Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3121
Peer-review started: June 3, 2014
First decision: June 27, 2014
Revised: July 15, 2014
Accepted: September 5, 2014
Article in press: September 5, 2014
Published online: March 14, 2015
Processing time: 288 Days and 5.6 Hours
Endoscopic submucosal dissection (ESD) is now widely accepted as a strategy to treat superficial esophageal neoplasms. The rate of adverse events, such as perforation, has been decreasing with the improvement of devices and techniques. In this paper, we report a case of esophageal cancer that had a diverticulum under cancerous epithelium. The diverticulum was not detected during preoperative examination, and led to perforation during the ESD procedure. Our case shows that, although rare, some diverticula can exist underneath the mucosal surface without obvious depression. If there is any sign of hidden diverticula during ESD, surgeons should proceed with caution or, depending on the case, the procedure should be discontinued to avoid adverse events.
Core tip: We report a case of esophageal cancer with a diverticulum in a patient who underwent endoscopic submucosal dissection (ESD). Although most esophageal diverticula can be diagnosed by endoscopy or computed tomography scans, the diverticulum in this case was not detected by these examinations before ESD, and led to perforation during the ESD procedure. This is a rare case; however, we should be aware that there could be diverticula without obvious depression.
- Citation: Tanaka S, Toyonaga T, Ohara Y, Yoshizaki T, Kawara F, Ishida T, Hoshi N, Morita Y, Azuma T. Esophageal diverticulum exposed during endoscopic submucosal dissection of superficial cancer. World J Gastroenterol 2015; 21(10): 3121-3126
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/3121.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.3121
An increasing number of superficial esophageal neoplasms are treated by endoscopic submucosal dissection (ESD)[1-3]. However, to our knowledge, there has been only one case reported in which ESD was performed in esophageal cancer with diverticula[4]. This is mainly because the patient will undergo surgical resection regardless of the depth of the tumor, if the cancer lesion is found on a diverticulum[5]. We present a case of esophageal cancer with diverticulum that underwent ESD. Esophageal diverticulum was not diagnosed preoperatively, but was exposed while dissecting the cancer lesion.
