Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1498
Revised: February 1, 2013
Accepted: February 8, 2013
Published online: March 7, 2013
Processing time: 97 Days and 18.6 Hours
Multiple primary carcinoma (MPC) is defined as two or more carcinomas without subordinate relationship detected in the same or other organs of an individual patient. The diagnosis of MPC must comply with the following standards: each of the tumors must present a definite picture of malignancy, each tumor must be histologically distinct, and the probability of one being a metastasis of the other must be excluded. MPC often occurs in the digestive system, but its pathogenesis remains unclear involving genetic susceptibility, tumor immunity and iatrogenic factors, including radiotherapy and chemotherapy. Most MPC patients are double primary malignancy; the occurrence of quadruple primary malignancy is below 0.1%. Here we present a rare case of quadruple primary malignancy involving the small intestine, descending colon, renal pelvis and pancreas. Due to its rarity, the relevant literature is also reviewed. In general, the incidence of MPC is rising, so prevention, early diagnosis and treatment will become necessary and important. Therefore, further research should focus on the etiology and mechanism of MPC.
- Citation: Jiao F, Hu H, Wang LW. Quadruple primary malignancy patient with survival time more than 20 years. World J Gastroenterol 2013; 19(9): 1498-1501
- URL: https://www.wjgnet.com/1007-9327/full/v19/i9/1498.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i9.1498
Multiple primary carcinoma (MPC) is an infrequently occurring disease that is defined as two or more carcinomas without subordinate relationship detected in the same or other organs of an individual patient. It is also called multiple primary malignant neoplasms or multiplicity cancer. The current criteria for the diagnosis of MPC were first presented by Warren et al[1] in 1932: Each of the tumors must present a definite picture of malignancy, each tumor must be histologically distinct and the probability of one being a metastasis of the other must be excluded. MPC could be classified into two categories depending on the diagnosis time of each malignancy. Synchronous MPC refers to the malignancies occurring at the same time or within an interval of six months, while metachronous MPC refers to malignancies following in sequence and more than six months apart[2]. MPC often occurs in the digestive system. Of all the MPC patients, most are double primary malignancy; the occurrence of quadruple primary malignancy has been reported to be below 0.1%[3]. Here we present a rare case of quadruple primary malignancy involving the small intestine, descending colon, renal pelvis and pancreas. Considering its rarity, we also reviewed relevant literature.
Our patient, a 64-year-old man from Shanghai, China, is still alive and healthy now. He has undergone five surgeries, four for primary malignancies, and one for chronic cholecystitis and cholelithiasis. His mother died of hepatic carcinoma at the age of 81 years, and other members (his wife, daughter and younger brother) in the family have no history of malignancy. He has been suffering from hypertension for 30 years and diabetes for 20 years, and being treated with telmisartan and insulin for each disease, respectively. In addition, he is allergic to penicillin and sulfa drugs. He smokes one pack of cigarettes per day and drinks beer temperately. Other history of trauma and surgery are denied. The following are the detailed records of his medical history.
The first primary malignancy was small intestine adenocarcinoma, which was detected in 1992. According to the description of the patient, the initial symptom was mild pain in the upper abdomen. Considering his good physical condition, he did not pay much attention to it. The pains worsened over time, and he eventually visited Shanghai Wujing Hospital. Strangely, all of the related examination results were negative, so an exploratory laparotomy was performed immediately. Exposure of the surgical site showed that the small intestine was infected and its contents poured into the peritoneal cavity. A small intestine resection surgery was necessary. The postoperative pathology result revealed small intestine adenocarcinoma. Unfortunately, we no longer have access to the surgery records or the record of the adenocarcinoma because too much time has passed. Owing to anemia caused by long-term absorption disorder after the operation, the patient underwent a blood transfusion that led to hepatitis C infection. Aside from the anemia and transfusion complications, the postoperative recovery of the patient was near perfect and he was scheduled for regular follow-up appointments.
