Published online Jun 28, 2015. doi: 10.3748/wjg.v21.i24.7608
Peer-review started: December 8, 2014
First decision: January 8, 2015
Revised: February 13, 2015
Accepted: March 18, 2015
Article in press: March 19, 2015
Published online: June 28, 2015
Processing time: 203 Days and 19.5 Hours
Duodenal adenocarcinoma, especially duodenal bulb with neuroendocrine features (NEF), is extremely rare. Here, we report one such case of duodenal bulb adenocarcinoma with neuroendocrine features. A 63-year-old Han Chinese woman was admitted to our department with the diagnosis of a duodenal bulb polyp and underwent an endoscopic mucosal resection. The pathological findings confirmed it as duodenal bulb adenocarcinoma with NEF. The patient remains curative after one and half a years of follow-up. Duodenal adenocarcinoma with NEF might be a low malignant neuroendocrine tumor rather than a conventional adenocarcinoma. Endoscopic treatment, including endoscopic mucosal resection, might be an ideal option for the adenocarcinomas with NEF.
Core tip: We report one extremely rare case of duodenal bulb adenocarcinoma with neuroendocrine features (NEF). Duodenal adenocarcinoma with NEF might be a low malignant neuroendocrine tumor rather than a conventional adenocarcinoma. Endoscopic treatment, including endoscopic mucosal resection, is plausibly an ideal option for adenocarcinomas with NEF.
- Citation: Wen MY, Wang Y, Meng XY, Xie HP. Endoscopic mucosal resection of duodenal bulb adenocarcinoma with neuroendocrine features: An extremely rare case report. World J Gastroenterol 2015; 21(24): 7608-7612
- URL: https://www.wjgnet.com/1007-9327/full/v21/i24/7608.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i24.7608
Primary malignant tumors of the duodenum represent 0.3% of all gastrointestinal tract tumors.