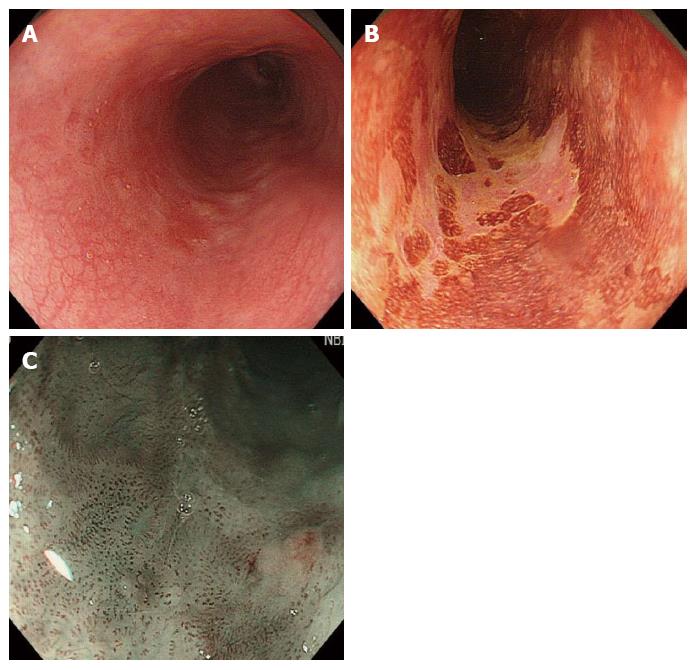
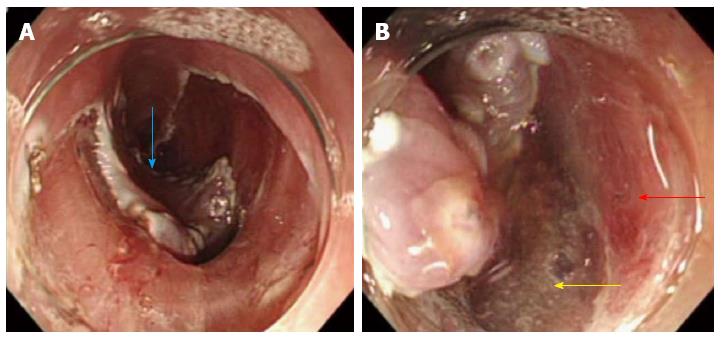
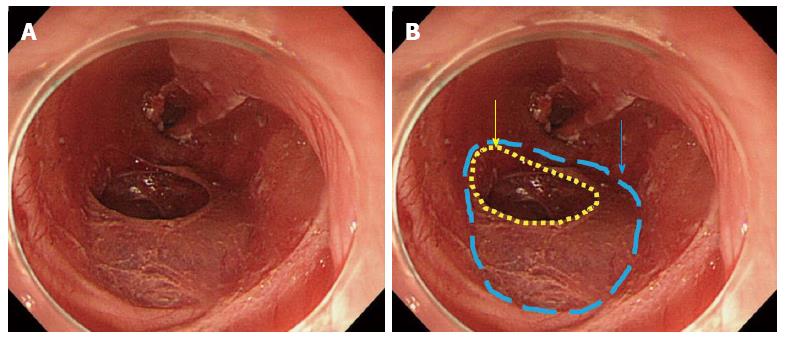
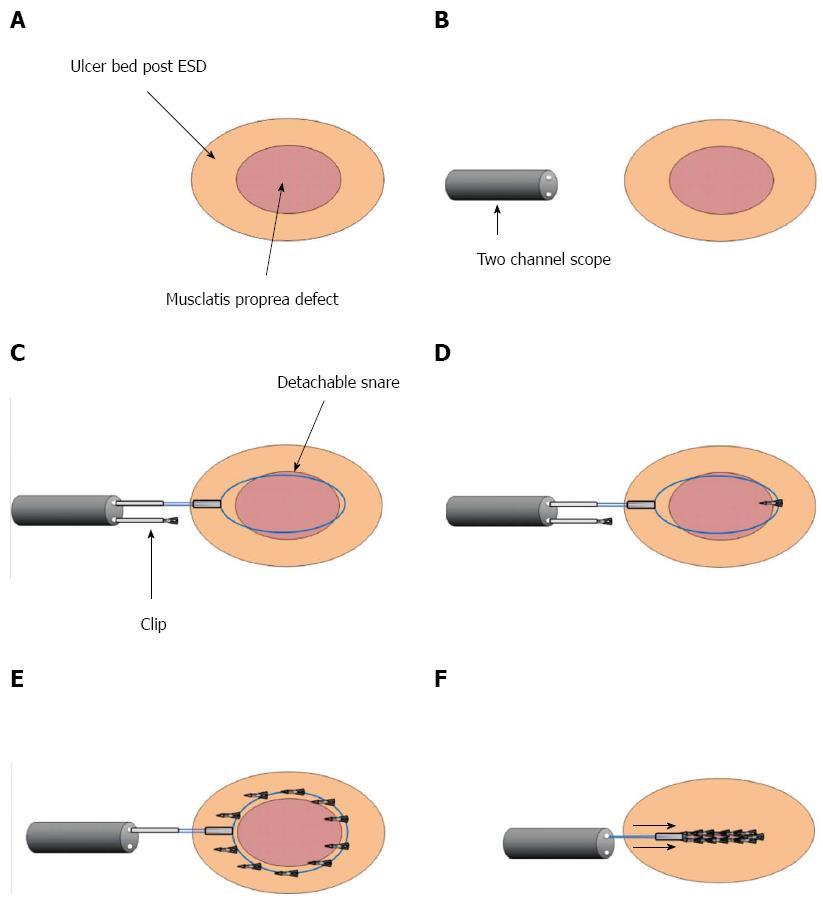
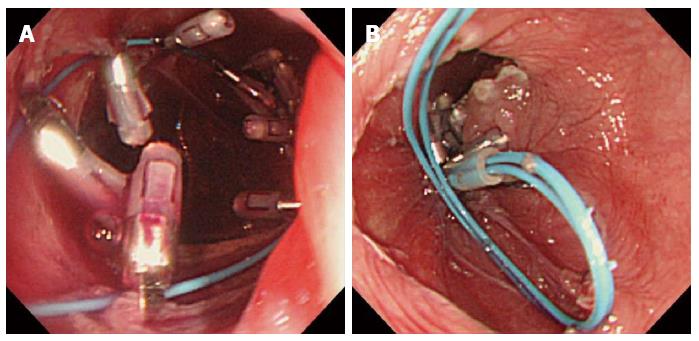
A 55-year-old woman underwent screening by esophagogastroduodenoscopy, and a cancer lesion was detected on the left side of the middle thoracic esophagus. The macroscopic type was 0-IIc, and it had expanded to half of the circumference of the esophagus (Figure 1A and B). In magnified narrow band imaging (NBI) observation, an intraepithelial papillary capillary loop (IPCL) was detected as a small dot pattern (Figure 1C). We diagnosed that the lesion was limited to epithelial (EP) or lamina propria mucosal (LPM) invasion due to the lack of findings indicative of submucosal invasion, such as fold convergence, elevation of mucosa surrounding the lesion or advanced irregularity of IPCL. Computed tomography (CT) scans taken before ESD did not show the existence of diverticula in the esophagus. ESD was indicated for the treatment. The ESD procedure was performed using a FlushKnife BT 1.5 mm (Fujifilm Medical, Tokyo, Japan), and VIO 300D (ERBE Elektromedizin, GmbH, Tübingen, Germany) was used as the power source for electrical cutting and coagulation. Submucosal injection and mucosal incision were performed without any abnormal events. However, during the course of the dissection, a depression in the center of the cancer lesion became noticeable (Figure 2A). When the dissection reached the edge of the depression, the muscularis propria layer abruptly ended. There was an area where muscularis propria was missing, which indicated that there was a shallow pulsion diverticulum under the tumor (Figure 2B). We proceeded cautiously with the dissection to separate submucosa and adventitia while attempting to maintain the appropriate dissection level, but perforation occurred at the bottom of the defect of