Published online Nov 21, 2014. doi: 10.3748/wjg.v20.i43.16368
Revised: June 18, 2014
Accepted: July 16, 2014
Published online: November 21, 2014
Processing time: 223 Days and 22.4 Hours
Eosinophilic gastroenteritis is a rare disease of unknown etiology. It is characterized by patchy or diffuse eosinophilic infiltration of the bowel wall to a variable depth and various gastrointestinal manifestations. We describe a case of severe eosinophilic gastroenteritis presenting as frequent bowel obstruction and diarrhea in a 35-year-old man. The patient was misdiagnosed and underwent surgery because of intestinal obstruction when he was first admitted to a local hospital. Then he was misdiagnosed as having Crohn’s disease in another university teaching hospital. Finally, the patient asked for further treatment from our hospital because of the on-going clinical trial for treating refractory Crohn’s disease by fecal microbiota transplantation. Physical examination revealed a slight distended abdomen with diffuse tenderness. Laboratory investigation showed the total number of normal leukocytes with neutrophilia as 90.5%, as well as eosinopenia, monocytopenia and lymphocytopenia. Barium radiography and sigmoidoscopy confirmed inflammatory stenosis of the sigmoid colon. We diagnosed the patient as having eosinophilic gastroenteritis by multi-examinations. The patient was treated by fecal microbiota transplantation combined with oral prednisone, and was free from gastrointestinal symptoms at the time when we reported his disease. This case highlights the importance of awareness of manifestations of a rare disease like eosinophilic gastroenteritis.
Core tip: We report a case of severe eosinophilic gastroenteritis presenting as frequent bowel obstruction and diarrhea in a 35-year-old man. The patient was misdiagnosed and underwent surgery because of intestinal obstruction when he was first admitted to a local hospital. Then he was misdiagnosed as having Crohn’s disease in another hospital. Here we present our experience of diagnosis and treatment with fecal microbiota transplantation and oral prednisone for this case. This case is characterized by the unusual features of eosinophilic gastroenteritis and effects of novel therapy.
- Citation: Dai YX, Shi CB, Cui BT, Wang M, Ji GZ, Zhang FM. Fecal microbiota transplantation and prednisone for severe eosinophilic gastroenteritis. World J Gastroenterol 2014; 20(43): 16368-16371
- URL: https://www.wjgnet.com/1007-9327/full/v20/i43/16368.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i43.16368
Eosinophilic gastroenteritis is a rare disease characterized by patchy or diffuse eosinophilic infiltration of the bowel wall to a variable depth and symptoms associated with the gastrointestinal tract[1,2]. The first description of the disease was made by Talley et al[3]. The pathogenesis and etiology of the disease remain unknown[4,5]. Diagnostic criteria include demonstration of eosinophilic infiltration of the bowel wall, lack of evidence of extra-intestinal disease, and exclusion of various disorders that could mimic a similar condition[1]. Here we present our experience of diagnosis and novel therapy for a case of severe eosinophilic gastroenteritis presenting as frequent bowel obstruction and diarrhea.
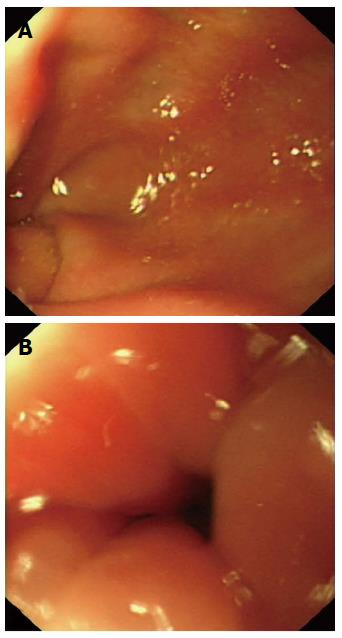
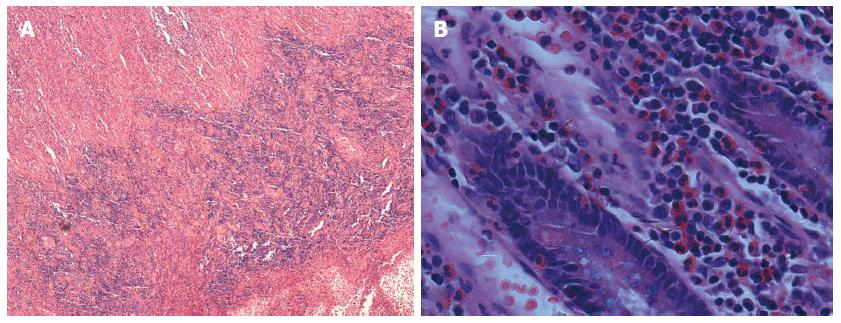
A 35-year-old man was first admitted to a local hospital in March 2012 for progressing abdominal pain and distension. Computer tomography scan demonstrated marked wall thickening and stenosis of the intestine in the lower right abdomen. An emergency laparotomy was performed for the consideration of acute appendicitis. Exploration revealed focal stricture in the ileocecal junction. Segmental resection of the ileocecum and end to end anastomosis were performed. After the operation, diarrhea and incomplete ileus still occurred frequently, and symptomatic treatment had little effect. Severe intestinal obstruction recurred in September 2012, at which time doctors in another university teaching hospital reviewed previous surgical biopsy and diagnosed