Published online Jun 21, 2015. doi: 10.3748/wjg.v21.i23.7326
Peer-review started: January 16, 2015
First decision: March 10, 2015
Revised: March 25, 2015
Accepted: April 28, 2015
Article in press: April 28, 2015
Published online: June 21, 2015
Processing time: 157 Days and 0.6 Hours
Hemangioma is the most common type of benign tumor that arises in the liver. Although rupture and hemorrhage of hepatic hemangioma are rare complications, they can be the cause of mortality. The authors report a case of hemorrhagic hepatic hemangioma: in a 54-year-old woman who was admitted with epigastric pain. She had taken oral contraceptives several weeks prior. The results of a blood examination were normal. An abdominal computed tomography scan revealed a tumor in hepatic segment 4, and a hemorrhage inside the cystic mass was suspected. The mass was removed laparoscopically to confirm the tumor properties and control the hemorrhage. The pathologic findings of the resected mass were consistent with hepatic hemangioma with intratumoral hemorrhage. The patient was discharged 8 d after the surgery, without further complications or complaints, and the patient’s condition was found to have improved during follow-up.
Core tip: Hemangioma is the most common type of benign tumor arising in the liver. Although rupture and hemorrhage of hepatic hemangioma are rare complications, they can be fatal. The authors report a case of hemorrhagic hepatic hemangioma. Compared to other benign hepatic tumor masses, the clinical importance of hemangioma can be easily overlooked. However, if the patient exhibits abdominal symptoms with a history associated with increased blood estrogen levels, a careful examination is necessary to determine whether these symptoms might be accompanied by internal hemorrhage.
- Citation: Kim JM, Chung WJ, Jang BK, Hwang JS, Kim YH, Kwon JH, Choi MS. Hemorrhagic hemangioma in the liver: A case report. World J Gastroenterol 2015; 21(23): 7326-7330
- URL: https://www.wjgnet.com/1007-9327/full/v21/i23/7326.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i23.7326
Hemangioma is the most common type of benign tumor arising in the liver and is frequently detected incidentally during imaging examinations[1]. The prevalence of biopsy-confirmed hemangioma is about 3%-20%, and is most common in middle-aged women[2].
Because patients with hepatic hemangioma often do not have clear symptoms, and most exhibit normal liver function[3], in many cases, tumor progression is monitored without treatment. Treatment becomes necessary when the tumor size increases to the point of causing symptoms such as abdominal pain, vomiting, abdominal discomfort, loss of appetite, or complications such as tumor rupture or hemorrhage[4-6].
Although rupture and hemorrhage of hepatic hemangioma are rare complications, , they can be fatal[7]. While there have been a considerable number of reports on the natural rupture of hemangioma to date[7-10], reports on internal hemorrhage are rare[11-13]. The authors report a case of hemorrhagic hepatic hemangioma diagnosed incidentally during the examination of a 54-year-old woman hospitalized for epigastric pain.
A 54-year-old woman was admitted to Keimyung University Dongsan Hospital. She experienced persistent pain in the epigastrium lasting 2 mo, and initially visited a private clinic, where a tumor mass was detected by an ultrasound examination. She continued to experience a dull pain which eventually intensified. She had no history of viral hepatitis, had taken oral contraceptives several weeks prior, and did not experience recent weight loss. Her father had died of lung cancer, but no other notable conditions were present in the family history. On physical examination, her conjunctiva was not pale, jaundice was not observed in her sclera, and no irregular noise was heard from her heart or lungs on auscultation. Her liver was not palpable below the costal margin, but epigastric tenderness was observed without rebound tenderness. No ascites or lower extremity edema was observed.
A blood test identified the following: white blood cell count: 4400/mm3 (normal range: 5200-12000/mm3), hemoglobin level: 12.4 g/dL (normal range: 12-18 g/dL), platelet count: 289000/mm3(normal range: 130000-400000/mm3), alkaline phosphatase (ALP) level: 56 U/L (normal range: 104-338 U/L), aspartate aminotransferase (AST) level: 27 U/L (normal range: 8-38 U/L), alanine transaminase (ALT) level: 16 U/L (normal range: 4-44 U/L), γ-glutamyltransferase (γ-GT) level: 23 U/L (normal range: 16-73 U/L), bilirubin level: 0.9 mg/dL (normal range: 0.0-0.4 mg/dL), HBsAg negative, anti-HBs Ab positive, and anti-HCV Ab negative. Concentrations of all tumor markers were within the normal range: alpha fetoprotein (AFP): 2.96 ng/mL (normal range: < 8.1 ng/mL), carcinoembryonic antigen(CEA): 2.65 ng/mL(normal range: < 2.5 ng/mL), and carbohydrate antigen 19-9 (CA 19-9): 0.60 U/mL (normal range: < 37 U/mL).
