Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3150
Peer-review started: July 20, 2014
First decision: August 15, 2014
Revised: September 14, 2014
Accepted: October 14, 2014
Article in press: October 15, 2014
Published online: March 14, 2015
Processing time: 239 Days and 18.1 Hours
Familial adenomatous polyposis (FAP) or Gardner’s syndrome is often accompanied by adenomas of the stomach and duodenum. We experienced a case of adenomas of the common bile duct in a 40-year-old woman with FAP presenting with acute cholangitis. Only 8 cases of adenomas or adenocarcinoma of the common bile duct have been reported in the literature in patients with FAP or Gardner’s syndrome. Those patients presented with acute cholangitis or pancreatitis. Local excision or Whipple procedure may be the reasonable surgical option.
Core tip: Adenomas or adenocarcinoma in familial adenomatous polyposis (FAP) and Gardner’s syndrome are less frequently in the common bile duct (CBD). We report a case of FAP associated with CBD adenomas presenting with symptoms of acute cholangitis and cured after a radical Whipple procedure.
- Citation: Yan ML, Pan JY, Bai YN, Lai ZD, Chen Z, Wang YD. Adenomas of the common bile duct in familial adenomatous polyposis. World J Gastroenterol 2015; 21(10): 3150-3153
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/3150.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.3150
Adenomas or adenocarcinomas in familial adenomatous polyposis (FAP) and Gardner’s syndrome (GS) are often found frequently in the colon and rectum, and less frequently in the ampulla of Vater[1-3], stomach[4-6] and duodenum[7-10]. There are a few reports[11-15] of patients with FAP or GS who have developed pancreatitis or acute cholangitis caused by adenomas of the common bile duct (CBD). Here, we report a case of acute cholangitis due to adenomas of the CBD in a patient with FAP, accompanied by adenomatous changes in the stomach, duodenum and the ampulla of Vater.
A 40-year-old woman was admitted to our hospital in July 2013 for fever and abdominal pain. Eleven months ago, she underwent laparoscopic cholecystectomy, CBD exploration and mass resection with T-tube drainage at the local hospital for acute cholangitis. Multiple polypoid lesions were seen in the distal CBD. Pathological analysis showed adenomas with mild to moderate dysplasia. She underwent adenoma resection through the T-tube in the CBD 8 mo ago, and pathology showed villous adenomas with moderate to severe dysplasia. Three days ago, she felt painful in the right upper quadrant with temperature up to 39.5 °C and symptomatic treatment was given at the local hospital.
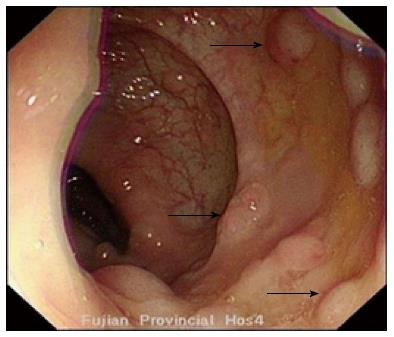
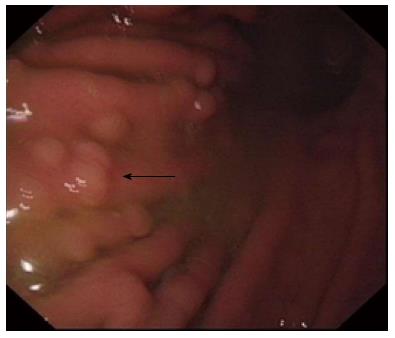
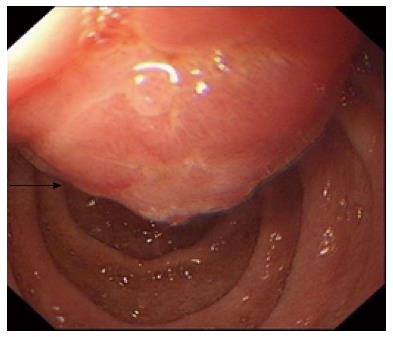
On admission, her liver function tests showed that total bilirubin was 1.0 mg/dL, serum amylase 145 IU/L, ALT 168 U/L, AST 88 U/L, GGT 858 U/L, and alkaline phosphatase 520 U/L. Magnetic resonance cholangiopancreatography revealed numerous masses in the CBD and the greatest diameter of the CBD was up to 1.7 cm (Figure 1). Her mother, younger brother and one of three sisters had FAP. Colonoscopy revealed villous polyps in the colon with the diameter from 0.3 to 2.5 cm (Figure 2). Duodenoscopy showed multiple polyps in the duodenum and the distal stomach (Figure 3). The ampulla of Vater was apparently protuberant and the surface was rough (Figure 4). The polyps were adenomas with low-grade intraepithelial neoplasia. Capsule endoscopy found no abnormality in the small intestine.
