], they may not have visited the hospital or their condition may have been misdiagnosed as diarrhea or constipation by a clinician. Even if patients visit the hospital and receive an imaging examination, calcification in the colonic wall or along the tributaries of the superior mesenteric vein may not have occurred during the early stage of this disease. Some asymptomatic patients exhibiting typical imaging characteristics may experience symptoms during an extended follow-up duration.
Previously, the majority of phlebosclerotic colitis patients underwent surgery; however, at present, conservative treatment with close follow-up is preferred if there are no signs of bowel compromise[27-29]. Surgery has been suggested for patients with severe complications, such as intestinal obstruction, perforation, peritonitis and sepsis. The patients in our study received only conservative treatment because they lacked any complications that would require surgical treatment.
In conclusion, radiologic findings play a crucial role in diagnosing phlebosclerotic colitis, and a CT study is the most useful diagnostic tool for evaluating the severity of mesenteric venous calcification. The extent of mesenteric venous calcification is strongly positively associated with the number of episodes of active disease.
Phlebosclerotic colitis is a rare disease, and its etiology and risk factors remain uncertain. The presence of calcifications in the mesenteric veins is a typical radiographic characteristic of this disease.
The radiographic and pathological characteristics of this disease were previously described in several reports. However, the correlation between the severity of venous calcification and these clinical symptoms remains unclear.
The author’s finding improves the understanding of phlebosclerotic colitis.
A positive relationship between venous calcifications and the clinical symptoms of phlebosclerotic colitis was observed. The scoring system of venous calcification may help predict the prognosis and guide the treatment of this disease.
Phlebosclerotic colitis is a rare disease causing chronic ischemic colitis and sclerosis of the mesenteric veins.
The authors detail the radiographic characteristics of phlebosclerotic colitis and the relationship between imaging findings and clinical presentation. The results show that the extent of mesenteric venous calcifications is positively associated with the number of episodes of active disease.
| 1. | Balthazar EJ, Yen BC, Gordon RB. Ischemic colitis: CT evaluation of 54 cases. Radiology. 1999;211:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 126] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Grendell JH, Ockner RK. Mesenteric venous thrombosis. Gastroenterology. 1982;82:358-372. [PubMed] |
| 3. | Yoshinaga S, Harada N, Araki Y, Kubo H, Nawata H, Hotokezaka M, Nishi H, Chijiiwa Y, Nagase S. Chronic ischemic colonic lesion caused by phlebosclerosis: a case report. Gastrointest Endosc. 2001;53:107-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Hoashi T, Maeda K, Matsui T, Yao T, Futami K, Arima T, Iwashita A, Nakatake K. Ischemic intestinal lesion caused by phlebosclerosis with marked venous calcification, report of a case. Stomach Intestine. 1993;28:967-973. |
| 5. | Koyama N, Koyama H, Hanajima T. Chronic ischemic colitis causing stenosis. Report of a case. Stomach Intestine. 1991;26:455-460. |
| 6. | Tsuda M, Kubota S, Nakamura T, Sakaguchi K, Uokawa H, Inushima K, Fukui K, Miura M, Koide R, Yu H. Ischemic intestinal lesion caused by phlebosclerosis, report of a case. Stomach Intestine. 1995;30:709-714. |
| 7. | Kitamura T, Kubo M, Nakanishi T, Fushimi H, Yoshikawa K, Taenaka N, Furukawa T, Tsujimura T, Kameyama M. Phlebosclerosis of the colon with positive anti-centromere antibody. Intern Med. 1999;38:416-421. [PubMed] |
