Published online May 14, 2015. doi: 10.3748/wjg.v21.i18.5641
Peer-review started: November 15, 2014
First decision: December 26, 2014
Revised: January 15, 2015
Accepted: February 12, 2015
Article in press: February 13, 2015
Published online: May 14, 2015
Processing time: 186 Days and 2.8 Hours
AIM: To investigate the prevalence of erectile dysfunction (ED) and its association with depression in patients with chronic viral hepatitis.
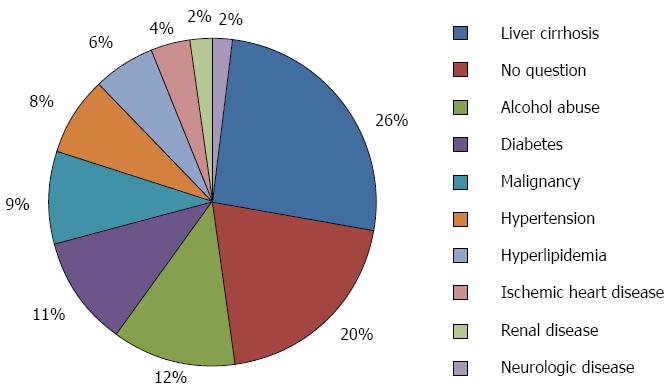
METHODS: This single center cross-sectional study was conducted from August 2013 through January 2014. All outpatients with chronic viral hepatitis in our liver clinic between 18 and 80 years of age were considered eligible for this study. The exclusion criteria included well-established causes of ED, such as diabetes, hypertension, hyperlipidemia, alcohol abuse, liver cirrhosis, ischemic heart disease, renal disease, neurologic disease, and malignancy. We also excluded the patients who had incompletely answered the questionnaires. ED was assessed using the validated Korean version of the International Index of Erectile Function (IIEF-5) scale. The Korean version of the self-administered Beck Depression Inventory (BDI) scale was used to assess depression in the patients. Demographic and medical data were obtained from the patients’ medical records. Current or past history of psychiatric diagnosis and drug history including the use of an antiviral agent and an antidepressant were also recorded.
RESULTS: A total of 727 patients met the initial eligibility criteria. Six hundred seventeen patients were excluded because their medical records contained one or more of the previously determined exclusion criteria. The remaining 110 patients were assessed based on the BDI and IIEF-5 questionnaires. Based on the IIEF-5 scale, the prevalence of ED among patients with chronic viral hepatitis was 40%. Compared with the non-ED group, patients in the ED group were older. The proportion of patients in the ED group who had a job or who were naïve peg-interferon users was lower than that in patients in the non-ED group. Patients with ED had significantly lower scores on the IIEF-5 scale than patients without ED (11.75 ± 4.88 vs 21.33 ± 1.86, P = 0.000). Patients with ED rated significantly higher scores on the BDI scale compared with patients without ED (12.59 ± 7.08 vs 5.30 ± 4.00, P = 0.000). Also, the IIEF-5 scores were negatively correlated with age, employment, and BDI scores. In the multiple logistic regression analysis, age and depression were independently associated with erectile dysfunction (P = 0.019 and 0.000, respectively).
CONCLUSION: Patients with chronic viral hepatitis have a high prevalence of ED. Age and depression are independent factors for ED in male patients with chronic viral hepatitis.
Core tip: The prevalence of erectile dysfunction among patients with chronic viral hepatitis is high. We assessed the prevalence of erectile dysfunction and its association with depression after excluding confounding factors. We confirmed that patients with chronic viral hepatitis have a high prevalence of erectile dysfunction, which is associated with depression.
- Citation: Ma BO, Shim SG, Yang HJ. Association of erectile dysfunction with depression in patients with chronic viral hepatitis. World J Gastroenterol 2015; 21(18): 5641-5646
- URL: https://www.wjgnet.com/1007-9327/full/v21/i18/5641.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i18.5641
Erectile dysfunction (ED) is defined as the inability to achieve or maintain an erection sufficient for satisfactory sexual performance[1]. The overall frequency of ED is reportedly 32% and 53.3% among male populations in the United States and South Korea, respectively[2,3]. Based on this high prevalence of ED, extensive investigations into the clinical and pathophysiologic mechanisms of sexual dysfunction have been carried out during the last decade[4-6]. However, ED in patients with chronic viral hepatitis has been investigated in few limited studies, which are often not comparable because they use different surveys and patient-sampling methodologies[7,8]. Moreover, few studies have evaluated the association between ED and depression in patients with chronic viral hepatitis. To date, none of the previous studies have investigated the relationship between ED and depression in patients with chronic viral liver disease.
