Published online May 7, 2015. doi: 10.3748/wjg.v21.i17.5427
Peer-review started: October 18, 2014
First decision: November 14, 2014
Revised: December 1, 2014
Accepted: January 16, 2015
Article in press: January 16, 2015
Published online: May 7, 2015
Processing time: 209 Days and 7.3 Hours
Primary retroperitoneal mucinous cystic tumors are extremely rare. These tumors can be classified as a primary retroperitoneal mucinous cystadenoma with or without borderline malignancy or primary retroperitoneal mucinous cystadenocarcinoma. The most common of these is primary retroperitoneal mucinous cystadenoma, which almost always occurs in female patients; only ten cases have been reported in males. The most common clinical findings for this tumor type include nonspecific abdominal pain and a palpable abdominal mass. A definitive diagnosis is usually obtained from histopathology after surgical excision. Here, we report the case of a 60-year-old female patient who complained of abdominal pain that had been present for 3 mo and presented with a palpable abdominal mass. Multidetector computed tomography scanning revealed a large, unilocular cystic mass in the left retroperitoneal space. Surgical intervention was performed and the tumor was completely removed. Histopathologic examination confirmed that the tumor was a primary retroperitoneal mucinous cystadenoma. Two years after surgery, the patient remains disease free.
Core tip: Primary retroperitoneal mucinous cystadenomas are very rare tumors for which the biologic behavior and histogenesis remain speculative. No effective diagnostic measures have been established for an accurate preoperative diagnosis of these tumors. Symptoms of these retroperitoneal masses are caused by exertion of pressure and obstructive effects on adjacent organs. This report describes a case of a large, primary retroperitoneal mucinous cystadenoma in a female patient, which was visualized on multidetector computed tomography exam and completely enucleated at laparotomy.
- Citation: Knezevic S, Ignjatovic I, Lukic S, Matic S, Dugalic V, Knezevic D, Micev M, Dragasevic S. Primary retroperitoneal mucinous cystadenoma: A case report. World J Gastroenterol 2015; 21(17): 5427-5431
- URL: https://www.wjgnet.com/1007-9327/full/v21/i17/5427.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i17.5427
Primary retroperitoneal mucinous (PRM) cystic tumors can be classified as PRM cystadenoma, PRM cystadenoma with borderline malignancy, and PRM cystadenocarcinoma. First described by Handfield[1] in 1924, PRM cystadenomas are the most common of these tumor types[2-4]. Because of its rarity, the biologic behavior and histogenesis of this disease remain unclear[5]. A review of EMBASE and MEDLINE databases revealed 48 reported cases of PRM cystadenoma[2-4,6], ten cases with borderline malignancy[6,7], and 27 cases of PRM cystadenocarcinoma[6,8,9] in the English literature. These tumors almost always occur in female patients, with only ten cases reported in males[2-4,6-12].
Tumors range between 7 cm and 30 cm in size[4], and most commonly present with nonspecific abdominal pain or distension and a palpable abdominal mass, which induces mass effect on adjacent organs. Acute abdomen pain due to intestinal obstruction caused by PRM cystadenoma has also been reported[5]. PRM cystadenomas are typically discovered with standard imaging modalities [computed tomography (CT), magnetic resonance imaging (MRI), ultrasound]. However, laboratory and imaging findings are inconclusive in the majority of cases, and definitive diagnosis is obtained only after histologic examination. In this report, we describe a case of a large PRM cystadenoma in a female patient, which was visualized on multidetector CT exam and completely enucleated at laparotomy.
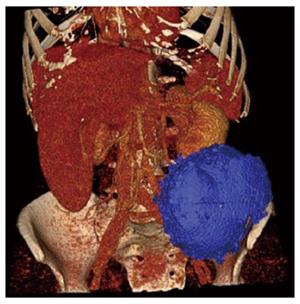
A 60-year-old female patient was admitted to our hospital because of abdominal pain and a palpable mass in the left lower abdominal quadrant. The symptoms had been present for 3 mo. Laboratory findings and tumor markers were within reference ranges. Multidetector CT (MDCT) scanning revealed a large (12.3 cm × 10.8 cm) cystic mass in the left hemiabdomen located within the retroperitoneal space (Figure 1). Volume rendering and three-dimensional reconstruction of the MDCT showed an oval, well-delimited, cystic lesion located in the left retroperitoneal space and embedded in the left iliac fossa, but without infiltration of surrounding structures (Figure 2). The differential diagnosis included a mesenterial pseudocyst and cyst of the left ovary.
