Published online Jan 7, 2015. doi: 10.3748/wjg.v21.i1.84
Peer-review started: July 8, 2014
First decision: August 6, 2014
Revised: August 20, 2014
Accepted: October 14, 2014
Article in press: October 15, 2014
Published online: January 7, 2015
Processing time: 184 Days and 0.5 Hours
Colorectal cancer (CRC) is one of the most common malignancies with high prevalence and low 5-year survival. CRC is a heterogeneous disease with a complex, genetic and biochemical background. It is now generally accepted that a few important intracellular signaling pathways, including Wnt/β-catenin signaling, Ras signaling, and p53 signaling are frequently dysregulated in CRC. Patients with mutant p53 gene are often resistant to current therapies, conferring poor prognosis. Tumor suppressor p53 protein is a transcription factor inducing cell cycle arrest, senescence, and apoptosis under cellular stress. Emerging evidence from laboratories and clinical trials shows that some small molecule inhibitors exert anti-cancer effect via reactivation and restoration of p53 function. In this review, we summarize the p53 function and characterize its mutations in CRC. The involvement of p53 mutations in pathogenesis of CRC and their clinical impacts will be highlighted. Moreover, we also describe the current achievements of using p53 modulators to reactivate this pathway in CRC, which may have great potential as novel anti-cancer therapy.
Core tip: Dysregulation of p53 tumor suppressor gene is one of the most frequent events contributing to the transformation of colorectal cancer (CRC), as well as the aggressive and metastatic features of CRC. Mutant p53 reactivator, PRIMA-1MET has been tested in Phase I/II clinical trials and shows encouraging benefits. In this review, we systemically and comprehensively summarize the current understanding of p53 mutations in the pathogenesis of CRC and current progress in reactivation of p53 as a novel therapeutic strategy. We hope this review will promote more investigations of reactivation of p53 as a viable treatment option of patients with CRC.
-
Citation: Li XL, Zhou J, Chen ZR, Chng WJ.
p53 mutations in colorectal cancer- molecular pathogenesis and pharmacological reactivation. World J Gastroenterol 2015; 21(1): 84-93 - URL: https://www.wjgnet.com/1007-9327/full/v21/i1/84.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i1.84
Colorectal cancer (CRC) is the third most common cancer in men and the second most common cancer in women worldwide (http://http://www.wcrf.org). Although diagnosis and therapy have advanced significantly in the last ten years, its prevalence is rising, and the 5-year survival rate is still poor. In 2012, it accounts for nearly 14.1 million cases and 694000 deaths around the world (http://http://www.wcrf.org; http://www.who.int). CRC becomes a serious problem for healthcare in Asian countries too, such as China, Japan, South Korea and Singapore, with a 2-4 fold increase in the incidence during last decades[1]. So more efficacious approaches are urgently needed for CRC patients.
p53 was first discovered and classified as a cellular SV40 large T antigen-binding protein[2,3]. This finding marks the beginning of a brand-new period in cancer research that is expected to have a major impact in the clinic. p53 is a stress-inducible transcription factor, which regulates a large number of diverse downstream genes to exert regulative function in multiple signaling processes. p53 mutation occurs in approximately 40%-50% of sporadic CRC[4]. The status of p53 mutation is closely related to the progression and outcome of sporadic CRC. In recent years, some small molecule compounds have been intensively investigated for reactivation and restoration of p53 via different mechanisms. These promising compounds are being tested in clinical trials and may be approved for the treatment of CRC patients in near future.
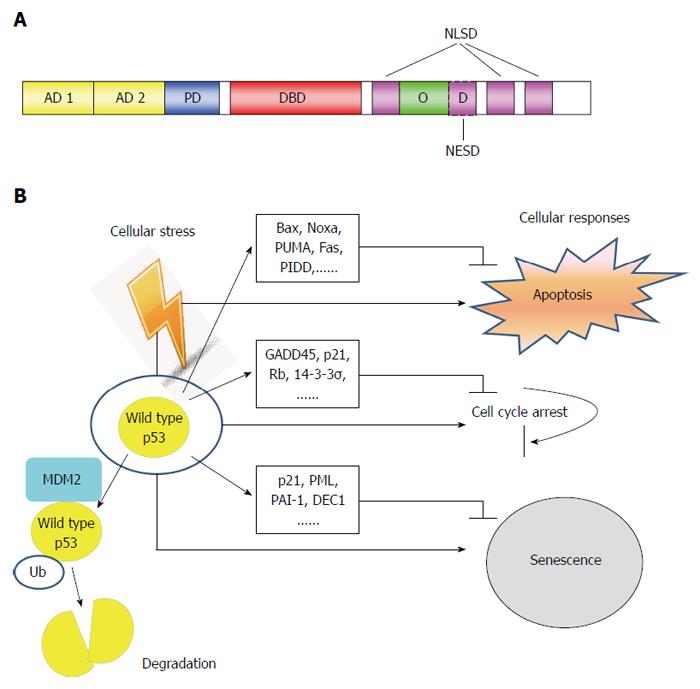
The human TP53 gene is located on chromosome 17p, and consists of 11 exons and 10 introns[5]. Wild type p53 protein consists of 393 amino acid residues, and several functional domains. In the order from N-terminus to C-terminus, they are: transactivation domain (TAD), proline-rich domain, tetramerization domain and basic domain (Figure 1A). Once activated, p53 upregulates its negative regulator, MDM2 (murine/human double minute 2). MDM2 functions as an E3 ubiquitin-ligase, to regulate the ubiquitination of p53 which leads to its degradation[6]. This forms a negative feedback loop that maintains low levels of p53 in normal cells[7]. Depending on specific context, p53 can induce cell cycle arrest, or apoptosis, or senescence, in the presence of cellular stress, such as DNA damage, hypoxia, oncogene activation, etc. (Figure 1B).
