Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3093
Peer-review started: May 4, 2014
First decision: June 10, 2014
Revised: July 21, 2014
Accepted: November 8, 2014
Article in press: November 11, 2014
Published online: March 14, 2015
Processing time: 318 Days and 17.1 Hours
AIM: To compare the clinical outcomes between jejunal interposition reconstruction and Roux-en-Y anastomosis after total gastrostomy in patients with gastric cancer.
METHODS: A systematic literature search was conducted by two independent researchers on PubMed, EMBASE, the Cochrane Library, Google Scholar, and other English literature databases, as well as the Chinese Academic Journal, Chinese Biomedical Literature Database, and other Chinese literature databases using “Gastrostomy”, “Roux-en-Y”, and “Interposition” as keywords. Data extraction and verification were performed on the literature included in this study. RevMan 5.2 software was used for data processing. A fixed-effects model was applied in the absence of heterogeneity between studies. A random effects model was applied in the presence of heterogeneity between studies.
RESULTS: Ten studies with a total of 762 gastric cancer patients who underwent total gastrostomy were included in this study. Among them, 357 received jejunal interposition reconstruction after total gastrostomy, and 405 received Roux-en-Y anastomosis. Compared with Roux-en-Y anastomosis, jejunal interposition reconstruction significantly decreased the incidence of dumping syndrome (OR = 0.18, 95%CI: 0.10-0.31; P < 0.001), increased the prognostic nutritional index [weighted mean difference (WMD) = 6.02, 95%CI: 1.82-10.22; P < 0.001], and improved the degree of postoperative weight loss [WMD = 2.47, 95%CI: -3.19-(-1.75); P < 0.001]. However, there is no statistically significant difference in operative time, hospital stay, or incidence of reflux esophagitis.
CONCLUSION: Compared with Roux-en-Y anastomosis, patients who underwent jejunal interposition reconstruction after total gastrostomy had a lower risk of postoperative long-term complications and improved life quality.
Core tip: This study compared the clinical outcomes between jejunal interposition reconstruction and Roux-en-Y anastomosis after total gastrostomy in patients with gastric cancer through systematic review and meta-analysis. We found compared with Roux-en-Y anastomosis, jejunal interposition reconstruction significantly decreased the incidence of dumping syndrome, increased the prognostic nutritional index, and improved the degree of postoperative weight loss. However, there is no statistically significant difference in operative time, hospital stay, or incidence of reflux esophagitis. Therefore, we conclude that patients who underwent jejunal interposition reconstruction after total gastrostomy had a lower risk of postoperative long-term complications and improved life quality.
- Citation: Fan KX, Xu ZF, Wang MR, Li DT, Yang XS, Guo J. Outcomes for jejunal interposition reconstruction compared with Roux-en-Y anastomosis: A meta-analysis. World J Gastroenterol 2015; 21(10): 3093-3099
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/3093.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.3093
To date, there are approximately 70 types of digestive tract reconstructions after total gastrostomy[1]. Although operative technique is gradually improving, there is still no relatively ideal and standard surgical approach to digestive tract reconstruction after total gastrostomy. There are two main surgical approaches: esophagojejunal anastomosis and jejunal interposition reconstruction with preservation of the duodenum passage[2]. However, which type of digestive tract reconstruction should be applied after total gastrostomy has long remained controversial among both domestic and foreign researchers[3-9]. The main controversial issues focus on (1) the necessity of preserving the duodenum passage; and (2) the necessity of creating a gastric pouch and what form of pouch reconstruction better duplicates human physiological function. Because esophagojejunal anastomosis (Roux-en-Y anastomosis) can be relatively easily performed, the incidence of postoperative complications is lower[10]; in addition, it can resolve possible reflux esophagitis relatively well and has been accepted by most surgeons and researchers. However, this procedure has not been fully accepted in light of the poor postoperative quality of life caused by insufficient food intake and malabsorption in gastric cancer patients who have undergone Roux-en-Y reconstruction. Jejunal interposition reconstruction preserves the duodenum passage, in which food passes through the duodenum, stimulates the secretion of bile and pancreatic juice, and is fully mixed with chyme[11]. It is beneficial for food digestion and absorption and the regulation of gastrointestinal hormone. This surgical approach enhances the postoperative digestion and absorption of nutrients, therefore improving the long-term quality of life in patients with gastric cancer. However, the complexity of surgical procedure and longer operative time would certainly increase the risk of the intraoperative procedure and of postoperative complications[12]. Therefore, whether to apply jejunal interposition reconstruction has in recent years been a research topic of considerable interest in the surgical field of digestive tract reconstruction after total gastrostomy. This study performed a meta-analysis on the long-term postoperative complications and quality of life between these two digestive tract reconstructions; thus, it may provide medical evidence for choosing a reasonable surgical approach to digestive tract reconstruction after total gastrostomy in evidence-based practice.
