Published online Aug 14, 2014. doi: 10.3748/wjg.v20.i30.10628
Revised: March 29, 2014
Accepted: April 30, 2014
Published online: August 14, 2014
Processing time: 241 Days and 20.3 Hours
AIM: To evaluate the frequency of use of various treatment modalities for Budd-Chiari syndrome (BCS) in China by conducting a preliminary survey of relevant literature.
METHODS: All papers regarding the treatment of BCS in Chinese patients were identified by searching PubMed, Chinese Scientific and Technological Journal, and China National Knowledge Infrastructure databases. Data regarding the number of BCS patients treated with different treatment modalities over time were collected. The proportions of BCS patients undergoing various treatment modalities were calculated.
RESULTS: Overall, 300 of 3005 papers initially retrieved were included. These papers included 23352 BCS patients treated with different treatment modalities. The treatment modalities include surgery (n = 8625), interventional treatment (n = 13940), surgery combined with interventional treatment (n = 363), medical therapy (n = 277), other treatments (n = 91), and no treatment (n = 56). After 2005, the number of BCS patients treated with surgery was drastically decreased, but the number of BCS patients who underwent interventional treatment was almost maintained. Shunt surgery was the most common type of surgery (n = 3610). Liver transplantation was rarely employed (n = 2). Balloon angioplasty with or without stenting was the most common type of interventional treatment (n = 13747). Transjugular intrahepatic portosystemic shunt was rarely employed (n = 81).
CONCLUSION: Selection of treatment modalities for BCS might be different between China and Western countries. Further work should be necessary to establish a unanimous therapeutic strategy for BCS in China.
Core tip: This preliminary survey of published literature demonstrated that the selection of treatment modalities for Budd-Chiari syndrome (BCS) might be different between China and Western countries. Balloon angioplasty with or without stenting, also known as percutaneous recanalization, was the most common treatment modality for BCS in China.
- Citation: Qi XS, Ren WR, Fan DM, Han GH. Selection of treatment modalities for Budd-Chiari Syndrome in China: A preliminary survey of published literature. World J Gastroenterol 2014; 20(30): 10628-10636
- URL: https://www.wjgnet.com/1007-9327/full/v20/i30/10628.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i30.10628
In 1845, George Budd, a British internist, for the first time described the classic clinical triad of abdominal pain, hepatomegaly, and ascites in three patients with hepatic venous thrombosis secondary to abscess-induced phlebitis[1]. In 1899, Hans Chiari, an Austrian pathologist, documented the histological features of another three cases with obliterative endophlebitis of the large hepatic veins[2]. Subsequently, the nomenclature for Budd-Chiari syndrome (BCS) originated from the family names of the two famous doctors[3]. Recently, the European Group for the Study of Vascular Disorders of the Liver standardized the definition of BCS as the hepatic venous outflow obstruction at any level from the small hepatic veins to the junction of the inferior vena cava and the right atrium[4]. Notably, right heart failure, constrictive pericarditis or hepatic veno-occlusive disease (also known as sinusoidal obstruction syndrome) should be excluded from the definition of BCS[5].
Accumulated evidence demonstrated that the causes of BCS might be substantially different between Western countries and China. For example, more than 80% of Western patients had at least one thrombotic risk factor[5-7]; by contrast, thrombotic risk factors were rarely observed in Chinese patients[8-13]. In addition, the obstructive location was the hepatic vein in most of Western patients; contrarily, the combined obstruction of the hepatic vein and inferior vena cava was more common in Chinese patients[14]. Accordingly, it could be hypothesized that the different causes and types of obstruction might lead to the difference in the selection of treatment modalities for BCS between the two regions.
Although China might have the largest number of BCS patients in the world[15], no data have been systematically presented regarding the selection of treatment modalities for BCS in China. Herein, we conducted a preliminary survey of literature to evaluate the frequency of use of various treatment modalities for BCS in China.
As previously described[10,15,16], the PubMed database, the Chinese Scientific and Technological Journal (VIP) database, and the China National Knowledge Infrastructure database were searched from the database inception to February 20, 2012. The search items were the combination of “Budd Chiari” and “China”[15].