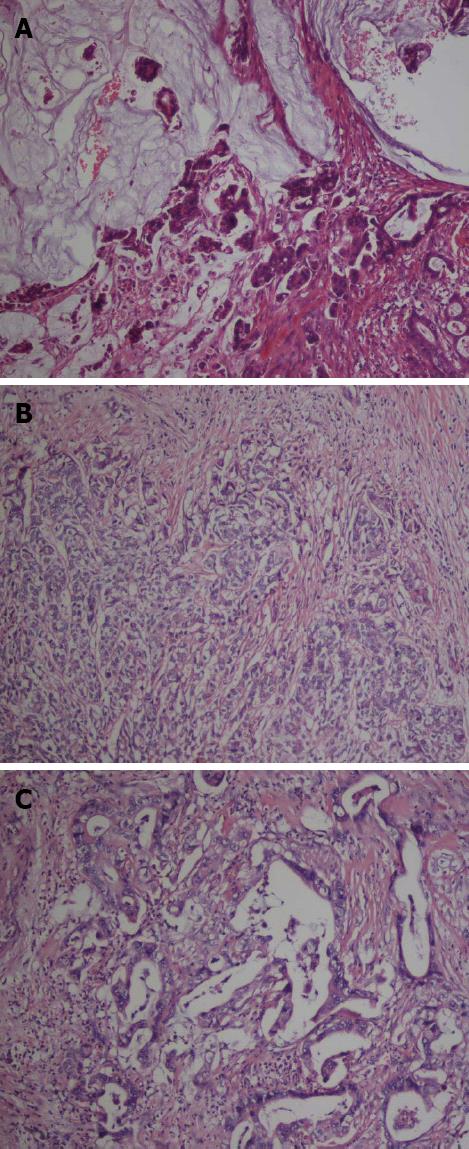
In March 2000, the patient was sent to the Shanghai Liqun Hospital because of a six-month abdominal dull pain and a two-week mucus bloody stool. Colonoscopy performed in the outpatient department showed a tumor in the descending colon. He then underwent a surgical resection after hospitalization. The postoperative histological examination report showed an ulcerated mucinous adenocarcinoma (Figure 1A). All the surgical margins and peripheral lymph nodes were negative. The patient’s postoperative recovery was excellent. He was treated with ten cycles of adjuvant chemotherapy after the operation, but the detailed regimen is not available now. All these medical treatment procedure were uneventful and he was scheduled for regular follow-up appointments.
In 2010, the patient was admitted to the department of urology of Ruijing Hospital due to observing gross hematuria symptoms for 20 d. No sign of urinary frequency, urgency, or dysuria were observed, and all physical examinations were normal except the left lumbar. B ultrasonic examination revealed the left renal pelvis was occupied by a solid mass and the ureter was expanded with hydronephrosis. In addition, an ensured abdominal computed tomography (CT) scan revealed left renal carcinoma with hydronephrosis and multiple cysts in both kidneys. Taken together, he was diagnosed as renal pelvic malignancies. Then a radical resection of the left kidney was performed. The postoperative histological examination results revealed high-level invasive urothelial carcinoma of the pelvis (Figure 1B) and vascular tumor thrombus. All surgical margins, perirenal adipose tissue and the left ureter were negative. After the operation, he underwent urinary bladder irrigation, but the detailed regimen is not available now. The patient was again scheduled for regular follow-up appointments.
At the end of 2011, he again complained of upper abdominal pain. A laboratory investigation showed that his CA 19-9 level was 1175.7 IU/mL, much higher than normal. Subsequently, an abdominal CT scan revealed a 2.86 cm × 3.81 cm mass in the tail of pancreas. As a result of comprehensive examinations above, he was diagnosed with pancreatic cancer. Subsequently, he was immediately transferred to Ruijin Hospital, where he underwent distal pancreatectomy, splenectomy and enterolysis. During the operation, a 4 cm cystic mass that infringed the retroperitoneal space was found. The postoperative histological examination reported grade II-III adenocarcinoma in the body and tail of the pancreas (Figure 1C), and positive peripancreatic lymph nodes (1/1). No tumor cells were found in the resection margins and the spleen. The postoperative recovery was uneventful and the patient was given postoperative adjuvant chemotherapy by using Xeloda. The patient is currently attending regular follow-up appointments and periodically goes to the department of general surgery for his chemotherapy.
MPC was proposed in 1889 by Billroth et al[4] in the form of case report. Though there have been an increasing amount of reports on this subject since then, cases of MPC were still considered to be medical curiosities until 1932 when Warren et al[1] gave an extremely detailed compilation study of 1259 cases. More importantly, they established the diagnostic criteria for MPC in their report, which is still used today. Despite its low incidence, the association of two malignancies in a single patient has been widely reported in the literature[5-7], while only a few cases of quadruple malignancies have been described[8]. Our patient presents a case of quadruple primary malignancy involving the small intestine, descending colon, pelvis and pancreas. All the malignancies were confirmed by surgery and postoperative pathology results, fulfilling the diagnostic criteria of MPC. Cases of quadruple primary malignancies are very rare, but what is even more astounding is the fact that this patient is still alive today, 20 years after his initial diagnosis. Further, his state of mind and physical condition are excellent, so much so that he cares for himself. Therefore we do think that this is a useful case worthy of our report.
MPC is still quite rare, but the occurrence is on the rise and differs by region and time. Age, diagnostictechnique improvements, and longer life spans are all contributing factors. As is widely known and broadly accepted, age is a risk factor for many diseases, and MPC is a no exception. Spratt et al[9] concluded that persons living to an extreme age were expected to have MPC with greater frequency. Another study showed that tumor survivors had a 14% higher risk of developing a new malignancy than would have been expected in the general population[10]. Based on these findings, we speculate that countries with aging populations will begin to see more and more patients with MPC. Individual genetic susceptibility and other factors, such as hormonal stimulation, iatrogenic factors, environmental degradation and immunologic defects may be involved in the carcinogenesis and progression of MPC. However, nearly all the studies on MPC are descriptive, and detailed studies exploring the molecular mechanisms of MPC are urgently needed. Many hypotheses have been proposed to explain the pathogenesis of MPC. Iioka et al[11] observed that patients with MPC had a high frequency of microsatellite instability (MSI), arguing that MSI affected the pathogenesis of some MPC cases. Field cancerization is another possible mechanism, which suggests that when an organ is exposed to carcinogens, other nearby organs are also exposed to the carcinogens and carry a high risk of cancer[12]. Lauchlan et al[13] suggested that cancers developing in other sites originate from histologically similar epithelium. Travis et al[14] discovered that radiotherapy, a kind of iatrogenic factor, following the treatment of a primary cancer lead to a second malignancy. The detailed etiology and mechanism for MPC formation still need further clarification.