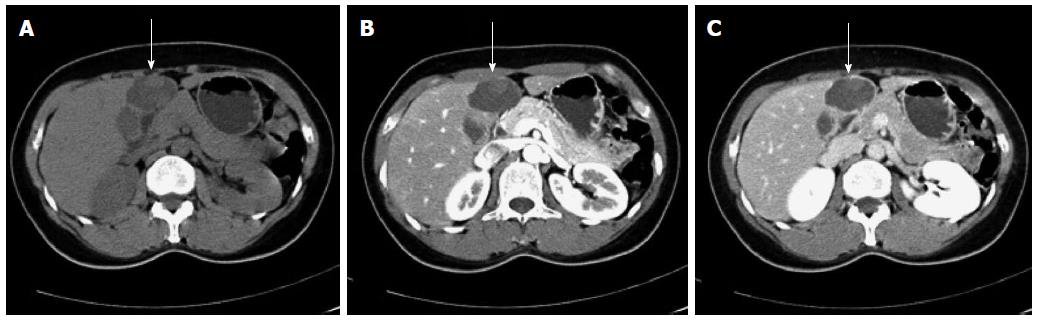
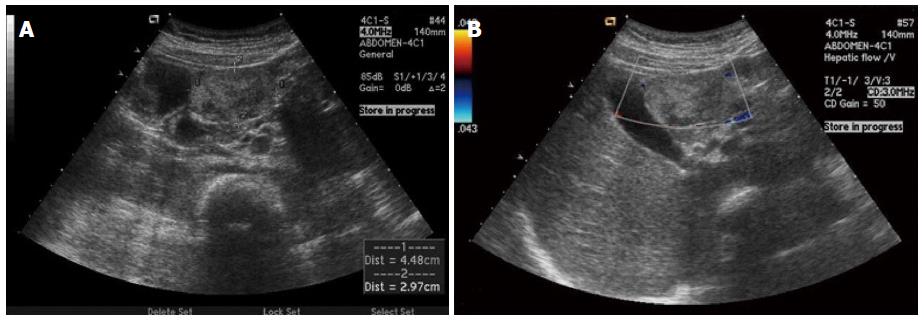
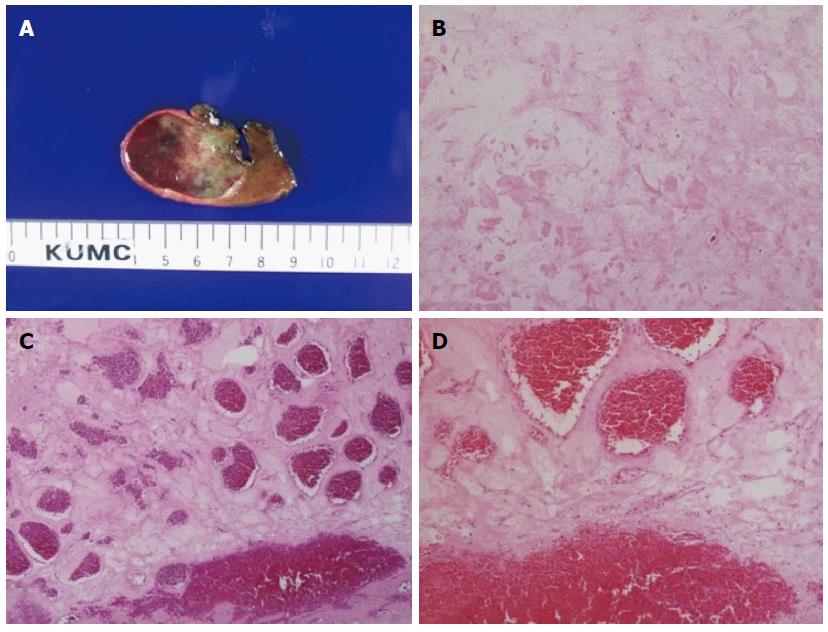
An ultrasound examination performed at a private clinic 3 d before admission, and revealed a cystic mass, approximately 5cm in size in the left lobe of the liver. An abdominal computed tomography (CT) scan identified a 44 mm × 28 mm cystic mass in hepatic segment 4 (Figure 1, arrows), and a high density, non-enhanced lesion was found within the cyst (Figure 1). While the overall size and shape of the liver were normal, a number of small cysts were observed. The spleen, pancreas, gall bladder and kidneys were unremarkable. Since hemorrhage inside the cystic mass was suspected upon abdominal CT scan, Doppler sonography was performed. Heterogeneous echotexture was found inside the round and solid mass upon Doppler sonography (Figure 2), but active bleeding was not found. Although a histological examination was performed to confirm the properties of the tumor, a firm conclusion could not be reached from the obtained data. Therefore, to confirm the tumor properties and control the hemorrhage, the mass was removed laparoscopically. The surgically confirmed mass was rubbery and round-shaped, containing necrotic materials and hemorrhagic components. The results of the histological examination of the resected mass were consistent with hepatic hemangioma with intratumoral hemorrhage (Figure 3).
