Published online Mar 28, 2014. doi: 10.3748/wjg.v20.i12.3364
Revised: October 31, 2013
Accepted: January 2, 2014
Published online: March 28, 2014
Processing time: 224 Days and 17.9 Hours
AIM: To explore the characteristics of multi-slice computed tomography (CT) manifestations of hepatic epithelioid angiomyolipoma (HEA), improve the rate of accurate diagnosis, and reduce the misdiagnostic rate.
METHODS: The multi-slice CT manifestations in five patients who were diagnosed with HEA definitely by postoperative pathological examination were analysed retrospectively. Three female patients and two male patients were included. Before operation, four patients received plain CT scanning and dynamic enhancement scanning, and the other patient only received enhancement scanning, with immunohistochemical analysis conducted after postoperative pathological examination. Four patients were misdiagnosed by CT, including three patients misdiagnosed with hepatic cell carcinoma and one patient with focal nodular hyperplasia.
RESULTS: Upper abdominal multi-slice spiral CT scanning and three-stage enhancement scanning were conducted in five patients with HEA before operation. HEA had certain characteristic CT manifestations: low density masses, a few relatively high-density masses or fat-density masses diffusely shown in foci, clear boundary, round or oval and large focus, and tumour size ranging from 3.1 cm × 2.5 cm to 7.0 cm × 5.2 cm. During enhancement scanning, the foci were significantly enhanced uniformly or non-uniformly during the arterial phase, while during the venous and equilibrium phases, the foci were enhanced continuously or showed obvious low-density masses. Obviously enhanced and widened vessels could be found adjacent to foci or in the central area of foci during the arterial phase.
CONCLUSION: CT manifestations of HEA have certain characteristics. Primary diagnosis can be obtained by combining CT findings with clinical data, but pathological examination is still needed for a definite diagnosis.
Core tip: The multi-slice computed tomography manifestations in five patients with HEA were analyzed in the study. In computed tomography scanning, low density masses, a few relatively high density masses or fat density masses were showed in foci, the boundary was clear, the focus was round or oval and large, and the size of the tumour was 3.1 cm × 2.5 cm to 7.0 cm × 5.2 cm. The foci were significantly enhanced during arterial phase, enhanced continuously or showed obvious low density masses during venous phase and equilibrium phase, and obviously enhanced and widened vessels could be found adjacent to foci or in the central area of foci.
- Citation: Dai CL, Xue LP, Li YM. Multi-slice computed tomography manifestations of hepatic epithelioid angiomyolipoma. World J Gastroenterol 2014; 20(12): 3364-3368
- URL: https://www.wjgnet.com/1007-9327/full/v20/i12/3364.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i12.3364
Angiomyolipoma commonly occurs in the kidney and liver, but is also found in the retroperitoneum, heart, mediastinum, lung, and vagina[1-3]. A typical angiomyolipoma consists of vessels, smooth muscles, and fat. Ishak[4] reported hepatic epithelioid angiomyolipoma (HEA) for the first time. HEA is a kind of rare mesenchymal benign tumour and a special type of angiomyolipoma. HEA consists of epithelioid cells and is commonly found in females, with the male to female ratio of 1:5[5,6]. HEA does not have special clinical manifestations and may be easily confused with many kinds of tumours. Therefore, the rate of misdiagnosis is very high.
At present, HEA is considered a kind of epithelioid tumour adjacent to vessels and different from hamartoma[7,8]. The pathological diagnosis depends on immunohistochemical examination[9]. The biological behaviour of HEA is benign generally, but malignant HEA has been reported, and the prognosis of some patients are bad. Now many scholars have realised that the biological behaviour of HEA has malignant potential[10-14]. Some studies have shown that high expression of Ki-67 is one of the characteristics of HEA[15]. Therefore, early diagnosis of HEA is very important.
Multi-slice spiral computed tomography (MSCT) is an important method for preoperative diagnosis of HEA, but the CT manifestations are various because HEA does not contain or rarely contains mature adipose tissue[16-18]. Thus, diagnosis is difficult, with the accuracy rate of preoperative diagnosis being 32% or less, and diagnosis mainly depends on puncture and biopsy currently[19,20]. This study retrospectively analysed CT manifestations in five patients who were diagnosed with HEA definitely by pathological examination and immunohistochemical examination, in order to improve diagnosis of the disease and provide a reference for improving the rate of accurate preoperative diagnosis of HEA.
