Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.17247
Revised: June 15, 2014
Accepted: July 29, 2014
Published online: December 7, 2014
Processing time: 260 Days and 8.4 Hours
A lymphoepithelial cyst (LEC) of the pancreas is a rare benign lesion. Because patients with LEC of the pancreas have a good prognosis, it is important that these lesions are accurately differentiated from other more aggressive pancreatic neoplasms for an appropriate treatment strategy. Previous studies have reported that a definitive diagnosis of LEC often cannot be obtained based solely on the findings of preoperative imaging (e.g., Computed tomography or Magnetic resonance imaging). In this study, we reviewed four cases of pancreatic LECs to investigate the feature of LECs. We reviewed these cases with regard to symptoms, imaging findings, surgical procedures, and other clinical factors. We found that LEC was associated with unique characteristics on imaging findings. A preoperative diagnosis of LEC may be possible by comprehensively evaluating its clinical and imaging findings.
Core tip: A lymphoepithelial cyst of the pancreas is a rare benign lesion. In this study, we reviewed four cases of pancreatic lymphoepithelial cyst (LECs) to investigate the feature of LECs. We found that LEC was associated with unique characteristics on imaging findings. A preoperative diagnosis of LEC may be possible by comprehensively evaluating its clinical and imaging findings.
- Citation: Terakawa H, Makino I, Nakagawara H, Miyashita T, Tajima H, Kitagawa H, Fujimura T, Inoue D, Kozaka K, Gabata T, Ohta T. Clinical and radiological feature of lymphoepithelial cyst of the pancreas. World J Gastroenterol 2014; 20(45): 17247-17253
- URL: https://www.wjgnet.com/1007-9327/full/v20/i45/17247.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.17247
The differentiation and classification of cystic lesions of the pancreas are important for an appropriate treatment strategy. A lymphoepithelial cyst (LEC) of the pancreas is a rare benign cystic lesion[1,2]. It has been thought to be difficult to differentiate LEC from other pancreatic lesions such as serous cystic neoplasms (SCNs), mucinous cystic neoplasms (MCNs) and intraductal papillary mucinous neoplasms (IPMNs) because the appearance on imaging of LEC varies from patient to patient and sometimes similar to other pancreatic lesions[3]. In many patients, the lesion is surgically resected because a neoplastic cyst cannot be ruled out[4-6]. If a LEC can be diagnosed preoperatively, many unnecessary surgeries may be avoided. In this paper, we present four patients with LEC who underwent surgical resection and were confined as LEC. We summarized clinical and radiological features of LECs.
A retrospective review of our institutional database revealed four cases of LEC of the pancreas in recent 10 years. We reviewed these cases with regard to symptoms, imaging findings, surgical procedures, and other clinical factors. Various imaging studies were performed during the preoperative evaluation of the lesions. Imaging studies included abdominal ultrasonography (US), computed tomography (CT), magnetic resonance imaging (MRI), endoscopic ultrasonography (EUS) and endoscopic retrograde cholangiopancreatography (ERCP). All of the lesions were surgically resected and pathologically diagnosed as LEC.
Table 1 summarized the patient demographics. Three patients were men and one patient was a woman. The average age was 55 years. All of the lesions were detected incidentally during a work-up for unrelated reasons. In Patient #1 and Patient #3, the cystic lesions were localized in the body of the pancreas; in Patient #2, in the tail of the pancreas; and in Patient #4, in the head of the pancreas. The mean cystic size was 62.5 mm (range, 40-90 mm). Three patients had a multilocular cystic appearance and one patient had a unilocular cystic appearance. Three patients had elevated serum CA19-9 levels.