Duodenal adenocarcinoma accounts for half of all small bowel adenocarcinomas[1-3]. Histologically, 40% of small bowel cancer are adenocarcinoma and another 40% are neuroendocrine tumors. Recently, a rare case of duodenal adenocarcinoma with neuroendocrine features (NEF) was reported that was neither a conventional neuroendocrine tumor nor a typical duodenal adenocarcinoma[4]. It remains unclear whether duodenal adenocarcinoma with NEF should be treated as adenocarcinoma or neuroendocrine tumors or both. Here we report one extremely rare case of duodenal bulb adenocarcinoma with NEF which was successfully removed by endoscopic mucosal resection (EMR) and enjoyed a good survival without recurrence or metastasis during one and half a years of follow-up.
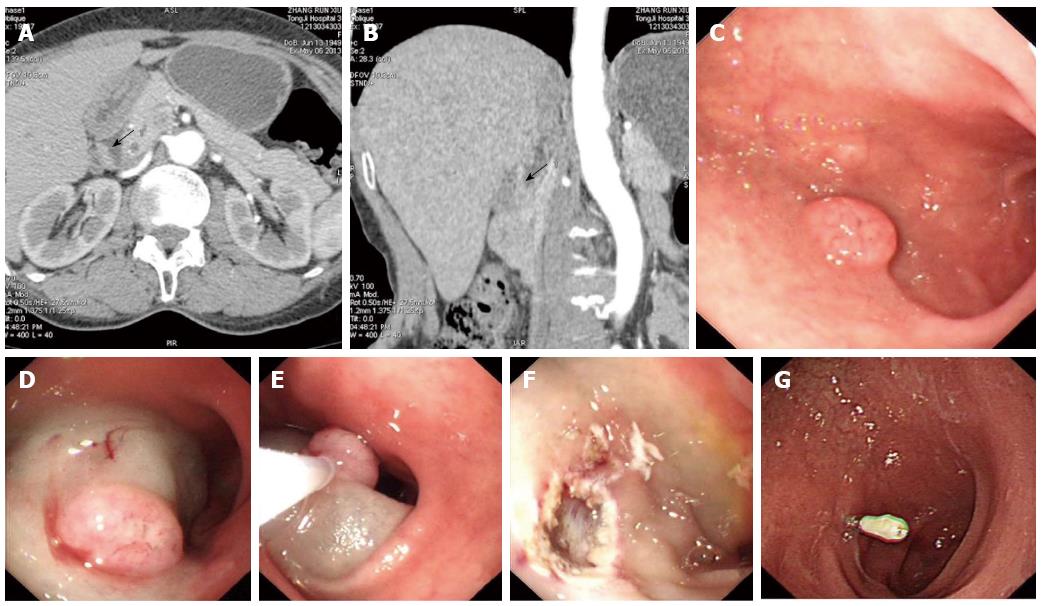
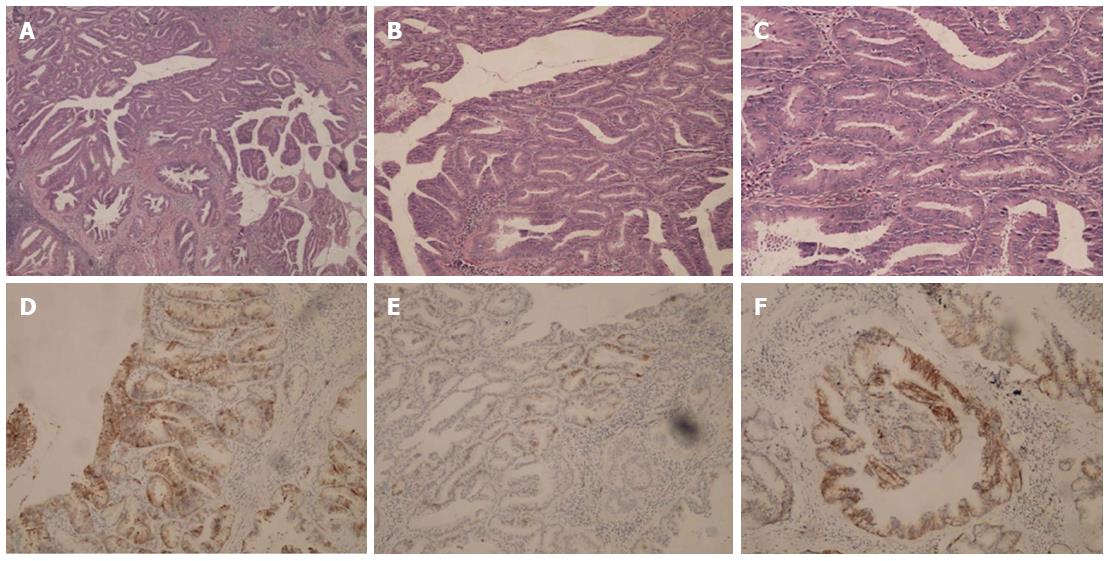
A 63-year-old Han Chinese woman was admitted to our department with anorexia and epigastric fullness for over two years. She complained of aggravation after eating and remission after belching. There were no significant prior diseases in the medical history. Esophagogastroduodenoscopy from the local hospital revealed a protrusion in the duodenum the size of 0.6 cm × 0.6 cm and she was admitted with an intention of “polypectomy”. There were no remarkable findings from the physician examinations. Biochemical examinations were all in normal range, except that the serum chromogranin (CgA) level was 151 ng/mL (reference: 27-94 ng/mL). The multi-row computed tomography (CT) of the small intestine detected a protrusion of duodenum without lymph node involvement. The protrusion was removed by EMR (endoscopic mucosal resection) successfully (Figure 1). The pathological report revealed a diagnosis of highly differentiated adenocarcinoma with a clean margin, but the immunohistochemical staining for synaptophysin (Syn), CgA and CD56 was positive (Figure 2). The tumor did not meet the diagnostic criteria for neuroendocrine tumors or carcinoids. Thus, we diagnosed duodenal adenocarcinoma with NEF. The patient refused further surgical treatment and was followed-up without any further treatment. There were no signs of recurrence or metastasis on esophagogastroduodenoscopy and color Doppler ultrasound of the epigastrium at the 2nd and 18th mo after EMR.