Activation of p53 can trigger both the mitochondrial (intrinsic) and the death-receptor-induced (extrinsic) apoptotic pathways[8]. p53 induces the expression of pro-apoptotic Bcl-2 (B-cell lymphoma-2) family proteins, mainly Bax, Noxa and PUMA, but downregulates the pro-survival Bcl-2, leading to permeabilization of outer mitochondrial membrane. Then cytochrome c releases from the mitochondria binds to Apaf-1, and induces the activation of the initiator caspase-9, eventually resulting in the activation of executioner caspase-3, -6 and -7[9]. On the other hand, activated p53 also upregulates the expression of some DRs (death receptors), such as Fas (CD95/APO-1), DR5 (TRAIL-R2), and PIDD (p53-induced protein with death domain). Together with caspase-8, they form the death-inducing signaling complex, subsequently activating caspase-3 and inducing apoptosis (Figure 1B). The progression of cell cycle is tightly controlled by cyclins and cyclin-dependent kinases (CDK). p21(WAF1) is one member of CDK inhibitor family, which hinder cell cycle transition from G1 to S phase. p21(WAF1) is a well-characterized p53-downstream gene and its promoter contains consensus p53-binding sequences. It has been shown that p21(WAF1) is one of the major mediator of p53-induced growth arrest. In response to DNA damage, p53 induces not only cell cycle G1 phase arrest, but also G2/M checkpoint arrest. Repression of CDC2, the CDK necessary for initiation of mitosis, by p53 plays an important role in G2/M arrest. Some other p53 target genes, for example, GADD45, p21(WAF1), retinoblastoma protein (Rb), and 14-3-3σ, also cRRIMA-1MET contribute to G2/M arrest. p21(WAF1) and Rb are involved in both G1 to S phase arrest and G2/M arrest induced by p53 (Figure 1B).
Cellular senescence is a specific form of cell cycle arrest, which is prolonged and irreversible[10]. Morphologically, senescence cells significantly increase in size and have prominent nucleoli, as well as abundant cytoplasmic vacuoles[11]. Cellular senescence is an important mechanism for preventing the development of potentially cancerous cells in response to stress-induced DNA damage[12]. Various stress stimuli including DNA-damage response, dysfunctional telomeres, oncogenes, oxidative stress, usually trigger one of the two pivotal routines, either the p53-p21(WAF1) or the p16 (CDKN2A)-Rb pathways to induce senescence[11,13]. In addition to p21(WAF1)[14], genes have been reported as important in p53-induced senescence include tumor suppressor promyelocytic leukemia (PML)[15,16], plasminogen activator inhibitor-1[17], and deleted in esophageal cancer 1 (DEC1)[18] (Figure 1B).
Activating transcription factor 3 (ATF3) is one of the p53 target genes and involved in the complicated process of cellular stress response[19,20]. In addition, ATF3 also acts as a co-transcripition factor for p53 achieving maximal induction of DR5 expression upon DNA damage in CRC[21]. DR5 is a trans-membrane TNF (tumor necrosis factor) receptor containing a death domain, which binds to the ligand TRAIL (tumor necrosis factor-related apoptosis-inducing ligand), and triggers cell death by activating the extrinsic apoptotic pathway[22]. Ectopic expression of ATF3 suppresses colon tumor growth and metastasisin mouse xenografts[23]. Post-translational modification of ATF3 by SUMO (small ubiquitin-related modifier) plays a negative role in the regulation of p53 activity[24]. ATF3 was also found to be bound to mutant p53, inactiving its oncogenic potential[25]. Of note, SUMO-1, a member of the SUMO protein family, involves a variety of biologically distinct functions through SUMO attachment of target proteins[26]. Over-expression of SUMO-1 causes the accumulation of sumoylated p53 proteins in colon cancer cells, which leads to more frequent metastasis[27].
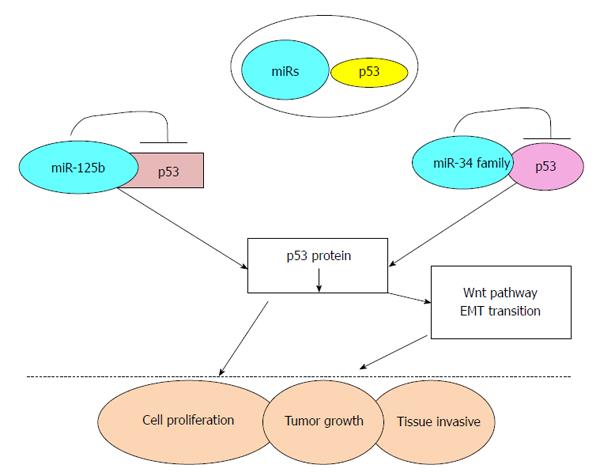
MicroRNA (miRs) are small non-coding RNA molecules consisting of 19-25 nucleotides, with functions in transcriptional and post-transcriptional regulation of gene expression[28]. miRs are believed to be important factors for cell proliferation, apoptosis, senescence and metabolism, which all play crucial role in the carcinogenic process[29]. For example, the high expression of miR-125b which directly targets the 3’UTR of TP53, repressed the endogenous level of p53 proteins, thereby promoting tumor growth and invasion. So, miR-125 acts as oncogene and is associated with the poor prognosis in CRC patients[30]. miR-125b had also been shown to repress both cell cycle-arrest and apoptotic regulators in the p53 network, implicating its role in oncogenesis[31,32] (Figure 2). Conversely, the miR-34 family (miR-34a/b/c) are transcriptional targets of p53[33], and directly suppresses a range of Wnt and epithelial-mesenchymal transition (EMT) genes[34-37]. Thus, part of p53 tumor suppressor function is due to its inhibition of Wnt pathway and EMT transition through miR-34 and loss of this inhibition could trigger the proliferation and tissue-invasion of CRC cells[34,35] (Figure 2).