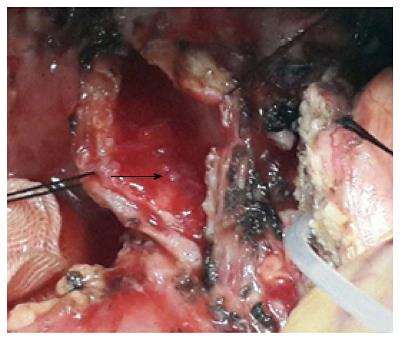
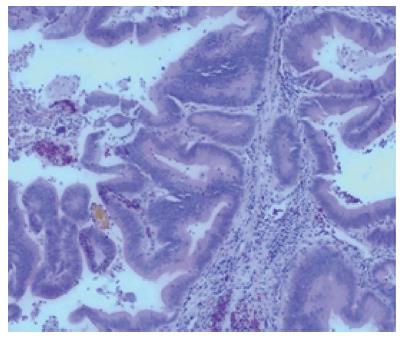
On July 29, a radical Whipple procedure was performed. After the operation, we found a 5 cm × 4 cm mass in the ampulla of Vater, and multiple polyps in the descendant duodenum and distal stomach with the largest diameter from 0.1 to 0.7 cm. Numerous polyps filled the middle and distal CBD, and the greatest diameter of polyps was about 1.2 cm (Figure 5). Microscopic examination of the ampullary and distal CBD polypoid lesions showed adenomas with high-grade intraepithelial neoplasia (Figure 6). She had an uneventful postoperative recovery. Seven months later, she underwent subtotal colectomy with ileosigmoid anastomosis. There were hundreds of polyps in the colon which turned out to be tubular adenomas pathologically.
There are a few reports of patients with FAP or GS who presented with abdominal pain, acute cholangitis or pancreatitis because of adenomas[12,15] or carcinoma[11,13,14] of the CBD. Previous cases[11-15] in the literature with FAP associated with adenomas in the CBD are summarized in Table 1.
| Ref. | Sex | Age | Presentation | Site of obstruction | Treatment | Pathology |
| Lees et al[11] | M | 22 | Jaundice | Distal CBD | T-tube drainage | Adenocarcinoma |
| F | 40 | Jaundice, pruritus, bifurcation | Hepatic duct, radiation | T-tube drainage | Adenocarcinoma | |
| Järvinen et al[12] | M | 58 | Jaundice with pain | CBD, left hepatic duct | T-tube drainage | Adenocarcinoma |
| F | 27 | Choledochoscopy | Distal CBD | Whipple | Adenoma | |
| Komorowski et al[13] | F | 56 | Abdominal pain | Distal CBD | Whipple | Carcinoma in situ |
| Spigelman et al[14] | M | 78 | Weight loss, abdominal pain | Extrahepatic duct | Not described | Adenocarcinoma |
| Futami et al[15] | F | 40 | Acute pancreatitis | Inferior CBD | Sphincterotomy | Adenoma |
| Present case | F | 40 | Acute cholangitis | Distal CBD | Whipple | Adenoma |
Treatments for adenomas of FAP in the CBD include local excision and radical resection. Local excision is recommended for benign lesions of the inferior CBD[16], but its major problem is high risk of recurrence[3]. Therefore, complete resection of adenomas will not only improve the symptomatology but also prevent the development of carcinoma. Surgical resection is necessary when adenomas have malignant potential or when there are complications[2,7,17]. The present patient had many adenomas in the stomach, duodenum and CBD, and the Whipple procedure is the best choice for her. The Whipple procedure for advanced duodenal and ampullary adenomatosis in FAP is a safe and efficient therapeutic option[2,7]. For the patients in whom complete resection is possible, the long-term prognosis can be good.
It is worth mentioning that our patient firstly presented with biliary obstruction rather than those adenomas in the colon and rectum. We recommend that the patients with FAP or GS undergo endoscopic surveillance of the upper gastrointestinal tract and ultrasonography of the hepatobiliary system, especially those patients with elevated liver enzyme.
A case of familial adenomatous polyposis (FAP) with adenomas of the common bile duct (CBD) presented with acute cholangitis.
The patient was initially admitted for acute cholangitis.
Liver function tests showed that the total bilirubin was 1.0 mg/dL, serum amylase 145 IU/L, ALT 168 U/L, AST 88 U/L, GGT 858 U/L, and alkaline phosphatase 520 U/L.
Preoperative magnetic resonance cholangiopancreatography indicated numerous masses in the CBD and the greatest diameter of the CBD was up to 1.7 cm.
Microscopic examination of the ampullary and distal CBD polypoid lesions indicated adenomas with high-grade intraepithelial neoplasia.
