Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.2912
Peer-review started: August 2, 2014
First decision: August 27, 2014
Revised: September 20, 2014
Accepted: November 30, 2014
Article in press: December 1, 2014
Published online: March 14, 2015
Processing time: 227 Days and 20.2 Hours
AIM: To investigate the pharmacological effect of TongXie-YaoFang (TXYF) formula and its underlying mechanisms.
METHODS: A neonatal maternal separation plus restraint stress (NMS + RS) model of diarrhea-predominant irritable bowel syndrome was developed by subjecting male Sprague-Dawley rats to daily maternal separation from postnatal days 2 to 21 plus restraint stress from days 50 to 59. Rats were randomly divided into two groups (NMS + RS and TXYF formula), and rats with no handling or separation were used as normal controls. Starting from postnatal day 60, rats were administered TXYF formula (9.84 g/100 g body weight) orally twice daily for 14 consecutive days, while the normal and NMS + RS groups were given distilled water. The distinctions of movement index (MI, area under the curve of contraction intensity/min, mg/min) and contraction frequency (CF, number of contractions/min, times/min) of isolated colonic longitudinal smooth muscle strips (CLSMs) in the three groups before and after treatment were observed with a Power Lab system. Different inhibitors were applied, and then 10-4 mol/L acetylcholine chloride (Ach) was added to CLSMs to induce muscle contraction.
RESULTS: Before treatment, the MI of CLSMs in the NMS + RS and TXYF formula groups was similar and both higher than that in the normal group (545.49 ± 73.66 mg/min vs 245.76 ± 34.44 mg/min and 551.09 ± 54.29 mg/min vs 245.76 ± 34.44 mg/min, P < 0.01, respectively). After treatment, the MI in the TXYF formula group was lower than that in the NMS + RS group (261.39 ± 38.59 mg/min vs 533.9 ± 61.63 mg/min, P < 0.01). In the same way, the CF of CLSMs in the NMS + RS and TXYF formula groups was similar and both higher than that in the normal group (3.42 ± 0.25 times/min and 3.31 ± 0.21 vs 1.1 ± 0.17 times/min, P < 0.01) before treatment. After treatment, the CF in the TXYF formula group was lower than that in the NMS + RS group (1.42 ± 0.87 times/min vs 3.11 ± 0.82 times/min, P < 0.01) and similar to that in the normal group (1.42 ± 0.87 times/min vs 1.09 ± 0.13 times/min). When 8-(N,N-diethylamino)octyl 3,4,5-trimethoxybenzoate hydrochloride and 4-aminopyridine were added to the bath and equilibrated for 30 min, respectively, and 10-4 mol/L Ach was added to CLSMs to induce muscle contraction, MI of the CLSMs in the TXYF formula group was lower than that in the normal group (666 ± 36.32 mg/min vs 747.77 ± 49.47 mg/min, and 686.53 ± 39.17 mg/min vs 750.45 ± 29.39 mg/min; P < 0.01, respectively). The MI of CLSMs in the TXYF formula group was lower than that in the normal group after treatment with nifedipine (689.48 ± 30.84 mg/min vs 741.65 ± 32.41 mg/min; P < 0.05).
CONCLUSION: TXYF formula inhibits colon contraction in rats. This may be related to activation of specific potassium channels and inhibition of extracellular calcium internal flow.
Core tip: Diarrhea-predominant irritable bowel syndrome (D-IBS) is a chronic gastrointestinal disease that seriously affects quality of life. Colon dysmotility is recognized as one of the pathophysiological factors. TongXie-YaoFang formula can effectively relieve diarrhea and lower visceral hypersensitivity in D-IBS rats, mainly via inhibiting the amplitude and frequency of colonic longitudinal smooth muscle contraction. Its action of mechanism may be related to the activation of specific potassium channels, inhibition of extracellular calcium internal flow, and reduction of intracellular free Ca2+ concentration.