Five patients with HEA who were diagnosed definitely by pathological examination after operation at our hospital from May 2010 to June 2012 were included, including two men and three women. Their mean age was 56.5 years (range: 46-61 years). Three patients were found with a liver space-occupying lesion and without any clinical symptoms; two patients visited the hospital because of distending pain in the right upper quadrant without obvious causative factors. All five patients were found to be HBsAg- and alpha fetoprotein-negative and have normal hepatic function. Before operation, four patients received plain CT scanning and dynamic enhancement scanning, and the other patient only received enhancement scanning.
All patients were asked to comply with an absolute diet for 6-8 h before scanning. The patients were supine when scanning was performed, using 64-MSCT (Siemens, Germany). The scanning parameters were as follows: the spiral collimation was 64 × 0.625; the thickness of each slice was 5 mm; the interval thickness was 5 mm; the speed of couch movement was 12 mm/s; the tube voltage was 120 kV; and the tube current was 260-320 mAs. The extent of scanning was as follows: during the plain scanning phase, arterial phase, venous phase, and equilibrium phase, the extent of scanning was from the diaphragmatic dome to the level of the inferior pole of the kidney, including the whole liver; the scanning was finished for one time when the patient held their breath at the end of inspiration. Anconal venous transfusion of non-ionic contrast medium (OmniPaque 300 or Ultravist 300, 80-100 mL) with a high pressure injector was used during enhancement scanning. The rate of injection was 3.0 mL/s. The starting times of the arterial phase, venous phase, and equilibrium phase were 25, 35, and 60 s after the beginning of injection, respectively. After scanning, the original data were processed by thin slice reconstruction (one millimetre, the interval between two adjacent slices was one millimetre). The images of all patients received multiplanar reconstruction.
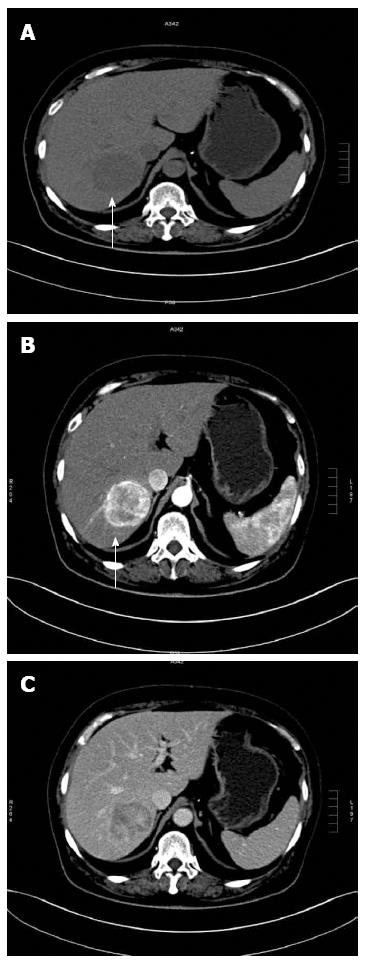
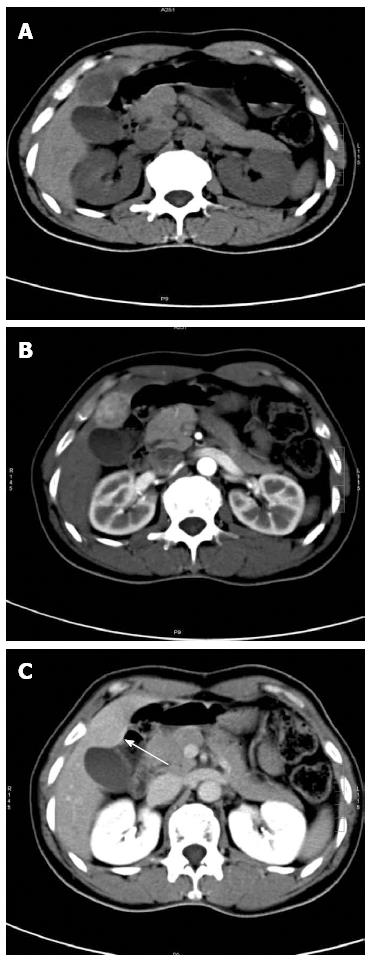
Upper abdominal multi-slice spiral CT scanning and three-stage enhancement scanning were conducted in the five patients before operation. The growth positions of HEA included the right lobe of the liver (three patients) and the left lobe of the liver (two patients). The size of tumour was 3.1 cm × 2.5 cm to 7.0 cm × 5.2 cm. The CT manifestations of HEA were: the tumours were round; slightly low-density masses were found in four patients (Figure 1A) and a low-density mass was found in one patient (Figure 2A); the boundary of tumours was clear; and no bleeding, necrosis, cystic degeneration, or calcification was found. A little fatty density was found in one case, but dilatation of adjacent intrahepatic bile duct was not found.