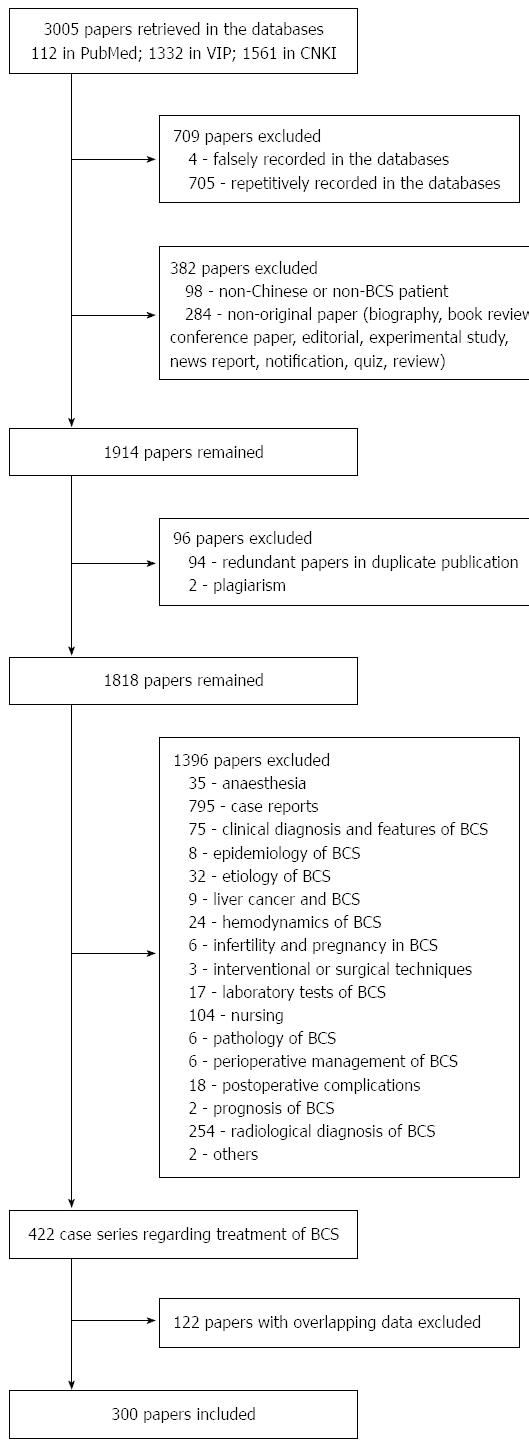
First, all full text copies of retrieved articles were obtained. Papers that were falsely or repetitively recorded in the three databases were excluded.
Second, papers regarding neither Chinese nor BCS patients were excluded.
Third, the clinical studies were identified. The other types of papers, such as notification, book review, biography, news report, quiz, review, editorial, conference paper and experimental studies, were excluded.
Fourth, the redundant papers from the covert duplicate publication and plagiarism were excluded.
Fifth, the clinical studies regarding the treatment of BCS were included. The clinical studies regarding other fields, such as anaesthesia, clinical or radiological diagnosis and features, epidemiology, etiology, hemodynamics, infertility and pregnancy in BCS, interventional or surgical techniques, laboratory tests, liver cancer and BCS, nursing, pathology of BCS, perioperative management, postoperative complications and prognosis, were also excluded. Additionally, case reports (< 10 patients) were excluded.
Sixth, among the studies with overlapping data, the studies with more extensive enrollment period and larger sample size were finally included in the present systematic review.
The primary items included first author’s region and affiliation, year of publication, number of patients, treatment modalities (i.e., surgery, interventional treatment, combination of interventional treatment and surgery, medical treatment, other treatments or no treatment) and type of surgery and interventional treatment. The secondary items included sex and age of patients, type of BCS, treatment-related complications and death, efficacy, follow-up time and survival. Notably, because most of included papers reported the combined outcome of various treatment modalities (i.e., interventional treatment and surgery) in patients with different types of BCS, it is often impossible for the review authors to extract the data regarding the safety and efficacy of individual treatment modality.
The data were reported in text and Excel table. The number and percentage of BCS patients treated with different treatment modalities and the number of BCS papers according to the publication year were shown in bar and line charts. Additionally, the frequencies of use of different types of surgery and interventional treatment were shown in pie charts.