Two researchers independently conducted a systematic literature search. “Gastrostomy”, “Roux-en-Y”, and “Interposition” were used as keywords to search the papers published in PubMed, EMBASE, the Cochrane Library, Google Scholar, and other English literature databases. “Gastrostomy”, “Roux-en-Y”, and “Interposition” were also used as keywords to search the papers published in the Chinese Academic Journal, Chinese Biomedical Literature Database, China Science and Technology Journal Database, and other Chinese literature databases. In addition, we explored the links to the “related articles” to expand the search to all abstracts, studies, and citation retrievals with related topics. The final date of database information retrieval was December 2013. We also retrieved the full texts from related publication groups.
Inclusion criteria were as follows: (1) the study design was a randomized controlled trial; (2) the study subjects were gastric cancer patients who underwent total gastrostomy; the study compared two digestive tract reconstruction approaches, Roux-en-Y anastomosis and jejunal interposition reconstruction; and (3) the assessment parameters included operative time, hospital stay, dumping syndrome, reflux esophagitis, prognostic nutritional index (PNI), and postoperative weight loss. Exclusion criteria were as follows: (1) non-randomized controlled trials, retrospective or observational studies; (2) study of patients with non-primary gastric cancer or benign gastric tumor, or recurrent gastric cancer; (3) studies published in neither Chinese nor in English; (4) animal or molecular studies; and (5) duplicate publication or studies without detailed retrievable data.
Two researchers retrieved and browsed the titles and abstracts of studies independently. After excluding studies that obviously did not meet the inclusion criteria, they read the full texts of potentially included studies. Only studies published in English and Chinese were included in this study analysis. Data were extracted in accordance with the standard criteria table and cross-checked. For publications where the two researchers disagreed on inclusion in the analysis, the decision was made by thorough discussion or with assistance from a third researcher. The extracted data included the author, date of publication, time the study was conducted, sample size, study design, whether it was a multi-center study, operative time, hospital stay, dumping syndrome, reflux esophagitis, PNI, and postoperative weight loss. In the absence of sufficient information to extract the data from the original publications, the necessary data would be obtained from the corresponding author by email. If the corresponding author could not be reached, the studies were excluded from this analysis.
We used the Jadad scale to evaluate the quality of randomized controlled trials (RCTs) in accordance with the randomization, double-blinding, and numbers of withdrawals and dropouts from the study. We evaluated each study as follows: (1) a score of 2 indicates appropriately established randomization; a score of 1 indicates unclear randomization; and a score of 0 was given for inappropriate randomization; (2) an appropriate blocked randomization design was given a score of 2; a score of 1 was given for unclear design; and a score of 0 was given to an inappropriate or absent blocked randomization design; (3) an appropriately applied blinding design was given a score of 2; unclear blinding received a score of 1; and a score of 0 was given to RCTs without blinding design; and (4) a score of 1 was given to a study if it recorded the number and cause of withdrawals and dropouts. No report of withdrawals and dropouts was given a score of 0. A study with a Jadad scale score of 1-3 has lower quality, whereas scores of 4-7 represent higher-quality literature.