Development of CRC is a multi-factorial and multi-stage process involving the activation of oncogenes and inactivation of tumor suppressor genes. Confirmed by numerous studies, p53 is a key tumor suppressor gene and is one of the most important elements of our body’s anticancer defense[38]. It is generally known that the progression of CRC follows mutations of the APC, K-Ras, and p53 genes[39]. p53 is the most commonly mutated gene in human cancers[40]. It is thought that p53 mutations play a critical role in the adenoma-carcinoma transition during tumorous pathological process[41]. p53 mutation in CRC occurs in 34% of the proximal colon tumors, and in 45% of the distal colorectal tumors[8,42]. Majority of these mutations occur in exon 5 to 8 (DNA binding doman), and mainly in some hotspot codons, such as 175, 245, 248, 273 and 282, comprising of G to A, C to T transition and leading to the substitution of a single amino acid in p53 protein[41,42] (Table 1). Such substitutions most commonly cluster in the DNA binding domain, causing the disruption of specific DNA binding and sequential transactivation[7,42].
| Exon | Codon | Codon change | Nucleotide change | Amino acid change |
| 5 | 175 | CGC→CAC | G→A | Arg→His |
| 7 | 245 | GGC→AGC | G→A | Gly→Ser |
| 7 | 245 | GGC→GAC | G→A | Gly→Asp |
| 7 | 248 | CGG→TGG | C→T | Arg→Trp |
| 7 | 248 | CGG→CAG | G→A | Arg→Gln |
| 8 | 273 | CGT→TGT | C→T | Arg→Cys |
| 8 | 273 | CGT→CAT | G→A | Arg→His |
| 8 | 282 | CGG→TGG | C→T | Arg→Trp |
Different types of p53 mutations play a pivotal role in determining the biologic behavior of CRC, such as invasive depth, metastatic site and even the prognosis of patients. p53 mutations are associated with lymphatic invasion in proximal colon cancer, and show significant correlation with both lymphatic and vascular invasion in distal CRC[42] (Table 2). CRC patients with mutant p53 appear more chemo-resistance and have poorer prognosis than those with wild-type p53[43]. In a TP53 colorectal cancer international collaborative study, it was observed that patients with mutant p53 in exon 5 had worse outcome for proximal colon cancer[42] and inactivating mutation of p53 occurred more frequent in advanced stage tumors and were negatively associated with survival[44] (Table 2).
| Ref. | Major conclusions |
| Taketani et al[21] | p53 partners with ATF3 in maximal induction of DR5 upon |
| DNA damage | |
| Wei et al[25] | ATF3 binds mutant p53 and inhibits its oncogenic function |
| Nishida et al[30] | High expression of miRNA-125b predicts poor survival in CRC. miRNA-125 decreases p53 expression |
| Kim et al[34,35] | Loss of p53 de-represses Wnt pathway and EMT transition through miRNA-34 |
| López et al[41] | p53 mutations occur in 54% of sporadic CRC |
| Russo et al[42] | p53 mutations correlate with the site, biologic behaviour and outcome of CRC |
| Iacopetta et al[44] | p53 mutations that lose transactivational ability are more common in advanced CRC and associated with poor survival |
Results from a large number of studies have unequivocally evidence demonstrated that mutant p53 not only plays a pivotal role in the transformation of CRC, but also contributes to the aggressiveness and invasiveness of CRC. It is not surprising that manipulation of the p53 pathway has attracted interest soon after the discovery of p53 gene. Although reintroduction of wild type p53 by gene therapy appears a straightforward and logical choice, this approached is impeded by the technical challenge of efficient gene delivery and safety issues inherent in the use of viral vectors[45]. In recent years, we witness an array of small molecule inhibitors modulating the p53 pathway being developed (Figure 3). Some of these compounds have been tested as potential therapeutic agents in CRC.
MDM2 protein, the E3 ubiquitin protein ligase, binds to the amino-terminal of p53, and ubiquitylates p53, leading to its proteasomal degradiaiton; this inhibits its suppressive function in cancer cells[46]. Pharmacological inhibitors of MDM2 have already been extensively researched for their anti-cancer activities through stabilization of p53 protein[47-49]. Activation of p53 without DNA damage should be a great advantage, compared to many traditional chemotherapeutic agents[47].
MIs (MDM2 Inhibitors): In recent years, a number of MIs that disrupt the MDM2-p53 interaction have been discovered. The spiro oxindole MI-43 is one of these specific MDM2 antagonists that cause p53 accumulation and lead to the induction of target genes, e.g., p21, Puma, and Noxa[50]. In colon cancer cells, cell cycle arrest and apoptosis were induced by MI-43 in a p53-dependent manner[51]. MI-219 is an improved MDM2-p53 inhibitor with improved pharmacokinetic profile and higher binding affinity to MDM2. MI-219 showed potent efficacy as a single agent in inducing apoptosis in HCT-116 colon cancer cell line. Furthermore, the combination of MI-219 with chemotherapeutic drug, Oxaliplatin, achieved high synergism in p53-mediated apoptotic response[52].
Nutlins: Nutlins are cis-imidazoline analogs, which occupy the binding pocket of MDM2, thus disrupting MDM2-p53 interaction. Nutlins were first discovered using biochemical screening strategy by Vassilev and colleagues in Roche in 2004[53]. Among them, Nutlin-3 (R1772) has been widely tested in a variety of cancers in vitro, in mouse xenografts bearing human tumors, as well as clinical trials in human subjects[54]. Nutlin-3 was observed to act as MDM2 antagonist, stabilize p53 and activate p53 target genes in CRC cells expressing wild-type p53. MDMX, another member of MDM protein family, shares a similar amino acid sequence and structural organization with MDM2. Although both MDM2 and MDMX negatively regulate p53, the relative abundance of MDM2 and MDMX level influences cancer cells response to Nutlin-3. Cancer cells overexpressing MDM2 are sensitive to Nutlin-3, in contrast, cancer cells overexpressing MDMX are resistant to Nutlin-3 due to its inability to block p53-MDMX interaction[55]. Nutlin-3a, but not the aftermentioned RIAT (reactivation of p53 and induction of tumor cell apoptosis), has been shown to specifically downregulate α5 integrin in p53 wild type colon cancer[56]. These findings are useful in patient selection in a clinical trial aiming to evaluate Nutlin-3 against CRC. Nutlin may offer clinical benefits for CRC bearing high expression MDM2 or α5 integrin.
