Published online May 28, 2014. doi: 10.3748/wjg.v20.i20.6309
Revised: February 23, 2014
Accepted: March 19, 2014
Published online: May 28, 2014
Processing time: 233 Days and 9.7 Hours
AIM: To assess outcomes after colonic stent insertion for obstructing colorectal malignancies performed by an endoscopist without radiologist support.
METHODS: This is a retrospective study of all stents inserted by a single surgeon in a District General Hospital over an eight year period. All stents were inserted for patients with acute large bowel obstruction secondary to a malignant colorectal pathology either for palliation or as a bridge to surgery. Procedures were performed by a single surgeon endoscopically with fluoroscopic control in the X-ray department but without the support of an interventional radiologist. Data was collected prospectively on a pre-designed database.
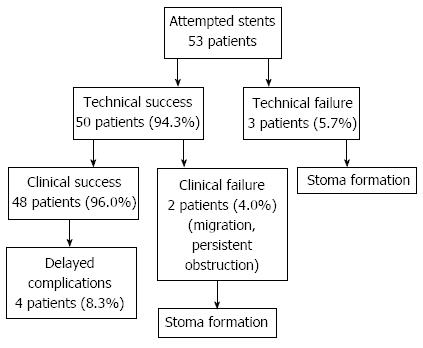
RESULTS: The indication for all stent procedures was an obstructing colorectal malignancy. Out of 53 patients, the overall success rate was 90.6%. Eight patients had a stent intended as a bridge to surgery and 45 as a palliative procedure. Technical success was achieved in 50 out of 53 procedures (94.3%) and clinical success in 48 of those remaining 50 (96.0%). Those with unsuccessful technical or clinical procedures went on to have defunctioning stomas to treat their obstruction. There were six complications from the technically successful stents (12.0%). These included one migration, one persisting obstructive symptoms and four cases of tumour overgrowth of the stents at a later date. Haemorrhagic complications, perforation or mortality were not observed in our series. Our results are comparable to several other studies assessing stent outcomes for obstructing bowel cancer.
CONCLUSION: Our data suggests that colorectal stents can be inserted without radiologist support by an adequately trained individual with good outcomes.
Core tip: There is now a good amount of evidence showing that colonic stents are a safe management option for obstruction secondary to colonic malignancy despite other safety concerns in the literature. Despite guideline recommendations that they should be performed as a joint procedure with both an endoscopist and radiologist, limitations of everyday practice may restrict this. Our data shows that procedures can be performed just as safely by only an endoscopist with good success rates and few complications. This may help improve availability of such procedures and reduced financial costs.
- Citation: Mehmood RK, Parker J, Kirkbride P, Ahmed S, Akbar F, Qasem E, Zeeshan M, Jehangir E. Outcomes after stenting for malignant large bowel obstruction without radiologist support. World J Gastroenterol 2014; 20(20): 6309-6313
- URL: https://www.wjgnet.com/1007-9327/full/v20/i20/6309.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i20.6309
The National Institute of Clinical Excellence (NICE) guidelines have recommended the establishment of facilities in acute surgical admission units to allow the placement of colonic stents for patients with large intestinal obstruction as an alternative to emergency surgery[1]. It is widely accepted that endoscopic stents are a safe technique in the treatment of large bowel obstruction[2-6]. Colonic cancer is common in the United Kingdom with over 40000 people being diagnosed every year[7] and as up to 70% occur in the left side of the colon, stents for obstructing lesions can often be an option[8]. They can present in a variety of ways but a significant proportion will be diagnosed in the acute care setting with symptoms of colonic obstruction that can result in major morbidity or mortality. Up to 1 in 4 patients with colorectal cancer will present with obstruction[9] and at this time patients may be significantly unwell making the traditional option of major surgical intervention risky with mortality rates between 10% to 30%[10]. Stents can be an alternative to emergency surgery either as a palliation method or as a strategy to delay surgery until a safer time and avoid unnecessary risks. Other advantages in addition to patient optimisation include time to allow accurate disease staging, a reduced risk of either temporary or permanent stomas (and hence better quality of life), adequate opportunity to counsel the patient and reduced health care costs[11]. NICE have recognised the use of stents in an emergency setting and recommend that provisions for them should be available in departments dealing with such surgical emergencies[1].