The manifestations during dynamic enhancement scanning were: the lesions of five patients were enhanced significantly during the arterial phase; and the enhancement degree was stronger than that of liver parenchyma, including four patients with non-uniform enhancement (Figure 1B) and one patient with uniform enhancement (Figure 2B). Contrast agent disappearance was found in three patients during the venous phase and equilibrium phase, including two patients with an obvious decrease of enhancement degree, which was significantly lower than that of normal liver parenchyma, and one patient with a decrease of enhancement degree that was slightly lower than that of normal liver parenchyma (Figure 1C). The lesions of two patients were enhanced continuously. The enhancement degree of lesions during the venous phase was stronger than that of normal liver parenchyma, and the enhancement degree of lesions during the equilibrium phase was similar to that of liver parenchyma (Figure 2C). Enlarged vessels were found near the tumour or in the central area of the tumour of two patients (Figure 1B).
Among the five patients with HEA, four were misdiagnosed, including three diagnosed with hepatic cell carcinoma (HCC) and one with focal nodular hyperplasia (FNH). Multi-slice CT manifestations in five patients with HEA are displayed in Table 1.
| Shape | Boundary | Density | Enhancement | Abnormal vessels adjacent to tumors and intratumoral abnormal vessels |
| Oval | Clear | Slightly low, uniform | Fast in and slow out enhancement | No |
| Oval | Clear | Slightly low, non-uniform, containing a few lipid | Fast in and fast out enhancement pattern, non-uniform enhancement | No |
| Oval | Clear | Slightly low, uniform | Fast in and fast out enhancement pattern, non-uniform enhancement | Yes |
| Oval | Clear | Slightly low, uniform | Fast in and slow out enhancement pattern, continuous and non-uniform enhancement | No |
| Oval | Clear | Slightly low, uniform | Fast in and slow out enhancement pattern, continuous and non-uniform enhancement | Yes |
HEA is a kind of very rare mesenchymal tumour and mainly consists of epithelioid cells[3]. HEA does not contain adipose tissue or contains little mature adipose tissue, so its diagnosis is difficult. In recent years, it has been reported that angiomyolipoma is a true neoplasm[20], but there are previous few reports on imaging of HEA, and the prognosis of some patients is bad[21,22]. Therefore, more attention should be paid to the disease. In this study, the diagnosis of HEA was improved by retrospectively analysing the imaging data of five patients with HEA.
CT manifestations of HEA vary and diagnosis is difficult. Most of the patients were diagnosed definitely by puncture and biopsy[23,24]. Peh and partners[25] reported three patients with HEA of different manifestations, including one case whose CT manifestations were similar to those of FNH, one case whose CT manifestations were similar to those of HCC, and one case with typical CT manifestations of HEA (coexistence of lipid, widened vessels, and smooth muscle tissue, which were similar to the reported manifestations). It is easy to diagnose typical HEA mixed with lipid, but most of the HEA foci had no lipid, which made diagnosis difficult[5].
Analysis of CT manifestations in five patients with HEA showed that the boundary of foci of the five patients was clear, the foci were large, round or oval. The densities in four patients were relatively uniform and without lipid; the density in one patient was not uniform, with a little adipose tissue in focus. During enhancement scanning, the foci of five patients were obviously enhanced during the arterial phase, including the foci of four patients that were enhanced non-uniformly and the focus of one patient that was enhanced uniformly. The vessels adjacent to foci or in the central area of foci widened. During the venous phase, four patients showed low-density masses, and one patient showed a high-density mass. This mass continued to be present in the equilibrium phase, showing equidensity mass.
It is concluded that it is not difficult to diagnose the lesions with adipose density in foci, while for the lesions without adipose density in foci, HEA should be considered when the following conditions appear: low density is shown in plain CT scanning, the boundary is clear, the foci are round or oval, and the size of foci is large (the long diameter of foci in the study was 3.1 cm or more); during enhancement scanning, the foci are obviously enhanced uniformly or non-uniformly during the arterial phase, then the foci show high density or obvious low density during the venous phase and equilibrium phase; and obviously enhanced and widened vessels are found in the area adjacent to foci or in the central area of foci during the arterial phase.