Our research group has two hypotheses relating to the prevalence of MPC. The first is genetic susceptibility. All the members of a family share the similar living environment, why one does not get cancer, another may develop single primary cancer (SPC), while others may have multiple primary cancer? Maybe genetic susceptibility is a very important factor. The second is tumor immunity. The survival time of metachronous MPC patients is longer than synchronous MPC patients and metastatic SPC patients on average. A most interesting phenomenon is that the longer the interval between the malignancies, the better the prognosis of the patients (our unpublished data). Immunity abnormality is thought to exist in these patients. We speculate that theimmunity of an organism is first impaired, but then is triggered and becomes strengthened bycytokines and growth factors secreted by tumor and other cells, and finally exhausted. This triggered and strengthened immunity is likely to contribute to the longer survival time of the metachronous MPC patients. Although our group has been doing relevant work and has yielded important information, both of these hypotheses still need further study and verification. In conclusion, MPC occurs rarely but is increasing in prevalence. Prevention, early diagnosis, and treatment are important factors in treating MPC. The etiology and its mechanism remain controversial, and thus further research should focus on this distinctive group - MPC patients.
| 1. | Warren S, Gates O. Multiple primary malignant tumors: survey of the literature and a statistical study. Am J Cancer. 1932;16:1358-1414. |
| 2. | Moertel CG. Multiple primary malignant neoplasms: historical perspectives. Cancer. 1977;40:1786-1792. [PubMed] |
| 3. | Németh Z, Czigner J, Iván L, Ujpál M, Barabás J, Szabó G. Quadruple cancer, including triple cancers in the head and neck region. Neoplasma. 2002;49:412-414. [PubMed] |
| 4. | Billroth T, von Winiwarter A. General surgical pathology and therapeutics in 51 Vorlesungen: A textbook for students and physicians in fifty-one lectures. 14th ed. Berlin: G Rerimer 1889; . |
| 5. | Cui Y, Liu T, Zhou Y, Ji Y, Hou Y, Jin W, Feng Y. Five cases report of solid tumor synchronously with hematologic malignancy. Cancer Res Treat. 2012;44:63-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Klochikhin AL, Markov GI, Kashmanov AE, Movergoz SV, Chernov NV. A case of successful treatment of multiple primary cancer of the oropharynx and the lung. Vestn Otorinolaringol. 2004;49-50. [PubMed] |
| 7. | Naka H, Ishikawa N, Maeda S, Muraoka H, Negishi T, Kamiyama R. Multiple primary cancers of the head and neck. Gan No Rinsho. 1990;36:2404-2408. [PubMed] |
| 8. | Noh SK, Yoon JY, Ryoo UN, Choi CH, Sung CO, Kim TJ, Bae DS, Kim BG. A case report of quadruple cancer in a single patient including the breast, rectum, ovary, and endometrium. J Gynecol Oncol. 2008;19:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Spratt JS, Hoag MG. Incidence of multiple primary cancers per man-year of follow up: 20-year review from the Ellis Fischel State Cancer Hospital. Ann Surg. 1966;164:775-784. [PubMed] |
| 10. | Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, Tucker MA, Fraumeni Jr JF. New malignancies among cancer survivors: SEER Cancer Registries, 1973-2000. Bethesda: National Cancer Institute 2006; No.05-5302. |
| 11. | Iioka Y, Tsuchida A, Okubo K, Ogiso M, Ichimiya H, Saito K, Osaka Y, Sato S, Aoki T, Koyanagi Y. Metachronous triple cancers of the sigmoid colon, stomach, and esophagus: report of a case. Surg Today. 2000;30:368-371. [PubMed] |
| 12. | Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer. 1953;6:963-968. [PubMed] |
| 13. | Lauchlan SC. Conceptual unity of the Müllerian tumor group. A histologic study. Cancer. 1968;22:601-610. [PubMed] |
| 14. | Travis LB, Fosså SD, Schonfeld SJ, McMaster ML, Lynch CF, Storm H, Hall P, Holowaty E, Andersen A, Pukkala E. Second cancers among 40,576 testicular cancer patients: focus on long-term survivors. J Natl Cancer Inst. 2005;97:1354-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 626] [Cited by in RCA: 597] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
P- Reviewer Chapel A S- Editor Wen LL L- Editor A E- Editor Li JY