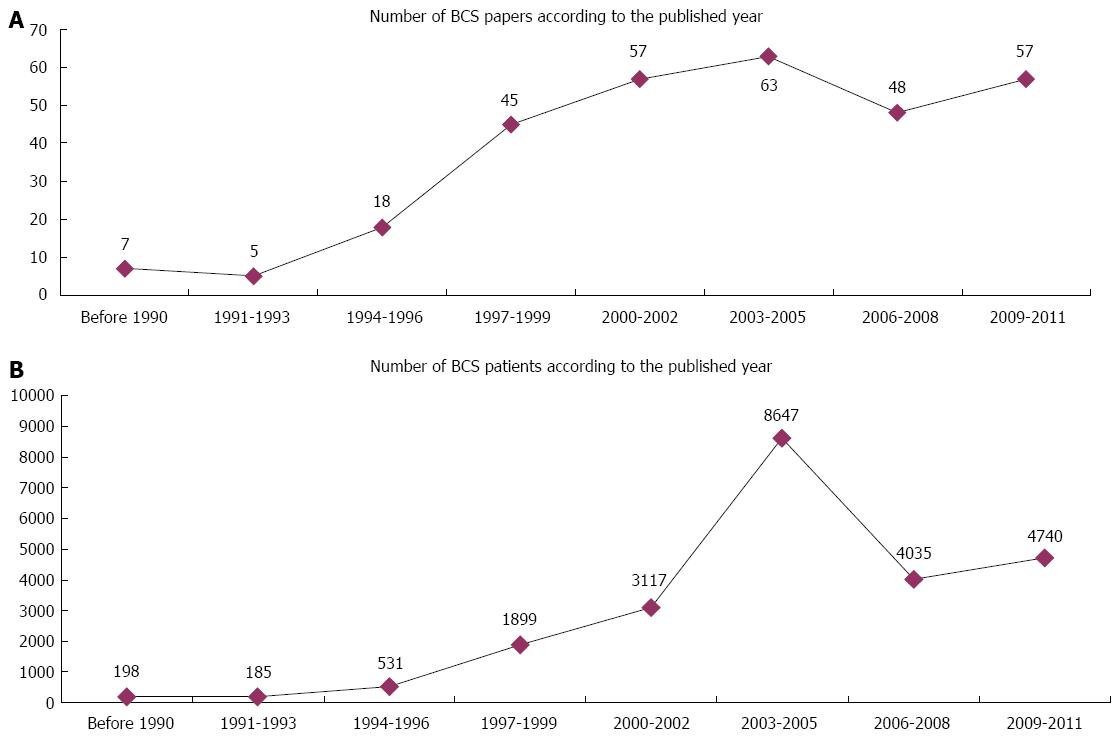
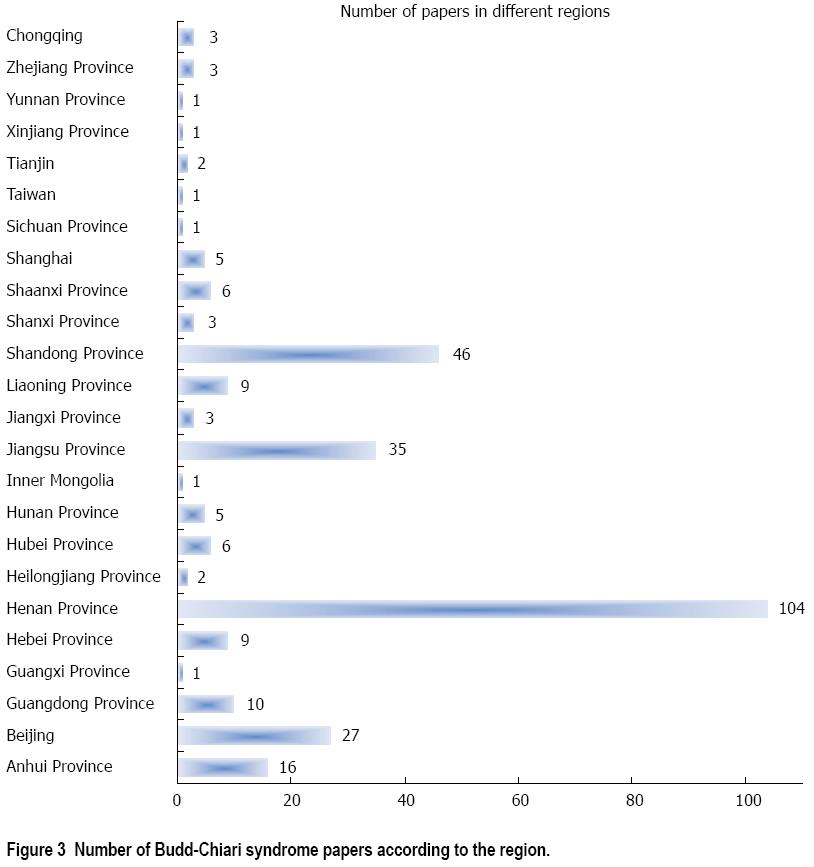
A total of 3005 papers were initially retrieved from the three databases. Among them, 300 papers were included in the systematic review (Figure 1). The number of BCS papers and patients reported gradually increased over time (Figure 2). Notably, the numbers of BCS papers and patients reported during the period of 2003-2005 were the largest. Additionally, the majority of BCS papers were written by researchers from Henan (35%), Shandong (15%), Jiangsu (12%), Beijing (9%) and Anhui (5%) provinces (Figure 3). These papers were produced by 151 affiliations (Table 1). Notably, the First Affiliated Hospital of Zhengzhou University (Zhengzhou, Henan province) had the largest number of papers per affiliation (n = 33).