Among the five patients with HEA in the study, three showed low-density masses or slightly low-density masses during plain scanning, and they were misdiagnosed as HCC because of the characteristic of ‘fast in and fast out enhancement pattern’; and one patient showed a slightly low-density mass during plain scanning, and the patient was misdiagnosed with FNH because of the characteristic of ‘fast in and slow out enhancement pattern’. Thus, HEA needs to be differentiated from the following diseases.
Patients with HCC often show an irregular low-density mass, and most of them have medical histories of hepatitis B or liver cirrhosis. The level of alpha foetoprotein is high, and portal vein cancer embolus formation is often found. Large foci are enhanced obviously and non-uniformly during enhancement scanning. In contrast, HEA is a round or oval mass with slightly low or low density. The foci are large with a ‘fast in and fast out enhancement pattern’, and the enhancement of foci is not uniform generally. The patients do not have a medical history of hepatitis B and the results of laboratory examination are negative[23-25].
The foci are equidensity and equisignal masses compared with liver parenchyma on CT. The characteristic is a star scar in the central area of foci, which show a ‘fast in and slow out enhancement pattern’ and continuous enhancement, but the star scar cannot be enhanced. Conversely, the foci of HEA are slightly low-density or low-density masses, without a scar in the central area of foci[23-25].
In short, the imaging manifestations of HEA have certain characteristics. Primary diagnosis can be obtained by combining CT findings and clinical data (e.g., without a medical history of hepatitis B and negative results of laboratory examination), but a definite diagnosis depends on puncture and biopsy or histopathological examination.
Hepatic epithelioid angiomyolipoma (HEA) is a kind of very rare mesenchymal tumour and mainly consists of epithelioid cells. HEA does not contain adipose tissue or contains little mature adipose tissue, so its diagnosis is difficult. In recent years, it has been reported that angiomyolipoma is a true neoplasm, but there are previous few reports on imaging of HEA, and the prognosis of some patients is bad. Therefore, more attention should be paid to the disease. In this study, the diagnosis of HEA was improved by retrospectively analysing the imaging data of five patients with HEA.
In recent years, it has been reported that angiomyolipoma is a true neoplasm, but there are previous few reports on imaging of HEA, and the prognosis of some patients is bad. Therefore, more attention should be paid to the disease.
In this study, the diagnosis of HEA was improved by retrospectively analysing the imaging data of five patients with HEA.
Computed tomography (CT) manifestations in patients with HEA have certain characteristics. Primary diagnosis can be obtained by combining CT findings with clinical data, but pathological examination is still needed for a definite diagnosis.
In this manuscript, the authors explores and analyzes CT manifestations of five patients with HEA who were diagnosed definitely by pathological examination and immunohistochemistry, and provide reference for improving accurate rate of diagnosis. The manuscript is very well written.
| 1. | Eble JN. Angiomyolipoma of kidney. Semin Diagn Pathol. 1998;15:21-40. [PubMed] |
| 2. | Murakata LA, Ishak KG, Nzeako UC. Clear cell carcinoma of the liver: a comparative immunohistochemical study with renal clear cell carcinoma. Mod Pathol. 2000;13:874-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Graziano A, Santangelo M, Umana DS. Clinical evaluation of epithelioid angiomyolipoma. Ann Ital Chir. 2008;79:135-138. [PubMed] |
| 4. | Ishak KG. Primary hepatic tumors in childhood. Prog Liver Dis. 1976;5:636-667. [PubMed] |
| 5. | Schlingemann RO, Rietveld FJ, Kwaspen F, van de Kerkhof PC, de Waal RM, Ruiter DJ. Differential expression of markers for endothelial cells, pericytes, and basal lamina in the microvasculature of tumors and granulation tissue. Am J Pathol. 1991;138:1335-1347. [PubMed] |
| 6. | Mai KT, Belanger EC. Perivascular epithelioid cell tumour (PEComa) of the soft tissue. Pathology. 2006;38:415-420. [PubMed] |