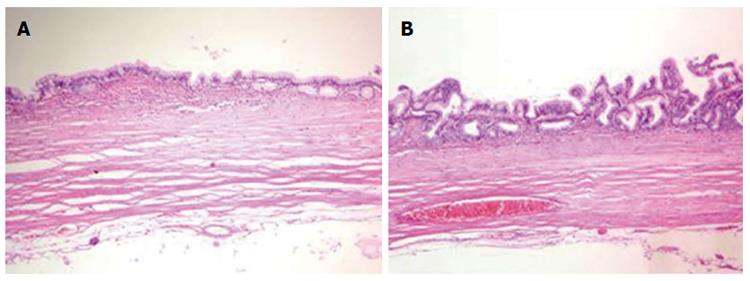
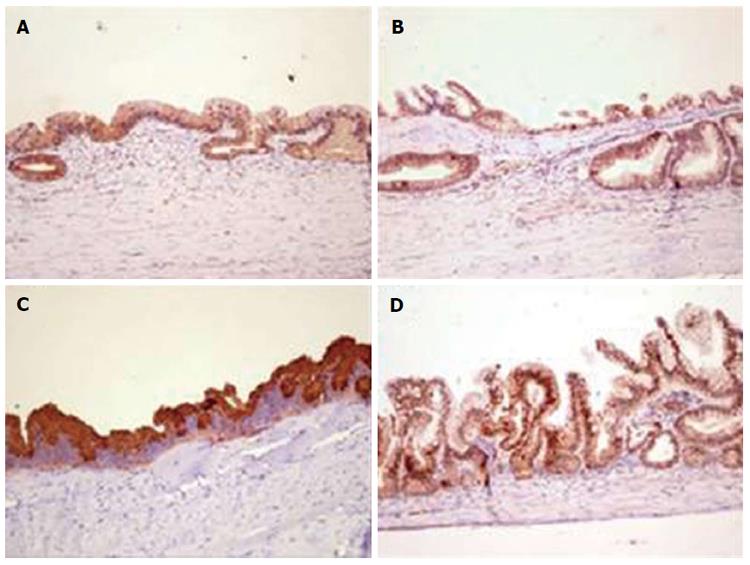
A midline laparotomy was performed, revealing the mass located between the left portion of the anterior abdominal wall and the lateral border of the left psoas muscle, embedded in the left iliac fossa. The cystic tumor was completely removed (Figure 3) and sent for histopathologic assessment. Hematoxylin and eosin staining revealed a single layer of mucin (MUC)-producing columnar epithelium with underlying fibrous connective tissue and rare papillation, but without invasion (Figure 4). Immunohistochemistry for MUC identified unevenly distributed moderate cytoplasmic expression of MUC1 and MUC2, and strong cytoplasmic expression of MUC5AC (Figure 5). Strong nuclear CDX2 immunoreactivity was also observed. Therefore, a diagnosis of PRM cystadenoma was confirmed.
The postoperative period was uneventful and the patient was discharged on the fifth postoperative day. Regular check-ups demonstrated that the patient was completely symptom free. Two years after surgery, abdominal CT revealed no signs of disease recurrence.
There are several theories explaining the development of PRM cystademonas, including origination from a teratoma, ectopic ovary, or mucinous metaplasia of the mesothelial lining. Subramony et al[13] found that stromal cells in PRM cystademonas express the estrogen receptor, which may be why these tumors are more frequently found in women. Also, the growth of the tumor could be a consequence of estrogen activity via estrogen receptor activation. In men, the undescended testicle is a potential source of tumor cells, as the retroperitoneum has no epithelial cells[9].
There are no pathognomonic clinical or radiologic findings for this disease, thus obtaining an accurate preoperative diagnosis with standard imaging modalities is nearly impossible. PRM cystadenomas usually present as a multi- or unilocular cystic mass, varying in size and localized anywhere in the retroperitoneal space, without adherence to the ovaries. Imaging findings often include displacement of the ureter, kidney, liver, and large abdominal vessels. The diagnostic value of MRI and CT is similar; MRI provides a variety of images and can identify correlations between the mass and the soft tissues[8], whereas CT reveals the extension of the mass and shows mural calcifications, which support the diagnosis of cystadenoma rather than teratoma.
Differential diagnoses should include cystic teratoma, cystic mesothelioma, Müllerian cyst, epidermoid cyst, pancreatic pseudocyst, lymphocele, and urinoma. Aspiration and cytology examination cannot reveal the type of lining cells of these cystic tumors[7]. In our case, a retroperitoneal enteric duplication cyst was suspected after standard histopathologic analysis. The diagnosis of PRM cystadenoma was subsequently confirmed by immunohistochemical analysis.
Laparotomy with complete surgical excision of the tumor has been the therapy of choice in most reported cases, as well as it was in our case; although, a laparoscopic approach can also be successfully performed[14]. When diagnosed, complete surgical enucleation of the tumor is always advised, due to complications such as compression effect on adjacent organs, infection, and rupture or malignant transformation of the tumor. Therefore, when a retroperitoneal cystic mass is encountered, mucinous cystadenoma should be taken into consideration. The small number of globally registered cases and insufficient surveillance data show that there is a need for effective registration and further study of these rare tumors.