the muscularis propria, when the en bloc resection was nearly complete. We quickly removed the dissected tissue and analyzed the perforation in detail. The defect of the muscularis propria was about 3 cm x 2 cm in size, and located in the center of the dissected mucosal defect. The perforation hole was found at the anal side of the muscularis propria defect (Figure 3A and B). Since the muscularis propria defect and the perforation hole were too large to close using clips, we decided to close the entire muscularis propria defect using clips and a detachable snare. The detachable snare was fixed surrounding the defect of the muscularis propria using clips placed approximately every 0.5 cm using a 2-channel scope (GIF-2TQ260M) (Figure 4A-D). Clipping was started from the anal side followed by placing clips one by one on the right side and the left side; 10 clips were used in total to surround the entire defect (Figure 4E). The rubber stopper was tightened, and it was successfully closed (Figure 5A, B). It took 60 min to dissect the cancer lesion and 20 min to close the muscularis propria defect, making the total operation time 80 min.
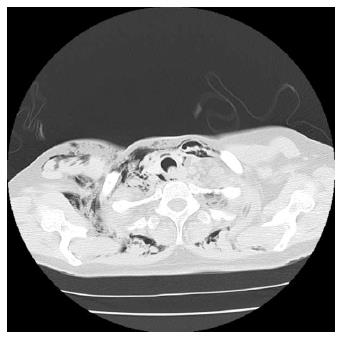
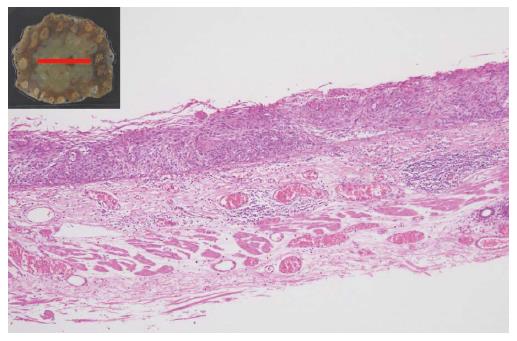
CT scans after the ESD revealed marked mediastinal and subcutaneous emphysema (Figure 6). The patient underwent fasting and a course of antibiotic treatment (meropenem trihydrate at 1 g/d for 10 d). The mediastinal and subcutaneous emphysema was improved by day 3 after ESD. She had high fever over 38 degrees Celsius, chest pain, and the white blood cell count was elevated up to 14000/μL, but these symptoms had all resolved by day 7. Contrast examination of the esophagus using diatrizoic acid (Gastrografin®) was undertaken on day 13, confirming that there was no leakage from the perforated hole. Although 14 d of fasting and 21 d of admission were required, she was treated conservatively. Histology revealed that squamous cell carcinoma was limited within EP, and the muscularis propria layer was not seen in the resected specimen (Figure 7), proving that the defect of the muscularis propria was not the result of deep dissection of the esophageal tissue.