The aim of this study was to evaluate the prevalence of ED in patients with chronic viral hepatitis. We also aimed to determine whether there is any correlation between ED and depression in patients with chronic viral hepatitis by using two questionnaires.
This was a single center cross-sectional study of outpatients with chronic viral hepatitis who were recruited between August 2013 and January 2014 at the Samsung Changwon Hospital, South Korea. All outpatients with chronic viral hepatitis between 18 and 80 years of age who were being treated in the liver clinic were considered eligible for this study. Many factors can cause ED. Therefore, in an effort to avoid confounding factors, we excluded patients suffering from diseases that might contribute, such as diabetes, hypertension, hyperlipidemia, alcohol abuse (including alcoholic liver disease), liver cirrhosis, ischemic heart disease, renal disease, neurologic disease, and malignancy (including hepatocellular carcinoma)[9-13]. We also excluded the patients who had answered the two questionnaires incompletely.
Erectile function was assessed using the validated Korean five-item version of the International Index of Erectile Function-5 (IIEF-5). The IIEF-5 includes five items from the IIEF, and it has favorable properties for detecting the presence and severity of ED[14]. The Korean version of the IIEF-5 has also been proven to be valid and reliable[15]. It consists of four items focusing on erectile function, and one item focusing on intercourse satisfaction. All items were rated on a five-point scale. IIEF-5 scores are obtained by calculating the sum of the item responses, with 1 being the worst possible score and 25 being the best score. ED is usually diagnosed below a score of 21 points. However, Ahn et al[15] reported the most appropriate cutoff score between ED and no ED was 17 for Korean patients (sensitivity = 91.3%, specificity = 86.3%) and ED is classified as follows: 5-9, severe ED; 10-13, moderate ED; 14-17, mild ED; and 18-25, no ED.
The Korean version of the self-administered Beck Depression Inventory (K-BDI) was used to evaluate the patients’ subjective depressive mood. Its use to assess depressive mood has been validated[16,17]. The BDI consists of 21 items, each of which is rated from 0 to 3. BDI scores range from 0 to 63. The categories of depression are usually defined as follows: < 10, normal; 10-15, mild; and ≥ 16, moderate to severe[18]. Therefore, in this study, the subjects were considered as having depression when the K-BDI score exceeded 10 points.
The following data were retrospectively collected from the medical records of the patients: age, smoking status, alcohol use, employment, health insurance, religion, habitation, presence of viral hepatitis, diabetes, hypertension, hyperlipidemia, cardiovascular disease, body weight, and height. A history of any psychiatric diagnosis, such as major depressive disorder and anxiety/panic disorders was recorded. A drug history including use of antiviral agents and antidepressants was also recorded. Body mass index (BMI) was calculated as kg/m2.
Continuous variables are presented as mean ± SD. Differences in independent variables were analyzed by Student’s t and by Pearson’s χ2 tests for categorical variables. Spearman’s single regression analysis was used to determine the relationships between variables. Multivariate analysis using logistic regression was performed to evaluate the association of ED and other parameters. P < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, United States).
This cross sectional study initially included 727 patients who met the eligibility criteria. We excluded 617 patients according to the previously determined exclusion criteria (Figure 1). The remaining 110 patients were assessed based on the self-administered BDI and IIEF-5 questionnaires.
Descriptive data are presented in Table 1. The mean age of the patients was 47.17 ± 10.98 years. Using the IIEF-5 scale, the prevalence of ED (IIEF-5 score ≤ 17) was found to be 40%. There was no significant difference between the ED group and the non-ED group in viral etiology, smoking, BMI, health insurance, religion, or habitation. Compared with the non-ED group, patients in the ED group were significantly older (P = 0.001). The proportion of patients in the ED group who had a job or who were naïve peg-interferon users was lower than that in patients in the non-ED group (both P < 0.05).