A 60-year-old female patient presented with severe abdominal pain.
A palpable mass in the left lower abdominal quadrant, with no palpable lymphadenopathy or hepatosplenomegaly.
Mesenterial pseudocyst; cyst of the left ovary.
Laboratory findings and tumor markers were within reference ranges.
Multidetector computed tomography (CT) scan revealed a large (12.3 cm × 10.8 cm) cystic mass in the left hemiabdomen within the retroperitoneal space.
Histopathologic analysis disclosed mainly a single layer of mucin (MUC)-producing columnar epithelium with underlying fibrous connective tissue and rare papillation, but without invasion. Immunohistochemistry identified unevenly distributed, moderate, cytoplasmic MUC1 and MUC2 staining, strong cytoplasmic MUC5AC staining, and strong nuclear CDX2 antigen staining.
Laparotomy with complete surgical excision of the tumor.
Primary retroperitoneal mucinous tumors are rare. Primary retroperitoneal mucinous cystadenomas are the most common type of these tumors that can arise at any location in the retroperitoneum, with histologic similarities to ovarian mucinous cystadenomas.
This report describes a female patient with abdominal pain and a palpable mass in the left lower abdominal quadrant. Laboratory findings were within reference ranges, and a large cystic mass was observed in the left hemiabdomen within the retroperitoneal space upon multidetector CT scanning. The tumor was diagnosed as a primary retroperitoneal mucinous cystadenomas upon histopathologic examination.
This article applies laparotomy and the complete resection of the tumor, with pathologic and valuable immunohistochemistry reports to confirm the final diagnosis of primary retroperitoneal mucinous cystadenoma.
| 1. | Handfield JR. Retroperitoneal cysts: their pathology, diagnosis and treatment. Br J Surg. 1924;12:119-134. [RCA] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Mattei J, Kim FJ, Phillips J, Zhelnin KE, Said S, Sehrt D, Molina WR. Male primary retroperitoneal mucinous cystadenoma. Urology. 2013;82:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Prabhuraj AR, Basu A, Sistla SC, Jagdish S, Jayanthi S. Primary retroperitoneal mucinous cystadenoma in a man. Am J Clin Oncol. 2008;31:519-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Yan SL, Lin H, Kuo CL, Wu HS, Huang MH, Lee YT. Primary retroperitoneal mucinous cystadenoma: Report of a case and review of the literature. World J Gastroenterol. 2008;14:5769-5772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | de León DC, Pérez-Montiel D, Chanona-Vilchis J, Dueñas-González A, Villavicencio-Valencia V, Zavala-Casas G. Primary retroperitoneal mucinous cystadenocarcinoma: report of two cases. World J Surg Oncol. 2007;5:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Bakker RF, Stoot JH, Blok P, Merkus JW. Primary retroperitoneal mucinous cystadenoma with sarcoma-like mural nodule: a case report and review of the literature. Virchows Arch. 2007;451:853-857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Falidas E, Konstandoudakis S, Vlachos K, Archontovasilis F, Mathioulakis S, Boutzouvis S, Villias C. Primary retroperitoneal mucinous cystadenoma of borderline malignancy in a male patient. Case report and review of the literature. World J Surg Oncol. 2011;9:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Hrora A, Reggoug S, Jallal H, Sabbah F, Benamer A, Alaoui M, Raiss M, Ahallat M. Primary retroperitoneal mucinous cystadenocarcinoma in a male patient: a case report. Cases J. 2009;2:7196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Thamboo TP, Sim R, Tan SY, Yap WM. Primary retroperitoneal mucinous cystadenocarcinoma in a male patient. J Clin Pathol. 2006;59:655-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Lai KKT, Chan YYR, Chin ACW, Ng WF, Huang YHH, Mak YLM, Wong WC. Primary retroperitoneal mucinous cystadenoma in a 52-year-old man. J H K Coll Radiol. 2004;7:223-225. |
| 11. | Motoyama T, Chida T, Fujiwara T, Watanabe H. Mucinous cystic tumor of the retroperitoneum. A report of two cases. Acta Cytol. 1994;38:261-266. [PubMed] |
| 12. | Benkirane A, Mikou A, Jahid A, Zouaidia F, Laraqui L, Bernoussi Z, Mahassini N. Primary retroperitoneal mucinous cystadenoma with borderline malignancy in a male patient: a case report. Cases J. 2009;2:9098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Subramony C, Habibpour S, Hashimoto LA. Retroperitoneal mucinous cystadenoma. Arch Pathol Lab Med. 2001;125:691-694. [PubMed] |
| 14. | Chen JS, Lee WJ, Chang YJ, Wu MZ, Chiu KM. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma: report of a case. Surg Today. 1998;28:343-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Caracappa D, Demetrashvili Z S- Editor: Yu J L- Editor: A E- Editor: Zhang DN