Although esophageal stricture developed two months after ESD, it was not severe and required two sessions of endoscopic balloon dilation (EBD) to improve. No recurrence of cancer has been recorded as of 12 mo after the treatment.
Esophageal diverticula are rare, with a prevalence of 0.06% to 3.6% based on radiologic and endoscopic series[7,8]. The high risk of developing malignancy has also been described, for which the carcinogenetic factors include chronic mechanical irritation by food, repeated physical injury and inflammation; however, the involved mechanism remains elusive[9]. Esophageal diverticula are classically divided into two types: pulsion (false) and traction (true) diverticula. Pulsion diverticula occur as a result of increased intraluminal pressure and form protrusions of mucosa through the muscular wall; therefore, they lack muscularis propria. Zenker’s diverticulum and epiphrenic diverticulum are included in pulsion diverticula. Traction diverticula are created by the pulling force of the outside esophagus due to periesophageal inflammation, fibrosis and adhesions to surrounding structures. Most traction diverticula occur in the mid-esophagus, and the common causes include tuberculosis, histoplasmosis and malignancy. Most diverticula are easily recognized as mucosal depressions by endoscopic observation. However, in the present case, we could not diagnose the diverticulum preoperatively because the depression was obscured during endoscopy, and CT scans could not capture it. Although this is a rare case, it indicates that some esophageal diverticula can exist under the mucosal surface without obvious depression.
Esophageal cancer that involves diverticula is generally treated by surgery, regardless of the depth of invasion[5,9]. However, in the process of selecting the therapeutic strategy, it may be important to consider what type of diverticulum is involved. In the case of traction diverticulum, which has muscularis propria, the risk of perforation is presumably less than for pulsion diverticulum. Therefore, if the cancer invasion is within EP or LPM, ESD could be indicated.
The use of endoscopic ultrasound (EUS) will help to detect diverticula; however, EUS is not routinely performed for superficial esophageal cancer especially shallow lesion, and accordingly, it was not performed in the present case. Nevertheless, our case suggests that preoperative EUS examination should be considered before ESD, if the coexistence of diverticula is suspected. When the cancer lesion is on a pulsion diverticulum, ESD should be avoided.
In addition, the location of diverticula should be taken into account. If the diverticulum is located at the edge and only partly involved in the cancer lesion, ESD is technically possible irrespective of the type of diverticulum. This is because only part of the mucosal layer covering the diverticulum will be dissected, and even if perforation occurs, the hole would be small enough to close using clips. However, if the diverticulum is found in the center of the cancer lesion, the entire mucosa over the diverticulum will be dissected, which can lead to a high risk of perforation. Moreover, it will require closure of the entire diverticulum, which can be large and may further require advanced skill and devices other than just clips, as shown in our case.
Closure of the ulcer after ESD for the lesion with diverticula is essential to prevent delayed perforation. We closed the perforation hole and the defect of the muscularis propria layer using clips and a detachable snare. This method was originally reported to suture a large mucosal defect after endoscopic resection of colorectal neoplasm[10]. We adopted this method for the esophagus in the present case, and the perforation hole and muscularis propria defect were successfully closed. Recently, the effectiveness of polyglycolic acid sheets and fibrin glue, and the use of an Over-the-Scope Clip to close the perforation of a digestive tract were reported[11,12]. These new methods might have been effective in our case; however, they require special devices or reagents. Therefore, we adopted the method using clips and a detachable snare, which does not require other tools besides those in regular clinical therapy.
When the perforation occurred, we considered discontinuation of the ESD. However, we decided to complete the procedure as long as the vital signs were stable. This was because alternative treatment, such as surgery or chemoradiation therapy, would involve overtreatment for the cancer stage of the present case. Fortunately, the patient’s vital signs were stable until the procedure was complete. Of note, we routinely use CO2 insufflation during esophageal ESD. We consider CO2 insufflation to be absolutely imperative because it is safer then room air insufflation in the case of unpredictable complications like this.
In conclusion, we experienced a case of esophageal cancer with diverticulum, which was not diagnosed preoperatively. Although it is a rare case, we should be aware that there could be diverticula without an obvious depression. In the case of unpredicted perforation with the diverticulum, the method using clips and a detachable snare could be very effective to manage the simultaneous closure of perforation hole and diverticulum.
A 55-year-old woman underwent screening esophagogastroduodenoscopy, and a cancer lesion was detected on the left side of the middle thoracic esophagus.