| Characteristic | Non-ED | ED | P value |
| (n = 66) | (n = 44) | ||
| Age, yr | 44.38 ± 8.90 | 51.36 ± 12.48 | 0.001 |
| Viral etiology | |||
| HBV | 52 (78.8) | 29 (65.9) | 0.1331 |
| HCV | 14 (21.2) | 15 (34.1) | 0.1331 |
| Smoking | 27 (40.9) | 18 (40.9) | 1.000 |
| BMI, kg/m2 | 23.93 ± 2.63 | 24.03 ± 3.16 | 0.859 |
| Employment | 64 (97.0) | 35 (79.5) | 0.003 |
| Health insurance2 | 1 (1.5) | 1 (2.3) | 0.771 |
| Religion, yes | 18 (27.3) | 19 (43.2) | 0.084 |
| Habitation, rural | 11 (16.7) | 11 (25.0) | 0.284 |
| Peg-interferon, yes | 6 (9.1) | 11 (25.0) | 0.024 |
Patients with ED had significantly lower scores on the IIEF-5 scale than the patients without ED (11.75 ± 4.88 vs 21.33 ± 1.86, P = 0.000). Patients with ED reported significantly higher scores on the K-BDI scale compared with patients without ED (12.59 ± 7.08 vs 5.30 ± 4.00, P = 0.000).
The correlations between IIEF-5 scores and the patients’ characteristics are displayed in Table 2. IIEF-5 scores were negatively correlated with age, employment, and K-BDI score (all P = 0.000). In the multiple logistic regression analysis, age and depression were independent factors associated with ED after adjustment for BMI, smoking, employment, health insurance, religion, habitation, viral etiology, and use of peg-interferon (both P < 0.05) (Table 3).
| Characteristic | IIEF-5 scores | |
| ρ | P value | |
| Age | -0.359 | 0.000 |
| Viral etiology (HBV) | -0.148 | 0.123 |
| Smoking | -0.021 | 0.825 |
| BMI | 0.089 | 0.356 |
| Employment | -0.338 | 0.000 |
| Health insurance | -0.013 | 0.894 |
| Religion | 0.165 | 0.085 |
| Habitation | 0.132 | 0.169 |
| Peg-interferon | 0.185 | 0.053 |
| K-BDI scores | -0.563 | 0.000 |
| Factor | Erectile dysfunction | |||
| β | SE | Exp(B) | P value | |
| Age | 0.064 | 0.027 | 1.066 | 0.019 |
| Depression | 2.511 | 0.544 | 12.322 | 0 |
The reported prevalence of ED in patients with chronic viral hepatitis ranges from 14% to 78%[7,8,19]. We found that 40% of the patients with chronic viral hepatitis have ED, based on the IIEF-5 scores ≤ 17. This prevalence is lower than that observed in the general Korean population (53.3%)[3]. However, the actual difference in prevalence between patients with ED and general populations may change, because we excluded confounding factors that might contribute to ED. We found that age and depression were independently associated with ED in patients with chronic viral hepatitis.
There are some explanations for the high prevalence of ED in patients with chronic viral hepatitis. One explanation involves an inflammatory-based pathway. Several complex mechanisms of HCV and other mediators of viral hepatitis that lead to inflammation, increased oxidative stress, insulin resistance, and apoptosis may be associated with the development of ED[8,20,21]. Chronic systemic inflammation accompanied by increased C-reactive protein levels decreases nitric oxide synthesis in endothelial cells, ultimately leading to endothelial dysfunction, which may account for the association between ED and hepatitis-related liver disease[8,22,23].
Various conditions are associated with ED[19]. Besides strict exclusion of these conditions, we additionally analyzed other demographic conditions. In our study, age, employment, and K-BDI scores were significantly associated with ED. However, only age was correlated with ED in the logistic regression analysis. This finding is consistent with the other previously reported results[8,19]. Interestingly, Chung et al[8] reported that in the oldest age group (> 69 years), no significant difference was observed in the frequency of prior hepatitis diagnosis between ED patients and controls. They explained that these elderly men suffered from ED due to age-related factors, which are unrelated to hepatitis, such as lower testosterone level and higher peripheral vascular resistance. Three men belonging to the oldest group were included in our study. Two had both ED and depression, and one had ED without depression. Further studies assessing the correlation between ED and depression in the oldest age group are recommended.
Depression is associated with impairments of sexual function and satisfaction[24,25]. However, whether depression has a direct influence on ED is debatable[26,27]. Although the prevalence of depression is high in patients with chronic viral hepatitis[28,29], little is known about the association between depression and ED. In this study, depression had an independent negative impact on ED in patients with chronic viral hepatitis.