| Item | Number of affiliations |
| No. papers = 1 | 102 |
| No. papers = 2 | 26 |
| No. papers = 3 | 8 |
| No. papers = 4 | 6 |
| No. papers = 6 | 2 |
| No. papers = 7 | 2 |
| No. papers = 8 | 1 |
| No. papers = 9 | 1 |
| No. papers = 10 | 1 |
| No. papers = 12 | 1 |
| No. papers = 33 | 1 |
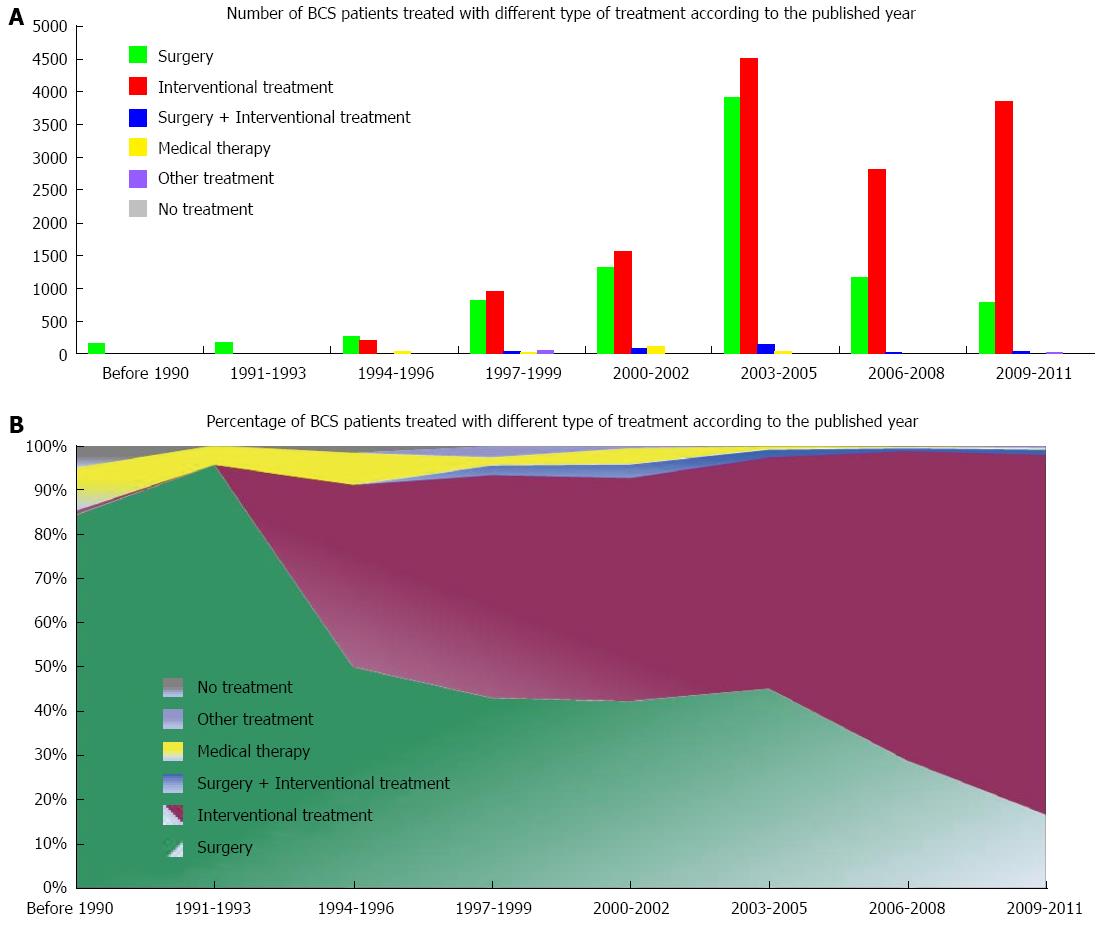
A total of 23352 BCS patients treated with various treatment modalities were reported in these included papers. The treatment modalities include surgery (n = 8625), interventional treatment (n = 13940), surgery combined with interventional treatment (n = 363), medical therapy (n = 277), other treatments (n = 91) and no treatment (n = 56). The trend in the number of BCS patients treated with various types of treatment modalities over time is described in Figure 4A. Before 2005, the number of BCS patients treated with surgery and interventional treatment gradually increased over time. Since then, the number of BCS patients treated with surgery drastically decreased, but the number of BCS patients who underwent interventional treatment was almost maintained. Before 1996, the number of BCS patients treated with surgery was larger than that with interventional treatment (610 vs 220). However, this case was reversed after 1996 (8015 vs 13720).
The trend in the percentage of BCS patients treated with various types of treatment modalities over time is descried in Figure 4B. Notably, the percentage of BCS patients treated with surgery persistently decreased; contrarily, the percentage of BCS patients who underwent interventional treatment gradually increased.