| Year | Age | Gender | Size (mm) | Symptom | Location | CA19-9 (U/mL) | |
| Case 1 | 2004 | 59 | Male | 90 | Nonspecific | Body | 4 |
| Case 2 | 2009 | 49 | Female | 60 | Nonspecific | Tail | 298 |
| Case 3 | 2012 | 56 | Male | 40 | Nonspecific | Body | 75 |
| Case 4 | 2012 | 56 | Male | 60 | Nonspecific | Head | 96 |
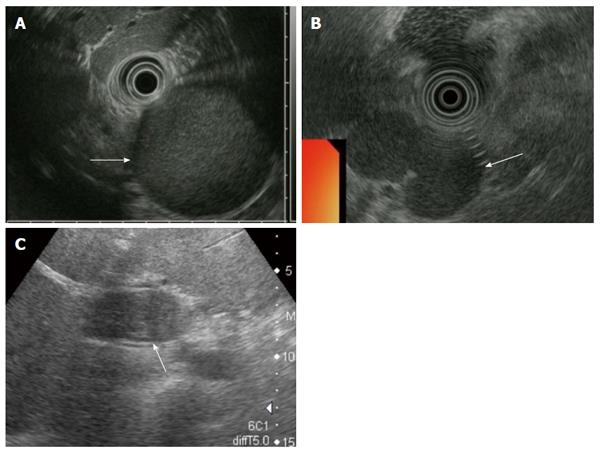
The cystic lesion in Patient #2 had a slightly hyperechoic appearance. The cystic lesion had a homogenous hypoechoic appearance in Patient #3. The cystic lesion in Patient #4 displayed a mosaic pattern. None of the three patients had solid portions the cysts (Figure 1).
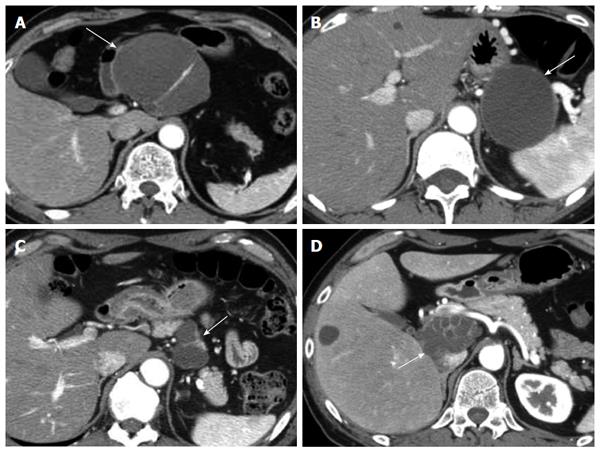
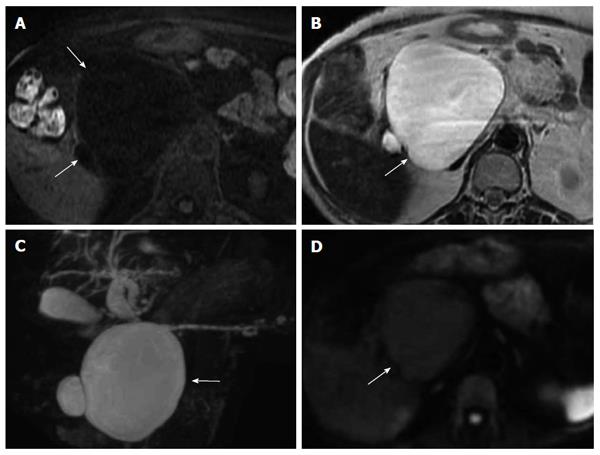
All lesions were well-defined and were exophytic off the pancreatic parenchyma. The lesion in Patient #2 had a unilocular cystic appearance, whereas the lesions in the other patients had a multilocular cystic appearance. The wall and septum of the cysts were enhanced. The contents of the cysts seemed homogeneous low density without enhancement. There were no solid portions within the cysts, calcification of the wall of the cyst, or dilatation of the main pancreatic duct, in any of the patients (Figure 2).
All patients had normal pancreatic ducts. No patients had a communication between the pancreatic duct and the cystic lesion.
