Published online Mar 7, 2013. doi: 10.3748/wjg.v19.i9.1489
Revised: November 30, 2012
Accepted: December 15, 2012
Published online: March 7, 2013
Processing time: 168 Days and 5.9 Hours
A 36-year-old male was admitted with right lower abdominal pain and diarrhea for more than 3 mo. Colonoscopy and a barium enema study revealed a submucosal tumor over the cecum, but computed tomography showed an ileal lipoma. There was no definitive diagnosis preoperatively, but ileocolic intussusception was noted during surgery. Single port laparoscopic radical right hemicolectomy was performed because intra-operative reduction failed. The histological diagnosis of the resected tumor was lipoma. Single port laparoscopic surgery has recently been proven to be safe and feasible. There are advantages compared with conventional laparoscopic surgery, such as smaller incision wounds, fewer port site complications, and easier conversion. However, there are some drawbacks which need to be overcome, such as difficulties in triangulation and instrument clashing. If there are no contraindications to laparoscopy, single port laparoscopic surgery can be performed safely and should be considered for diagnosis and treatment of intussusception in adults. Here, we report the first case of ileocolic intussusception successfully treated by single port laparoscopic surgery.
- Citation: Chen JH, Wu JS. Single port laparoscopic right hemicolectomy for ileocolic intussusception. World J Gastroenterol 2013; 19(9): 1489-1493
- URL: https://www.wjgnet.com/1007-9327/full/v19/i9/1489.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i9.1489
Intussusception is primarily a childhood disease. It is uncommon in adults and about 70%-90% of adult intussusception cases have a leading cause[1,2]. Lipoma, which frequently arises in the terminal ileum, is the second most common benign tumor of the small intestine, and it tends to cause intussusception[3]. As adult patients are at high risk of malignancy, surgical intervention is recommended in cases of intussusception. In recent years, laparoscopic surgery has been able to confirm the diagnosis and to resect the tumor causing intussusception of the small intestine in adults[4]. Furthermore, single port laparoscopic surgery has been used for various abdominal procedures with safety and feasibility[5]. We report the first case of ileocolic intussusception successfully treated by single port laparoscopic radical right hemicolectomy.
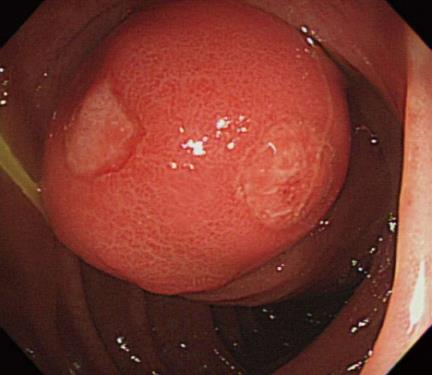
A 36-year-old male was admitted because of right lower abdominal pain and diarrhea for more than 3 mo. Colonoscopy disclosed a submucosal tumor over the cecum. The mass was a ball-like form with an eroded surface (Figure 1). The tumor was initially diagnosed as an ulcer and confirmed by biopsy.
On physical examination, no palpable mass was noted in the abdomen. There was no swelling of superficial lymph nodes. He had no specific past history or family history. Laboratory studies on admission yielded normal blood hematology and chemistry results. The levels of carcinoembryonic antigen and carbohydrate antigen 19-9 were within normal limits. An X-ray of the abdomen was normal. An abdominal computed tomography scan showed a round and low density mass about 2.5 cm in the right pelvic region (Figure 2). A barium enema study showed a bulging lesion over the cecum (Figure 3).
The diagnosis was a cecal submucosal tumor or ileal lipoma. His symptoms were not remarkable. Thus, elective single port laparoscopic right hemicolectomy or single port laparoscopic enterotomy with lipoma resection was scheduled. Through inspection of the abdomen via the single port, the terminal ileum was found to be invaginated through the ileocecal valve, and ileocolic intussusception was observed (Figure 4). Initially, we tried manipulation and reduction of the intussusception, but failed. Then we performed single port radical right hemicolectomy because of the high risk of a malignant cause.