- Citation: Yang C, Zhang SS, Li XL, Wang ZF, Zhao LQ. Inhibitory effect of TongXie-YaoFang formula on colonic contraction in rats. World J Gastroenterol 2015; 21(10): 2912-2917
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/2912.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.2912
Diarrhea-predominant irritable bowel syndrome (D-IBS) is a chronic functional gastrointestinal disease. The diagnosis of D-IBS is based on symptom assessment and the Rome III diagnostic criteria[1]. The pathogenesis of D-IBS has not been fully clarified and colon dysmotility is recognized as one of the pathophysiological factors[2]. The usual treatment of the disease in Western medicine involves symptomatic therapy, which is unsatisfactory for patients, while simultaneously increasing the use of healthcare resources[3,4]. Traditional Chinese medicine (TCM) can significantly improve symptoms and quality of life, therefore, increasing numbers of patients have begun to seek treatment with TCM[5,6]. Many clinical studies have shown that TongXie-YaoFang (TXYF) formula can significantly improve D-IBS clinical symptoms and enhance quality of life[7,8]. However, the specific mechanism of action has not been completely elaborated. The purpose of this study was to observe the effect of TXYF formula on contraction of colon smooth muscle in D-IBS rats, and discuss its mechanism of action.
Neonatal Sprague-Dawley rats were obtained on postnatal day 1 from Vital River Laboratories Animal Technology Co. Ltd. (Beijing, China), and kept at Dongzhimen Hospital Affiliated with Beijing University of Chinese Medicine. The pups were randomly assigned to one of the following two rearing conditions: (1) neonatal maternal separation plus restraint stress (NMS + RS); or (2) no handling or separation (normal).
The NMS + RS litters were removed from their cages and separated from their dams for 3 h each day, whereas the normal pups remained in their home cages during the period of postnatal days 2-21[9,10]. During the 3-h period of separation, the pups were removed from the nest to stand-alone compartments, where the temperature was maintained at 23 ± 0.5 °C in a thermally regulated facility. The litters were returned to their home cages immediately after separation[11]. All the rats were reared on a 12:12 h light-dark cycle (lights on at 08:00 h) with access to food and water ad libitum. On day 22, the sexes of the pups, including those in the normal group, were distinguishable, so the females were removed and the males retained[12].
On days 50-59, the NMS + RS rats were placed in transparent plastic restraint cylinders (4 cm × 4 cm × 18 cm), in which they could move forward and backward but could not turn around[13]. The rats remained in the restraint cylinders for 3 h, with access to food and water ad libitum, in the morning and afternoon of each day. The NMS + RS rats were divided into two groups (NMS + RS and TXYF formula).
All animal care and experimental procedures were conducted according to the institutional ethical guidelines and conformed to the requirements of the Institutional Animal Care and Use Committee of Beijing University of Chinese Medicine and the Animal Ethics Committee of Dongzhimen Hospital Affiliated with Beijing University of Chinese Medicine.
TXYF formula is composed of the following traditional Chinese herbal medicines: Bai zhu (Atractylodesm macrocephala Koidz - Acta Horti Gothoburgensis 1938; 12: 310), 93.75 g; Shao yao (Paeonia lactiflora Pall - Reise Russ Reich 1776; 3: 286), 62.5 g; Chen pi (Citrus reticulata Blanco - Fl Filip 1837; 610), 46.875 g; and Fang feng [Saposhnikovia divaricata (Turcz) Schischk - Fl URSS 1951; 17: 359], 31.25 g. It was manufactured by Preparation Room for TCM of Beijing Chinese Medicine Hospital. All raw materials in the formula were examined according to the quality control criteria in the Chinese Pharmacopeia[14].
From postnatal day 60, the rats in the TXYF formula group were treated daily with orally administered TXYF formula (9.84 g/100 g body weight). The normal and NMS + RS groups were given distilled water. The delivery volume in each group was always 2 mL/100 g/d, for 14 consecutive days.
Rats were anesthetized abdominally with 7% chlorohydrate (35 mg/100 g body weight). The distal colon (6-7 cm from the anus) was quickly taken and incised longitudinally along the mesenteric border. Two longitudinal smooth muscle strips (0.8 cm × 0.2 cm) were obtained[15]. Specimens of intestinal muscle were ligatured with a medical thread at both ends. One end of the specimen was fixed to the bottom of the bath with the other connected to a physiological recorder through the tonotransducer. Specimens of the initial load was 1 g (2 mV) to maintain basic tension. Krebs solution (15 mL) was injected into the four baths at a temperature of 37 °C with consecutively circulating 95% oxygen and 5% CO2. The tissues were allowed to equilibrate for 60 min with fresh Krebs solution at 15-min intervals before the experiment[16].