The patient was discharged 8 d after the surgery, without further complications or complaints, and the patient’s condition was found to have improved during follow-up.
Because most hemangiomas are relatively small, they are typically observed only after significant time has passed. Various imaging techniques are used to diagnose hemangioma; while ultrasound, CT, or magnetic resonance imaging (MRI) are the techniques most often used, occasionally positron emission tomography (PET) or angiography are used for diagnosis. The sensitivities of ultrasound, CT, or MRI are greater than 90%, while specificity reportedly ranges from 55%-85%[14]. Using ultrasound, hemangioma appears as a uniform hyperechoic mass with a relatively clear boundary, but can appear hypoechoic when the mass is accompanied by hemorrhage, fibrosis, or calcification[15]. In multiphasic CT, nodular or spherical contrast enhancement around the tumor edges is observed in the initial contrast phase, and afferent contrast is enhanced as time progresses. In the late contrast phase, contrast is uniformly enhanced in the entire tumor[16]. In addition, when intratumoral hemorrhage is present, the hemangioma appears as a mass with a highly dense interior[13].
A hemangioma larger than 4 cm is classified as a “giant hemangioma”[17] and causes abdominal discomfort or pain as the tumor size increases. Treatment, including surgery, is necessary for giant hemangioma accompanied by symptoms or complications[4-6]. The most serious complications include tumor rupture, internal hemorrhage, and a coagulation disorder called Kasabach-Merritt syndrome. Since the mortality rate is very high when these complications occur, immediate treatment is necessary. Because the patient in the current case complained of epigastric pain, and a hemangioma larger than 4 cm accompanied by internal hemorrhage was found upon examination, immediate treatment was considered necessary, and surgery was performed.
The treatment methods for hepatic hemangioma include transarterial embolization, radiological therapy, and liver transplantation, in addition to surgical resection[6,18]. Transarterial embolization increases surgical safety by reducing hemorrhage. Radiotherapy and hepatic artery ligation therapy are known to be less effective than transarterial embolization. Liver transplantation is an option for treating giant hemangioma for which surgical resection is impossible[19]. In a recent report, a hemangioma was shrunk using monoclonal antibodies such as bevacizumab[14] or sorafenib[20].
While the pathophysiology of hemangioma is not clearly defined, it is known that abnormal vasculogenesis and angiogenesis may be involved[21]. These processes are prompted by an increase in angiogenic factors such as vascular endothelial growth factors (VEGF) and matrix metalloproteinases (MMPs) and a decrease in anti-angiogenic factors[22,23]. Tumor growth is promoted by high blood estrogen levels during puberty, pregnancy, oral contraceptive use, and androgen treatment[2]. The patient in the current case had taken oral birth control pills for an extended period of time, and there is a possibility that this led to an internal hemorrhage in the hemangioma.
Reports on internal hemorrhage of hemangioma are very rare, and only three cases have been reported worldwide. Graham et al[12] reported a case of internal hemorrhage of hemangioma in a pregnant patient, and Shimoji et al[13] reported a case of hemangioma accompanied by subacute hemorrhage and hemorrhagic anemia in a patient who was undergoing a 5-year follow-up after being diagnosed with hemangioma. Feldman et al[11] reported a case of internal hemorrhage of hemangioma in a 39-year-old man without any indicative factors in his history. Although there have been cases of hemangioma rupture in Korea, there have been no reported cases of internal hemorrhage of hemangioma. Compared to other benign hepatic tumor masses, the clinical importance of hemangioma can be easily overlooked, since it is relatively common and mostly asymptomatic. However, if the patient exhibits abdominal symptoms with a history indicative of increased blood estrogen levels, a careful examination is necessary to determine whether these symptoms might be accompanied by internal hemorrhage.
A 54-year-old female with a history of taking oral contraceptives presented with epigastric pain.
Hepatic hemangioma.
Hepatic adenoma, sarcoma, hepatocellular carcinoma.
WBC 4400/mm3; HGB 12.4 g/dL; liver function test and tumor markers were within normal limits.
Computed tomography scan showed a cystic mass in hepatic segment 4, and intratumoral hemorrhage was suspected.
Pathologic review revealed a hepatic hemangioma with intratumoral hemorrhage.
The patient was treated with laparoscopic removal of the mass.
Reports on internal hemorrhage of hemangioma are very rare, and only three cases have been reported worldwide.