ED is associated with substantially broader aspects of a man’s life than just erectile functioning[30]. It is significantly associated with a poor sexual relationship and sexual satisfaction, diminished confidence, and low self-esteem[30]. Our study reveals that depression is associated with ED. Therefore, depression may contribute to poor outcomes in patients with chronic viral hepatitis. Although the impact of depression on adverse outcomes, such as deteriorating liver function and poor survival in patients with chronic viral hepatitis, was not examined in this study, our results suggest that it is important to develop systematic approaches to screen these patients for depression, and to plan proper treatment strategies for these patients.
There are some limitations to our study. First, the number of study participants was relatively small, therefore, the results cannot be generalized. Second, it is considered shameful to admit to the existence of ED; hence the number of patients suffering from ED could have been underestimated. In our study, 20% of the initially enrolled patients refused to answer the questionnaire. After excluding these non-responders, we categorized the participants into an ED group and non-ED group to minimize bias. Third, our study did not provide information on a causal relationship between ED and depression, due to the cross-sectional design of the study. Therefore, further large-scale randomized clinical trials are required to determine whether screening and therapeutic interventions can prevent and control ED, improve depression, and positively affect the clinical outcomes of patients with chronic viral hepatitis. Finally, several factors that we did not exclude can act as confounders and may have introduced bias.
In conclusion, patients with chronic viral hepatitis have a high prevalence of ED, which is associated with depression. In patients with chronic viral hepatitis, detection of depression and active interventions should be considered for proper management of ED.
We thank all the outpatients in our liver clinic who contributed data to the databases used in this study. We also acknowledge the technical assistance provided by Gun Woong Na. This work is supported by Samsung Biomedical Institute grant.
Erectile dysfunction (ED) is associated with substantially broader aspects of a man’s life. But ED in patients with chronic viral hepatitis has been investigated in few and limited studies. Moreover few studies have evaluated the association of ED and depression in patients with chronic viral hepatitis.
The authors evaluated the prevalence of ED and the relationships between ED and depression in patients with chronic viral hepatitis.
To minimize the effect of confounding factors that might influence ED, the authors set various conditions as exclusion criteria.
The study suggests that patients with chronic viral hepatitis have a high prevalence of ED, which is associated with depression.
ED is defined as the inability to achieve or maintain an erection sufficient for satisfactory sexual performance.
This manuscript is a good cross-sectional study in which authors evaluated the prevalence of ED and the association with depression in patients with chronic viral hepatitis. The results are interesting. The authors emphasize that detection of depression and active interventions should be considered to properly manage ED in patients with chronic viral hepatitis.
| 1. | NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1292] [Cited by in RCA: 1317] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 2. | Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007;120:151-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 480] [Cited by in RCA: 528] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 3. | Lee JY, Moon KH, Park TC. The assessment of sexual function in men who visited health screening center: a study using the Korean version of IIEF (International Index of Erectile Dysfunction) questionnaire. Korean J Urol. 2001;42:334-340. |
| 4. | Montague DK, Jarow JP, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, Milbank AJ, Nehra A, Sharlip ID. Chapter 1: The management of erectile dysfunction: an AUA update. J Urol. 2005;174:230-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 181] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Costa IC, Carvalho HN, Pacheco-Figueiredo L, Tomada I, Tomada N. Hormonal modulation in aging patients with erectile dysfunction and metabolic syndrome. Int J Endocrinol. 2013;2013:107869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Carvalheira A, Forjaz V, Pereira NM. Adherence to phosphdiesterase type 5 inhibitors in the treatment of erectile dysfunction in long-term users: how do men use the inhibitors? Sex Med. 2014;2:96-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Simsek I, Aslan G, Akarsu M, Koseoglu H, Esen A. Assessment of sexual functions in patients with chronic liver disease. Int J Impot Res. 2005;17:343-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 8. | Chung SD, Keller JJ, Liang YC, Lin HC. Association between viral hepatitis and erectile dysfunction: a population-based case-control analysis. J Sex Med. 2012;9:1295-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Celik O, Ipekci T, Akarken I, Ekin G, Koksal T. To evaluate the etiology of erectile dysfunction: What should we know currently? Arch Ital Urol Androl. 