| 7. | Saito M, Tsukamoto T, Takahashi T, Sai K, Fujii H, Nagashima K. Multifocal angiomyolipoma affecting the liver and lung without tuberous sclerosis. J Clin Pathol. 2004;57:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Li T, Wang L, Yu HH, Sun HC, Qin LX, Ye QH, Fan J, Tang ZY. Hepatic angiomyolipoma: a retrospective study of 25 cases. Surg Today. 2008;38:529-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Ren N, Qin LX, Tang ZY, Wu ZQ, Fan J. Diagnosis and treatment of hepatic angiomyolipoma in 26 cases. World J Gastroenterol. 2003;9:1856-1858. [PubMed] |
| 10. | Dalle I, Sciot R, de Vos R, Aerts R, van Damme B, Desmet V, Roskams T. Malignant angiomyolipoma of the liver: a hitherto unreported variant. Histopathology. 2000;36:443-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 136] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Warakaulle DR, Phillips RR, Turner GD, Davies D, Protheroe AS. Malignant monotypic epithelioid angiomyolipoma of the kidney. Clin Radiol. 2004;59:849-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Martignoni G, Pea M, Bonetti F, Zamboni G, Carbonara C, Longa L, Zancanaro C, Maran M, Brisigotti M, Mariuzzi GM. Carcinomalike monotypic epithelioid angiomyolipoma in patients without evidence of tuberous sclerosis: a clinicopathologic and genetic study. Am J Surg Pathol. 1998;22:663-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 127] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Martignoni G, Pea M, Reghellin D, Zamboni G, Bonetti F. PEComas: the past, the present and the future. Virchows Arch. 2008;452:119-132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 337] [Cited by in RCA: 384] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 14. | Hornick JL, Fletcher CD. PEComa: what do we know so far? Histopathology. 2006;48:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 325] [Article Influence: 16.3] [Reference Citation Analysis (1)] |
| 15. | Dimmler A, Seitz G, Hohenberger W, Kirchner T, Faller G. Late pulmonary metastasis in uterine PEComa. J Clin Pathol. 2003;56:627-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 72] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Xu PJ, Shan Y, Yan FH, Ji Y, Ding Y, Zhou ML. Epithelioid angiomyolipoma of the liver: cross-sectional imaging findings of 10 immunohistochemically-verified cases. World J Gastroenterol. 2009;15:4576-4581. [PubMed] |
| 17. | Xiao W, Zhou M, Lou H, Wang Z, Zhang M. Hemodynamic characterization of hepatic angiomyolipoma with least amount of fat evaluated by contrast-enhanced magnetic resonance angiography. Abdom Imaging. 2010;35:203-207. [PubMed] |
| 18. | Iannaccone R, Piacentini F, Murakami T, Paradis V, Belghiti J, Hori M, Kim T, Durand F, Wakasa K, Monden M. Hepatocellular carcinoma in patients with nonalcoholic fatty liver disease: helical CT and MR imaging findings with clinical-pathologic comparison. Radiology. 2007;243:422-430. [PubMed] |
| 19. | Yang CY, Ho MC, Jeng YM, Hu RH, Wu YM, Lee PH. Management of hepatic angiomyolipoma. J Gastrointest Surg. 2007;11:452-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Messiaen T, Lefebvre C, Van Beers B, Sempoux C, Cosyns JP, Geubel A. Hepatic angiomyo(myelo)lipoma: difficulties in radiological diagnosis and interest of fine needle aspiration biopsy. Liver. 1996;16:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Nussbaumer AL, Samain F, Malinovskii VL, Häner R. Supramolecular polymerization of oligopyrenotides--control by single, natural nucleotides. Org Biomol Chem. 2012;10:4891-4898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Yamasaki S, Tanaka S, Fujii H, Matsumoto T, Okuda C, Watanabe G, Suda K. Monotypic epithelioid angiomyolipoma of the liver. Histopathology. 2000;36:451-456. [PubMed] |
| 23. | Alatassi H, Sahoo S. Epithelioid angiomyolipoma of the liver with striking giant cell component: fine-needle aspiration biopsy findings of a rare neoplasm. Diagn Cytopathol. 2009;37:192-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Fernandes ES, Bernardo RL, Fernandes MM, Araújo RM, Sebbe R, Monte A, Coelho JF, Souza AA, Ribeiro Filho J. Extrahepatic right hepatic duct diverticulum: a rare entity. Hepatobiliary Pancreat Dis Int. 2010;9:213-215. [PubMed] |
| 25. | Peh WC, Ngan H, Fan ST, Ng IO. Case report: variable imaging appearances of angiomyolipomas of the liver. Br J Radiol. 1995;68:540-544. [PubMed] |
P- Reviewers: Seth D, Simpson ND S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang DN