Published online Jan 14, 2015. doi: 10.3748/wjg.v21.i2.637
Peer-review started: May 13, 2014
First decision: June 10, 2014
Revised: July 7, 2014
Accepted: August 28, 2014
Article in press: August 28, 2014
Published online: January 14, 2015
Processing time: 250 Days and 19.6 Hours
AIM: To evaluate adherence of primary care physicians (PCPs) to international guidelines when referring patients for upper-gastrointestinal endoscopy (UGE), evaluate the importance of alarm symptoms and the performance of the American Society for Gastrointestinal Endoscopy (ASGE) guidelines in a Saudi population.
METHODS: A prospective, observational cross-sectional study on dyspeptic patients undergoing UGE who were referred by PCPs over a 4 mo period. Referrals were classified as appropriate or inappropriate according to adherence to ASGE guidelines.
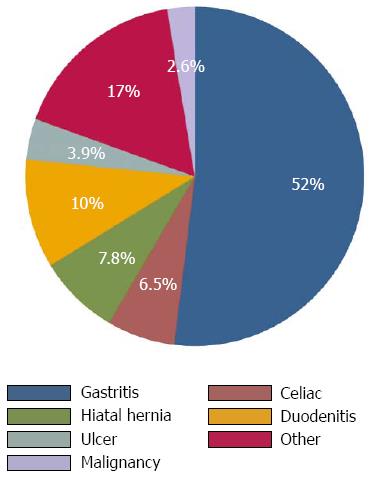
RESULTS: Total of 221 dyspeptic patients was enrolled; 161 patients met our inclusion criteria. Mean age was 40.3 years (SD ± 18.1). Females comprised 70.1%. Alarm symptoms included low hemoglobin level (39%), weight loss (18%), vomiting (16%), loss of appetite (16%), difficulty swallowing (3%), and gastrointestinal bleeding (3%). Abnormal endoscopy findings included gastritis (52%), duodenitis (10%), hiatus hernia (7.8%), features suggestive of celiac disease (6.5%), ulcers (3.9%), malignancy (2.6%) and gastroesophageal reflux disease (GERD: 17%). Among patients who underwent UGE, 63% met ASGE guidelines, and 50% had abnormal endoscopic findings. Endoscopy was not indicated in remaining 37% of patients. Among the latter group, endoscopy was normal in 54% of patients. There was no difference in proportion of abnormal endoscopic findings between two groups (P = 0.639).
CONCLUSION: Dyspeptic patients had a low prevalence of important endoscopic lesions, and none of the alarm symptoms could significantly predict abnormal endoscopic findings.
Core tip: A prospective study looking at the practice of primary care physicians in referring dyspeptic patients for endoscopy in Saudi Arabia, such study is the first prospective study to evaluate such practice in high Helicobacter pylori endemic area and the adherence of general practitioners to the international guidelines for a common gastroenterology disorder, and this will shed light on the approach for such disease.
- Citation: Azzam NA, Almadi MA, Alamar HH, Almalki LA, Alrashedi RN, Alghamdi RS, Al-hamoudi W. Performance of American Society for Gastrointestinal Endoscopy guidelines for dyspepsia in Saudi population: Prospective observational study. World J Gastroenterol 2015; 21(2): 637-643
- URL: https://www.wjgnet.com/1007-9327/full/v21/i2/637.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i2.637
Dyspepsia is a complex condition comprising a spectrum of chronic and recurrent symptoms related to the upper gastrointestinal tract. The cardinal symptoms are epigastric pain, discomfort, including postprandial fullness and early satiety, which may overlap with heartburn and regurgitation[1]. These symptoms could be the result of underlying organic pathology, such as chronic peptic ulcer disease, gastro-esophageal reflux or malignancy (organic dyspepsia). Dyspepsia can also present without evidence of organic cause (functional dyspepsia). Dyspepsia is a common condition that affects up to 80% of the population at some point during an individual’s lifetime[2]. Multiple studies have shown that the condition is experienced by approximately 20%-40% of the general adult population and accounts for 3%-4% of all consultations in primary care[3-5]. In Western countries, studies have suggested that dyspepsia affects approximately a one-fourth of the population[6,7]. In Japan, India, and Turkey, the prevalence of dyspepsia has been estimated to be 17%, 30.4%, and 28.4%, respectively[8-10].