Krebs solution had the following composition: 117 mmol/L NaCl, 4.7 mmol/L KCl, 1.2 mmol/L MgCl2, 24.8 mmol/L NaHCO3, 1.2 mmol/L KH2PO4, 2.56 mmol/L CaCl2 and 11.1 mmol/L glucose. 8-(N,N- diethylamino)octyl 3,4,5-trimethoxybenzoate hydrochloride (TMB-8), 4-aminopyridine (4-AP), nifedipine, apamin, N-ethylmaleimide (NEM), methylene blue, and NG-nitro-L-arginine methyl ester (L-NAME) were used. All of the reagents were purchased from Sigma-Aldrich (St Louis, MO, United States).
ML110 Powerlab amplifier, ML740 four-channel recorder, MLT02021D tonotransducer, and Power Lab/4sp analysis system for physiological data were all purchased from AD Instruments Shanghai Trading Co., Ltd (Pudong New Area, Shanghai, China).
All experimental data are expressed as mean ± SE. The changes before and after treatment were analyzed using one-way analysis of variance. The differences between groups were analyzed by comparing the values for each group using a paired t test. P < 0.05 was considered statistically significant.
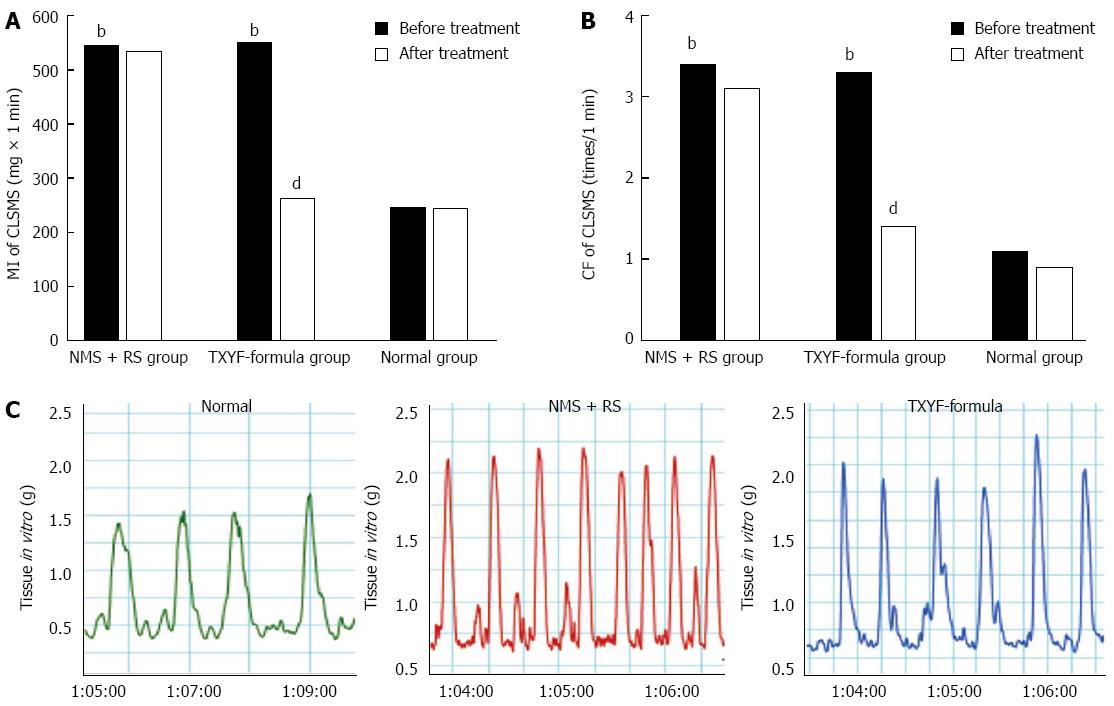
Under baseline conditions, the movement index (MI) of colonic longitudinal smooth muscle strips (CLSMs) in the NMS + RS and TXYF formula groups was similar and higher than that in the normal group (545.49 ± 73.66 mg/min and 551.09 ± 54.29 mg/min vs 245.76 ± 34.44 mg/min, n = 8, P < 0.01; Figure 1A). After treatment, MI in the TXYF formula group was lower than that in the NMS + RS group (261.39 ± 38.59 mg/min vs 533.9 ± 61.63 mg/min, n = 8, P < 0.01; Figure 1A) and similar to that in the normal group (261.39 ± 38.59 mg/min vs 244.78 ± 32.15 mg/min, n = 8, P = 0.365; Figure 1A).