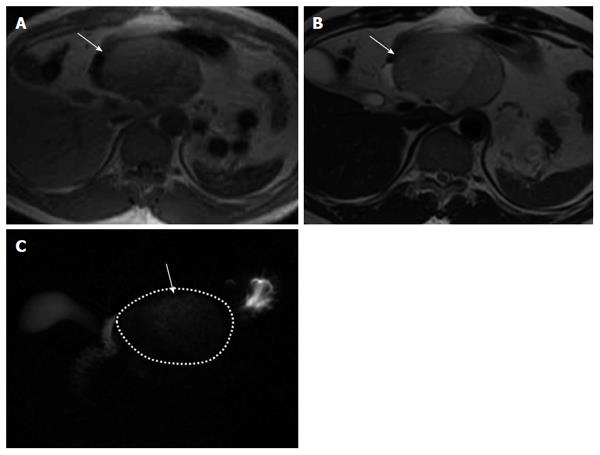
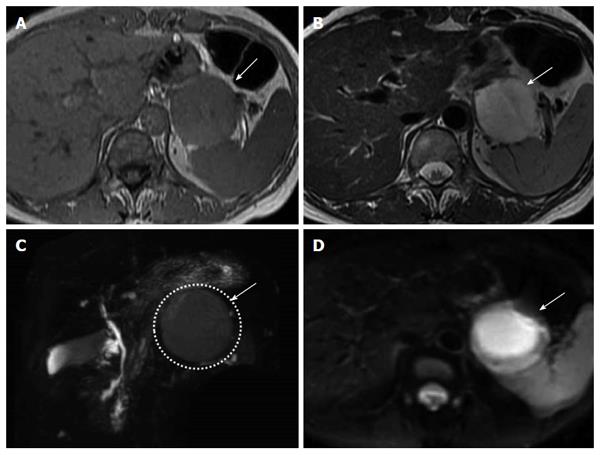
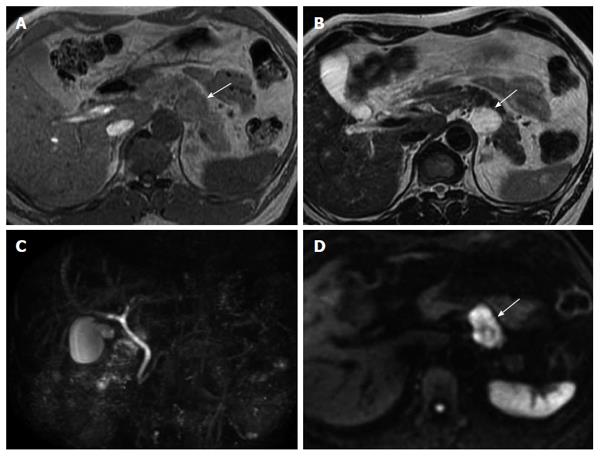
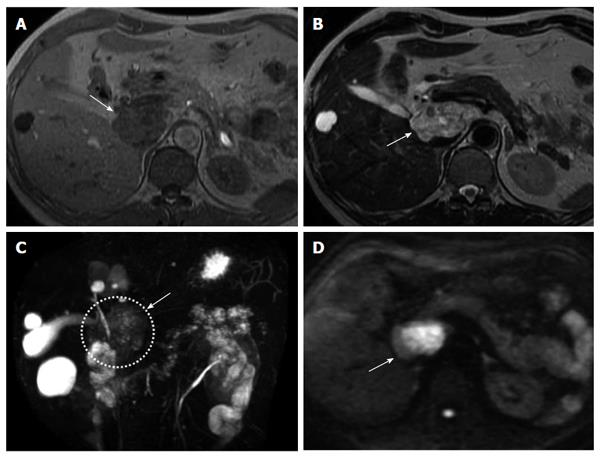
Figures 3, 4, 5, 6 present the MRI findings of four patients. We presented MRI imaging of a case of SCN which had similar signal intensity with free water for comparing with the four cases (Figure 7). T1-weighted imaging of four patients showed a higher intensity than that of SCN. T2-weighted imaging and MRCP of four patients showed a lower intensity than those of SCN. Diffusion-weighted imaging (DWI) showed a higher intensity for cystic lesions than for the SCN. In particular, on DWI, the cystic lesions showed high intense signal in the central part and iso-intense in the periphery. Signal reduction in out-of phase and in-phase was not occurred in all patients.
A LEC is a rare benign lesion, which is lined with mature keratinizing squamous epithelium and surrounded by lymphoid tissue. It typically develops in middle-aged and elderly men, and it is localized to all parts of the pancreas with equal frequency. The mean size of these cysts is 47 mm. The cyst may be multilocular (60% of patients) or unilocular (40% of patients)[7]. Many patients with LEC have elevated serum levels of CA19-9[8-10]. The cyst contents may vary from serous to caseous-like, depending on the degree of keratin formation[2].