Previously, Kato et al[4] reported one case of duodenal adenocarcinoma with NEF at the descending part in a 67-year-old woman. However, it was accompanied by acromegaly and other types of tumors, namely GH-producing pituitary adenoma and thyroid papillary adenocarcinoma with familial clustering. As per the published literature, our report is the second instance of duodenal adenocarcinoma with NEF, especially without any concomitant endocrine diseases or other tumors. Moreover, it was located at the duodenal bulb, which is supposed to be physiologically, immunologically or otherwise uniquely privileged to virtually escape oncogenic transformation based on the extreme rarity of duodenal bulb adenocarcinoma[3]. Only five cases of adenocarcinoma have been clearly defined arising from the mucosa of the duodenal bulb on a diligent review of 724 reported cases in the published literature[3].
Generally, the prognosis of duodenal adenocarcinoma is poor; lymph node metastasis is the only independent predictor of decreased survival. Early surgery is required, although risk of surgical complications and death due to surgery are not ruled out[5-8]. Surgical resection can be variable and depends mainly on the location of the tumor. Tumors arising in the first, second or third portion of the duodenum typically require pancreaticoduodenectomy, whereas tumors occurring in the fourth portion may be more amenable to segmental duodenal resection[8]. However, the neuroendocrine component may have a considerable impact on duodenal adenocarcinoma[9]. One case of duodenal adenocarcinoma with NEF combined with liver metastasis survived for more than 24 mo without progression of the primary and metastatic lesions. It is plausible that duodenal adenocarcinoma with NEF is predominantly a neuroendocrine tumor of low malignancy potential, rather than a common adenocarcinoma[4]. Malignant NET, such as type 3 gastric NETs which are considered to be aggressive and often with metastasis, can also be treated successfully by endoscopic treatment, including EMR[10]. Endoscopic resection appears to be a safe and effective treatment for duodenal carcinoid tumors measuring ≤ 10 mm in diameter and confined to the submucosal layer[11]. Here, we removed the tumor with the lift and cut EMR method, in compliance with neuroendocrine tumors. This might be an optimal method for the treatment of duodenal adenocarcinomas with neuroendocrine differentiation (NED). The curative therapy in our case indicates that the treatment for the NEF component in duodenal adenocarcinoma is adequate.
Incidentally, the presence of NED remains a poor prognostic factor in other adenocarcinomas. In gastric adenocarcinomas, even a minor proportion of 10% of NED is associated with significantly poorer survival[12]. In a meta-analysis of 1587 cases of colorectal adenocarcinoma, patients with NED had a poor 5 year survival rate compared to those without NED[13]. In prostate cancer, NED is also a poorer prognostic factor. The levels of serum CgA are increased in patients with prostate cancer compared with benign conditions. The early detection of high serum levels of CgA could be an indicator for a change to a more aggressive therapy[14]. Although the exact function of the NEF component is still unknown, it is evident that the NEF component in duodenal and other adenocarcinomas apparently has different functions.
Here, we present a rare case of duodenal bulb adenocarcinoma with NED, which was successfully removed by EMR and has remained curative during the follow-up time. Duodenal adenocarcinoma with NEF might be treated as a neuroendocrine tumor and the role of NED in duodenal adenocarcinoma still needs further study.
We would like to give our thanks to Dr. P Sivaramakrishna Rachakongda from the Division of Molecular Genetic Epidemiology at the German Cancer Research Center for the revision of the manuscript.
A 63-year-old Han Chinese woman complained of anorexia and epigastric fullness for over two years.
One lesion of duodenal bulb was detected by endoscopy.
The differential diagnosis of lesion of the duodenal bulb should be polyps and other benign diseases.
Biochemical examinations were all in the normal range, except that the serum chromogranin (CgA) level was 151 ng/mL (reference: 27-94 ng/mL).
Esophagogastroduodenoscopy from the local hospital revealed a protrusion in the duodenum the size of 0.6 cm × 0.6 cm, which was also detected by the multi-row computed tomography of the small intestine, without lymph node involvement.
The pathological report revealed a diagnosis of highly differentiated adenocarcinoma with positive immunohistochemical staining for synaptophysin (Syn), CgA and CD56, which did not meet the diagnostic criteria for neuroendocrine tumors or carcinoids and duodenal adenocarcinoma with neuroendocrine features (NEF) was diagnosed.
The duodenal protrusion was successfully removed by endoscopic mucosal resection (EMR).
One case of duodenal adenocarcinoma with NEF with liver metastasis reported in a 67-year-old woman was accompanied by acromegaly and other types of tumors, namely GH-producing pituitary adenoma and thyroid papillary adenocarcinoma with familial clustering.