Dyspepsia is the most common indication for upper gastrointestinal endoscopy (UGE)[11-13]. It has been estimated that approximately 50% of all UGE referrals are dyspepsia related[14]. In approximately half of all dyspeptic cases, the endoscopic investigation reveals no underlying organic lesion[15-17].
The overwhelming number of dyspeptic patients referred for UGE has led to prolonged waiting times for endoscopic procedures, especially in the setting of open-access endoscopy units that allow general practitioners to request an endoscopic procedure without referral to a specialist. Concerns include the high cost, unnecessary burden on available resources and long waiting lists[18]. To reduce these problems and increase the effectiveness of endoscopy, adherence to treatment guidelines has been recommended[19,20]. Despite variability in composition, the recommendations of the majority of the guidelines are similar[21]. All suggest that dyspeptic patients who are over the age of 50 years and/or those with alarm symptoms at any age need urgent referral for endoscopy as an initial management strategy because endoscopy would change the management of this subset of patients[22-24]. In young patients without alarm symptoms, however, either a “test or treat” for Helicobacter pylori (H. pylori) in high-prevalence areas or an empirical acid-suppression trial are the initial management strategies of choice[24]. Saudi Arabia is considered to be a high prevalence area and estimated to be around 50%[25].
At King Khalid University Hospital (KKUH), the endoscopy unit is an open-access unit that receives a large number of referrals from various general and specialty clinics and from in-patient wards. Annually, more than eight thousand procedures are completed in the unit. The most common indication for UGE is dyspepsia, accounting for thousands of referrals, with approximately 50% from the primary care clinics[26]. This creates a significant burden on the allocated resources and negatively impacts waiting times. In this prospective study, we aimed to evaluate the adherence of primary care physicians (PCPs) to dyspepsia guidelines, to describe the common endoscopic findings, to evaluate the importance of “red flag” symptoms and to estimate the prevalence of H. pylori in dyspeptic patients. To our knowledge, this is the first study to evaluate such practices in an H. pylori high-prevalence region.
Prospective, cross-sectional study on dyspeptic patients undergoing UGE in an open-access endoscopy unit was conducted. Data on all adult patients referred from PCPs to the Endoscopy Unit at KKUH, Riyadh, KSA, were prospectively collected over a period of 4 mo, starting from December 2012 and ending in April 2013. Dyspepsia was defined as chronic and recurrent epigastric pain or discomfort (including postprandial fullness and early satiety) with or without heartburn and regurgitation. Patients who had gastroesophageal reflux disease (GERD)-predominant symptoms such as heartburn or acid regurgitation alone, inflammatory bowel disease, a previously diagnosed malignancy or advanced liver disease were excluded from the study.
Upon presentation to the endoscopy unit, all patients who met our inclusion criteria were enrolled in the study and provided informed consent. The participants were interviewed by an endoscopist using a pre-designed data collection sheet (Table 1).
| Variable | Description |
| Age | < 50 yr of age |
| ≥ 50 yr of age | |
| Gender | Male or female |
| Alarm symptoms | Anemia |
| Hemoglobin level | |
| Male: < 13 g/dL | |
| Female: < 12 g/dL | |
| Weight loss of more than 4 kg | |
| Vomiting | |
| Loss of appetite | |
| Dysphagia | |
| Gastrointestinal bleeding | |
| Palpable abdominal mass | |
| Other independent variables | Smoking |
| Use of NSAID | |
| History of Helicobacter pylori treatment |
Endoscopic findings were noted, and gastric biopsies were obtained to rule out H. pylori by utilizing the rapid urease test (Lencomm trade international, Poland). The biopsy samples were inoculated immediately into the rapid urease test gel. If the gel color changed within 20 min up to a maximum of 60 min the sample was considered positive for H. pylori.
Referrals were classified as appropriate or inappropriate according to adherence to ASGE guidelines. These included patients over the age of 50 years or those that presented with alarm symptoms at any age. Alarm symptoms included anemia, vomiting, loss of appetite, weight loss, gastrointestinal bleeding, dysphagia or the presence of a palpable abdominal mass. The endoscopic findings were categorized as normal or abnormal. Abnormal findings included gastritis, duodenitis, peptic ulcer, varices, features of celiac disease, hiatus hernia malignancy and others. Endoscopic findings were defined as important if the abnormalities included gastric or duodenal ulcers, varices, duodenitis, adenomatous polyps or malignancy[3].