As with all procedures there are potential risks and these commonly include technical or clinical failure, perforation, stent migration or haemorrhagic complications[2-6]. Tumour cell dissemination can also be a concern[12]. Stents are also expensive in terms of equipment cost and specialist training for staff although there is evidence that stent insertion followed by elective surgery is more cost effective than primary emergency surgery[13]. Clinical success rates for emergency colonic stenting are thought to be up to 76% with an overall mortality of 0.58%[6].
Stents should be inserted by appropriately trained individuals and NICE, in addition to other literature recommend the combination of an interventional radiologist and endoscopist working together[1,11]. The Interdisciplinary Canadian Guidelines on the use of metal stents in the gastrointestinal tract for oncological indications[11] do not recommend endoscopist only procedures although in practicality this may not be adhered to by all centres. The department included in the study is a laparoscopic colorectal unit run according to NICE recommendations except for the absence of radiological support for endoscopic stents. This paper is the first to evaluate the outcomes of colonic stents without the input of a radiologist which may provide benefits in procedure provision and cost. Our aim is to assess the success and complications rates in procedures performed by an endoscopist alone in a District General Hospital (DGH).
This is a retrospective study of all colorectal stents inserted by one consultant colorectal surgeon in a single DGH. Data was collected between December 2004 and August 2012 by a Colorectal Specialist Nurse on a pre designed proforma and collated onto a database. The performing consultant reviewed and validated all the collected data. All patients who received colonic stents within this period for obstructing colonic malignancy were included in the analysis.
Stents were inserted by a single consultant surgeon using a variety of devices which were all inserted in accordance with the manufacturer’s guidelines. The majority were Cooks® or Pennamed® colorectal stents. Two sizes (8 cm and 10 cm) were used and were inserted to include at least 2 cm overlap for the proximal and distal margins (Table 1). Their diameter was 2.4 cm. Stents were uncovered and inserted through the scope.
| Example tumour size (cm) | Stent size (cm) | Covered/ uncovered | Through the scope (TIS) | Stent diameter (cm) |
| 3 | 8 | Uncovered | Yes | 2.4 |
| 5 | 10 | Uncovered | Yes | 2.4 |
All were inserted endoscopically with fluoroscopic guidance in the X-ray department. Data collected included indications for stenting, technical and clinical success and complications. Basic statistical analysis was performed.
During the study period a total of 53 patients received a colonic stent. The indication for in all patients was for an obstructing large bowel malignancy presenting as an emergency. Of these, eight were intended as a bridge to surgery and 45 were inserted for palliation.
Technical success was achieved in 50 out of 53 patients (94.3%) with 3 failed procedures who went on to have defunctioning stomas to treat their obstruction. Out of the 50 that were technically successful, 48 went on to be clinically successful in the immediate follow up period (96.0%). The two that were unsuccessful were secondary to persisting obstructive symptoms and stent migration. They both went on to have a stoma. Delayed complications after initial clinical success occurred in four patients and these were all due to tumour overgrowth at the distal end of the stent. All these patients had an attempted second stent but all unfortunately failed. They also went on to have stomas. This gives an overall immediate and delayed complication rate of 6 out of 50 procedures (12.0%). These results are summarised in Table 2 and Figure 1.
| Complication | Number (out of 50 patients) | Management |
| Early complications | ||
| Stent migration | 1 (2.0) | Stoma formation |
| Late complications | ||
| Persistent obstructive symptoms | 1 (2.0) | Stoma formation |
| Tumour overgrowth on distal end of stent | 4 (8.0) | All had failed re stenting and went on to have stomas |
Most stents were performed for palliation and these patients survived for a few weeks and either died peacefully at home or occasionally readmitted and died in hospital. Patients who received bridging stents had surgery performed in next two three weeks or as previously planned.
Haemorrhagic complications or perforation were not seen on any occasion and there were no mortalities secondary to stent insertion. If there were no complications then patients were discharged the day after their bowels had worked with the stent in situ. There were no noted operative difficulties due to the stent in those patients who went on to have further surgery.