The same result was seen for contraction frequency (CF) of CLSMs. Before treatment, CF in the NMS + RS and TXYF formula groups was similar and higher than that in the normal group (3.42 ± 0.25 times/min and 3.31 ± 0.21 times/min vs 1.1 ± 0.17 times/min, n = 8, P < 0.01; Figure 1B). After treatment, CF in the TXYF formula group was lower than that in the NMS + RS group (1.42 ± 0.87 times/min vs 3.11 ± 0.82 times/min, n = 8, P < 0.01; Figure 1B). After treatment, the CF in the TXYF formula group was lower than that in the NMS + RS group and close to that in the normal group.
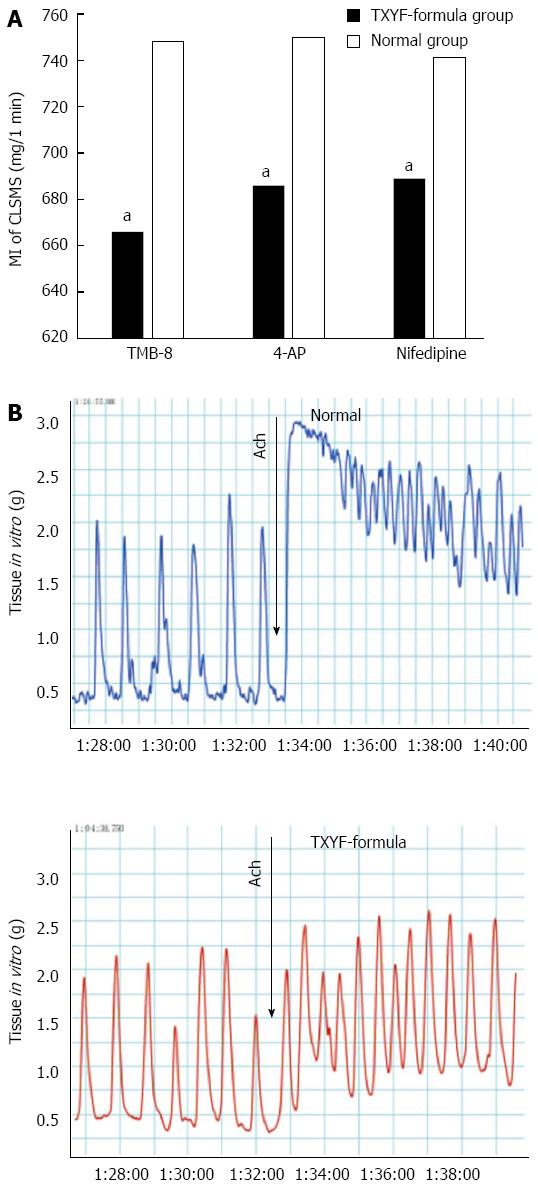
When TMB-8 was added to the bath and equilibrated for 30 min, and 10-4 mol/L Ach was added to CLSMs to induce muscle contraction, the MI of rat CLSMs in the TXYF formula group was lower than that in the normal group (666 ± 36.32 mg/min vs 747.77 ± 49.47 mg/min, n = 6, P < 0.05; Figure 2A and B). There were significant differences in MI of CLSMs between the TXYF formula and normal groups after treatment with 4-AP and nifedipine (686.53 ± 39.17 mg/min vs 750.45 ± 29.39 mg/min, and 689.48 ± 30.84 mg/min vs 741.65 ± 32.41 mg/min, n = 6, P < 0.05; Figure 2A).