Because LEC is a benign lesion, it is often possible to select conservative treatment for ones without any significant symptoms if they can be diagnosed correctly[11]. However, surgical resection is still commonly performed because it is difficult to distinguish them from other cystic lesions that require surgical intervention on account of their malignant potential[4-6]. EUS-guided biopsy coupled with biochemical/tumor marker studies have recently helped to improve the diagnostic accuracy of pancreatic cysts[12,13]. However, EUS-guided biopsy for cystic lesions of the pancreas is not generally performed in Japan because of the risk of the dissemination of tumor cells or the development of pseudomyxoma. Therefore, a preoperative pathological diagnosis is difficult and imaging studies are very important for treating cystic lesions of pancreas in Japanese.
We summarized the characteristics of LEC obtained from our cases and previous reports in Table 2.
| Characteristics | |
| Age, gender | Middle-aged and elderly men |
| Laboratory date | Elevation of serum CA19-9 level |
| The form | Well-defined |
| Exophytic off the pancreatic parenchyma | |
| Multilocular (60%) or Unilocular (40%) | |
| US findings | Mosaic pattern, depending on the degree of keratin formation |
| CT findings | Enhancement of the wall and septum of the cyst |
| Low density cystic lesion without enhancement | |
| No pancreatic duct dilatation | |
| MRI findings | |
| T1-weighted | Higher intensity than water |
| T2-weighted | Lower intensity than water |
| MRCP | Lower intensity than water |
| No communication with the main pancreatic duct | |
| Diffusion-weighted | Higher intensity than water |
A LEC typically develops in middle-aged and elderly men[2]. Many patients with LEC have elevated serum CA19-9[8-10].
The form of a cystic lesion was well-defined and was exophytic off the pancreatic parenchyma. It might be multilocular or unilocular[12].
The US or EUS findings sometimes displayed a mosaic pattern, depending on the degree of keratin formation[5,13,14].
The CT findings demonstrated enhancement of the wall and septum of the cyst. The cyst itself showed uniform low density without enhancement[12]. The cyst contained no solid portions within it.
The MRI findings of the four patients we reviewed were characteristic of LEC, when comparing the intensity of the lesion with that of free water. Many cystic tumors have an intensity that is similar to that of free water on MRI. In contrast, T1-weighted imaging of LEC showed a higher intensity than that of free water because the content of LEC included keratin formation. T2-weighted imaging and MRCP showed lower intensity than that of free water[15]. Diffusion-weighted imaging showed higher intensity than that of free water[10]. In particular, on DWI, the cystic lesions showed high intense signal in the central part and iso-intense in the periphery. It seemed that the part showing high intense signal indicated keratin formation and iso-intense in periphery indicated the wall.
However, these findings should be cautiously interpreted, because MCN and IPMN can sometimes show similar signal intensity if bleeding into the cyst has occurred[16].
In summary, the clinical and radiological findings are sufficiently characteristic of LEC to establish a preoperative diagnosis for a majority of patients of LEC. It might be possible to select conservative treatment for asymptomatic patients with LEC.
Four cases were incidentally detected the pancreatic tumors and performed surgery.
Three patients had a multilocular cystic appearance and one patient had a unilocular cystic appearance.
Serous cystic neoplasms, Mucinous cystic neoplasms, intraductal papillary mucinous neoplasms.
Three patients had elevated serum CA19-9 levels.
All lesions were well-defined and were exophytic off the pancreatic parenchyma.
All of the lesions were pathologically diagnosed as the lymphoepithelial cyst.
All of the lesions were surgically resected.
A lymphoepithelial cyst of the pancreas has been thought to be difficult to differentiate from other pancreatic lesions.
The authors found that the lymphoepithelial cyst was associated with unique characteristics on imaging findings. A preoperative diagnosis of the lymphoepithelial cyst may be possible by comprehensively evaluating its clinical and imaging findings.