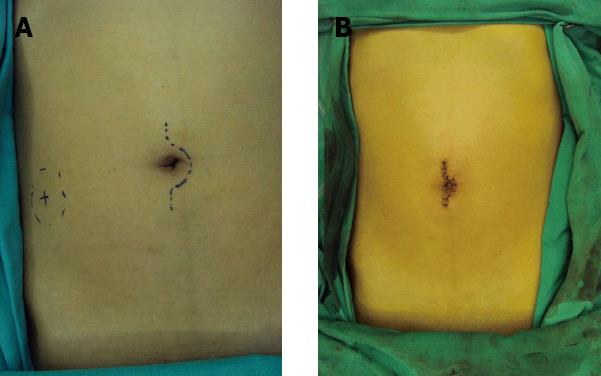
For the single-port laparoscopic approach (Figure 5), a vertical incision was created through the umbilicus approximately 3 cm in length to accommodate the single-port access device. The SILS Port from Covidien Inc. (Mansfield, MA, United States) was used as the single-port access device. This included an insufflation attachment and 3 access ports with associated minitrochars. A rigid 10-mm, 30° laparoscope was used for viewing and 5-mm instruments were used for manipulation of tissues and dissection. In general, a lateral to medial approach was used. The hepatic flexure and lateral peritoneal reflection was mobilized from superior to inferior. The ileocolic pedicle was elevated to allow dissection beneath the ileocolic vessels with identification of the origin of the right colic artery and then the duodenum. The right colon and proximal transverse colon were then lifted off the retroperitoneum. The ileocolic vascular pedicle underwent ligation with the use of a high energy device. The portion of the omentum attached to the specimen was then divided proximally. The right branch of the middle colon was divided. After placement of a wound protector, the tumor was exteriorized via the umbilical incision. After resection of the tumor, ileocolic end-to-end anastomosis was performed. The bowel was returned to the abdomen, and then reexamined in situ. The fascial incision was closed with a Vicryl suture. Care was taken to maintain oncologic principles, with tight vascular ligation and minimal tumor manipulation. The total surgical time was 3 h and blood loss was about 30 mL.
The diagnosis was ileocolic intussusception caused by lipoma in the ileal region. Macroscopically, the tumor measured 2.5 cm × 2.5 cm × 2.0 cm, and was located 15 cm from the ileocecal valve (Figure 6). The tumor was ball-like with an irregular surface and soft consistency. The cut surface was yellowish-white, and histopathologic examination revealed fat cells proliferating in the submucosal layer. These characteristics confirmed a diagnosis of lipoma of the ileum.
Postoperative recovery was good and the patient was discharged on the 7th postoperative day. At present, 3 mo after surgery, he is free of symptoms and continues an uneventful course.
Single port laparoscopic surgery has been performed for the resection of benign and malignant gastrointestinal tumors in recent years; however, its safety and feasibility is still controversial. Waters et al[6] reported that single port laparoscopic right hemicolectomy is a safe and effective technique for cases of colonic malignant and benign lesions. There are also several reports of benign ileocolic intussusception successfully treated by laparoscopy[7]. Here, we successfully resected an ileal lipoma causing intussusception using single port laparoscopic radical right hemicolectomy, and to date, no report has described an ileocolic intussusception caused by ileal lipoma which was resected via single port laparoscopy.
In 1956, Dean et al[8] classified adult intussusception as enteric; colocolic; ileocecal, with the ileocecal valve as lead point; and ileocolic, with the ileum through the ileocecal valve. The most common type is enteric, occurring in 43% of patients[9] and our patient had the ileocolic type with ileal lipoma as the leading cause.