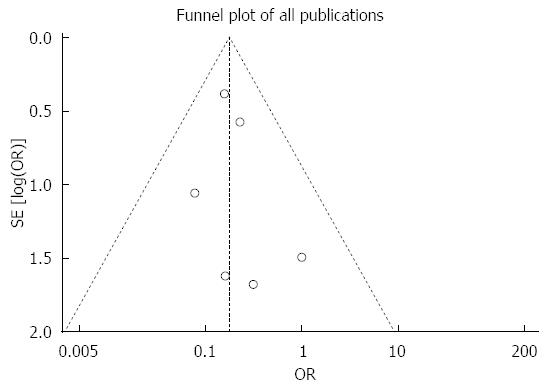
We used the RevMan 5.0 statistical software provided by the Cochrane collaboration network for analysis. The OR was used as a categorical variable to evaluate the efficacy of the two digestive tract reconstruction approaches after total gastrostomy for gastric cancer for statistical analysis. The weighted mean difference (WMD) was used as a continuous variable to measure the effect size. The Q-test was used to evaluate the heterogeneity between studies. Heterogeneity was considered to be present if the P-value was greater than 0.1. The extent of heterogeneity between results was quantitatively analyzed. A fixed-effects model was applied in the absence of heterogeneity between studies. A random-effects model was applied in the presence of heterogeneity between studies. The ORs and corresponding 95%CIs were calculated afterward. The P-value of the overall effect was tested by the Z-test. Forest plots represented the pooled ORs and 95%CIs. A funnel plot was drawn to detect publication bias.
The preliminary literature selection included 497 English studies and 147 Chinese studies. By browsing the titles and abstracts, we excluded 623 non-related studies and non-randomized controlled trials. The analysis preliminarily included 21 studies. We read the full texts of the studies and excluded studies that did not meet the inclusion criteria and those for which the data could not be extracted from the study results, indicated by a histogram or line graph. Ultimately, we included 10 studies[13-22], of which 7 were English studies and 3 Chinese studies.
The ten RCT studies included a total of 762 cases that underwent digestive tract reconstruction after total gastrostomy. Among these cases, 357 underwent jejunal interposition reconstruction (PJI group), and 405 underwent Roux-en-Y anastomosis (R-Y group). All studies employed randomization, blocked randomization and blinding design. Follow-up studies were completed postoperatively in all 10 studies (Table 1). Five studies reported lost cases within the follow-up period. One study performed intention-to-treat analysis. The quality of the included RCTs was evaluated using the Jadad scale. The baseline data of the two groups are similar, presenting relatively high comparability. The methodological evaluation showed that the scores of all 10 studies were above 4, indicating high study quality.
| Ref. | Publication year | Case (n) | Randomization | Outcomes | |
| Roux-en-Y group | PJI group | ||||
| Ishigami et al[13] | 2011 | 51 | 52 | Yes | Operation time; length of hospital stay |
| Pan et al[14] | 2008 | 87 | 45 | Yes | Prognostic nutritional index; body mass change; reflux esophagitis incidence; incidence of dumping syndrome |
| Adachi et al[15] | 2003 | 10 | 10 | Yes | Operation time; length of hospital stay; incidence of dumping syndrome |
| Nakane et al[16] | 2001 | 15 | 15 | Yes | Reflux esophagitis incidence; incidence of dumping syndrome |
| Schwarz et al[17] | 1996 | 30 | 30 | Yes | Operation time |
| Nakane et al[18] | 1995 | 10 | 10 | Yes | Incidence of dumping syndrome |
| Zherlov et al[19] | 2006 | 83 | 75 | Yes | Operation time; incidence of dumping syndrome |
| Yang et al[20] | 2006 | 15 | 16 | Yes | Body mass change |
| Liu et al[21] | 2005 | 74 | 74 | Yes | Reflux esophagitis incidence; incidence of dumping syndrome |
| Lu et al[22] | 2003 | 30 | 30 | Yes | Prognostic nutritional index; body mass change |
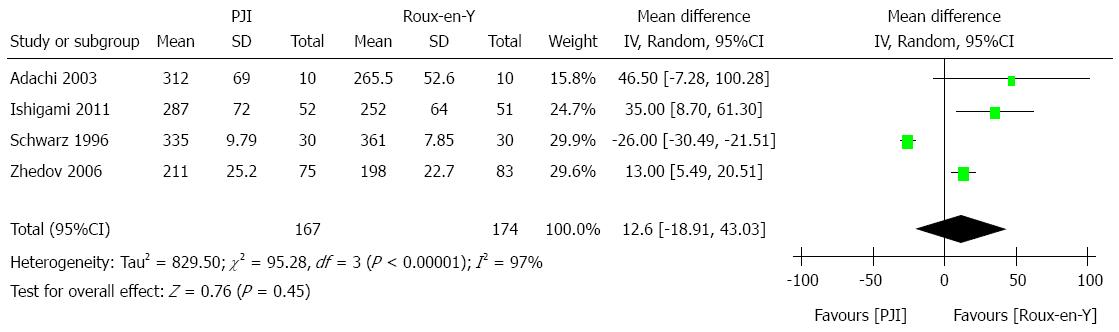
Operative time: Four studies reported operative time[6,8,10,12]. Heterogeneity was present among the studies (P < 0.01, I2 = 97%), and thus a random-effects model was applied for the pooled analysis. The results showed no statistically significant difference in operative time between the two groups (WMD = 12.06, 95%CI: -18.91-43.03, P = 0.45). The result is shown in Figure 1.