Sample size calculation: Based on an a priori baseline prevalence of abnormal findings on endoscopy of 60%[25], Using the rule of 10 outcome events per predictor variable, and given we wished to include up to 9 variables in our multivariable model, we estimated that 150 individuals would be needed to provide sufficient accuracy within the multivariable analysis.
Data analysis: included descriptive statistics computed for continuous variables, including means, SD, minimum and maximum values, as well as 95%CI. Frequencies are used for categorical variables. We used hypothesis testing, the t test with unequal variances, as well as Fisher’s exact test where appropriate.
Univariable and multivariable logistic regressions were used to examine the association between independent variables and the dependent variable the presence of an abnormality at endoscopy. Independent variables included; age, gender, smoking status, the use of non-steroidal anti-inflammatory medications (NSAIDs), history of weight loss, vomiting, loss of appetite, dysphagia, gastrointestinal bleeding, history of prior endoscopy, as well as the patients hemoglobin level as well as if they were infected with H. pylori. OR and 95%CI were calculated. Characteristics of test procedure (sensitivity, specificity) were used to evaluate the performance of the latest ASGE guidelines in detecting abnormalities on endoscopy.
We used the software STATA 11.2 (Stata Corp, TX, United States) in our analysis. A statistical significance threshold of P = 0.05 was adopted. No attempt at imputation was made for missing data.
A total of 221 patients were screened and 161 patients met our inclusion criteria. The mean age was 40.3 years (SD ± 18.1), and age ranged from 18 years to 98 years. Females represented 70.1% of the patients, while males represented 29.9%. The proportion of patients with alarm symptoms in our study was 39%; 39% had a low hemoglobin level, 18% had weight loss, 16% had vomiting, 16% had loss of appetite, 3% had difficulty in swallowing, 3% had gastrointestinal bleeding, and 2% had an epigastric mass on physical examination (Table 2). At least one alarm feature was observed in 79.4% of the females, and one alarm feature was observed in only 20.6% of the males (P value < 0.01). A proportion of the patients included in the study had incurred prior endoscopic procedures (29%); 60% of those had one prior endoscopy, 20% had two prior endoscopies, 6% had 3 prior endoscopies, and 12% had 4 previous endoscopies.
| Characteristics | Percentage of patients | Normal | Abnormal | P value | Univariable analysis |
| OR (95%CI) | |||||
| Female | 70.1% | 53% | 47% | 0.399 | 0.7 (0.37-1.47) |
| Male | 29.9% | 45% | 55% | 0.711 | 1.02 (0.97-1.56) |
| Age ≥ 50 | 29% | 60% | 40% | 0.094 | 1.01 (0.99-1.04) |
| Smoker | 12% | 42% | 58% | 0.671 | 1.49 (0.56-3.94) |
| Taking NSAID | 14% | 35% | 65% | 0.094 | 2.16 (0.86-5.44) |
| Vomiting | 18% | 47% | 53% | 0.285 | 1.25 (0.54-2.91) |
| Prior endoscopy | 29% | 38% | 62% | 0.039 | 2.06 (1.02-4.13) |
| Weight loss | 16% | 46% | 54% | 0.283 | 1.2 5(0.54-2.91) |
| Loss of appetite | 16% | 46% | 54% | 0.283 | 1.25 (0.54-2.91) |
| Dysphagia | 3% | 20% | 80% | 0.161 | 4.32 (0.47-39.52) |
| GI bleeding | 3% | 20% | 80% | 0.161 | 4.32 (0.47-39.52) |
| Epigastric mass | 2% | 0% | 100% | 0.075 | |
| Low Hb | 39% | 41% | 59% | 0.245 | 1.08 (0.94-1.25) |
| Presence of H. pylori | 22% | 36% | 64% | 0.044 | 2.2 (1.01-4.87) |
The mean hemoglobin level was 12.89 ± 0.17 g/dL.
According to the ASGE guidelines, 63% of the endoscopies were considered to be indicated; the results were abnormal in 50%, while 50% were normal.