A careful examination is necessary to determine whether the patient’s symptoms might be accompanied by internal hemorrhage
The authors described an uncommon and interesting case of a patient with hemorrhagic hepatic hemangioma and they reviewed 3 documented cases with intratumoral hemorrhage in hepatic hemangioma.
| 1. | Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975;59:995-1013. [PubMed] |
| 2. | Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol. 2005;39:401-412. [PubMed] |
| 3. | Gandolfi L, Leo P, Solmi L, Vitelli E, Verros G, Colecchia A. Natural history of hepatic haemangiomas: clinical and ultrasound study. Gut. 1991;32:677-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 182] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Althaus S, Ashdown B, Coldwell D, Helton WS, Freeny PC. Transcatheter arterial embolization of two symptomatic giant cavernous hemangiomas of the liver. Cardiovasc Intervent Radiol. 1996;19:364-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Giavroglou C, Economou H, Ioannidis I. Arterial embolization of giant hepatic hemangiomas. Cardiovasc Intervent Radiol. 2003;26:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Srivastava DN, Gandhi D, Seith A, Pande GK, Sahni P. Transcatheter arterial embolization in the treatment of symptomatic cavernous hemangiomas of the liver: a prospective study. Abdom Imaging. 2001;26:510-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 80] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | SEWELL JH, WEISS K. Spontaneous rupture of hemangioma of the liver. A review of the literature and presentation of illustrative case. Arch Surg. 1961;83:729-733. [PubMed] |
| 8. | Donati M, Stavrou GA, Donati A, Oldhafer KJ. The risk of spontaneous rupture of liver hemangiomas: a critical review of the literature. J Hepatobiliary Pancreat Sci. 2011;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Gupta S, Agarwal V, Acharya AN. Spontaneous rupture of a giant hepatic hemangioma-report of a case. Indian J Surg. 2012;74:434-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Jain V, Ramachandran V, Garg R, Pal S, Gamanagatti SR, Srivastava DN. Spontaneous rupture of a giant hepatic hemangioma - sequential management with transcatheter arterial embolization and resection. Saudi J Gastroenterol. 2010;16:116-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Feldman PA, Regev A. Atypical giant hepatic hemangiomas with intratumoral hemorrhage. Clin Gastroenterol Hepatol. 2007;5:A24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Graham E, Cohen AW, Soulen M, Faye R. Symptomatic liver hemangioma with intra-tumor hemorrhage treated by angiography and embolization during pregnancy. Obstet Gynecol. 1993;81:813-816. [PubMed] |
| 13. | Shimoji K, Shiraishi R, Kuwatsuru A, Maehara T, Matsumoto T, Kurosaki Y. Spontaneous subacute intratumoral hemorrhage of hepatic cavernous hemangioma. Abdom Imaging. 2004;29:443-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Toro A, Mahfouz AE, Ardiri A, Malaguarnera M, Malaguarnera G, Loria F, Bertino G, Di Carlo I. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann Hepatol. 2014;13:327-339. [PubMed] |
| 15. | Ho HY, Wu TH, Yu MC, Lee WC, Chao TC, Chen MF. Surgical management of giant hepatic hemangiomas: complications and review of the literature. Chang Gung Med J. 2012;35:70-78. [PubMed] |
| 16. | Valette PJ, Pilleul F, Crombé-Ternamian A. MDCT of benign liver tumors and metastases. Eur Radiol. 2003;13 Suppl 5:M31-M41. [PubMed] |
| 17. | Nelson RC, Chezmar JL. Diagnostic approach to hepatic hemangiomas. Radiology. 1990;176:11-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 91] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Alper A, Ariogul O, Emre A, Uras A, Okten A. Treatment of liver hemangiomas by enucleation. Arch Surg. 1988;123:660-661. [PubMed] |
| 19. | Ferraz AA, Sette MJ, Maia M, Lopes EP, Godoy MM, Petribú AT, Meira M, Borges Oda R. Liver transplant for the treatment of giant hepatic hemangioma. Liver Transpl. 2004;10:1436-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Yamashita S, Okita K, Harada K, Hirano A, Kimura T, Kato A, Okita K. Giant cavernous hepatic hemangioma shrunk by use of sorafenib. Clin J Gastroenterol. 2013;6:55-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Giannitrapani L, Soresi M, La Spada E, Cervello M, D’Alessandro N, Montalto G. Sex hormones and risk of liver tumor. Ann N Y Acad Sci. 2006;1089:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 22. | Chang J, Most D, Bresnick S, Mehrara B, Steinbrech DS, Reinisch J, Longaker MT, Turk AE. Proliferative hemangiomas: analysis of cytokine gene expression and angiogenesis. Plast Reconstr Surg. 1999;103:1-9; discussion 10. [PubMed] |
| 23. | Takahashi K, Mulliken JB, Kozakewich HP, Rogers RA, Folkman J, Ezekowitz RA. Cellular markers that distinguish the phases of hemangioma during infancy and childhood. J Clin Invest. 1994;93:2357-2364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 454] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Coy CSR, Kang WK S- Editor: Yu J L- Editor: A E- Editor: Liu XM