Hospital stay: Two studies reported hospital stay[6,8]. Heterogeneity was present between the studies (P = 0.04, I2 = 76%), and thus a random-effects model was applied for the pooled analysis. The results showed no statistically significant difference in hospital stay between the two groups (WMD = 1.26, 95%CI: -8.44-10.95; P = 0.80).
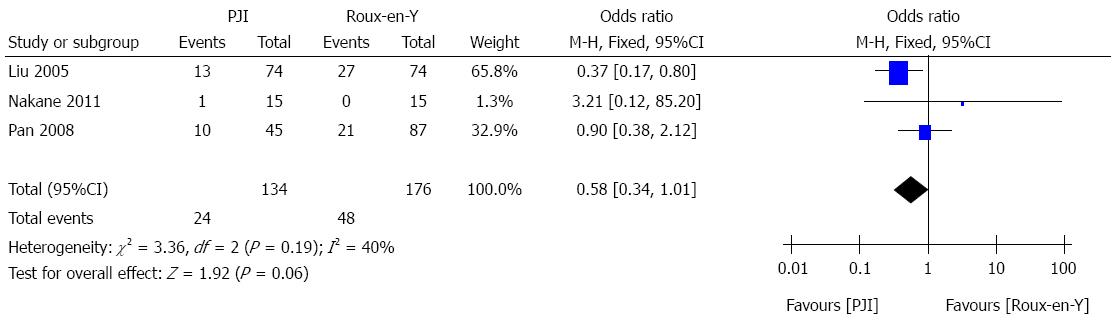
Incidence of reflux esophagitis: Three studies reported the incidence of reflux esophagitis[7,9,14]. No heterogeneity between studies was present (P = 0.19, I2 = 40%), and thus a fixed-effects model was applied for the pooled analysis. The results showed no statistically significant difference in incidence of reflux esophagitis between the two groups (OR = 0.58, 95%CI: 0.34-1.01; P = 0.06). The result is shown in Figure 2.
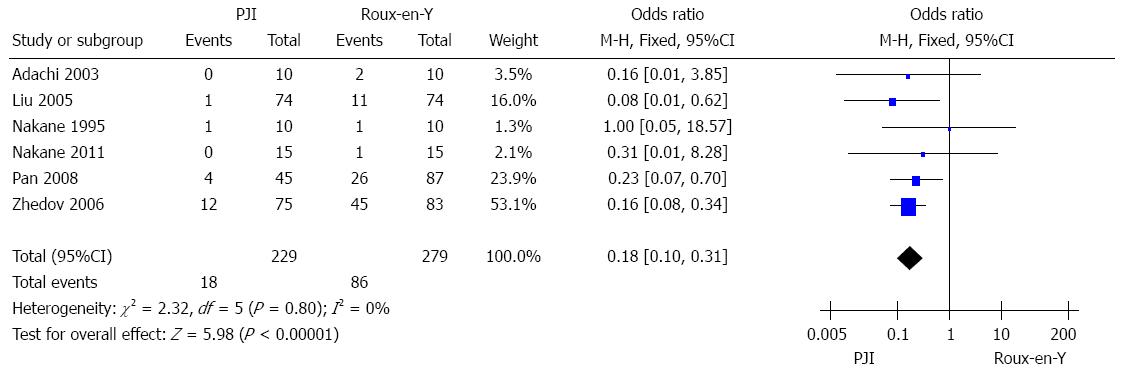
Incidence of dumping syndrome: Six studies[7-9,11,12,14] reported the incidence of dumping syndrome. No heterogeneity between studies was present (P = 0.45, I2 = 0%), and thus a fixed-effects model was applied for the pooled analysis. The results showed that compared with the R-Y group, the incidence of dumping syndrome was significantly lower in the PJI group (OR = 0.18, 95%CI: 0.10-0.31; P < 0.001). The result is shown in Figure 3.