Cancer cells often acquire secondary resistance after a prolonged exposure of single agent, so it is clinically desirable to treatment the cancer patients with combination therapy. Nutlin has been tested in combination with other drugs in CRC. Tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL) is one of the DNA damage-inducible p53 target gene[57]. Notably, TRAIL induces cell death mainly through the induction of extrinsic apoptosis pathway, while Nutlin works predominately through inducing the intrinsic apoptosis pathway. Combination of Nutlin-3 and TRAIL synergistically enhances cell death in human p53 wild type sarcoma HOS cells and colon cancer HCT116 cells owing to the simultaneous engagement of intrinsic and extrinsic apoptosis pathways[58]. Furthermore, Nutlin-3 treatment increases DR5 expression on both mRNA and protein levels[58,59]. Controlled, concomitant release of Nutlin-3 and Doxil, the liposomal preparation of doxorubicin, by novel drug engineering, leads to synergistic anti-proliferative effect and induction of cell death in CRC cells carrying both wild-type and mutant p53[60]. Combination treatment with Nutlin-3 and Inauhzin, a SIRT1 (Sirtuin 1) inhibitor in colon and lung cancer cell lines, is able to enhances their apoptotic effect in a p53-dependent manner[61]. It is also noteworthy that Nutlin-3 can mediate the phosphorylation of p53 at key DNA-damage-specific serine residues (Ser15, 20 and 37) and initiate the DNA damage signaling pathway which resulted in cell cycle arrest in p53-independent manner[62]. Currently, Nutlin-3 has already been evaluated in phase I clinical trial to treat patients suffering from hematologic neoplasms[63]. Taken together, Nutlin-3 may be a helpful addition to our armamentarium combating CRC, particularly used in conjunction with other drugs.
RITA: RITA was identified from National Cancer Institute library compound Challenge set for its ability to inhibit the proliferation of HCT-116 (p53 wild type) much more than its p53 null counterpart[64]. RITA has been shown to suppress colon cancer growth in a mouse xenofgraft model. Mechanically, this compound directly binds to p53 rather than MDM2, and induces a conformational change in p53, which interfered with the p53-MDM2 interaction, and p53 ubiquitination, resulting in p53 accumulation and cellular apoptosis[64,65]. The study carried out by Di Marzo et al[66] implicated that RITA also reactivated mutant p53 function in malignant mesothelioma. Whether RITA is also effective in CRC cells harboring mutant p53 would merit further investigation.
In addition to p53, the p53 family includes two other members, p63 and p73[67]. They encode proteins with significant sequence homology and functional similarity with p53. A derivative of the cytotoxic plant alkaloid ellipticine, NSC176327 induced potent killing in CRC cells regardless of p53 status. Further experiments revealed that NSC176327 treatment increased the expression of p73, p21 and DR5, while knockdown of p73 in p53 null cells rendered these cells resistant to this drug treatment[68]. The notion that p73 is also a drug target in CRC is reinforced by other studies. Ray et al[69] reported that MDM2 inhibitors, like Nutlin-3 , could also disrupt the MDM2-p73 binding, and induce the expression of apoptotic proteins such as Noxa, PUMA and cell cycle arrest protein p21 in CRC cells lacking of functional p53[70]. Securinine, a widely used alkaloid, was identified to promote p73-dependent apoptosis in p53-deficent CRC cells[71]. In conclusion, these results shed new light on the induction of p73 as a therapeutic option in CRC patients with either mutant p53 or p53 null.
It has been long recognized that mutant p53 protein not only abrogates the tumor suppressor function, but also gain novel oncogenic function, which promotes a more aggressive, metastatic cancer phenotype. However, it is until recently that promising compounds that specifically targeting this type of mutant oncogenic p53 proteins have been developed. Aiming to screen compounds that specifically targeting mutant p53, Bykov et al[72] discovered one compound 2,2-bis(hydroxymethyl)-1-azabicyclo[2,2,2]octan -3-one, which inhibited the growth of Saos-2-His-273 cells, a Tet-off mutant p53 cell line. This compound was named PRIMA-1 (p53-reactivation and induction of massive apoptosis-1, APR-017)[72]. Late, its methylated form, RRIMA-1MET (APR-246) which is more efficient, was developed by the same group[73]. PRIMA-1 restores the sequence-specific DNA binding region via forming adducts with thiols in mutant p53 and activating several p53 target genes, promoting apoptosis in human cancer cells with mutant p53[74]. The initial consideration was that these two compounds had potent effects on p53-mutant cells, compared to cells with wild-type p53. However, emerging evidence demonstrated that unfolded mutant p53 and unfolded wild-type p53 could also be refolded by PRIMA-1 and PRIMA-1MET[74,75]. So PRIMA-1 and PRIMA-1MET may induce apoptosis in cancer cells carrying either wild-type p53 or mutant p53. Among the class of small molecules that can selectively induce apoptosis in cancer cells with mutant p53, PRIMA-1MET is the first drug which has already advanced to a phase I/II clinical trial for hematologic malignancies and prostate cancer[76,77]. However, there is little investigation about the ability of PRIMA-1MET to induce apoptosis and inhibit tumor growth in different CRC cell lines with different p53 status, thus, more studies are necessary to intensively explore RRIMA-1MET as a novel therapeutic strategy in CRC.
Recently, the anticancer function of agents extracted from nature plants is attracting some attention. The mechanisms implicated have been uncovered constantly.
Maslinic acid: Maslinic acid (MA) is a natural triterpene from Olea europaea, and possesses potent anticancer property aganist CRC cells. Exposure to MA induced the expression of JNK (c-Jun NH2-terminal kinase), p53, and increased the mitochondrial apoptotic signaling molecules, resulting in cell cycle arrest and apoptosis[78,79]. In p53-deficient CRC cells, apoptosis could also be induced by MA without requiring the mitochondrial pathway[80].