Although 37% of the endoscopies were considered inappropriate, 54% had abnormal findings. There was no difference in the proportion of abnormal endoscopic findings between the two groups (P = 0.639; Table 3).
| Endoscopy finding | ASGE indicated | ASGE not indicated | P value |
| (63%) | (37%) | ||
| Normal | 50% | 54% | |
| Abnormal | 50% | 46% | 0.6390 |
| Important endoscopic finding | 8% | 3% | 0.7806 |
The most common endoscopic findings were gastritis in 52%, duodenitis in 10%, hiatus hernia in 7.8%, ulcers in 3.9% and malignancy in 2.6% of the patients; the remaining 17% were found to have reflux esophagitis signifying GERD. Furthermore, 6.5% had endoscopic features suggestive of celiac disease (Figure 1).
The rapid urease test was positive in 22% of the patients. The majority (62%) of those was younger than 50 years of age, and 20% had a history of receiving eradication therapy for H. pylori.
All procedures were completed successfully, and no adverse events occurred.
The only factors associated with the presence abnormal endoscopy on univariable analysis were H. pylori OR = 2.2 (95%CI: 1.01-4.87) and having undergone a previous endoscopy OR = 2.0 (95%CI: 1.02-4.13).
Using stepwise multivariable logistic regression, none of the variables included in the study could predict the finding of abnormalities at the time of endoscopy.
This prospective observational study found that overuse of upper gastrointestinal endoscopy is common in dyspeptic patients, between 25% and 40% of individuals with dyspepsia will consult a PCP as a result of their symptoms[27]. With such high prevalence, dyspepsia is a diagnostic and therapeutic challenge to physicians. Furthermore, most patients with dyspepsia have no detectable organic abnormality[22,28].Thus, endoscopic evaluation as an initial step in management is not recommended[9,29]. Endoscopic evaluation is recommended for older patients (older than 50 years), those with alarm symptoms, those taking NSAID, and those with persistent symptoms after acid suppression therapy and/or H. pylori eradication[18,30].
We found that approximately 40% of the patients complaining of upper abdominal symptoms had a normal finding according to the dyspepsia guidelines[20]. The specialty of the referring physicians affects the presumed etiology of upper gastrointestinal symptoms. The sensitivity and specificity for the diagnosis of functional dyspepsia was 61% and 84% for PCPs, respectively, while it was 73% and 37% for gastroenterologists, respectively[31]. In a large Canadian study, 1040 patients were evaluated for symptoms and underwent endoscopy within 10 d of referral. In this study, the predominant symptom was not predictive of the endoscopic findings, and the presence of alarm symptoms did not correlate with the demonstration of clinically significant endoscopic findings[16]. Another study evaluated alarm symptoms in functional dyspepsia and concluded that the value of symptoms in diagnosing functional dyspepsia was poor[32]. These data suggest that these symptoms are of limited value in the assessment of dyspepsia.
Our study confirmed that the majority of patients with dyspepsia referred by PCPs had no important endoscopic lesion; approximately 40% were not indicated per the guidelines. Endoscopic abnormalities were found in only 48% of the patients; the majority had nonspecific gastritis, while important findings were observed in approximately 6%, with 2.6% of these patients having gastrointestinal malignancy. These results were similar to the findings of Choomsri et al[33] in which only important endoscopic lesions were found in 7% of the patients in the form of gastric ulcers and only 1% had gastric cancer. Moreover, in the present study, there were no clinical data such as age, smoking, NSAID use or alarm symptoms that could be used to predict the presence of important endoscopic lesions. This is in agreement with studies that found a poor positive predictive value for these symptoms[34,35]. It is thought that the presence of these alarm features are often indicative of advanced disease[36] and carry low diagnostic yield[37].
In young patients with uncomplicated dyspepsia, either a “test and treat” for H. pylori approach[38] or an empirical acid-suppression trial are recommended as first-line management strategies by most guidelines[20,39], depending on the prevalence of H. pylori.
The prevalence of H. pylori in the present study was 22%, and the majority of these patients were younger than 50 years (62%). Of interest, 20% of those testing positive for H. pylori had a previous history of receiving eradication therapy for H. pylori.