Colonic stents are now widely accepted as a useful alternative for managing malignant large bowel obstruction and have been in use for over 10 years[2-4,6,14]. There have been some concerns over safety and several studies have required early cessation due to this[15-16]. However several papers have now published reassuring results with low complication rates[2,6]. It seems to be a useful technique in appropriate patients to avoid the high risks of mortality and morbidity and to reduce health care costs of emergency surgery. A randomised control trial however is still awaited and as a recent systematic review has noted, there are few papers regarding stents with good sample sizes clearly limiting the quality and validity of evidence for their benefits[17]. The overall consensus from one study is that technical and clinical success rates were lower than anticipated[17].
Literature has only been published regarding centres performing stents with the combined efforts of both endoscopic and radiological interventionalists[2,6]. Our series looks at using only an endoscopist who is a consultant colorectal surgeon which may reduce service and financial pressures on the health service. This may be the standard practice in many centres already despite the absence of data assessing its safety.
Our technical success, clinical success and complication rates are comparable to papers published using techniques involving the two parties[2-4,6]. Blake et al[2] reported a technical and clinical success rate of 86% and 84% respectively and our data exceeds both of these. Complications were reported in 22.5% of their cases and our rate is much lower.
Sebastian et al[6] reported perforation rates at 3.8%, migration rates of 11.8% and recurrent obstruction of 7.3% in a pooled analysis of 54 studies and complications reported here are lower. The technical failures went on to have stomas as an alternative method of relieving their obstruction as in our series.
The alternative strategy of emergency surgery in these patients with the likely use of either a temporary or permanent stoma has much higher risks especially in the cohort of often elderly and compromised patients who present with malignant bowel obstruction. Mortality of emergency surgery can be between 10%-30% depending on the patient (compared to 0% in our study) with morbidity rates as high as 39%[10]. Stents can help avoid surgery in those where it is not appropriate or allow adequate time for pre operative preparation, counselling and staging for those who are suitable for further intervention. It is important to highlight here however, that each patient should always be assessed on an individual basis and the most appropriate course of action taken. The use of emergency surgery instead of a stent should not be thought of as an unsuccessful management[18].
From our series the success rates are high and complication rates low which is comparable with similar studies suggesting that radiological support is not necessary in the presence of an adequately trained endoscopist. Our data does not agree with recent data suggesting that complications can occur in up to a third of procedures[19]. This may improve availability and costs of the procedure due to fewer necessary staff and may justify this method wherever it is already used. Colonic stents have only been used for around 10 years so it is reasonable to suggest that the success and complication figures will improve as the learning curve progresses.
Colonic stents have been shown to be cost effective in a study by Targownik et al[13]. It was associated with a mean lower cost per patient, less operations, lower mortality and an 83% reduction in stoma requirement[13]. Any procedure not requiring a radiologist would only be cheaper. There still will be significant time and cost for training and materials in any service developing provisions for stents but it is likely to be cost effective in the long term.
Our study adds to the current data confirming that colonic stents in acute obstruction secondary to bowel cancer are a successful and safe strategy. It is appropriate for this to be done without radiologist support with a good success rate and without higher than expected adverse events providing the endoscopist is adequately experienced. In the study hospital, there was only one surgeon with stenting experience. His lowest success rate is around 94.3% and others performing similar techniques should publish their data for comparison. Those appropriately trained could provide this service with hopefully an increased provision and reduced costs for this procedure due to the absence of radiology support.
We are very grateful to Patricia Kirbride, Janette Southward, Gill Wilkinson and Anne Skinner for their kind support throughout.
Colonic stenting is a widely used technique to relieve bowel obstruction either in palliation or as a bridge to surgery. It can help avoid major surgery in acutely unwell patients. Guidelines advise these procedures are performed by both an endoscopist and radiologist which provides logistical and financial issues. There is currently no evidence regarding the outcomes of patients who have stents placed by an endoscopist alone.
The safety and efficacy of stent insertion by an endoscopist alone has not been proven. The success rates and outcomes need to be assessed in order to ensure that this technique is safe. Papers have published on joint procedures but this is the first regarding procedures without radiologist support.