| 8. | Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003;46:209-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 9. | Ikehata A, Hiwatashi N, Kawarada H, Yamazaki H, Ito K, Kinouchi Y, Kimura M, Noguchi M, Maekawa H, Suzuki H. Chronic Ischemic Colitis Associated with Marked Calcifications of the Mesenteric Vessels - Report of Two Cases. Digestive Endoscopy. 1994;6:355-364. [RCA] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Arimura Y, Kondoh Y, Kurokawa S, Azuma N, Sekiya M, Nakagawa N, Endo T, Satoh M, Imai K. Chronic ischemic colonic lesion caused by phlebosclerosis with calcification. Am J Gastroenterol. 1998;93:2290-2292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Yao T, Iwashita A, Hoashi T, Matsui T, Sakurai T, Arima S, Ono H, Schlemper RJ. Phlebosclerotic colitis: value of radiography in diagnosis--report of three cases. Radiology. 2000;214:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Hagiwara H, Nagashima T, Andoh K, Moriya N, Nakamura N. End-stage phlebosclerotic colitis: a rare cause of intramural calcification of the colon. Eur J Radiol Extra. 2004;52:73-77. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Kwok K, Lo S, Fung H, Fan T, Wong W. Mesenteric phlebosclerosis-features on plain radiograph and computed tomography scan. J HK Coll Radiol. 2010;12:136-138. |
| 14. | Fang YL, Hsu HC, Chou YH, Wu CC, Chou YY. Phlebosclerotic colitis: A case report and review of the literature. Exp Ther Med. 2014;7:583-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827-832. [PubMed] |
| 16. | Liao CH, Shen WC, Lin WC, Ho YJ, Chen JH, Chiu YF, Chung SW. CT Imaging features of Phlebosclerotic Colotis: Correlation of Calcification of the Mesenteric Vein with the Modalities of Treatment in 10 Cases. AOCR. 2010;. |
| 17. | Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi F. Perforated phlebosclerotic colitis--description of a case and review of this condition. Colorectal Dis. 2010;12:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Yang WC, Hwang SJ. Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transplant. 2008;23:3977-3982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 172] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Chang KM. New histologic findings in idiopathic mesenteric phlebosclerosis: clues to its pathogenesis and etiology--probably ingested toxic agent-related. J Chin Med Assoc. 2007;70:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Miyazaki M, Nakamura S, Matsumoto T. Idiopathic mesenteric phlebosclerosis occurring in a wife and her husband. Clin Gastroenterol Hepatol. 2009;7:e32-e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Nishiura H, Nakase H, Chiba T. Sustained abdominal discomfort in a 57-year-old woman. Idiopathic mesenteric phlebosclerosis. Gut. 2010;59:578, 594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Ayuso C, Luburich P, Vilana R, Bru C, Bruix J. Calcifications in the portal venous system: comparison of plain films, sonography, and CT. AJR Am J Roentgenol. 1992;159:321-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Markos V, Kelly S, Yee WC, Davis JE, Cheifetz RE, Alsheikh A. Phlebosclerotic colitis: imaging findings of a rare entity. AJR Am J Roentgenol. 2005;184:1584-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Ying KS, Huang JC, Chan LP, Wu SH, Chang TY, CH . L. Chronic phlebosclerotic ischemic colitis. Zhonghua Fangshexue Zazhi. 2002;27:129-134. |
| 26. | Kusanagi M, Matsui O, Kawashima H, Gabata T, Ida M, Abo H, Isse K. Phlebosclerotic colitis: imaging-pathologic correlation. AJR Am J Roentgenol. 2005;185:441-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Yu CJ, Wang HH, Chou JW, Lai HC, Huang WH, Peng CY, Cheng KS, Chen YF. Phlebosclerotic colitis with nonsurgical treatment. Int J Colorectal Dis. 2009;24:1241-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Hoshino Y, Matsumoto R, Takasaki T, Nagahara H, Shiratori K. Education and imaging. Gastrointestinal: Phlebosclerotic colitis. J Gastroenterol Hepatol. 2008;23:670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Ho T, Cheung C, Wong W, Chan F. Phlebosclerotic colitis: an unusual cause of ischaemic colitis in a 65-year-old man. J HK Coll Radiol. 2005;8:53. |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Sakaguchi T, Sulkowski S, Walldorf J S- Editor: Yu J L- Editor: Wang TQ E- Editor: Ma S