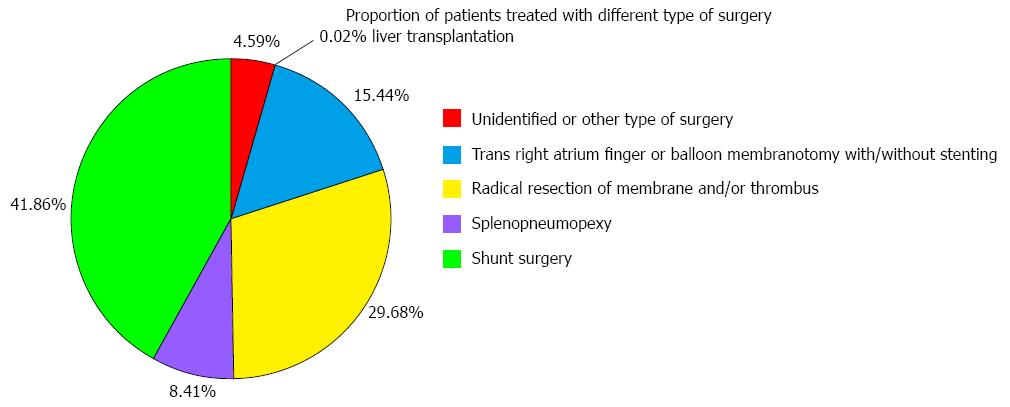
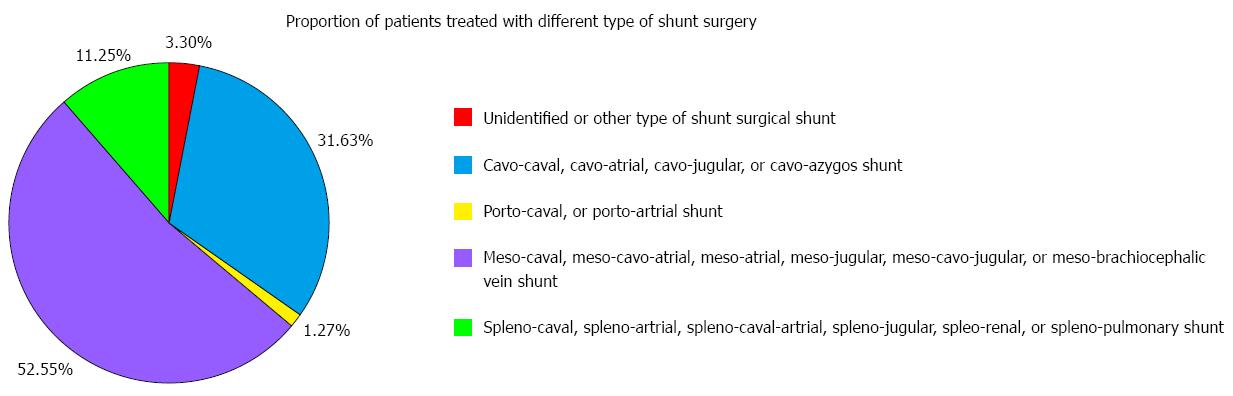
The proportion of BCS patients treated with various types of surgery is described in Figure 5. The most common type of surgery used in China was shunt surgery (n = 3610), followed by radical resection of membrane and/or thrombus (n = 2560), trans-right atrium finger or balloon membranotomy with or without stenting (n = 1332), and others (n = 1123). Notably, liver transplantation was rarely employed (n = 2). Additionally, the proportion of BCS patients treated with various types of shunt surgery is described in Figure 6. Meso-caval, meso-cavo-atrial, meso-atrial, meso-jugular, meso-cavo-jugular, and meso-brachiocephalic vein shunts were the most common types of shunt surgery (n = 1897).
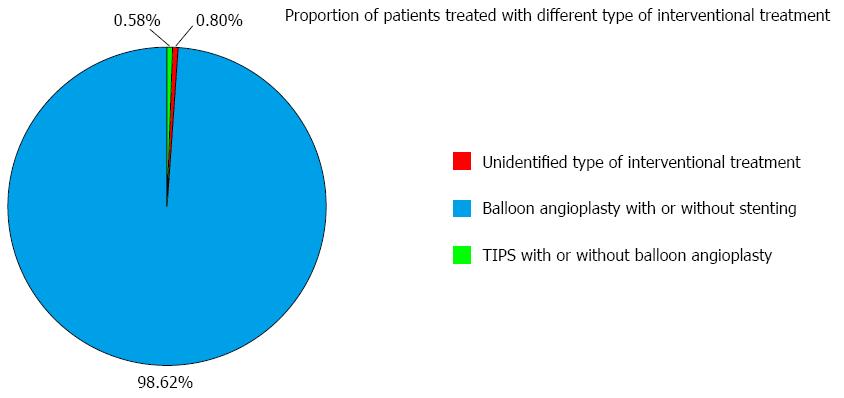
The proportion of BCS patients who underwent various types of interventional treatment is described in Figure 7. Balloon angioplasty with or without stenting, also known as percutaneous recanalization, was the most common type of interventional treatment (n = 13747). However, transjugular intrahepatic portosystemic shunt (TIPS) in combination with or without percutaneous recanalization was rarely employed (n = 81).