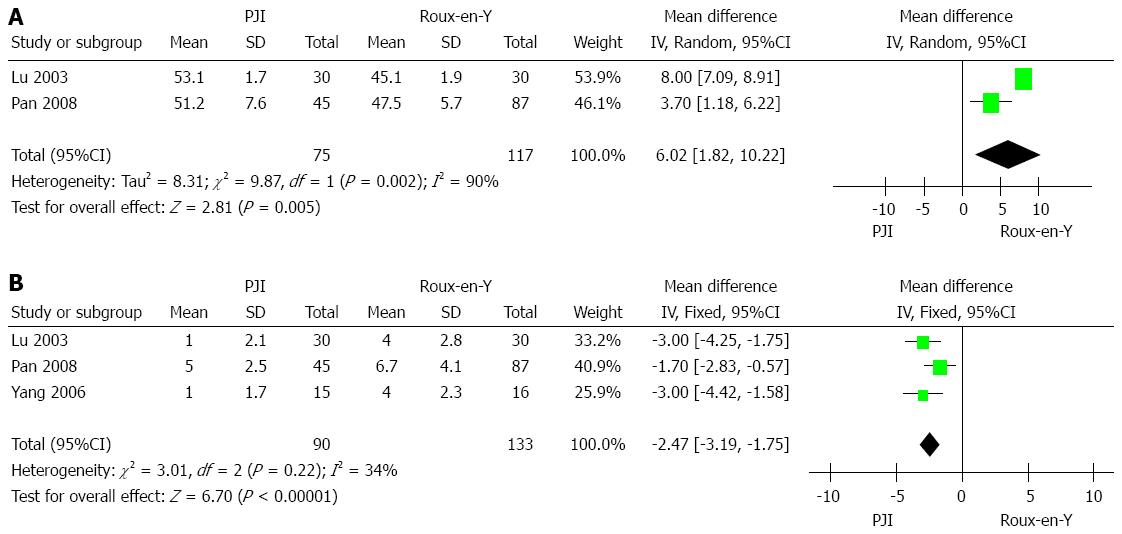
Prognostic nutritional index: Two studies[7,15] reported the prognostic nutritional index. Heterogeneity was present between the studies (P = 0.002, I2 = 90%), and thus a random-effects model was applied for the pooled analysis. The results showed that the prognostic nutritional index was significantly higher in the PJI group than in the R-Y group (WMD = 6.02, 95%CI: 1.82-10.22; P < 0.01). The result is shown in Figure 4A.
Postoperative weight loss: Three studies[7,13,15] reported the postoperative weight loss. No heterogeneity was present among the studies (P = 0.22, I2 = 34%), and thus a fixed-effects model was applied for the pooled analysis. The results showed that postoperative weight loss was significantly improved in the PJI group compared with the R-Y group [WMD = -(-2.47), 95%CI: -3.19-(-1.75); P < 0.01]. The result is shown in Figure 4B.
The distribution of the funnel plot was relatively symmetrical in the incidence analysis of dumping syndrome, indicating that publication bias was relatively small, as shown in Figure 5. Regarding other measured parameters, fewer than 5 studies were included in this analysis; therefore, the funnel plot analysis was not performed and the possibility of publication bias cannot be ruled out.
This systematic analysis showed that compared with Roux-en-Y anastomosis, jejunal interposition reconstruction has a lower incidence of dumping syndrome, a higher prognostic nutritional index, and a lower postoperative weight loss. There was no statistically significant difference in operative time, hospital stay, or incidence of reflux esophagitis between the two reconstruction procedures (P > 0.05 for all).