Epicatechin gallate: Experimental and epidemiological evidences reveal that dietary polyphenolic plant-derived compounds have anti-proliferative and anti-invasive activity in cancers of gastrointestinal tract, lung, skin, prostate and breast[81-83]. Epicatechin gallate (ECG) is one of the most important compounds of polyphenols found in green tea, which stimulated the expression of p53, p21, and MAPKs (mitogen-activated protein kinases) in CRC cells, leading to cell cycle arrest at G0/G1-S phase in a time-dependent manner[82]. Furthermore, ECG could inhibit the degradation of p53 protein and RNA that contributed to the stabilization of p53.
p53 proteins can be targeted for proteasomal degradation in both normal and cancer cells. α - Lipoic acid (α-LA) is the most common drug worldwide to treat diabetic polyneuropathy. Yoo and colleagues had shown α-LA inhibited proliferation and induced apoptosis in colon cancer cells via preventing p53 degradation. Specifically, α-LA treatment downregulated ribosomal protein p90S6K (RPS6KA4) which was confirmed to inhibit p53 function. Furthermore, α-LA exerted an inhibitory effect on the nuclear translocation of nuclear factor-κB (NF-κB), which played an important role in regulating RPS6KA4 gene expression[84].
There is no doubt that reactivation and restoration of p53 function have great potential as a novel therapeutic strategy in CRC. However, the majority of molecules that lead to cell cycle arrest and apoptosis in CRC cells, has only been tested in cell lines and animal models, and has yet to enter in clinical trials. In addition, it is clear that mutant p53 promotes various oncogenic events. Nevertheless, the critical mechanisms are still not completely understood. The issue that different mutations might affect p53 function differently makes small molecule inhibitors targeting mutant p53 more complicated to assess in a clinical trial. This theme needs to be explored further. Importantly, resistance to treatments and poor prognosis for CRC patients with new p53 mutations will require the continuing development of new agent targeting these novel mutations. Riding on the last 30 years of intensive research in p53 area, this is now the time to harvest the fruits from this body of work and translate our knowledge of p53 into clinical practice for CRC patients.
| 1. | Moghimi-Dehkordi B, Safaee A. An overview of colorectal cancer survival rates and prognosis in Asia. World J Gastrointest Oncol. 2012;4:71-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 102] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (9)] |
| 2. | Farnebo M, Bykov VJ, Wiman KG. The p53 tumor suppressor: a master regulator of diverse cellular processes and therapeutic target in cancer. Biochem Biophys Res Commun. 2010;396:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 194] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 3. | Tan TH, Wallis J, Levine AJ. Identification of the p53 protein domain involved in formation of the simian virus 40 large T-antigen-p53 protein complex. J Virol. 1986;59:574-583. [PubMed] |
| 4. | Takayama T, Miyanishi K, Hayashi T, Sato Y, Niitsu Y. Colorectal cancer: genetics of development and metastasis. J Gastroenterol. 2006;41:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 172] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Saha MN, Qiu L, Chang H. Targeting p53 by small molecules in hematological malignancies. J Hematol Oncol. 2013;6:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Li Q, Lozano G. Molecular pathways: targeting Mdm2 and Mdm4 in cancer therapy. Clin Cancer Res. 2013;19:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 155] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 7. | Zandi R, Selivanova G, Christensen CL, Gerds TA, Willumsen BM, Poulsen HS. PRIMA-1Met/APR-246 induces apoptosis and tumor growth delay in small cell lung cancer expressing mutant p53. Clin Cancer Res. 2011;17:2830-2841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Ryan KM, Phillips AC, Vousden KH. Regulation and function of the p53 tumor suppressor protein. Curr Opin Cell Biol. 2001;13:332-337. [PubMed] |
| 9. | Shen J, Vakifahmetoglu H, Stridh H, Zhivotovsky B, Wiman KG. PRIMA-1MET induces mitochondrial apoptosis through activation of caspase-2. Oncogene. 2008;27:6571-6580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Salama R, Sadaie M, Hoare M, Narita M. Cellular senescence and its effector programs. Genes Dev. 2014;28:99-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 609] [Cited by in RCA: 689] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 11. | Campisi J, d’Adda di Fagagna F. Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol. 2007;8:729-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2834] [Cited by in RCA: 3322] [Article Influence: 174.8] [Reference Citation Analysis (0)] |
| 12. | Mallette FA, Ferbeyre G. The DNA damage signaling pathway connects oncogenic stress to cellular senescence. Cell Cycle. 2007;6:1831-1836. [PubMed] |
| 13. | Shay JW, Pereira-Smith OM, Wright WE. A role for both RB and p53 in the regulation of human cellular senescence. Exp Cell Res. 1991;196:33-39. [PubMed] |
| 14. | Noda A, Ning Y, Venable SF, Pereira-Smith OM, Smith JR. Cloning of senescent cell-derived inhibitors of DNA synthesis using an expression screen. Exp Cell Res. 1994;211:90-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 983] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 15. | Ferbeyre G, de Stanchina E, Querido E, Baptiste N, Prives C, Lowe SW. PML is induced by oncogenic ras and promotes premature senescence. Genes Dev. 2000;14:2015-2027. [PubMed] |