To date, no randomized controlled trials regarding the selection of treatment modalities for BCS have been performed due to the rarity of this disease[4-7,17]. Accordingly, the current American Association for the Study of Liver Diseases recommendations and European Group for the Study of Hepatic Vascular Diseases consensus for the treatment of BCS originate from results of cohort studies and expert opinions[4,7]. In Western countries, a step-wise therapeutic strategy aimed at minimal invasiveness has been developed and widely employed[18-20]. This strategy mainly consists of four major steps. First, anticoagulation is employed for the recanalization of hepatic venous thrombosis and prevention of recurrent thrombosis, and diuretics is used for the treatment of ascites. Second, percutaneous recanalization of hepatic veins and/or the inferior vena cava is attempted in cases of failure of medical therapy. Third, TIPS is performed in the absence of response to previous therapy. Fourth, liver transplantation is further considered in patients with progressive diseases. Recently, a large prospective case series has confirmed the efficacy of the therapeutic strategy in Western BCS patients[19,20]. Importantly, medical therapy and TIPS placement have become the mainstay treatment options for BCS in Western countries. The proportions of BCS patients treated with medical therapy, percutaneous recanalization, TIPS and liver transplantation are 40%, 10%, 40%, and 10%, respectively[19,20]. In addition, it should be noted that surgery has been gradually replaced, and percutaneous recanalization is infrequently used for the management of BCS.
Whether or not Western experiences should be extrapolated to the management of Chinese BCS patients remains unclear. However, the fact suggests that the treatment selection seems to be different between Western countries and China. Our single-center case series of 177 BCS patients has recently demonstrated that percutaneous recanalization alone can achieve excellent long-term patency and survival in most Chinese patients with BCS[21]. The safety and efficacy of balloon angioplasty with or without stent-placement in Chinese patients are further confirmed by a larger experience of 903 cases treated with endovascular techniques[22]. Additionally, a Chinese single-center case series of 1360 BCS patients shows that the patients treated with surgery have excellent long-term survival with low perioperative death and complication rates[23]. The wide application of surgery and percutaneous recanalization in China is ascertained by a multi-center experience of 2564 patients[24]. Thus, the substantial discrepancy in the selection of treatment modalities impels us to further conduct the present study.
To the best of our knowledge, this study is the first systematic analysis of the literature regarding the selection of treatment modalities for BCS in China. Several important findings are as follows.
First, more than 20000 Chinese BCS patients treated with various treatment modalities have been reported.
Second, surgery and interventional treatment are the most common treatment modalities for BCS in China. Currently, interventional treatment is more common than surgery in Chinese BCS patients.
Third, unlike Western patients, very few Chinese patients are treated with medical therapy alone or liver transplantation. Surgical shunt, especially meso-caval, meso-cavo-atrial, meso-jugular, or meso-brachiocephalic vein shunt, is the most common type of surgery used in China. The reason why medical therapy alone is rarely employed in China might be attributed to the two following points: (1) In contrast with Western BCS patients who often have HV thrombosis, IVC obstruction is frequently observed in Chinese BCS patients. Anticoagulation therapy appears to be less effective for the recanalization of IVC obstruction; and (2) Most of Chinese patients have a relatively chronic disease course and live in poverty. Only if they present with relatively severe symptoms, these patients would be referred to the hospital and treated with more invasive treatment modalities.
Fourth, unlike Western patients, very few Chinese patients are treated with TIPS. Balloon angioplasty with or without stenting is the most common interventional treatment modality used in China. This inconsistent phenomenon might be explained by the three following points. First, TIPS procedure is applied only in some highly experienced interventional radiological centers[25], rather than widely in all Chinese medical centers[26,27]. By comparison, shunt surgery remains a mainstay treatment modality for BCS in China[23,24]. Second, percutaneous recanalization could achieve a relatively excellent outcome in Chinese BCS patients[21,22,28]. Thus, TIPS might be unnecessary in most of cases. Finally, the site of obstruction and etiological distribution are potentially different between China and Western countries[8-13].
Fifth, liver transplantation is rarely employed in BCS patients. This might be associated with a very high cost of this surgery for poor Chinese BCS patients and the shortage of donor organs. Collectively, our findings suggest that China may have a relatively large number of BCS patients treated, and the preferred treatment modalities for BCS are different between Western countries and China.
Our study has several strengths. First, literature retrieval is comprehensive, and one English-language database and two Chinese-language databases were searched. Second, all full-text copies are reviewed to avoid omitting the potentially eligible articles. Third, the eligibility criteria are strict. The papers unrelated to the treatment of BCS, as well as those with overlapping data, are excluded.