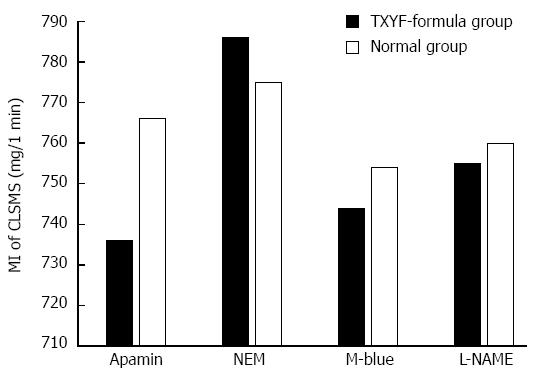
After treatment with apamin and NEM, MI of CLSMs in the TXYF formula and normal groups was similar (736.15 ± 32.41 mg/min vs 766.27 ± 32.41 mg/min, and 786.47 ± 32.11 mg/min vs 775.33 ± 35.93 mg/min, n = 6, P > 0.05, respectively; Figure 3). The MI of CLSMs in the TXYF formula and normal groups was similar after treatment with methylene blue and L-NAME (744.48 ± 37.75 mg/min vs 754.27 ± 27.69 mg/min, and 755.43 ± 36.15 mg/min vs 760.7 ± 33.08 mg/min, n = 6, P > 0.05, respectively; Figure 3).
Diarrhea, abdominal pain and discomfort are the primary clinical symptoms of D-IBS, whose etiology and pathogenesis are complex. Its pathophysiological changes mainly include abnormal gastrointestinal dynamic disorder and visceral sensory sensitivity[17,18]. In TCM, D-IBS belongs to diarrhea or abdominal pain, according to its clinical manifestation. Its main pathogenesis is stagnation of liver qi and spleen deficiency, disharmony between liver and spleen, and spleen deficiency wet-sheng[19].
The role of Bai zhu, in the TXYF formula, is Jian-Pi Hua-Shi (invigorating spleen and eliminating dampness), while Shao yao is Yang-Yin Rou-Gan (nourishing yin and soothing liver). Modern pharmacological studies have shown that they had an analgesic effect on visceral pain and an inhibitory effect on bowel movement[20,21]. The role of Chen pi, in the TXYF formula, is Li-Qi Xing-Pi (regulating qi-flowing and amusing spleen), and Fang feng is Qu-Shi Zhi-Tong (dispelling dampness and relieving pain). A previous pharmacological study has shown that Fang feng increases intestinal pressure threshold in rats so as to exert its analgesic effect[22]. In this study, we used the method of NMS combined with RS to establish an animal mode of D-IBS, with the main simultaneous symptoms of diarrhea and high visceral sensitivity. This recapitulates the clinical symptoms of patients with D-IBS.
Modern pharmacological studies have shown that TXYF formula has an inhibitory effect on bowel movement and reduces intestinal peristalsis[23,24]. One study has demonstrated that NMS upregulates L-type Ca2+ channel expression in the colon, which contributes to colonic motility disorder[25]. Yuan et al[26] have shown that TCYF inhibits the contraction of isolated rat colonic smooth muscle strips, mainly by preventing the influx of extracellular Ca2+.
In the present study, the contraction amplitude of CLSMs excited by Ach was lower in the TXYF formula group than in the normal group after incubation with nifedipine for 20 min. This indicated that the diastolic effect of TXYF-formula on CLSMs is probably achieved by inhibiting voltage dependent calcium channel and reducing intracellular Ca2+ concentration. After treatment with TMB-8 and 4-AP for 30 min, contraction amplitude of CLSMs induced by Ach in the TXYF formula group was lower than that in the normal group. This demonstrated that the inhibitory effects of TXYF formula on CLSM contraction might be achieved by means of: (1) inhibition of calcium release in intracellular sarcoplasmic reticulum, which results in a decrease of intracellular calcium concentration; and (2) activation of specific potassium channels.
In conclusion, TXYF formula inhibited the contraction of isolated CLSMs in rats with D-IBS. Its mechanism may be related to the activation of specific potassium channels, inhibition of extracellular calcium internal flow, and reduction of intracellular free Ca2 + concentration.
Diarrhea-predominant irritable bowel syndrome (D-IBS) is a chronic functional gastrointestinal disease. It seriously affects quality of life. The pathogenesis of D-IBS has not been fully clarified, although colon dysmotility is recognized as one of the pathophysiological factors. The usual treatment in Western medicine involves symptomatic therapy, which is unsatisfactory for patients, while simultaneously increasing the use of healthcare resources. Traditional Chinese medicine (TCM) can significantly improve symptoms and quality of life, so increasing numbers of patients have begun to seek treatment with TCM. Many clinical studies have shown that TongXie-YaoFang (TXYF) formula can significantly improve D-IBS clinical symptoms and enhance their quality of life.