This systematic analysis has certain limitations: (1) only a few studies were included in the studies; moreover, a certain study was conducted with a small sample size, both of which could affect the results of meta-analysis; (2) only a few measured parameters were described in those studies, which may affect the argument strength of the analysis; (3) we did not search for RCTs published in other languages, which may result in a biased distribution; and (4) when we performed the pooled analysis, a random-effects model was used for three measured parameters because of poor homogeneity among the studies. The random-effects model tends to draw conservative conclusions, which may affect the analytical results. Therefore, future clinical trials of digestive tract reconstructions after total gastrostomy should be reported using the “consolidated Standards of Reporting Trials” guidelines, which have been internationally accepted. We should pay more attention to studies of quality of life in gastric cancer patients, especially in those with advanced gastric cancer. Moreover, we should pay attention to the results of placebo-controlled clinical trials.
In conclusion, compared with Roux-en-Y anastomosis, jejunal interposition reconstruction after total gastrostomy for gastric cancer could improve the long-term quality of life in patients. Moreover, it would not extend operative time or hospital stay. It is a safe and effective digestive tract reconstruction procedure.
To date, there are approximately 70 types of digestive tract reconstructions after total gastrostomy. Although operative technique is gradually improving, there is still no relatively ideal and standard surgical approach to digestive tract reconstruction after total gastrostomy.
There are two main surgical approaches: esophagojejunal anastomosis and jejunal interposition reconstruction with preservation of the duodenum passage. In order to assess accurately the clinical outcomes of these two reconstruction methods, the authors strictly limited inclusion criteria and carried out a comprehensive meta-analysis. This will contribute to a more systematic and objective evaluation of these two methods in gastric cancer treatment.
This study performed a meta-analysis on the long-term postoperative complications and quality of life between these two digestive tract reconstructions; thus, it may provide medical evidence for choosing a reasonable surgical approach to digestive tract reconstruction after total gastrostomy in evidence-based practice.
Compared with Roux-en-Y anastomosis, gastric cancer patients who underwent jejunal interposition reconstruction after total gastrostomy had a lower risk of postoperative long-term complications, and their quality of life was significantly improved.
This is a well written article. As the author pointed out, the deflection of the case is seen, and most of parameters depend on the Chinese cases. The author should search articles written in other language, such as Russian, South Korean and Japanese.
| 1. | Fukuchi M, Mochiki E, Suzuki O, Ishiguro T, Sobajima J, Saito K, Naitoh H, Kumagai Y, Baba H, Ishibashi K. Is gastric tube reconstruction the optimal surgical procedure for Siewert type II esophagogastric junction carcinoma? Anticancer Res. 2014;34:915-919. [PubMed] |
| 2. | Linke GR, Borovicka J, Tutuian R, Warschkow R, Zerz A, Lange J, Zünd M. Altered esophageal motility and gastroesophageal barrier in patients with jejunal interposition after distal esophageal resection for early stage adenocarcinoma. J Gastrointest Surg. 2007;11:1262-1267. [PubMed] |
| 3. | Zilberstein B, Jacob CE, Barchi LC, Yagi OK, Ribeiro-Jr U, Coimbra BG, Cecconello I. Simplified technique for reconstruction of the digestive tract after total and subtotal gastrectomy for gastric cancer. Arq Bras Cir Dig. 2014;27:133-137. [PubMed] |