Several limitations should be also clarified as follows. First, the number of BCS patients reported in the published literature may not fully reflect the actual number of BCS patients treated in the real world. Thus, the number of BCS patients might be underestimated. Certainly, the difficulty of performing a nationwide investigation is huge. Second, the major goal of this preliminary survey is just to analyze the frequency of use of various treatment modalities. But we have to acknowledge that other important issues, such as the safety and efficacy of various treatment modalities and prognosis of BCS patients, are not evaluated due to the difficulty in data collection. Indeed, we initially intended to collect the data regarding the efficacy and safety. However, the work was largely restricted by the following aspects: (1) type of BCS, follow-up length, and criteria for assessing the efficacy and safety were different among studies; (2) only the combined outcomes of all treatment modalities were reported in studies in which the patients underwent different treatment modalities, but the separate outcome of individual treatment modality could not be extracted; and (3) the information regarding the number of patients who were lost to follow-up was often unavailable.
In conclusion, this preliminary survey shows the following features of the selection of treatment modalities in Chinese BCS patients: (1) medical therapy alone is infrequently used in China; (2) balloon angioplasty with or without stenting is the preferred treatment modality in China, but TIPS placement is rarely employed; (3) liver transplantation is very rare in China; and (4) although the number of patients treated with surgery gradually decreases, surgery remains the mainstay treatment modality. Given the substantial difference in the selection of treatment between China and Western countries, further work should be conducted to establish a unanimous therapeutic strategy for BCS in China.
A step-wise therapeutic strategy for Budd-Chiari syndrome (BCS) has been widely employed in Western patients, including medical therapy, percutaneous recanalization, transjugular intrahepatic portosystemic shunt (TIPS) and liver transplantation. Given the difference in the etiology and obstructive location of BCS between Western countries and China, it remains unclear whether or not Western experiences should be extrapolated to the management of Chinese BCS patients.
In West countries, medical therapy and TIPS placement have become the mainstay treatment options for BCS. The proportions of BCS patients treated with medical therapy, percutaneous recanalization, TIPS and liver transplantation are 40%, 10%, 40%, and 10%, respectively.
This study is the first systematic analysis of the literature regarding the selection of treatment modalities for BCS in China. Medical therapy alone is infrequently used in China. Balloon angioplasty with or without stenting is the preferred treatment modality in China, but TIPS placement is rarely employed. Liver transplantation is very rare in China. Although the number of patients treated with surgery gradually decreases, surgery remains the mainstay treatment modality.
Given the substantial difference in the selection of treatment between China and Western countries, further work should be conducted to establish a unanimous therapeutic strategy for BCS in China.
The authors searched a very large number of relevant papers and systematically evaluate the frequency of use of different treatment modalities in Chinese patients with Budd-Chiari syndrome. They found that selection of treatment was different between China and Western countries. These results are useful to recognize the current status about the selection of treatment in Chinese patients with Budd-Chiari syndrome.
| 1. | Budd G. Diseases of the liver. London: John Churchill 1945; . |
| 2. | Chiari H. Ueber die selbstandige Phlebitis obliterans der Hauptstammeder Venae hepaticae als Todesursache. Beitr Z Pathol Anat U Z Allg Pathol. 1899;26:1-18. |
| 3. | Okuda K, Kage M, Shrestha SM. Proposal of a new nomenclature for Budd-Chiari syndrome: hepatic vein thrombosis versus thrombosis of the inferior vena cava at its hepatic portion. Hepatology. 1998;28:1191-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 116] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Janssen HL, Garcia-Pagan JC, Elias E, Mentha G, Hadengue A, Valla DC. Budd-Chiari syndrome: a review by an expert panel. J Hepatol. 2003;38:364-371. [PubMed] |
| 5. | Valla DC. Primary Budd-Chiari syndrome. J Hepatol. 2009;50:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 221] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | De Stefano V, Martinelli I. Splanchnic vein thrombosis: clinical presentation, risk factors and treatment. Intern Emerg Med. 2010;5:487-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 95] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 739] [Cited by in RCA: 669] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 8. | Cheng D, Xu H, Lu ZJ, Hua R, Qiu H, Du H, Xu X, Zhang J. Clinical features and etiology of Budd-Chiari syndrome in Chinese patients: a single-center study. J Gastroenterol Hepatol. 2013;28:1061-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (2)] |