| 16. | Pearson M, Carbone R, Sebastiani C, Cioce M, Fagioli M, Saito S, Higashimoto Y, Appella E, Minucci S, Pandolfi PP. PML regulates p53 acetylation and premature senescence induced by oncogenic Ras. Nature. 2000;406:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 542] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 17. | Kortlever RM, Higgins PJ, Bernards R. Plasminogen activator inhibitor-1 is a critical downstream target of p53 in the induction of replicative senescence. Nat Cell Biol. 2006;8:877-884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 460] [Cited by in RCA: 469] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 18. | Qian Y, Zhang J, Yan B, Chen X. DEC1, a basic helix-loop-helix transcription factor and a novel target gene of the p53 family, mediates p53-dependent premature senescence. J Biol Chem. 2008;283:2896-2905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Zhang C, Gao C, Kawauchi J, Hashimoto Y, Tsuchida N, Kitajima S. Transcriptional activation of the human stress-inducible transcriptional repressor ATF3 gene promoter by p53. Biochem Biophys Res Commun. 2002;297:1302-1310. [PubMed] |
| 20. | Kannan K, Amariglio N, Rechavi G, Jakob-Hirsch J, Kela I, Kaminski N, Getz G, Domany E, Givol D. DNA microarrays identification of primary and secondary target genes regulated by p53. Oncogene. 2001;20:2225-2234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 255] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 21. | Taketani K, Kawauchi J, Tanaka-Okamoto M, Ishizaki H, Tanaka Y, Sakai T, Miyoshi J, Maehara Y, Kitajima S. Key role of ATF3 in p53-dependent DR5 induction upon DNA damage of human colon cancer cells. Oncogene. 2012;31:2210-2221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 22. | MacFarlane M, Ahmad M, Srinivasula SM, Fernandes-Alnemri T, Cohen GM, Alnemri ES. Identification and molecular cloning of two novel receptors for the cytotoxic ligand TRAIL. J Biol Chem. 1997;272:25417-25420. [PubMed] |
| 23. | Hackl C, Lang SA, Moser C, Mori A, Fichtner-Feigl S, Hellerbrand C, Dietmeier W, Schlitt HJ, Geissler EK, Stoeltzing O. Activating transcription factor-3 (ATF3) functions as a tumor suppressor in colon cancer and is up-regulated upon heat-shock protein 90 (Hsp90) inhibition. BMC Cancer. 2010;10:668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Wang CM, Brennan VC, Gutierrez NM, Wang X, Wang L, Yang WH. SUMOylation of ATF3 alters its transcriptional activity on regulation of TP53 gene. J Cell Biochem. 2013;114:589-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Wei S, Wang H, Lu C, Malmut S, Zhang J, Ren S, Yu G, Wang W, Tang DD, Yan C. The activating transcription factor 3 protein suppresses the oncogenic function of mutant p53 proteins. J Biol Chem. 2014;289:8947-8959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Barry J, Lock RB. Small ubiquitin-related modifier-1: Wrestling with protein regulation. Int J Biochem Cell Biol. 2011;43:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Zhang H, Kuai X, Ji Z, Li Z, Shi R. Over-expression of small ubiquitin-related modifier-1 and sumoylated p53 in colon cancer. Cell Biochem Biophys. 2013;67:1081-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Bi CL, Chng WJ. miRNA deregulation in multiple myeloma. Chin Med J (Engl). 2011;124:3164-3169. [PubMed] |
| 29. | Ye JJ, Cao J. MicroRNAs in colorectal cancer as markers and targets: Recent advances. World J Gastroenterol. 2014;20:4288-4299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Nishida N, Yokobori T, Mimori K, Sudo T, Tanaka F, Shibata K, Ishii H, Doki Y, Kuwano H, Mori M. MicroRNA miR-125b is a prognostic marker in human colorectal cancer. Int J Oncol. 2011;38:1437-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Le MT, Shyh-Chang N, Khaw SL, Chin L, Teh C, Tay J, O’Day E, Korzh V, Yang H, Lal A. Conserved regulation of p53 network dosage by microRNA-125b occurs through evolving miRNA-target gene pairs. PLoS Genet. 2011;7:e1002242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 132] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 32. | Kumar M, Lu Z, Takwi AA, Chen W, Callander NS, Ramos KS, Young KH, Li Y. Negative regulation of the tumor suppressor p53 gene by microRNAs. Oncogene. 2011;30:843-853. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 222] [Cited by in RCA: 218] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 33. | He L, He X, Lim LP, de Stanchina E, Xuan Z, Liang Y, Xue W, Zender L, Magnus J, Ridzon D. A microRNA component of the p53 tumour suppressor network. Nature. 2007;447:1130-1134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2135] [Cited by in RCA: 2117] [Article Influence: 111.4] [Reference Citation Analysis (0)] |
| 34. | Kim NH, Kim HS, Kim NG, Lee I, Choi HS, Li XY, Kang SE, Cha SY, Ryu JK, Na JM. p53 and microRNA-34 are suppressors of canonical Wnt signaling. Sci Signal. 2011;4:ra71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 248] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 35. | Kim NH, Cha YH, Kang SE, Lee Y, Lee I, Cha SY, Ryu JK, Na JM, Park C, Yoon HG. p53 regulates nuclear GSK-3 levels through miR-34-mediated Axin2 suppression in colorectal cancer cells. Cell Cycle. 2013;12:1578-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 36. | Cha YH, Kim NH, Park C, Lee I, Kim HS, Yook JI. MiRNA-34 intrinsically links p53 tumor suppressor and Wnt signaling. Cell Cycle. 2012;11:1273-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 37. | Siemens H, Jackstadt R, Hünten S, Kaller M, Menssen A, Götz U, Hermeking H. miR-34 and SNAIL form a double-negative feedback loop to regulate epithelial-mesenchymal transitions. Cell Cycle. 2011;10:4256-4271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 487] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 38. | Levine AJ, Oren M. The first 30 years of p53: growing ever more complex. Nat Rev Cancer. 2009;9:749-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1292] [Cited by in RCA: 1468] [Article Influence: 86.4] [Reference Citation Analysis (0)] |
| 39. | Cottu PH, Muzeau F, Estreicher A, Fléjou JF, Iggo R, Thomas G, Hamelin R. Inverse correlation between RER+ status and p53 mutation in colorectal cancer cell lines. Oncogene. 1996;13:2727-2730. [PubMed] |
| 40. | Kandoth C, McLellan MD, Vandin F, Ye K, Niu B, Lu C, Xie M, Zhang Q, McMichael JF, Wyczalkowski MA. Mutational landscape and significance across 12 major cancer types. Nature. 2013;502:333-339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2931] [Cited by in RCA: 3463] [Article Influence: 266.4] [Reference Citation Analysis (0)] |