Stents are an excellent alternative in suitable patients to prevent the need of major surgical intervention in emergency bowel obstruction. Several previous studies have described its safety and efficacy and it is now widely used in emergency surgical practice.
The encouraging outcome of this paper shows that colonic stents can safely be inserted by an endoscopist without radiology support. This will provide an evidence base for centres already using this technique and may help change practice in other centres thereby reducing associated logistical and financial burdens.
The patients involved are relatively few and from a single centre. The application of these results depends on having an adequately experienced and skilled endoscopist. The outcomes from this study are comparable to evidence published for joint procedures suggesting that this technique can be safely employed in appropriate centres.
| 1. | NICE guidelines. Colorectal cancer: The diagnosis and management of colorectal cancer. Available from: http://www.nice.org.uk/nicemedia/pdf/CSGCCfullguidance.pdf. |
| 2. | Blake P, Delicata R, Cross N, Sturgeon G, Hargest R. Large bowel obstruction due to colorectal carcinoma can be safely treated by colonic stent insertion--case series from a UK district general hospital. Colorectal Dis. 2012;14:1489-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Baron TH, Dean PA, Yates MR, Canon C, Koehler RE. Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc. 1998;47:277-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 186] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Mainar A, De Gregorio Ariza MA, Tejero E, Tobío R, Alfonso E, Pinto I, Herrera M, Fernández JA. Acute colorectal obstruction: treatment with self-expandable metallic stents before scheduled surgery--results of a multicenter study. Radiology. 1999;210:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 130] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Stefanidis D, Brown K, Nazario H, Trevino HH, Ferral H, Brady CE, Gross GW, Postoak DW, Chadhury R, Rousseau DL. Safety and efficacy of metallic stents in the management of colorectal obstruction. JSLS. 2005;9:454-459. [PubMed] |
| 6. | Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004;99:2051-2057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 413] [Article Influence: 18.8] [Reference Citation Analysis (1)] |
| 7. | Available from: http://info.cancerresearchuk.org/cancerstats/types/bowel. |
| 8. | Fielding LP, Phillips RK, Fry JS, Hittinger R. Prediction of outcome after curative resection for large bowel cancer. Lancet. 1986;2:904-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 128] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Bhutani MS. Acute hemoperitoneum in an alcoholic man with ascites. Hosp Pract (1995). 1995;30:16G. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 365] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 10. | Riedl S, Wiebelt H, Bergmann U, Hermanek P. Postoperative complications and fatalities in surgical therapy of colon carcinoma. Results of the German multicenter study by the Colorectal Carcinoma Study Group. Chirurg. 1995;66:597-606. [PubMed] |
| 11. | Baerlocher MO, Asch MR, Dixon P, Kortan P, Myers A, Law C. Interdisciplinary Canadian guidelines on the use of metal stents in the gastrointestinal tract for oncological indications. Can Assoc Radiol J. 2008;59:107-122. [PubMed] |
| 12. | Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94:1151-1154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 13. | Targownik LE, Spiegel BM, Sack J, Hines OJ, Dulai GS, Gralnek IM, Farrell JJ. Colonic stent vs. emergency surgery for management of acute left-sided malignant colonic obstruction: a decision analysis. Gastrointest Endosc. 2004;60:865-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Saida Y, Sumiyama Y, Nagao J, Uramatsu M. Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum. 2003;46:S44-S49. [PubMed] |
| 15. | van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, Bemelman WA. Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy. 2008;40:184-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011;25:1814-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 227] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 17. | Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J. Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2013;22:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (2)] |
| 18. | Søreide K. Emergency management of acute obstructed left-sided colon cancer: loops, stents or tubes? Endoscopy. 2013;45:247-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Choi JH, Lee YJ, Kim ES, Choi JH, Cho KB, Park KS, Jang BK, Chung WJ, Hwang JS. Covered self-expandable metal stents are more associated with complications in the management of malignant colorectal obstruction. Surg Endosc. 2013;27:3220-3227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
P- Reviewers: Dormann AJ, Ge ZZ, Lu F S- Editor: Wen LL L- Editor: A E- Editor: Wang CH