| 9. | Qi X, He C, Han G, Yin Z, Wu F, Zhang Q, Niu J, Wu K, Fan D. Prevalence of paroxysmal nocturnal hemoglobinuria in Chinese patients with Budd-Chiari syndrome or portal vein thrombosis. J Gastroenterol Hepatol. 2013;28:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Qi X, Wu F, Ren W, He C, Yin Z, Niu J, Bai M, Yang Z, Wu K, Fan D. Thrombotic risk factors in Chinese Budd-Chiari syndrome patients. An observational study with a systematic review of the literature. Thromb Haemost. 2013;109:878-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Qi X, Yang Z, Bai M, Shi X, Han G, Fan D. Meta-analysis: the significance of screening for JAK2V617F mutation in Budd-Chiari syndrome and portal venous system thrombosis. Aliment Pharmacol Ther. 2011;33:1087-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Qi X, Zhang C, Han G, Zhang W, He C, Yin Z, Liu Z, Bai W, Li R, Bai M. Prevalence of the JAK2V617F mutation in Chinese patients with Budd-Chiari syndrome and portal vein thrombosis: a prospective study. J Gastroenterol Hepatol. 2012;27:1036-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Wang H, Sun G, Zhang P, Zhang J, Gui E, Zu M, Jia E, Xu H, Xu L, Zhang J. JAK2 V617F mutation and 46/1 haplotype in Chinese Budd-Chiari syndrome patients. J Gastroenterol Hepatol. 2014;29:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Valla DC. Hepatic venous outflow tract obstruction etiopathogenesis: Asia versus the West. J Gastroenterol Hepatol. 2004;19:S204-S211. |
| 15. | Qi X, Ren W, Liu L, Yang Z, Yang M, Fan D, Han G. Prevalence of covert duplicate publications in Budd-Chiari syndrome articles in China: a systematic analysis. Am J Med. 2013;126:633-9.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 16. | Qi X, Wang J, Ren W, Bai M, Yang M, Han G, Fan D. Familial Budd-Chiari Syndrome in China: A Systematic Review of the Literature. ISRN Hepatol. 2013;2013:7. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Qi X, Jia J, Ren W, Yang M, De Stefano V, Wang J, Fan D. Scientific publications on portal vein thrombosis and Budd-Chiari syndrome: a global survey of the literature. J Gastrointestin Liver Dis. 2014;23:65-71. [PubMed] |
| 18. | Plessier A, Sibert A, Consigny Y, Hakime A, Zappa M, Denninger MH, Condat B, Farges O, Chagneau C, de Ledinghen V. Aiming at minimal invasiveness as a therapeutic strategy for Budd-Chiari syndrome. Hepatology. 2006;44:1308-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 198] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 19. | Darwish Murad S, Plessier A, Hernandez-Guerra M, Fabris F, Eapen CE, Bahr MJ, Trebicka J, Morard I, Lasser L, Heller J. Etiology, management, and outcome of the Budd-Chiari syndrome. Ann Intern Med. 2009;151:167-175. [PubMed] |
| 20. | Seijo S, Plessier A, Hoekstra J, Dell’era A, Mandair D, Rifai K, Trebicka J, Morard I, Lasser L, Abraldes JG. Good long-term outcome of Budd-Chiari syndrome with a step-wise management. Hepatology. 2013;57:1962-1968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 233] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 21. | Han G, Qi X, Zhang W, He C, Yin Z, Wang J, Xia J, Xu K, Guo W, Niu J. Percutaneous recanalization for Budd-Chiari syndrome: an 11-year retrospective study on patency and survival in 177 Chinese patients from a single center. Radiology. 2013;266:657-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 22. | Meng QY, Sun NF, Wang JX, Wang RH, Liu ZX. Endovascular treatment of Budd-Chiari syndrome. Chin Med J (Engl). 2011;124:3289-3292. [PubMed] |
| 23. | Xu PQ, Ma XX, Ye XX, Feng LS, Dang XW, Zhao YF, Zhang SJ, Zhao LS, Tang Z, Lu XB. Surgical treatment of 1360 cases of Budd-Chiari syndrome: 20-year experience. Hepatobiliary Pancreat Dis Int. 2004;3:391-394. [PubMed] |
| 24. | Wang ZG, Zhang FJ, Yi MQ, Qiang LX. Evolution of management for Budd-Chiari syndrome: a team’s view from 2564 patients. ANZ J Surg. 2005;75:55-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Qi X, Yang M, Fan D, Han G. Transjugular intrahepatic portosystemic shunt in the treatment of Budd-Chiari syndrome: a critical review of literatures. Scand J Gastroenterol. 2013;48:771-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Qi X, Guo W, He C, Zhang W, Wu F, Yin Z, Bai M, Niu J, Yang Z, Fan D. Transjugular intrahepatic portosystemic shunt for Budd-Chiari syndrome: techniques, indications and results on 51 Chinese patients from a single centre. Liver Int. 2013;Oct 12; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 27. | Wu X, Ding W, Cao J, Han J, Li J. Modified transjugular intrahepatic portosystemic shunt in the treatment of Budd-Chiari syndrome. Int J Clin Pract. 2010;64:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Zhang CQ, Fu LN, Xu L, Zhang GQ, Jia T, Liu JY, Qin CY, Zhu JR. Long-term effect of stent placement in 115 patients with Budd-Chiari syndrome. World J Gastroenterol. 2003;9:2587-2591. [PubMed] |
P- Reviewer: Cura M, Han GH, Jeng KS S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Ma S