the patient as having Crohn’s disease. After eliminating infection, two weeks prednisone and two months nasogastric tube feeding of enteral nutrition and azathioprine did not improve the symptoms. He suffered from diarrhea over twenty times a day. Finally, the patient asked for further treatment from our hospital in November 2012 because of the on-going clinical trial (NCT01793831) for treating refractory Crohn’s disease by fecal microbiota transplantation (FMT). The patient had no history of drug allergy, asthma, or allergic rhinitis. Physical examination revealed a slight distended abdomen with diffuse tenderness. Laboratory investigation showed the total number of normal leukocytes, with neutrophilia of 90.5%, eosinopenia of 0%, monocytopenia of 2.2%, lymphocytopenia of 7.2%, erythrocyte sedimentation rate 42 mm/h, and C-reactive protein 69 mg/L. Blood and stool bacterial culture were negative. Blood tests for Cytomegalovirus and Epstein-Barr virus were negative. Sigmoidoscopy revealed an obvious stenosis and a smooth, diffusely inflamed sigmoid mucosa from which multiple biopsies were taken (Figure 1). Barium radiography confirmed a stricture of the sigmoid colon (Figure 2). Previous surgical biopsy showed a dense infiltration of eosinophils throughout the entire thickness of the bowel wall (Figure 3). After excluding the possibilities of malignancy by surgical pathology, parasitic disease by stool examination, and autoimmune disease by immunological tests, eosinophilic gastroenteritis was diagnosed. Antibiotics was used, but there was no clinical improvement. The patient strongly demanded FMT treatment for his disease, and the donor of the feces was his 9-year-old healthy daughter. The routine screening for potential pathogens was performed in all donors. After single standardized FMT through the mid-gut by gastroscope, referring to our previous protocol[6], the frequent diarrhea was dramatically reduced within one week. However, the stenosis still existed. For consideration of combined therapy, prednisone 35 mg/d was used in the first three weeks and gradually reduced until it was terminated within seven weeks. The patient recovered well and was free from gastrointestinal symptoms until six weeks after he stopped steroids. Diarrhea recurred but the stricture of the sigmoid colon disappeared during colonoscopy. A steroid was used again for six weeks. The patient was completely free of recurrence during the follow-up 11 mo, at which time he regained 10 kg and had normal working capability.
Eosinophilic gastroenteritis is an uncommon disease and can be seen anywhere in the gastrointestinal tract. In 1970, Klein et al[7] classified the disease into mucosal, muscular and serosal types based on the depth of involvement. The involvement of different layers usually gives rise to different clinical manifestations. The most common mucosal disease generally presents with diarrhea, bleeding, and protein-losing enteropathy, or malabsorption. Involvement of the muscle layer may cause bowel wall thickening and subsequent intestinal obstruction, which was the manifestation in this patient. The subserosal form usually presents with peritonitis and eosinophilic ascites, with or without any or all of the symptoms associated with mucosal and/or muscle layer disease[1,8].
Because the pathogenesis and etiology of the disease are not clear, there are no standards for the diagnosis of eosinophilic gastroenteritis. Talley et al[3] have identified three main diagnostic criteria: (1) the presence of gastrointestinal symptoms; (2) biopsies demonstrating eosinophilic infiltration of one or more areas of the gastrointestinal tract, or characteristic radiological findings with peripheral eosinophilia; or (3) no evidence of parasitic or extra-intestinal disease. However, the definitive diagnosis is the histologic demonstration of eosinophilic infiltration of some part of the gastrointestinal tract[2]. Rarely, Crohn’s disease or ulcerative colitis might be associated with peripheral eosinophilia, but they can usually be excluded by biopsy because of a lack of eosinophilia[9].
There is no consensus about the treatment of eosinophilic gastroenteritis, but long term steroid treatment is the mainstay management so far. It is now well appreciated that intestinal microbiota make up a microbial organ that is integral to overall host physiology, including pivotal roles in metabolism and immune system function[10]. The concept of FMT in traditional Chinese medicine has been recorded for at least 1700 years to treat intestinal diseases[11]. Reports of applications outside of Clostridium difficile infection are emerging because more patients request treatment and more clinics incorporate FMT into their treatment repertoire, which will pave the way for the use of FMT in several idiopathic conditions[12]. After all this comprehensive consideration, we eventually tried the combination treatment of FMT and prednisone, and achieved good clinical effects. We can differentiate between the effects of prednisone and FMT because FMT was used one week before prednisone and dramatically reduced the frequency of diarrhea within several days. This indicated the fast therapeutic role of FMT in eosinophilic gastroenteritis cases presenting as long-term diarrhea. Besides, the patient did not benefit from the two-week treatment with prednisone before he went to our hospital and appeared to respond to our combination treatment judging by the disappearance of the gastrointestinal symptoms. However, it remains unclear whether FMT could cure eosinophilic gastroenteritis or maintain long term clinical remission if prednisone was not given. As far as we know, this is the first report where FMT was used to treat severe eosinophilic gastroenteritis.
A case of severe eosinophilic gastroenteritis presenting as frequent bowel obstruction and diarrhea.
Clinical symptoms and surgical pathology are very important for the diagnosis of eosinophilic gastroenteritis.
Long term follow-up should be important for confirming or correcting previous diagnosis when it is difficult to make a differential diagnosis between Crohn’s disease and severe eosinophilic gastroenteritis.
Peripheral eosinophilia was not observed in this case.
X-ray barium radiography discloses typical stenosis of the sigmoid colon.
Microscopy of the resected ileocecum, revealing eosinophilic infiltration from the submucosa to the subserosa.
The combination treatment of fecal microbiota transplantation (FMT) and prednisone achieved good clinical effects after previous failure of treatment with prednisone, azathioprine and enteral nutrition.
Patients with severe intestinal disease might benefit from FMT.
FMT is a special therapeutic modulation which uses microbiota from stools.
Manifestations of a rare disease should draw clinical workers great attention.
This is the first report where FMT was used to treat severe eosinophilic gastroenteritis. However, Helicobacter pylori (H. pylori) was not detected in this case. It is important to evaluate infection by H. pylori due to a recent work in which the patient was cured from eosinophilic gastroenteritis just by eradicating the infection.
| 1. | Hsu YQ, Lo CY. A case of eosinophilic gastroenteritis. Hong Kong Med J. 1998;4:226-228. [PubMed] |
| 2. | Chen MJ, Chu CH, Lin SC, Shih SC, Wang TE. Eosinophilic gastroenteritis: clinical experience with 15 patients. World J Gastroenterol. 2003;9:2813-2816. [PubMed] |
| 3. | Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990;31:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 527] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 4. | Caldwell JH. Eosinophilic Gastroenteritis. Curr Treat Options Gastroenterol. 2002;5:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Alamo Martínez JM, Ibáñez Delgado F, Galindo Galindo A, Bernnal Bellido C, Durén Ferreras I, Suárez Artacho G, Martínez Vieira A. Intestinal obstruction by eosinophilic jejunitis. Rev Esp Enferm Dig. 2004;96:279-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zhang FM, Wang HG, Wang M, Cui BT, Fan ZN, Ji GZ. Fecal microbiota transplantation for severe enterocolonic fistulizing Crohn’s disease. World J Gastroenterol. 2013;19:7213-7216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 90] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (2)] |
| 7. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 412] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004;113:11-28; quiz 29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 627] [Cited by in RCA: 589] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 9. | Levy AM, Gleich GJ, Sandborn WJ, Tremaine WJ, Steiner BL, Phillips SF. Increased eosinophil granule proteins in gut lavage fluid from patients with inflammatory bowel disease. Mayo Clin Proc. 1997;72:117-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3394] [Cited by in RCA: 3632] [Article Influence: 173.0] [Reference Citation Analysis (5)] |
| 11. | Zhang F, Luo W, Shi Y, Fan Z, Ji G. Should we standardize the 1,700-year-old fecal microbiota transplantation? Am J Gastroenterol. 2012;107:1755; author reply 1755-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 422] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 12. | Borody TJ, Khoruts A. Fecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol. 2012;9:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 482] [Article Influence: 32.1] [Reference Citation Analysis (13)] |
P- Reviewer: Blanco LP, Freedberg DE, Xu CS S- Editor: Gou SX L- Editor: O’Neill M E- Editor: Zhang DN