| 41. | López I, P Oliveira L, Tucci P, Alvarez-Valín F, A Coudry R, Marín M. Different mutation profiles associated to P53 accumulation in colorectal cancer. Gene. 2012;499:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 42. | Russo A, Bazan V, Iacopetta B, Kerr D, Soussi T, Gebbia N. The TP53 colorectal cancer international collaborative study on the prognostic and predictive significance of p53 mutation: influence of tumor site, type of mutation, and adjuvant treatment. J Clin Oncol. 2005;23:7518-7528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 305] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 43. | Iacopetta B. TP53 mutation in colorectal cancer. Hum Mutat. 2003;21:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 242] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 44. | Iacopetta B, Russo A, Bazan V, Dardanoni G, Gebbia N, Soussi T, Kerr D, Elsaleh H, Soong R, Kandioler D. Functional categories of TP53 mutation in colorectal cancer: results of an International Collaborative Study. Ann Oncol. 2006;17:842-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 45. | Lane DP, Cheok CF, Lain S. p53-based cancer therapy. Cold Spring Harb Perspect Biol. 2010;2:a001222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 175] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 46. | Micel LN, Tentler JJ, Smith PG, Eckhardt GS. Role of ubiquitin ligases and the proteasome in oncogenesis: novel targets for anticancer therapies. J Clin Oncol. 2013;31:1231-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 152] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 47. | Rigatti MJ, Verma R, Belinsky GS, Rosenberg DW, Giardina C. Pharmacological inhibition of Mdm2 triggers growth arrest and promotes DNA breakage in mouse colon tumors and human colon cancer cells. Mol Carcinog. 2012;51:363-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 48. | Patel S, Player MR. Small-molecule inhibitors of the p53-HDM2 interaction for the treatment of cancer. Expert Opin Investig Drugs. 2008;17:1865-1882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 49. | Vassilev LT. MDM2 inhibitors for cancer therapy. Trends Mol Med. 2007;13:23-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 389] [Cited by in RCA: 414] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 50. | Sun SH, Zheng M, Ding K, Wang S, Sun Y. A small molecule that disrupts Mdm2-p53 binding activates p53, induces apoptosis and sensitizes lung cancer cells to chemotherapy. Cancer Biol Ther. 2008;7:845-852. [PubMed] |
| 51. | Shangary S, Ding K, Qiu S, Nikolovska-Coleska Z, Bauer JA, Liu M, Wang G, Lu Y, McEachern D, Bernard D. Reactivation of p53 by a specific MDM2 antagonist (MI-43) leads to p21-mediated cell cycle arrest and selective cell death in colon cancer. Mol Cancer Ther. 2008;7:1533-1542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 52. | Azmi AS, Banerjee S, Ali S, Wang Z, Bao B, Beck FW, Maitah M, Choi M, Shields TF, Philip PA. Network modeling of MDM2 inhibitor-oxaliplatin combination reveals biological synergy in wt-p53 solid tumors. Oncotarget. 2011;2:378-392. [PubMed] |
| 53. | Vassilev LT, Vu BT, Graves B, Carvajal D, Podlaski F, Filipovic Z, Kong N, Kammlott U, Lukacs C, Klein C. In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science. 2004;303:844-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3508] [Cited by in RCA: 3720] [Article Influence: 169.1] [Reference Citation Analysis (0)] |
| 54. | Shen H, Maki CG. Pharmacologic activation of p53 by small-molecule MDM2 antagonists. Curr Pharm Des. 2011;17:560-568. [PubMed] |
| 55. | Patton JT, Mayo LD, Singhi AD, Gudkov AV, Stark GR, Jackson MW. Levels of HdmX expression dictate the sensitivity of normal and transformed cells to Nutlin-3. Cancer Res. 2006;66:3169-3176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 151] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 56. | Janouskova H, Ray AM, Noulet F, Lelong-Rebel I, Choulier L, Schaffner F, Lehmann M, Martin S, Teisinger J, Dontenwill M. Activation of p53 pathway by Nutlin-3a inhibits the expression of the therapeutic target α5 integrin in colon cancer cells. Cancer Lett. 2013;336:307-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 57. | Wu GS, Burns TF, McDonald ER, Jiang W, Meng R, Krantz ID, Kao G, Gan DD, Zhou JY, Muschel R. KILLER/DR5 is a DNA damage-inducible p53-regulated death receptor gene. Nat Genet. 1997;17:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 762] [Cited by in RCA: 755] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 58. | Hori T, Kondo T, Kanamori M, Tabuchi Y, Ogawa R, Zhao QL, Ahmed K, Yasuda T, Seki S, Suzuki K. Nutlin-3 enhances tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis through up-regulation of death receptor 5 (DR5) in human sarcoma HOS cells and human colon cancer HCT116 cells. Cancer Lett. 2010;287:98-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 59. | Meijer A, Kruyt FA, van der Zee AG, Hollema H, Le P, ten Hoor KA, Groothuis GM, Quax WJ, de Vries EG, de Jong S. Nutlin-3 preferentially sensitises wild-type p53-expressing cancer cells to DR5-selective TRAIL over rhTRAIL. Br J Cancer. 2013;109:2685-2695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 60. | Nadler-Milbauer M, Apter L, Haupt Y, Haupt S, Barenholz Y, Minko T, Rubinstein A. Synchronized release of Doxil and Nutlin-3 by remote degradation of polysaccharide matrices and its possible use in the local treatment of colorectal cancer. J Drug Target. 2011;19:859-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Zhang Y, Zhang Q, Zeng SX, Zhang Y, Mayo LD, Lu H. Inauhzin and Nutlin3 synergistically activate p53 and suppress tumor growth. Cancer Biol Ther. 2012;13:915-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 62. | Valentine JM, Kumar S, Moumen A. A p53-independent role for the MDM2 antagonist Nutlin-3 in DNA damage response initiation. BMC Cancer. 2011;11:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 63. | Chen F, Wang W, El-Deiry WS. Current strategies to target p53 in cancer. Biochem Pharmacol. 