TXYF formula is a classic Chinese herbal formula for clinical treatment of D-IBS. In the area of treatment of D-IBS with TXYF formula, the research hotspot is its effect on colon movement, visceral sensitivity, and correlational ion channels.
Previous correlational studies have shown that TXYF formula can affect bowel movement mostly through the observation of intestinal fecal propulsion in D-IBS rats using the method of short-term building. There have been few studies on contraction amplitude and frequency of colon tissues in vitro. The current view is that D-IBS is a chronic disease and related to early adverse life events. In the present study, the movement index (area under the curve of contraction intensity/min, mg/min) and contraction frequency (the number of contraction/min, times/min) of isolated colonic longitudinal smooth muscle strips were observed with a Power Lab system.
The study results suggest that TXYF formula can inhibit the contraction of rat colon, including the amplitude and frequency. This may be related to the activation of specific potassium channels and inhibition of extracellular calcium internal flow.
D-IBS is a chronic functional gastrointestinal disease and related to early adverse life events. It seriously affects quality of life. TXYF formula can inhibit contraction amplitude and frequency of colon tissues in vitro. This may be related to the activation of specific potassium channels and inhibition of extracellular calcium internal flow.
TXYF formula, a Chinese herbal formula, can effectively relieve diarrhea and lower visceral hypersensitivity of D-IBS rats mainly via inhibiting the contraction of the colonic longitudinal smooth muscle. This research shows that the mechanism may be related to the activation of specific potassium channels, inhibition of extracellular calcium internal flow and reduction of intracellular free Ca2+ concentration.
| 1. | Drossman DA. Introduction. The Rome Foundation and Rome III. Neurogastroenterol Motil. 2007;19:783-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Chey WY, Jin HO, Lee MH, Sun SW, Lee KY. Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea. Am J Gastroenterol. 2001;96:1499-1506. [PubMed] |
| 3. | Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 528] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 4. | Schönrich S, Brockow T, Franke T, Dembski R, Resch KL, Cieza A. Analyzing the content of outcome measures in clinical trials on irritable bowel syndrome using the international classification of functioning, disability and health as a reference. Rehabilitation (Stuttg). 2006;45:172-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Zhang SS, Zhou T, Wang HB. The status quo and challenges in traditional Chinese medicine diagnosis and treatment of Irritable bowel syndrome. Shijia Huaren Xiaohua Zazhi. 2010;18:2216-2220. |
| 6. | Zhang SS. Thinking and strategy on the diagnosis and treatment of functional gastrointestinal disorders with integrative medicine. Chin J Integr Med. 2009;15:83-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Wang G, Li TQ, Wang L, Xia Q, Chang J, Zhang Y, Wan MH, Guo J, Cheng Y, Huang X. Tong-xie-ning, a Chinese herbal formula, in treatment of diarrhea-predominant irritable bowel syndrome: a prospective, randomized, double-blind, placebo-controlled trial. Chin Med J (Engl). 2006;119:2114-2119. [PubMed] |
| 8. | Lai LJ, Han YC, Zhang H, Zhu XW, Hu XM. The timeliness of Tongxie-Yaofang on patients with D-IBS about improving the clinical symptoms. Shiyong Zhongxiyi Jiehe Linchuang. 2013;13:27-28. |