A radical Whipple procedure was performed.
Only 2 cases of adenomas of the common bile duct have been reported in the literature in patients with FAP or Gardner’s syndrome.
The patient firstly presented with biliary obstruction rather than those adenomas in the colon and rectum. The authors recommend that the patients with FAP or Gardner’s syndrome undergo endoscopic surveillance of the upper gastrointestinal tract and ultrasonography of the hepatobiliary system, especially those patients with elevated liver enzyme.
The contents are interesting, but there is the part that does not make the appearance of the article. There is the need to correct.
| 1. | Laleman W, Verreth A, Topal B, Aerts R, Komuta M, Roskams T, Van der Merwe S, Cassiman D, Nevens F, Verslype C. Endoscopic resection of ampullary lesions: a single-center 8-year retrospective cohort study of 91 patients with long-term follow-up. Surg Endosc. 2013;27:3865-3876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Skipworth JR, Morkane C, Raptis DA, Vyas S, Olde Damink SW, Imber CJ, Pereira SP, Malago M, West N, Phillips RK. Pancreaticoduodenectomy for advanced duodenal and ampullary adenomatosis in familial adenomatous polyposis. HPB (Oxford). 2011;13:342-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Ma T, Jang EJ, Zukerberg LR, Odze R, Gala MK, Kelsey PB, Forcione DG, Brugge WR, Casey BW, Syngal S. Recurrences are common after endoscopic ampullectomy for adenoma in the familial adenomatous polyposis (FAP) syndrome. Surg Endosc. 2014;28:2349-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Wood LD, Salaria SN, Cruise MW, Giardiello FM, Montgomery EA. Upper GI tract lesions in familial adenomatous polyposis (FAP): enrichment of pyloric gland adenomas and other gastric and duodenal neoplasms. Am J Surg Pathol. 2014;38:389-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Garrean S, Hering J, Saied A, Jani J, Espat NJ. Gastric adenocarcinoma arising from fundic gland polyps in a patient with familial adenomatous polyposis syndrome. Am Surg. 2008;74:79-83. [PubMed] |
| 6. | Srinivasa D, Wray CJ. Total gastrectomy with isoperistaltic jejunal interposition flap for symptomatic management of gastric polyposis from familial adenomatous polyposis. J Gastrointest Oncol. 2014;5:E18-E21. [PubMed] |
| 7. | Caillié F, Paye F, Desaint B, Bennis M, Lefèvre JH, Parc Y, Svrcek M, Balladur P, Tiret E. Severe duodenal involvement in familial adenomatous polyposis treated by pylorus-preserving pancreaticoduodenectomy. Ann Surg Oncol. 2012;19:2924-2931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Alderlieste YA, Rauws EA, Mathus-Vliegen EM, Fockens P, Dekker E. Prospective enteroscopic evaluation of jejunal polyposis in patients with familial adenomatous polyposis and advanced duodenal polyposis. Fam Cancer. 2013;12:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | van Heumen BW, Nieuwenhuis MH, van Goor H, Mathus-Vliegen LE, Dekker E, Gouma DJ, Dees J, van Eijck CH, Vasen HF, Nagengast FM. Surgical management for advanced duodenal adenomatosis and duodenal cancer in Dutch patients with familial adenomatous polyposis: a nationwide retrospective cohort study. Surgery. 2012;151:681-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Alderlieste YA, Bastiaansen BA, Mathus-Vliegen EM, Gouma DJ, Dekker E. “High rate of recurrent adenomatosis during endoscopic surveillance after duodenectomy in patients with familial adenomatous polyposis”. Fam Cancer. 2013;12:699-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Lees CD, Hermann RE. Familial polyposis coli associated with bile duct cancer. Am J Surg. 1981;141:378-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Järvinen HJ, Nyberg M, Peltokallio P. Biliary involvement in familial adenomatosis coli. Dis Colon Rectum. 1983;26:525-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Komorowski RA, Tresp MG, Wilson SD. Pancreaticobiliary involvement in familial polyposis coli/Gardner’s syndrome. Dis Colon Rectum. 1986;29:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Spigelman AD, Farmer KC, James M, Richman PI, Phillips RK. Tumours of the liver, bile ducts, pancreas and duodenum in a single patient with familial adenomatous polyposis. Br J Surg. 1991;78:979-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Futami H, Furuta T, Hanai H, Nakamura S, Baba S, Kaneko E. Adenoma of the common human bile duct in Gardner’s syndrome may cause relapsing acute pancreatitis. J Gastroenterol. 1997;32:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Rafiq E, Alaradi O, Bawany M, Nawras A. A combination of snare polypectomy and apc therapy for prolapsing common bile duct adenoma. J Interv Gastroenterol. 2012;2:193-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Sakai Y, Sugiyama H S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Ma S