2014;86:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Viigimaa M, Vlachopoulos C, Lazaridis A, Doumas M. Management of erectile dysfunction in hypertension: Tips and tricks. World J Cardiol. 2014;6:908-915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Hatzimouratidis K, Hatzichristou D. How to treat erectile dysfunction in men with diabetes: from pathophysiology to treatment. Curr Diab Rep. 2014;14:545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Pauker-Sharon Y, Arbel Y, Finkelstein A, Halkin A, Herz I, Banai S, Justo D. Cardiovascular risk factors in men with ischemic heart disease and erectile dysfunction. Urology. 2013;82:377-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Chung SD, Chen YK, Kang JH, Keller JJ, Huang CC, Lin HC. Population-based estimates of medical comorbidities in erectile dysfunction in a Taiwanese population. J Sex Med. 2011;8:3316-3324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 14. | Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319-326. [PubMed] |
| 15. | Ahn TY, Lee DS, Kang WC, Hong JH, Kim YS. Validation of an abridged Korean version of the Interanational Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Korean J Urol. 2001;42:535-539. |
| 16. | Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23191] [Cited by in RCA: 23689] [Article Influence: 846.0] [Reference Citation Analysis (0)] |
| 17. | Rhee MK, Chung YC, Lee YH, Park SH, Sohn CH, Homg SK, Lee BK, Chang PL, Yoon AR. A standardization study of Beck Depression Inventory 1 - Korean version (K-BDI) : Reliability and factor analysis. Kor J Psychopathol. 1995;4:77-95. |
| 18. | Williams J. The psychological treatment of depression. A guide to the theory and practice of cognitive-behavioral therapy. 1984;. |
| 19. | Toda K, Miwa Y, Kuriyama S, Fukushima H, Shiraki M, Murakami N, Shimazaki M, Ito Y, Nakamura T, Sugihara J. Erectile dysfunction in patients with chronic viral liver disease: its relevance to protein malnutrition. J Gastroenterol. 2005;40:894-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Chen S, Wu R, Huang Y, Zheng F, Ou Y, Tu X, Zhang Y, Gao Y, Chen X, Zheng T. Insulin resistance is an independent determinate of ED in young adult men. PLoS One. 2013;8:e83951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Tomada N, Tomada I, Botelho F, Pacheco-Figueiredo L, Lopes T, Negrão R, Pestana M, Cruz F. Endothelial function in patients with metabolic syndrome and erectile dysfunction: a question of angiopoietin imbalance? Andrology. 2013;1:541-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Reriani M, Flammer AJ, Li J, Prasad M, Rihal C, Prasad A, Lennon R, Lerman LO, Lerman A. Microvascular endothelial dysfunction predicts the development of erectile dysfunction in men with coronary atherosclerosis without critical stenoses. Coron Artery Dis. 2014;25:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Huang SS, Lin CH, Chan CH, Loh el-W, Lan TH. Newly diagnosed major depressive disorder and the risk of erectile dysfunction: a population-based cohort study in Taiwan. Psychiatry Res. 2013;210:601-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Baldwin DS. Depression and sexual dysfunction. Br Med Bull. 2001;57:81-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 131] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | McCabe MP, Connaughton C. Psychosocial factors associated with male sexual difficulties. J Sex Res. 2014;51:31-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Mallis D, Moysidis K, Nakopoulou E, Papaharitou S, Hatzimouratidis K, Hatzichristou D. Psychiatric morbidity is frequently undetected in patients with erectile dysfunction. J Urol. 2005;174:1913-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Kantor J, Bilker WB, Glasser DB, Margolis DJ. Prevalence of erectile dysfunction and active depression: an analytic cross-sectional study of general medical patients. Am J Epidemiol. 2002;156:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Fábregas BC, de Ávila RE, Faria MN, Moura AS, Carmo RA, Teixeira AL. Health related quality of life among patients with chronic hepatitis C: a cross-sectional study of sociodemographic, psychopathological and psychiatric determinants. Braz J Infect Dis. 2013;17:633-639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Keskin G, Gümüs AB, Orgun F. Quality of life, depression, and anxiety among hepatitis B patients. Gastroenterol Nurs. 2013;36:346-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 30. | McCabe MP, Althof SE. A systematic review of the psychosocial outcomes associated with erectile dysfunction: does the impact of erectile dysfunction extend beyond a man’s inability to have sex? J Sex Med. 2014;11:347-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Xiong G S- Editor: Yu J L- Editor: AmEditor E- Editor: Ma S