The discussion is simple. In this article, there were any findings about PET-CT and something else.
| 1. | Lüchtrath H, Schriefers KH. [A pancreatic cyst with features of a so-called branchiogenic cyst]. Pathologe. 1985;6:217-219. [PubMed] |
| 2. | Volkan Adsay N. Cystic lesions of the pancreas. Mod Pathol. 2007;20 Suppl 1:S71-S93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Osiro S, Rodriguez JR, Tiwari KJ, Rodriguez II, Mathenge N, Tubbs RS, Loukas M. Is preoperative diagnosis possible? A clinical and radiological review of lymphoepithelial cysts of the pancreas. JOP. 2013;14:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 4. | Idetsu A, Ojima H, Saito K, Hirayama I, Hosouchi Y, Nishida Y, Nakajima T, Kuwano H. Lymphoepithelial cyst of the pancreas: report of a case. Surg Today. 2008;38:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Domen H, Ohara M, Kimura N, Takahashi M, Yamabuki T, Komuro K, Iwashiro N, Ishizaka M. Lymphoepithelial cyst of the pancreas. Case Rep Gastroenterol. 2012;6:604-611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Fukunaga N, Ishikawa M, Minato T, Yamamura Y, Ishikura H, Ichimori T, Kimura S, Sakata A, Fujii Y. Lymphoepithelial cyst of the pancreas that was difficult to distinguish from branch duct-type intraductal papillary mucinous neoplasm: report of a case. Surg Today. 2009;39:901-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Adsay NV, Hasteh F, Cheng JD, Klimstra DS. Squamous-lined cysts of the pancreas: lymphoepithelial cysts, dermoid cysts (teratomas), and accessory-splenic epidermoid cysts. Semin Diagn Pathol. 2000;17:56-65. [PubMed] |
| 8. | Yamaguchi T, Takahashi H, Kagawa R, Takeda R, Sakata S, Yamamoto M, Nishizaki D. Lymphoepithelial cyst of the pancreas associated with elevated CA 19-9 levels. J Hepatobiliary Pancreat Surg. 2008;15:652-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Ohta T, Nagakawa T, Fukushima W. Carbohydrate Antigen 19-9-Producing Lymphoepithelial Cyst of the Pancreas: A Case Report with an Immunohistochemical Study. Dig Surg. 1992;9:221-225. |
| 10. | Nam SJ, Hwang HK, Kim H, Yu JS, Yoon DS, Chung JJ, Kim JH, Kim KW. Lymphoepithelial cysts in the pancreas: MRI of two cases with emphasis of diffusion-weighted imaging characteristics. J Magn Reson Imaging. 2010;32:692-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | DiCorato MP, Schned AR. A rare lymphoepithelial cyst of the pancreas. Am J Clin Pathol. 1992;98:188-191. [PubMed] |
| 12. | Kavuturu S, Sarwani NE, Ruggeiro FM, Deshaies I, Kimchi ET, Kaifi JT, Staveley-O’Carroll KF, Gusani NJ. Lymphoepithelial cysts of the pancreas. Can preoperative imaging distinguish this benign lesion from malignant or pre-malignant cystic pancreatic lesions? JOP. 2013;14:250-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Foley KG, Christian A, Roberts SA. EUS-FNA diagnosis of a pancreatic lymphoepithelial cyst: three-year imaging follow-up. JOP. 2012;13:681-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Rino Y, Morohoshi T, Funo K, Imada T, Yamamoto Y, Jojima T, Abe M, Take H, Matsumoto A. Lymphoepithelial cyst of the pancreas: a preoperatively diagnosed case based on an aspiration biopsy. Surg Today. 1995;25:1043-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Shinmura R, Gabata T, Matsui O. Lymphoepithelial cyst of the pancreas: case report with special reference to imaging--pathologic correlation. Abdom Imaging. 2006;31:106-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Inoue T, Takada S, Shimizu H, Niizuma K, Fujimura M, Sato K, Endo H, Tominaga T. Signal changes on T2*-weighted magnetic resonance imaging from the acute to chronic phases in patients with subarachnoid hemorrhage. Cerebrovasc Dis. 2013;36:421-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
P- Reviewer: Chen F, Liu HB S- Editor: Qi Y L- Editor: A E- Editor: Wang CH