Abnormal endoscopic finding with important lesions were observed in only a small proportion of our study population, which is similar to a previous report[40]. The most cost-effective strategy in treating H. pylori is either empirical treatment or employment of a “test or treat” approach with consideration of endoscopy in a stepwise manner in dyspeptic patients, especially with the absence of alarm symptoms[41]. There is low prevalence of important endoscopic findings in H. pylori dyspeptic patients; therefore, a noninvasive method for diagnosing H. pylori would be the best modality rather than UGE because endoscopy remains a relatively expensive procedure and UGE is an invasive procedure that carries the risk of potential complications that may have grave consequences that exceed its benefit[42]. In our study, the presence of H. pylori was one of the predictors of an abnormal endoscopic finding. This has not been the case, however, according to multivariable analysis, which suggests the presence of an unmeasured confounder.
Gastroenterologists were found to be more likely than PCPs to comply with best practices for dyspepsia diagnosis and treatment, which could be due to PCPs having more concerns regarding long-term proton pump inhibitor use, which affects therapeutic decision making[26,43]. Studies showed an overall low dyspepsia guidelines compliance and such practice was observed in both developed and developing countries[25,33,40,43]. It is important to identify areas of disconnect between the guidelines and practices and to understand the predictors of low guideline compliance, which needs further studies employing larger populations.
The limitations of the present study included a relatively small sample size and the small number of important endoscopic lesions that were found, resulting in a low power to detect any clinically significant differences. Nonetheless, this study is one of the first prospective studies to address the appropriateness and diagnostic yield of endoscopy and adherence of PCPs to the international guidelines for dyspeptic patients in our region. We clearly demonstrate in this study the importance on adhering to the International dyspepsia guidelines when performing upper gastrointestinal endoscopy. We also believe that our hospital practices shed light on the medical approaches in our country that necessitate further studies. We, therefore advise the general practitioners to adopt these guidelines when evaluating patients with dyspepsia. Such practice would avoid unnecessary procedures and will result in an efficient utilization of resources.
In conclusion, the findings of the present study support selective UGE in patients with dyspepsia; a large number of UGE procedures in dyspeptic patients could be avoided. Further studies are needed to find prognostic markers for the abnormal findings in our patient population.
It’s a prospective study looking at the practice of primary care physicians in referring dyspeptic patients for endoscopy in Saudi Arabia, such study is the first prospective study to evaluate such practice in high Helicobacter pylori endemic area and the adherence of general practitioners to the international guidelines for a common gastroenterology disorder, and this will shed light on the approach for such disease.
To evaluate the adherence of primary care physicians to international guidelines when referring patients for upper-gastrointestinal endoscopy, describe the most common endoscopic findings, evaluate the importance of alarm symptoms and the performance of the American Society for Gastrointestinal Endoscopy (ASGE) guidelines in a Saudi population.
It’s a first of its kind prospective study looking at the practice of primary care physicians in referring dyspeptic patients for endoscopy in Saudi Arabia, such study might change the current practice of referring system for dyspeptic patients for upper gastrointestinal (GI) endoscopy, especially those with no alarming symptoms.
This proposal might change the current practice of referring system for dyspeptic patients for upper GI endoscopy, especially those with no alarming symptoms.
In this study, the authors have tried to demonstrate factors related to the positive endoscopic findings based on the ASGE guideline/ Study design is nice and analysis is clear. Their results should be useful for the general readers.