| 4. | Ishi Y, Nakayama N, Kobayashi H, Yamaguchi S, Terasaka S, Houkin K. Successful Removal of a Metastatic Gastrointestinal Stromal Tumor in the Craniovertebral Junction using an Occipital Artery to Posterior Inferior Cerebellar Artery Bypass. Case Rep Neurol. 2014;6:139-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Chen YS, Wu SD, Kong J. Transumbilical single-incision laparoscopic subtotal gastrectomy and total intracorporeal reconstruction of the digestive tract in the treatment of benign peptic ulcers. J Surg Res. 2014;192:421-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Kakinoki K, Okano K, Oshima M, Suto H, Kashiwagi H, Yamamoto N, Akamoto S, Fujiwara M, Yachida S, Takama T. A novel triple secured technique for pancreatic reconstruction following pancreaticoduodenectomy for a soft pancreas. Hepatogastroenterology. 2014;61:469-474. [PubMed] |
| 7. | Sasaki K, Fujiwara Y, Kishi K, Motoori M, Yano M, Ohigashi H, Ohue M, Noura S, Maruhashi S, Takahashi H. Pathological findings of gastric mucosa in patients with gastric remnant cancer. Hepatogastroenterology. 2014;61:251-254. [PubMed] |
| 8. | Burks FN, Santucci RA. Management of iatrogenic ureteral injury. Ther Adv Urol. 2014;6:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 9. | Du X, Fan C, Zhang H, Lu J. [Application value of magnetic compression anastomosis in digestive tract reconstruction]. Zhonghua Weichang Waike Zazhi. 2014;17:512-515. [PubMed] |
| 10. | Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014;26 Suppl 2:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Ida S, Morita M, Hiyoshi Y, Ikeda K, Ando K, Kimura Y, Saeki H, Oki E, Kusumoto T, Yoshida S. Surgical resection of hypopharynx and cervical esophageal cancer with a history of esophagectomy for thoracic esophageal cancer. Ann Surg Oncol. 2014;21:1175-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Ninomiya S, Arita T, Sonoda K, Bandoh T, Shiroshita H, Tajima M. Feasibility and functional efficacy of distal gastrectomy with jejunal interposition for gastric cancer: a case series. Int J Surg. 2014;12:56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Ishigami S, Natsugoe S, Hokita S, Aoki T, Kashiwagi H, Hirakawa K, Sawada T, Yamamura Y, Itoh S, Hirata K. Postoperative long-term evaluation of interposition reconstruction compared with Roux-en-Y after total gastrectomy in gastric cancer: prospective randomized controlled trial. Am J Surg. 2011;202:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Pan Y, Li Q, Wang DC, Wang JC, Liang H, Liu JZ, Cui QH, Sun T, Zhang RP, Kong DL. Beneficial effects of jejunal continuity and duodenal food passage after total gastrectomy: a retrospective study of 704 patients. Eur J Surg Oncol. 2008;34:17-22. [PubMed] |
| 15. | Adachi S, Inagawa S, Enomoto T, Shinozaki E, Oda T, Kawamoto T. Subjective and functional results after total gastrectomy: prospective study for longterm comparison of reconstruction procedures. Gastric Cancer. 2003;6:24-29. [PubMed] |
| 16. | Nakane Y, Michiura T, Inoue K, Iiyama H, Okumura S, Yamamichi K, Hioki K. A randomized clinical trial of pouch reconstruction after total gastrectomy for cancer: which is the better technique, Roux-en-Y or interposition? Hepatogastroenterology. 2001;48:903-907. [PubMed] |
| 17. | Schwarz A, Büchler M, Usinger K, Rieger H, Glasbrenner B, Friess H, Kunz R, Beger HG. Importance of the duodenal passage and pouch volume after total gastrectomy and reconstruction with the Ulm pouch: prospective randomized clinical study. World J Surg. 1996;20:60-66; discussion 66-67. [PubMed] |
| 18. | Nakane Y, Okumura S, Akehira K, Okamura S, Boku T, Okusa T, Tanaka K, Hioki K. Jejunal pouch reconstruction after total gastrectomy for cancer. A randomized controlled trial. Ann Surg. 1995;222:27-35. [PubMed] |
| 19. | Zherlov G, Koshel A, Orlova Y, Zykov D, Sokolov S, Rudaya N, Karpovitch A. New type of jejunal interposition method after gastrectomy. World J Surg. 2006;30:1475-1480. [PubMed] |
| 20. | Yang PM. [Comparison of two reconstruction methods of alimentary canal after total gastrectomy]. Zhonghua Wei Chang Wai Ke Zazhi. 2006;9:23-25. [PubMed] |
| 21. | Liu ZJ, Liu CA, Gong JP, Zhou HW, Luo YS, Cheng YD. Affection of life quality betwee Jejunum and Rou-en-Y anastomosis digestive tract reconstruction. Zhongguo Shiyong Waike Zazhi. 2005;25:420-422. |
| 22. | Lu HS, Zhang JZ, Wu XY, Huang CM, Wang C, Zhang XF. [A prospective randomized study on the method of reconstruction after total gastrectomy]. Zhonghua Zhong Liu Zazhi. 2003;25:255-257. [PubMed] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Inamori M S- Editor: Gou SX L- Editor: Wang TQ E- Editor: Ma S