| 9. | Ren TH, Wu J, Yew D, Ziea E, Lao L, Leung WK, Berman B, Hu PJ, Sung JJ. Effects of neonatal maternal separation on neurochemical and sensory response to colonic distension in a rat model of irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2007;292:G849-G856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 93] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Gareau MG, Jury J, Perdue MH. Neonatal maternal separation of rat pups results in abnormal cholinergic regulation of epithelial permeability. Am J Physiol Gastrointest Liver Physiol. 2007;293:G198-G203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Yoshimoto S, Babygirija R, Dobner A, Ludwig K, Takahashi T. Anti-stress effects of transcutaneous electrical nerve stimulation (TENS) on colonic motility in rats. Dig Dis Sci. 2012;57:1213-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Green PG, Chen X, Alvarez P, Ferrari LF, Levine JD. Early-life stress produces muscle hyperalgesia and nociceptor sensitization in the adult rat. Pain. 2011;152:2549-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 13. | Xu JR, Luo JY, Shang L, Kong WM. Effect of change in an inhibitory neurotransmitter of the myenteric plexus on the pathogenetic mechanism of irritable bowel syndrome subgroups in rat models. Chin J Dig Dis. 2006;7:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Pharmacopoeia Commission of the Ministry of Public Health of PRC. Chinese Pharmacopoeia: Chemical Industry Press 2005; 55-56. |
| 15. | Xue H, Tian YM, Yan M, Yang N, Chen X, Xing Y, Zhu JX. Appearance of segmental discrepancy of anion transport in rat distal colon. Biol Pharm Bull. 2007;30:1407-1411. [PubMed] |
| 16. | Saito YA, Strege PR, Tester DJ, Locke GR, Talley NJ, Bernard CE, Rae JL, Makielski JC, Ackerman MJ, Farrugia G. Sodium channel mutation in irritable bowel syndrome: evidence for an ion channelopathy. Am J Physiol Gastrointest Liver Physiol. 2009;296:G211-G218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Rahimi R, Abdollahi M. Herbal medicines for the management of irritable bowel syndrome: a comprehensive review. World J Gastroenterol. 2012;18:589-600. [PubMed] [DOI] [Full Text] |
| 18. | Lan L, Chen YL, Zhang H, Jia BL, Chu YJ, Wang J, Tang SX, Xia GD. Efficacy of tandospirone in patients with irritable bowel syndrome-diarrhea and anxiety. World J Gastroenterol. 2014;20:11422-11428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Li L, Zhang SS. The mechanism research status in Irritable bowel syndrome with traditional Chinese medicine. Shiyong Zhongxiyi Jiehe Linchuang. 2012;20:466-470. |
| 20. | Zhang XJ, Li Z, Leung WM, Liu L, Xu HX, Bian ZX. The analgesic effect of paeoniflorin on neonatal maternal separation-induced visceral hyperalgesia in rats. J Pain. 2008;9:497-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Zhang XJ, Chen HL, Li Z, Zhang HQ, Xu HX, Sung JJ, Bian ZX. Analgesic effect of paeoniflorin in rats with neonatal maternal separation-induced visceral hyperalgesia is mediated through adenosine A(1) receptor by inhibiting the extracellular signal-regulated protein kinase (ERK) pathway. Pharmacol Biochem Behav. 2009;94:88-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Hu XG, Liao SL, Wang YF, Gong MJ, Wang M, Liu SS, Han B. Effect of Radix Saposhnikoviae in Tongxie Yaofang on PAR2 mRNA Expression and Inflammatory Mediators in the Colon of Rats with Postinfection Irritable Bowel Syndrome. Zhongyao Xinyao Yu Linchuang Yaoli. 2013;24:5-9. |
| 23. | Wei MX, Wu YM, Liu ZQ, Tian L. Effect and Mechanisms of Composition of Tongxie Yaofang on in vitro Contraction of Colonic Smooth Muscle Strips of Rat. Zhongguo Shiyan Fang Ji Xue Zazhi. 2010;16:131-134. |
| 24. | Pan F, Zhang T, Zhang YH, Xu JJ, Chen FM. Effect of Tongxie Yaofang Granule in treating diarrhea-predominate irritable bowel syndrome. Chin J Integr Med. 2009;15:216-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Zhang M, Leung FP, Huang Y, Bian ZX. Increased colonic motility in a rat model of irritable bowel syndrome is associated with up-regulation of L-type calcium channels in colonic smooth muscle cells. Neurogastroenterol Motil. 2010;22:e162-e170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Yuan JY, Xie JQ, Wu DZ, Zheng Y, Pan XX, Fei XY, Xu HZ. [Tongxie Yaofang inhibits the contraction of colonic smooth muscle isolated from rats through a mechanism related to calcium mobilization]. Zhong Xi Yi Jie He Xue Bao. 2009;7:958-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Luo HS S- Editor: Gou SX L- Editor: Wang TQ E- Editor: Zhang DN