| 1. | National Institute for Health and Clinical Excellence. Dyspepsia: Management of dyspepsia in adults in primary care. Available from: http://www.nice.org.uk/CG017NICEguideline. |
| 2. | Grainger SL, Klass HJ, Rake MO, Williams JG. Prevalence of dyspepsia: the epidemiology of overlapping symptoms. Postgrad Med J. 1994;70:154-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Talley NJ, Vakil NB, Moayyedi P. American gastroenterological association technical review on the evaluation of dyspepsia. Gastroenterology. 2005;129:1756-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Heading RC. Prevalence of upper gastrointestinal symptoms in the general population: a systematic review. Scand J Gastroenterol Suppl. 1999;231:3-8. [PubMed] |
| 5. | El-Serag HB, Talley NJ. Systemic review: the prevalence and clinical course of functional dyspepsia. Aliment Pharmacol Ther. 2004;19:643-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 222] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 6. | Ikenberry SO, Harrison ME, Lichtenstein D, Dominitz JA, Anderson MA, Jagannath SB, Banerjee S, Cash BD, Fanelli RD, Gan SI. The role of endoscopy in dyspepsia. Gastrointest Endosc. 2007;66:1071-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12:2661-2666. [PubMed] |
| 8. | Hirakawa K, Adachi K, Amano K, Katsube T, Ishihara S, Fukuda R, Yamashita Y, Shiozawa S, Watanabe M, Kinoshita Y. Prevalence of non-ulcer dyspepsia in the Japanese population. J Gastroenterol Hepatol. 1999;14:1083-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Shah SS, Bhatia SJ, Mistry FP. Epidemiology of dyspepsia in the general population in Mumbai. Indian J Gastroenterol. 2001;20:103-106. [PubMed] |
| 10. | Kitapçioğlu G, Mandiracioğlu A, Caymaz Bor C, Bor S. Overlap of symptoms of dyspepsia and gastroesophageal reflux in the community. Turk J Gastroenterol. 2007;18:14-19. [PubMed] |
| 11. | Cooper GS. Indications and contraindications for upper gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 1994;4:439-454. [PubMed] |
| 12. | Taye M, Kassa E, Mengesha B, Gemechu T, Tsega E. Upper gastrointestinal endoscopy: a review of 10,000 cases. Ethiop Med J. 2004;42:97-107. [PubMed] |
| 13. | Olokoba AB, Olokoba LB, Jimoh AA, Salawu FK, Danburam A, Ehalaiye BF. Upper gastrointestinal tract endoscopy indications in northern Nigeria. J Coll Physicians Surg Pak. 2009;19:327-328. [PubMed] |
| 14. | Olokoba AB, Bojuwoye BJ. Indications for oesophagogastrod uodenoscopy in Ilorin, Nigeria-a 30 month review. Niger J Clin Pract. 2010;13:260-263. [PubMed] |
| 15. | Lieberman D, Fennerty MB, Morris CD, Holub J, Eisen G, Sonnenberg A. Endoscopic evaluation of patients with dyspepsia: results from the national endoscopic data repository. Gastroenterology. 2004;127:1067-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Thomson AB, Barkun AN, Armstrong D, Chiba N, White RJ, Daniels S, Escobedo S, Chakraborty B, Sinclair P, Van Zanten SJ. The prevalence of clinically significant endoscopic findings in primary care patients with uninvestigated dyspepsia: the Canadian Adult Dyspepsia Empiric Treatment - Prompt Endoscopy (CADET-PE) study. Aliment Pharmacol Ther. 2003;17:1481-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 177] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 17. | Vakil N, Moayyedi P, Fennerty MB, Talley NJ. Limited value of alarm features in the diagnosis of upper gastrointestinal malignancy: systematic review and meta-analysis. Gastroenterology. 2006;131:390-401; quiz 659-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 159] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 18. | Leddin D, Armstrong D, Barkun AN, Chen Y, Daniels S, Hollingworth R, Hunt RH, Paterson WG. Access to specialist gastroenterology care in Canada: comparison of wait times and consensus targets. Can J Gastroenterol. 2008;22:161-167. [PubMed] |
| 19. | Early DS, Ben-Menachem T, Decker GA, Evans JA, Fanelli RD, Fisher DA, Fukami N, Hwang JH, Jain R, Jue TL. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012;75:1127-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 187] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 20. | Talley NJ. American Gastroenterological Association medical position statement: evaluation of dyspepsia. Gastroenterology. 2005;129:1753-1755. [PubMed] |
| 21. | Ford AC, Moayyedi P. Current guidelines for dyspepsia management. Dig Dis. 2008;26:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, Stanghellini V. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466-1479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1243] [Cited by in RCA: 1207] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 23. | Meineche-Schmidt V, Jørgensen T. ‘Alarm symptoms’ in patients with dyspepsia: a three-year prospective study from general practice. Scand J Gastroenterol. 2002;37:999-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Shaw IS, Valori RM, Charlett A, McNulty CA. Limited impact on endoscopy demand from a primary care based ‘test and treat’ dyspepsia management strategy: the results of a randomised controlled trial. Br J Gen Pract. 2006;56:369-374. [PubMed] |