Esophageal cancer with diverticulum, which was not diagnosed preoperatively.
Esophageal cancer without coexisting diverticulum.
Routine laboratory tests showed no abnormal findings.
During endoscopic submucosal dissection (ESD), there was an area where muscularis propria was missing, which indicated that there was a shallow pulsion diverticulum under the tumor.
Histology revealed that squamous cell carcinoma was limited within epithelium, and the muscularis propria layer was not seen in the resected specimen.
The lesion was resected by ESD, but perforation occurred in the center of the dissected mucosal defect. After removing the dissected tissue, the authors closed the entire muscularis propria defect using clips and a detachable snare.
ESD for esophageal cancer with diverticulum is rare, with only 1 case reported in the literature.
Pulsion diverticula occur as a result of increased intraluminal pressure and form protrusions of mucosa through the muscular wall; therefore, they lack muscularis propria. Traction diverticula are created by the pulling force of the outside esophagus due to periesophageal inflammation, fibrosis and adhesions to surrounding structures; they have muscularis propria.
Although it is a rare case, the authors should be aware that there could be diverticula without an obvious depression.
The manuscript “An esophageal diverticulum exposed during endoscopic submucosal dissection of a superficial cancer” is an interesting case report. Overall, the authors did a nice job and presented the case in an adequate manner. The authors further briefly discussed the most important aspects of this case.
| 1. | Inoue H, Minami H, Kaga M, Sato Y, Kudo SE. Endoscopic mucosal resection and endoscopic submucosal dissection for esophageal dysplasia and carcinoma. Gastrointest Endosc Clin N Am. 2010;20:25-34, v-vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Toyonaga T, Man-I M, Fujita T, Nishino E, Ono W, Morita Y, Sanuki T, Masuda A, Yoshida M, Kutsumi H. The performance of a novel ball-tipped Flush knife for endoscopic submucosal dissection: a case-control study. Aliment Pharmacol Ther. 2010;32:908-915. [PubMed] |
| 3. | Linghu E, Feng X, Wang X, Meng J, Du H, Wang H. Endoscopic submucosal tunnel dissection for large esophageal neoplastic lesions. Endoscopy. 2013;45:60-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Gotoda T, Takenaka R, Inokuchi T, Fujiki S. Endoscopic submucosal dissection for a superficial esophageal squamous cell carcinoma within the parabronchial diverticula. Dig Endosc. 2013;25:91-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Brücher BL, Sarbia M, Oestreicher E, Molls M, Burian M, Biemer E, Stein HJ. Squamous cell carcinoma and Zenker diverticulum. Dis Esophagus. 2007;20:75-78. [PubMed] |
| 6. | Hoghooghi D, Coakley FV, Breiman RS, Qayyum A, Yeh BM. Frequency and etiology of midesophageal diverticula at barium esophagography. Clin Imaging. 2006;30:245-247. [PubMed] |
| 7. | Watanabe S, Matsuda K, Arima K, Uchida Y, Nishioka M, Haruo T, Uohashi T. Detection of subclinical disorders of the hypopharynx and larynx by gastrointestinal endoscopy. Endoscopy. 1996;28:295-298. [PubMed] |
| 8. | Herbella FA, Oliveira DR, Del Grande JC. Are idiopathic and Chagasic achalasia two different diseases? Dig Dis Sci. 2004;49:353-360. [PubMed] |
| 9. | Nakamura T, Ota M, Narumiya K, Sato T, Shirai Y, Yamamoto M, Kuramochi H, Hayashi K. [Docetaxel plus S-1 as a second-line chemotherapy for metastasis or recurrence of esophageal cancer]. Gan To Kagaku Ryoho. 2012;39:227-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Matsuda T, Fujii T, Emura F, Kozu T, Saito Y, Ikematsu H, Saito D. Complete closure of a large defect after EMR of a lateral spreading colorectal tumor when using a two-channel colonoscope. Gastrointest Endosc. 2004;60:836-838. [PubMed] |
| 11. | Takimoto K, Toyonaga T, Matsuyama K. Endoscopic tissue shielding to prevent delayed perforation associated with endoscopic submucosal dissection for duodenal neoplasms. Endoscopy. 2012;44 Suppl 2 UCTN:E414-E415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 101] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Dobrucali AM, Hummel R, Wittmann T S- Editor: Ma YJ L- Editor: Logan S E- Editor: Liu XM