EMR is an endoscopic technique used to remove cancerous or other abnormal lesions found in the gastrointestinal tract.
Lesions at the duodenal bulb should not be underestimated due to the risk of malignant diseases.
Duodenal adenocarcinoma with NEF might be a low malignant neuroendocrine tumor rather than a conventional adenocarcinoma. Endoscopic treatment, including EMR, might be an ideal option for adenocarcinomas with NEF. However, only one case cannot provide strong support for the idea.
| 1. | Aparicio T, Zaanan A, Svrcek M, Laurent-Puig P, Carrere N, Manfredi S, Locher C, Afchain P. Small bowel adenocarcinoma: epidemiology, risk factors, diagnosis and treatment. Dig Liver Dis. 2014;46:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 225] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 2. | Neugut AI, Jacobson JS, Suh S, Mukherjee R, Arber N. The epidemiology of cancer of the small bowel. Cancer Epidemiol Biomarkers Prev. 1998;7:243-251. [PubMed] |
| 3. | Goldner B, Stabile BE. Duodenal adenocarcinoma: why the extreme rarity of duodenal bulb primary tumors? Am Surg. 2014;80:956-959. [PubMed] |
| 4. | Kato K, Takeshita Y, Misu H, Ishikura K, Kakinoki K, Sawada-Kitamura S, Kaneko S, Takamura T. Duodenal adenocarcinoma with neuroendocrine features in a patient with acromegaly and thyroid papillary adenocarcinoma: a unique combination of endocrine neoplasia. Endocr J. 2012;59:791-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Rose DM, Hochwald SN, Klimstra DS, Brennan MF. Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg. 1996;183:89-96. [PubMed] |
| 6. | Scott-Coombes DM, Williamson RC. Surgical treatment of primary duodenal carcinoma: a personal series. Br J Surg. 1994;81:1472-1474. [PubMed] |
| 7. | Sohn TA, Lillemoe KD, Cameron JL, Pitt HA, Kaufman HS, Hruban RH, Yeo CJ. Adenocarcinoma of the duodenum: factors influencing long-term survival. J Gastrointest Surg. 1998;2:79-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 112] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Poultsides GA, Huang LC, Cameron JL, Tuli R, Lan L, Hruban RH, Pawlik TM, Herman JM, Edil BH, Ahuja N. Duodenal adenocarcinoma: clinicopathologic analysis and implications for treatment. Ann Surg Oncol. 2012;19:1928-1935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 9. | Elias D, Cavalcanti de Albuquerque A, Eggenspieler P, Plaud B, Ducreux M, Spielmann M, Theodore C, Bonvalot S, Lasser P. Resection of liver metastases from a noncolorectal primary: indications and results based on 147 monocentric patients. J Am Coll Surg. 1998;187:487-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 126] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Kwon YH, Jeon SW, Kim GH, Kim JI, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Choi KD. Long-term follow up of endoscopic resection for type 3 gastric NET. World J Gastroenterol. 2013;19:8703-8708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Kim GH, Kim JI, Jeon SW, Moon JS, Chung IK, Jee SR, Kim HU, Seo GS, Baik GH, Lee YC. Endoscopic resection for duodenal carcinoid tumors: a multicenter, retrospective study. J Gastroenterol Hepatol. 2014;29:318-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Park JY, Ryu MH, Park YS, Park HJ, Ryoo BY, Kim MG, Yook JH, Kim BS, Kang YK. Prognostic significance of neuroendocrine components in gastric carcinomas. Eur J Cancer. 2014;50:2802-2809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (2)] |
| 13. | Zeng YJ, Lai W, Liu L, Wu H, Luo XX, Wang J, Chu ZH. Prognostic significance of neuroendocrine differentiation in colorectal adenocarcinoma after radical operation: a meta-analysis. J Gastrointest Surg. 2014;18:968-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Sagnak L, Topaloglu H, Ozok U, Ersoy H. Prognostic significance of neuroendocrine differentiation in prostate adenocarcinoma. Clin Genitourin Cancer. 2011;9:73-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Arbizu EA, Ahmad J, Stift A S- Editor: Yu J L- Editor: Roemmele A E- Editor: Wang CH