| 25. | Aljebreen AM, Alswat K, Almadi MA. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy system. Saudi J Gastroenterol. 2013;19:219-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Ford AC, Forman D, Bailey AG, Cook MB, Axon AT, Moayyedi P. Who consults with dyspepsia? Results from a longitudinal 10-yr follow-up study. Am J Gastroenterol. 2007;102:957-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Fisher RS, Parkman HP. Management of nonulcer dyspepsia. N Engl J Med. 1998;339:1376-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Spiller RC. ABC of the upper gastrointestinal tract: Anorexia, nausea, vomiting, and pain. BMJ. 2001;323:1354-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Naji SA, Brunt PW, Hagen S, Mowat NA, Russell IT, Sinclair TS, Tang TM. Improving the selection of patients for upper gastrointestinal endoscopy. Gut. 1993;34:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Valle PC, Breckan RK, Amin A, Kristiansen MG, Husebye E, Nordgård K, Mortensen L, Kildahl-Andersen OA, Wessel-Berg AM. “Test, score and scope”: a selection strategy for safe reduction of upper gastrointestinal endoscopies in young dyspeptic patients referred from primary care. Scand J Gastroenterol. 2006;41:161-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Value of the unaided clinical diagnosis in dyspeptic patients in primary care. Am J Gastroenterol. 2001;96:1417-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Hammer J, Eslick GD, Howell SC, Altiparmak E, Talley NJ. Diagnostic yield of alarm features in irritable bowel syndrome and functional dyspepsia. Gut. 2004;53:666-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 33. | Choomsri P, Bumpenboon W, Wasuthit Y, Euanorasetr C, Sumritpradit P, suwanthuma W, Lertsithichai P. Upper Gastrointestinal Endoscopy Findings in Patients Presenting with Dyspepsia. Thai J Surg. 2010;31:7-12. |
| 34. | Kapoor N, Bassi A, Sturgess R, Bodger K. Predictive value of alarm features in a rapid access upper gastrointestinal cancer service. Gut. 2005;54:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 35. | Wallace MB, Durkalski VL, Vaughan J, Palesch YY, Libby ED, Jowell PS, Nickl NJ, Schutz SM, Leung JW, Cotton PB. Age and alarm symptoms do not predict endoscopic findings among patients with dyspepsia: a multicentre database study. Gut. 2001;49:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 36. | Blackshaw GR, Barry JD, Edwards P, Allison MC, Lewis WG. Open-access gastroscopy is associated with improved outcomes in gastric cancer. Eur J Gastroenterol Hepatol. 2003;15:1333-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Bowrey DJ, Griffin SM, Wayman J, Karat D, Hayes N, Raimes SA. Use of alarm symptoms to select dyspeptics for endoscopy causes patients with curable esophagogastric cancer to be overlooked. Surg Endosc. 2006;20:1725-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | Delaney BC, Wilson S, Roalfe A, Roberts L, Redman V, Wearn A, Hobbs FD. Randomised controlled trial of Helicobacter pylori testing and endoscopy for dyspepsia in primary care. BMJ. 2001;322:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Talley NJ, Vakil N. Guidelines for the management of dyspepsia. Am J Gastroenterol. 2005;100:2324-2337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 276] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 40. | Manes G, Balzano A, Marone P, Lioniello M, Mosca S. Appropriateness and diagnostic yield of upper gastrointestinal endoscopy in an open-access endoscopy system: a prospective observational study based on the Maastricht guidelines. Aliment Pharmacol Ther. 2002;16:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | Arents NL, Thijs JC, van Zwet AA, Oudkerk Pool M, Gotz JM, van de Werf GT, Reenders K, Sluiter WJ, Kleibeuker JH. Approach to treatment of dyspepsia in primary care: a randomized trial comparing “test-and-treat” with prompt endoscopy. Arch Intern Med. 2003;163:1606-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Minoli G, Prada A, Gambetta G, Formenti A, Schalling R, Lai L, Pera A. The ASGE guidelines for the appropriate use of upper gastrointestinal endoscopy in an open access system. Gastrointest Endosc. 1995;42:387-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Spiegel BM, Farid M, van Oijen MG, Laine L, Howden CW, Esrailian E. Adherence to best practice guidelines in dyspepsia: a survey comparing dyspepsia experts, community gastroenterologists and primary-care providers. Aliment Pharmacol Ther. 2009;29:871-881. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Amornyotin S, Kita H, Redondo-Cerezo E S- Editor: Qi Y L- Editor: A E- Editor: Liu XM