2010;80:724-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 64. | Issaeva N, Bozko P, Enge M, Protopopova M, Verhoef LG, Masucci M, Pramanik A, Selivanova G. Small molecule RITA binds to p53, blocks p53-HDM-2 interaction and activates p53 function in tumors. Nat Med. 2004;10:1321-1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 571] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 65. | Essmann F, Schulze-Osthoff K. Translational approaches targeting the p53 pathway for anti-cancer therapy. Br J Pharmacol. 2012;165:328-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 66. | Di Marzo D, Forte IM, Indovina P, Di Gennaro E, Rizzo V, Giorgi F, Mattioli E, Iannuzzi CA, Budillon A, Giordano A. Pharmacological targeting of p53 through RITA is an effective antitumoral strategy for malignant pleural mesothelioma. Cell Cycle. 2014;13:652-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 67. | Damia G, Broggini M. Cell cycle checkpoint proteins and cellular response to treatment by anticancer agents. Cell Cycle. 2004;3:46-50. [PubMed] |
| 68. | Lu C, Wang W, El-Deiry WS. Non-genotoxic anti-neoplastic effects of ellipticine derivative NSC176327 in p53-deficient human colon carcinoma cells involve stimulation of p73. Cancer Biol Ther. 2008;7:2039-2046. [PubMed] |
| 69. | Ray RM, Bhattacharya S, Johnson LR. Mdm2 inhibition induces apoptosis in p53 deficient human colon cancer cells by activating p73- and E2F1-mediated expression of PUMA and Siva-1. Apoptosis. 2011;16:35-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 70. | Hong B, Prabhu VV, Zhang S, van den Heuvel AP, Dicker DT, Kopelovich L, El-Deiry WS. Prodigiosin rescues deficient p53 signaling and antitumor effects via upregulating p73 and disrupting its interaction with mutant p53. Cancer Res. 2014;74:1153-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 71. | Rana S, Gupta K, Gomez J, Matsuyama S, Chakrabarti A, Agarwal ML, Agarwal A, Agarwal MK, Wald DN. Securinine induces p73-dependent apoptosis preferentially in p53-deficient colon cancer cells. FASEB J. 2010;24:2126-2134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 72. | Bykov VJ, Issaeva N, Shilov A, Hultcrantz M, Pugacheva E, Chumakov P, Bergman J, Wiman KG, Selivanova G. Restoration of the tumor suppressor function to mutant p53 by a low-molecular-weight compound. Nat Med. 2002;8:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 805] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 73. | Bykov VJ, Zache N, Stridh H, Westman J, Bergman J, Selivanova G, Wiman KG. PRIMA-1(MET) synergizes with cisplatin to induce tumor cell apoptosis. Oncogene. 2005;24:3484-3491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 198] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 74. | Lambert JM, Gorzov P, Veprintsev DB, Söderqvist M, Segerbäck D, Bergman J, Fersht AR, Hainaut P, Wiman KG, Bykov VJ. PRIMA-1 reactivates mutant p53 by covalent binding to the core domain. Cancer Cell. 2009;15:376-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 473] [Cited by in RCA: 467] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 75. | Rieber M, Strasberg-Rieber M. Hypoxia, Mn-SOD and H(2)O(2) regulate p53 reactivation and PRIMA-1 toxicity irrespective of p53 status in human breast cancer cells. Biochem Pharmacol. 2012;84:1563-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 76. | Cheok CF, Verma CS, Baselga J, Lane DP. Translating p53 into the clinic. Nat Rev Clin Oncol. 2011;8:25-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 295] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 77. | Lehmann S, Bykov VJ, Ali D, Andrén O, Cherif H, Tidefelt U, Uggla B, Yachnin J, Juliusson G, Moshfegh A. Targeting p53 in vivo: a first-in-human study with p53-targeting compound APR-246 in refractory hematologic malignancies and prostate cancer. J Clin Oncol. 2012;30:3633-3639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 306] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 78. | Rufino-Palomares EE, Reyes-Zurita FJ, García-Salguero L, Mokhtari K, Medina PP, Lupiáñez JA, Peragón J. Maslinic acid, a triterpenic anti-tumoural agent, interferes with cytoskeleton protein expression in HT29 human colon-cancer cells. J Proteomics. 2013;83:15-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 79. | Reyes-Zurita FJ, Pachón-Peña G, Lizárraga D, Rufino-Palomares EE, Cascante M, Lupiáñez JA. The natural triterpene maslinic acid induces apoptosis in HT29 colon cancer cells by a JNK-p53-dependent mechanism. BMC Cancer. 2011;11:154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 80. | Reyes-Zurita FJ, Rufino-Palomares EE, Medina PP, Leticia García-Salguero E, Peragón J, Cascante M, Lupiáñez JA. Antitumour activity on extrinsic apoptotic targets of the triterpenoid maslinic acid in p53-deficient Caco-2 adenocarcinoma cells. Biochimie. 2013;95:2157-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 81. | Baek SJ, Kim JS, Jackson FR, Eling TE, McEntee MF, Lee SH. Epicatechin gallate-induced expression of NAG-1 is associated with growth inhibition and apoptosis in colon cancer cells. Carcinogenesis. 2004;25:2425-2432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 127] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 82. | Cordero-Herrera I, Martín MA, Bravo L, Goya L, Ramos S. Epicatechin gallate induces cell death via p53 activation and stimulation of p38 and JNK in human colon cancer SW480 cells. Nutr Cancer. 2013;65:718-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 83. | Sánchez-Tena S, Alcarraz-Vizán G, Marín S, Torres JL, Cascante M. Epicatechin gallate impairs colon cancer cell metabolic productivity. J Agric Food Chem. 2013;61:4310-4317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 84. | Yoo TH, Lee JH, Chun HS, Chi SG. α-Lipoic acid prevents p53 degradation in colon cancer cells by blocking NF-κB induction of RPS6KA4. Anticancer Drugs. 2013;24:555-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Gao CM, Lakatos PL, Moussata D S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH