Published online Sep 14, 2014. doi: 10.3748/wjg.v20.i34.12277
Revised: April 9, 2014
Accepted: May 25, 2014
Published online: September 14, 2014
Processing time: 237 Days and 21.8 Hours
AIM: To investigate the impact of heartburn and regurgitation on the quality of life among patients with gastroesophageal reflux disease (GERD).
METHODS: Data from patients with GERD, who were diagnosed according to the Montreal definition, were collected between January 2009 and July 2010. The enrolled patients were assigned to a heartburn or a regurgitation group, and further assigned to an erosive esophagitis (EE) or a non-erosive reflux disease (NERD) subgroup, depending on the predominant symptoms and endoscopic findings, respectively. The general demographic data, the scores of the modified Chinese version of the GERDQ and the Short-form 36 (SF-36) questionnaire scores of these groups of patients were compared.
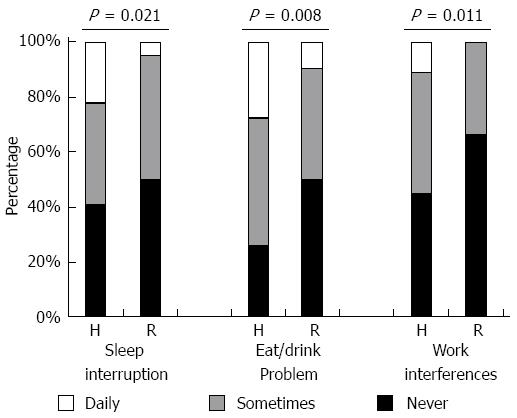
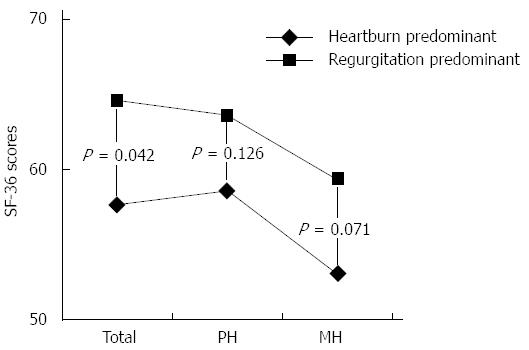
RESULTS: About 108 patients were classified in the heartburn group and 124 in the regurgitation group. The basic characteristics of the two groups were similar, except for male predominance in the regurgitation group. Patients in the heartburn group had more sleep interruptions (22.3% daily vs 4.8% daily, P = 0.021), more eating or drinking problems (27.8% daily vs 9.7% daily, P = 0.008), more work interferences (11.2% daily vs none, P = 0.011), and lower SF-36 scores (57.68 vs 64.69, P = 0.042), than patients in the regurgitation group did. Individuals with NERD in the regurgitation group had more impaired daily activities than those with EE did.
CONCLUSION: GERD patients with heartburn or regurgitation predominant had similar demographics, but those with heartburn predominant had more severely impaired daily activities and lower general health scores. The NERD cases had more severely impaired daily activity and lower scores than the EE ones did.
Core tip: The study was aimed to investigate the impact of heartburn and regurgitation on the quality of life among patients with gastroesophageal reflux disease (GERD). The results found GERD patients with heartburn predominant had more severely impaired daily activities and lower general health scores than those with regurgitation predominant. Non-erosive reflux disease greatly impaired daily function in regurgitation-predominant patients, but did not have such impact in those with heartburn predominant.
- Citation: Lee SW, Lien HC, Lee TY, Yang SS, Yeh HJ, Chang CS. Heartburn and regurgitation have different impacts on life quality of patients with gastroesophageal reflux disease. World J Gastroenterol 2014; 20(34): 12277-12282
- URL: https://www.wjgnet.com/1007-9327/full/v20/i34/12277.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i34.12277
Gastroesophageal reflux disease (GERD) is a common disorder of the upper gastrointestinal tract that is typically characterized by heartburn and acid regurgitation. According to the Montreal definition, GERD is a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications[1]. GERD has an impact on the daily lives of affected individuals, interfering with physical activity, impairing social functioning, disturbing sleep and reducing productivity at work[2-5]. According to the Genval guidelines, a negative impact on the quality of life is a criterion for reflux disease in patients with frequent heartburn[6]. GERD patients can be classified as having either erosive esophagitis (EE) or non-erosive reflux disorder (NERD) depending on endoscopic findings[7]. The aim of this study was to investigate the impact of two cardinal GERD symptoms, heartburn and regurgitation, on the quality of life of patients with EE and those with NERD.
Data from consecutive adult patients with GERD in our hospital, Taichung Veterans General Hospital, who were diagnosed according to the Montreal definition, were prospectively collected from January 2009 to July 2010. Exclusion criteria were as follows: (1) GERD combined with other structural gastrointestinal disorders, such as peptic ulcer disease, esophageal or gastric malignancy; (2) prior gastric surgery; (3) use of chronic anti-acid medication, such as proton pump inhibitors (PPIs) or H2-receptor antagonists (H2RAs), for more than 2 mo prior to enrollment; and (4) pregnancy. This study was conducted with the approval of the Clinical Research Ethics Committee of Taichung Veterans General Hospital.
The general data of enrolled patients, including age, gender, body weight, body mass index (BMI), symptom duration and lifestyle habits, were recorded. All patients underwent an open-access transoral upper gastrointestinal endoscopy, and the findings of esophagocardiac mucosal break, esophagocardiac junction (ECJ) ulcer, hiatal hernia or Helicobacter pylori (H. pylori) infection of each case were collected. All patients were asked to complete the questionnaires, including the modified Chinese version of GERDQ, the modified GERD impact scale, and the Short-form 36 (SF-36) questionnaire (Chinese version).
The modified Chinese version of GERDQ included questions about the severity of the symptoms of heartburn (“a burning feeling behind the breastbone”) and regurgitation (“unpleasant movement of material upwards from the stomach”). Answers were graded on a three-point Likert scale, as follows: mild was defined as symptoms that can be easily ignored; moderate, awareness of symptoms but easily tolerated; and advanced symptoms sufficient to cause an interference with normal activities. The enrolled patients were classified as having heartburn, defined as more severe symptoms of heartburn than regurgitation, and the regurgitation group, defined as more severe symptoms of regurgitation than heartburn.
The modified GERD impact scale measures the frequency of imparied daily activity, including sleep interruption, eating or drinking problems, and work interferences, graded on a three-point Likert scale, as follows: never, sometimes and daily. The SF-36 questionnaire measures generic quality of life, which allows comparisons between different disease states. It also measures health status in eight domains: physical functioning, role limitations-physical, bodily pain, general health, vitality, social functioning, role limitations-emotional, and mental health. Two summary scores were also calculated from subject responses: the physical health (PH) score and the mental health (MH) score. Scores on the SF-36 range from 0 to 100 in each dimension and on the summary scales, with higher scores indicating better quality of life.
Data are expressed as standard derivation of the mean for each of the measured parameters. Gender, hiatal hernia, H. pylori, ECJ ulcer, endoscopic findings and lifestyle habits, are expressed as a percentage of the total patient number. A P value below 0.05 was considered statistically significant. Statistical analyses were made using Pearson’s χ2 test to compare the effects of gender, hiatal hernia, lifestyle habits and GERD impact scale scores; ANOVA test was used to analyze age, body weight, BMI, and scores of the SF-36 questionnaires.
A total of 290 consecutive patients were enrolled, and 58 cases had similar severity of symptoms of heartburn and regurgitation. Among the remaining 232 patients, 108 (46.6%) were classified in the heartburn group and 124 (53.4%) were classified in the regurgitation group. The symptom severities were similar in these two groups, as shown in Table 1.
| Groups | Severity | Total | ||
| Mild | Moderate | Severe | ||
| Heartburn group | 4 (3.7) | 85 (78.7) | 19 (17.6) | 108 |
| Regurgitation group | 6 (4.8) | 102 (82.3) | 16 (12.9) | 124 |
The characteristics of the heartburn group and regurgitation group are presented in Table 2. The heartburn group had more males than the regurgitation group did (57.4% vs 38.7%, P = 0.044). Other general data, including age, body weight and BMI, were similar between the two groups. There were no significant differences in endoscopic findings, such as NERD/EE ratio, ECJ ulcer, hiatal hernia, H. pylori infection rate, or lifestyle habits, such as tea, alcohol, coffee consumption, and cigarette smoking.
| Characteristics | Heartburn group (n = 108, 46.6%) | Regurgitation group (n = 124, 53.4%) | P value | |||
| n (%) | mean ± SD | n (%) | mean ± SD | |||
| Mean age (yr) | 48.72 ± 13.97 | 44.92 ± 15.30 | 0.1301 | |||
| Gender | M | 62 (57.4) | 48 (38.7) | 0.0442 | ||
| F | 46 (42.6) | 76 (61.3) | ||||
| Weight (kg) | 62.30 ± 13.56 | 63.33 ± 11.85 | 0.8341 | |||
| BMI (kg/m2) | 22.97 ± 3.87 | 23.38 ± 3.42 | 0.8251 | |||
| H. pylori | 28 (25.9) | 22 (17.7) | 0.2852 | |||
| Hiatal hernia | 30 (27.8) | 34 (27.4) | 0.9662 | |||
| ECJ ulcer | 8 (7.4) | 12 (9.7) | 0.6642 | |||
| Endoscopic finding | NERE | 54 (50.0) | 56 (45.2) | 0.8362 | ||
| EE | 54 (50.0) | 68 (54.8) | ||||
| Life style | Coffee | 70 (64.8) | 76 (61.3) | 0.6952 | ||
| Alcohol | 44 (40.7) | 48 (38.7) | 0.8232 | |||
| Tea | 84 (77.8) | 104 (83.9) | 0.4042 | |||
| Smoke | 20 (18.5) | 16 (12.9) | 0.4052 | |||
The results of the modified GERD impact scale and the SF-36 questionnaire scores of the two groups are displayed in Figures 1 and 2, respectively. The heartburn group had significantly more sleep interruptions (22.3% daily vs 4.8% daily, P = 0.021), more eating or drinking problems (27.8% daily vs 9.7% daily, P = 0.008), and more work interferences (11.2% daily vs none, P = 0.011), than the regurgitation group did. Similarly, according to the results of the SF-36 questionnaire, the heartburn group had lower scores than the regurgitation group did, including total scores (57.68 vs 64.69, P = 0.042), PH scores (58.53 vs 63.52, P = 0.126), and MH scores (53.04 vs 59.31, P = 0.071).
There were 54 (50%) NERD patients and 54 (50%) EE patients in the heartburn group, and 56 (45.2%) NERD cases and 68 (54.8%) EE cases in the regurgitation group, respectively. The two main groups, the heartburn group and the regurgitation group, were further divided into four subgroups: NERD with heartburn, EE with heartburn, NERD with regurgitation and EE with regurgitation, depending on individual endoscopic findings.
The basic characteristics of the NERD and EE patients in the heartburn group and regurgitation group are shown in Table 3. Male predominance in the EE with heartburn subgroup (74.1%) and female predominance in the NERD with regurgitation subgroup (71.4%) were noted. More severe obesity, including higher body weight and BMI, were found in EE patients than in NERD cases in both subgroups, particularly in the EE with heartburn subgroup (mean body weight, 68 vs 56.59, P = 0.001; mean BMI, 24.24 vs 21.68, P = 0.014). ECJ ulcers were found in the EE with heartburn subgroup (14.8%) and the EE with regurgitation subgroup (17.6%). In the EE with heartburn subgroup, there were more cases of hiatal hernia than in the NERD with heartburn subgroup (40.7% vs 14.8%, P = 0.033), but the difference was not significant in the NERD with regurgitation subgroup. The ratio of H. pylori infection was similar among all 4 subgroups.
| Characteristics | Heartburn group | P value | Regurgitation group | P value | |||||||
| NERD (n = 54, 50%) | EE (n = 54, 50%) | NERD (n = 56, 45.2%) | EE (n = 68, 54.8%) | ||||||||
| n (%) | mean ± SD | n (%) | mean ± SD | n (%) | mean ± SD | n (%) | mean ± SD | ||||
| Mean age (yr) | 46.89 ± 14.75 | 50.56 ± 13.15 | 0.3401 | 39.64 ± 10.23 | 48.21 ± 19.77 | 0.0431 | |||||
| Gender | M | 22 (40.7) | 40 (74.1) | 0.0132 | 16 (28.6) | 32 (47.1) | 0.1372 | ||||
| F | 32 (59.3) | 14 (25.9) | 40 (71.4) | 36 (52.9) | |||||||
| Weight (kg) | 56.59 ± 10.07 | 68.00 ± 14.34 | 0.0011 | 60.28 ± 8.71 | 64.85 ± 13.67 | 0.1311 | |||||
| BMI (kg/m2) | 21.68 ± 3.43 | 24.24 ± 3.92 | 0.0141 | 22.59 ± 2.90 | 23.52 ± 3.65 | 0.2931 | |||||
| H. pylori | 14 (25.9) | 14 (25.9) | 1.0002 | 8 (14.3) | 14 (20.6) | 0.5182 | |||||
| Hiatal hernia | 8 (14.8) | 22 (40.7) | 0.0332 | 16 (28.6) | 18 (26.5) | 0.8542 | |||||
| ECJ ulcer | 0 | 8 (14.8) | 0.0503 | 0 | 12 (17.6) | 0.0283 | |||||
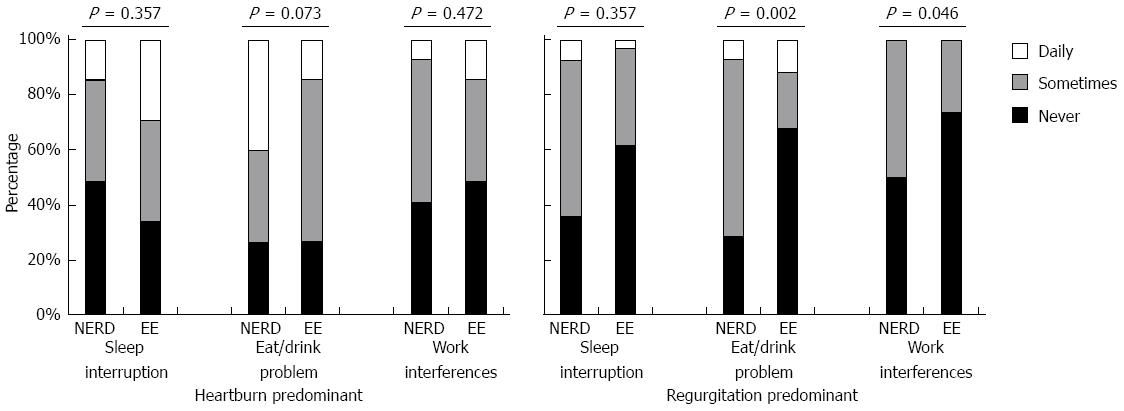
The results of the modified GERD impact scale of these four subgroups are shown in Figure 3. The NERD and EE with heartburn subgroups had a similar presentation of daily activities. However, the NERD with regurgitation subgroup had a significantly higher ratio of impaired daily activity than the EE with regurgitation subgroup did, in particular, eating or drinking problems (11.8% daily vs 7.1% daily, P = 0.002), and work interferences (50% “sometimes”vs 26.5% “sometimes”, P = 0.046).
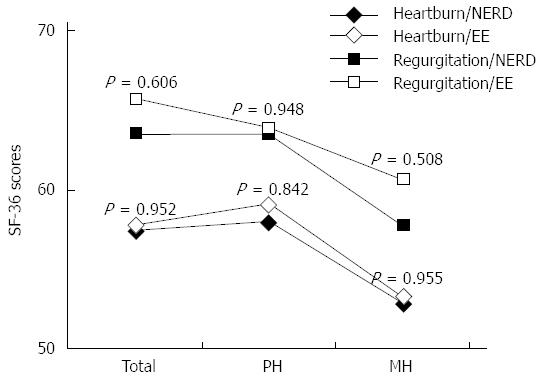
The SF-36 questionnaire scores of these four subgroups are listed in Figure 4. In general, the NERD patients had lower scores, both in the physical and mental dimensions, than the EE cases did, but the difference was not significant. The EE with regurgitation subgroup had the highest scores (mean total score 65.68, PH score 63.76, MH score 60.62), and the NERD with heartburn subgroup had the worst scores (mean total score 57.52, PH score 58, MH score 52.88).
GERD is a chronic disease that tends to relapse and cause complications. Typical symptoms associated with GERD include heartburn, acid regurgitation, and chest pain, as well as extraesophageal manifestations such as nausea, chronic cough, asthma, and hoarseness. Previous studies indicated that the risk factors in patients with GERD include age[4], obesity[5,8], hiatal hernia[9], and an unhealthy lifestyle, including alcohol consumption and cigarette smoking. The two typical presentations of GERD are heartburn and regurgitation. Heartburn is usually characterized as a burning substernal or epigastric discomfort which radiates towards the mouth, and regurgitation refers to reflux of food or bitter-tasting gastric contents from the stomach into the mouth. Though these two symptoms are often paired, they are different conditions, and sometimes one can affect a patient without the occurrence of the other.
Patients with GERD may present with a broad range of troublesome symptoms that can affect the quality of their daily lives[2-5]. The negative effects of GERD are dependent on the frequency and severity of symptoms rather than the presence of esophagitis. Studies conducted in Sweden’s general population, which assessed the impact of the severity and frequency of GERD symptoms, showed that even symptoms rated as mild are associated with a clinically meaningful reduction in well-being[10]. One large European multicenter observational study noted more than half of GERD cases had sleep disturbance, and persistent regurgitation was associated with more hours of work missed[11]. Other two previous studies documented increasing symptom frequency of heartburn that led to significant decreases in well-being[12,13].
Our study disclosed that patients with heartburn predominant had more severely impaired daily activity, including sleep interruption, eating or drinking problems and work interferences, than those with regurgitation predominant. Furthermore, the individuals with heartburn predominant also had lower SF-36 health scores. These results implied that there might be a difference in the presentation of symptoms and quality of life of GERD patients.
Furthermore, recent analyses of clinical trial data suggest regurgitation is less responsive to acid suppression than heartburn, and may be a common cause of incomplete treatment response[14,15]. To investigate the physicopathological presentations of heartburn and regurgitation, one study monitored 32 patients with symptoms suggesting GERD using 24-h ambulatory pH and impedance. The results showed that reflux episodes inducing regurgitation had a higher proximal extent of liquid component, but less esophageal pH drop, than episodes inducing heartburn[16].
Although patients with GERD have a broad range of troublesome symptoms that can adversely affect the quality of life, studies have shown that individuals with EE and NERD have similar total quality of life scores[17,18]. In our study, patients with EE and those with NERD had similar general quality of life scores, both in the heartburn subgroup and the regurgitation subgroup. However, the NERD patients with regurgitation predominant had more significantly impaired daily functions, including eating or drinking problems and work interferences, than the EE cases did. The results implied that NERD regurgitation predominance has a more negative impact on life quality than EE regurgitation predominance, but there were no differences in the heartburn-predominant cases.
There are some limitations in our study. Firstly, co-morbid diseases that tend to influence the severity of GERD, such as chronic heart failure or chronic obstructive pulmonary disease, were not considered, and this might have led to inaccurate outcomes. Secondly, the endoscopic findings were recorded by individual endoscopists, and inter-observer conflict and misclassification might have occurred. Thirdly, gender predominant was found in some subgroups, and that might influence the finial results. Fourthly, not all of our cases with NERD have accepted pH-metry monitoring, and it might lead to a misclassification of the individuals with functional heartburn as NERD. Fively, the lifestyle characteristics in our study only reflect the patients’ current status. Lastly, our study was hospital-based designed. Further research using representative samples of the general population are needed to confirm these results.
In conclusion, in the present study, GERD patients with heartburn and regurgitation predominant had similar demographics, but heartburn predominance had a more negative impact on daily activity and general health scores. In general, the NERD cases had more severely impaired daily activity and lower scores than the EE ones did.
Gastroesophageal reflux disease (GERD) is typically characterized by heartburn and acid regurgitation. GERD has an impact on the daily lives of affected individuals, interfering with physical activity, impairing social functioning and reducing productivity at work.
The aim of this study was to investigate the impact of two cardinal GERD symptoms, heartburn and regurgitation, on the quality of life of patients with GERD.
Patients in the heartburn group had more sleep interruptions, more eating or drinking problems, more work interferences, and lower SF-36 scores than patients in the regurgitation group did. Non-erosive reflux disease greatly impaired daily function in regurgitation-predominant cases, but did not have such impact in those with heartburn predominant.
GERD patients with heartburn predominant had a more negative impact on daily activity and general health scores than those with regurgitation predominant.
This is an interesting original manuscript assessing the impact of heartburn and regurgitation on quality of life in GERD patients.
This is an interesting original manuscript assessing the impact of heartburn and regurgitation on quality of life in GERD patients.
| 1. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. [The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper]. Z Gastroenterol. 2007;45:1125-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Wiklund I. Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis. 2004;22:108-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 142] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Wahlqvist P, Karlsson M, Johnson D, Carlsson J, Bolge SC, Wallander MA. Relationship between symptom load of gastro-oesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment Pharmacol Ther. 2008;27:960-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | Lee SW, Chang CM, Chang CS, Kao AW, Chou MC. Comparison of presentation and impact on quality of life of gastroesophageal reflux disease between young and old adults in a Chinese population. World J Gastroenterol. 2011;17:4614-4618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Lee SW, Lien HC, Chang CS, Peng YC, Ko CW, Chou MC. Impact of body mass index and gender on quality of life in patients with gastroesophageal reflux disease. World J Gastroenterol. 2012;18:5090-5095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | An evidence-based appraisal of reflux disease management--the Genval Workshop Report. Gut. 1999;44 Suppl 2:S1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 547] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 7. | Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, Lundell L, Margulies M, Richter JE, Spechler SJ. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996;111:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 754] [Cited by in RCA: 790] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 8. | El-Serag H. The association between obesity and GERD: a review of the epidemiological evidence. Dig Dis Sci. 2008;53:2307-2312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 206] [Cited by in RCA: 190] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 9. | Iovino P, Angrisani L, Galloro G, Consalvo D, Tremolaterra F, Pascariello A, Ciacci C. Proximal stomach function in obesity with normal or abnormal oesophageal acid exposure. Neurogastroenterol Motil. 2006;18:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Wiklund I, Carlsson J, Vakil N. Gastroesophageal reflux symptoms and well-being in a random sample of the general population of a Swedish community. Am J Gastroenterol. 2006;101:18-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 106] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Kahrilas PJ, Howden CW, Wernersson B, Denison H, Nuevo J, Gisbert JP. Impact of persistent, frequent regurgitation on quality of life in heartburn responders treated with acid suppression: a multinational primary care study. Aliment Pharmacol Ther. 2013;37:1005-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Revicki DA, Zodet MW, Joshua-Gotlib S, Levine D, Crawley JA. Health-related quality of life improves with treatment-related GERD symptom resolution after adjusting for baseline severity. Health Qual Life Outcomes. 2003;1:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Kaplan-Machlis B, Spiegler GE, Revicki DA. Health-related quality of life in primary care patients with gastroesophageal reflux disease. Ann Pharmacother. 1999;33:1032-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Kahrilas PJ, Howden CW, Hughes N. Response of regurgitation to proton pump inhibitor therapy in clinical trials of gastroesophageal reflux disease. Am J Gastroenterol. 2011;106:1419-125; quiz 1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 116] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Kahrilas PJ, Jonsson A, Denison H, Wernersson B, Hughes N, Howden CW. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10:612-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Bredenoord AJ, Weusten BL, Curvers WL, Timmer R, Smout AJ. Determinants of perception of heartburn and regurgitation. Gut. 2006;55:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 215] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | Oh JH, Kim TS, Choi MG, Lee H, Jeon EJ, Choi SW, Lee C, Chung IS. Relationship between Psychological Factors and Quality of Life in Subtypes of Gastroesophageal Reflux Disease. Gut Liver. 2009;3:259-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Kulig M, Leodolter A, Vieth M, Schulte E, Jaspersen D, Labenz J, Lind T, Meyer-Sabellek W, Malfertheiner P, Stolte M. Quality of life in relation to symptoms in patients with gastro-oesophageal reflux disease-- an analysis based on the ProGERD initiative. Aliment Pharmacol Ther. 2003;18:767-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
P- Reviewer: Blonski W, Homan M, Lai YC S- Editor: Nan J L- Editor: A E- Editor: Ma S