Adult intussusception is an uncommon clinical entity encountered by surgeons. The exact mechanism is unknown. However, it is believed that any lesion in the bowel wall or irritant within the lumen that alters normal peristaltic activity is able to initiate an invagination[2,10]. Ingested food and subsequent peristaltic activity of the bowel produce an area of constriction above the stimulus and relaxation below, thus telescoping the lead point (intussusceptum) through the distal bowel lumen (intussuscipiens)[1,2,10]. The most common locations are at the junctions between freely moving segments and retroperitoneally or adhesionally fixed segments[11].
The signs and symptoms of pediatric intussusception include a classic triad of a palpable mass, current jelly stools, and pain, and occur infrequently in adults. Adult intussusception commonly presents with nonspecific signs and symptoms similar to a bowel obstruction, such as colicky pain or cramps, nausea and vomiting, palpable abdominal mass, fever, hematochezia, and diarrhea[9]. The most common symptom is abdominal pain and the less common one is diarrhea. Our patient presented with chronic symptoms of abdominal pain and diarrhea. Because the symptoms often are nonspecific, correct preoperative diagnosis of intussusception is difficult. Eisen et al[12] reported a preoperative diagnosis rate of 40.7%. Similarly, our patient was not diagnosed with intussusception preoperatively. However, laparoscopy is able to evaluate the entire small and large bowel and is another diagnostic tool, too. Although we could not reduce the intussusception via single port laparoscopic surgery in our patient, we think that this new technique may provide a better way than conventional laparoscopic surgery to manipulate and reduce intussusceptions.
Symptoms could be acute or chronic. The duration was reported as less than 7 d in 34% of patients and between 7 d and 3 mo in 48%[13-15]. Gupta et al[13] and Stubenbord et al[14] reported that 22% experienced symptoms of more than 3 mo’ duration, while some patients have reported symptoms lasting up to 1 year[1]. Our patient presented with chronic symptoms for more than 3 mo. We found that the intussusception in our patient was dynamic, changing preoperatively from the colonoscopy and imaging studies. Spontaneous reduction of the intussusception may present in symptomatic or asymptomatic children and occurs more commonly than previously reported. These intussusceptions are usually short-segment, small-bowel intussusceptions with no recognizable leading cause[16]. Only a few case reports presented a spontaneous reduction of the intussusception in adults[17,18]. We postulated that spontaneous reduction of the intussusception in our patient led to obstruction and chronic symptoms, and made preoperative diagnosis more difficult.
A precipitating lesion is found in 90% of adult intussusception cases, but in only 10% of pediatric patients. In most infants and young children, reduction of the intussusception may be tried using barium enema or surgery. However, in adults, definitive surgical resection remains the recommended treatment in nearly all cases because of its nonspecific nature, varying duration of symptoms, the large proportion of structural anomalies, and the relatively high incidence of malignancy[2,19,20]. Although most authors agree that laparotomy is mandatory, the optimal surgical management of intussusception remains controversial. A reduction at surgery before resection may theoretically permit a more limited resection; however, the risks include intraluminal tumor seeding, a reduction in the externally viable bowel despite mucosal necrosis, venous embolization of malignant cells, spillage of fecal matter through inadvertent perforation, and anastomotic complications in cases of an edematous and weakened bowel[19]. The main problem is to distinguish benign from malignant lesions before reduction. The cause of intussusception in adults varied by location. Large bowel causative lesions were more frequently malignant than small bowel lesions. The incidence of either primary or metastatic malignancy in the small bowel was 31% compared with 70% in colon lesions[9]. Benign lesions, including lipomas that cause intussusception were predominantly found in the cecum and terminal ileum[1,21]. The most common benign lesions of the colon causing intussusception were lipomas[21].
In our patient, a cecal submucosal tumor or ileal lipoma was suspected preoperatively, but ileocolic intussusception was diagnosed during surgery. Because a benign lesion was highly suspected as the cause, we intended to reduce the intussusception initially, but in vain. Then we decided to perform radical right hemicolectomy.
Laparoscopic surgery has been a standard strategy for a variety of gastrointestinal diseases. The use of laparoscopic surgery for benign bowel tumors and ileocolic intussusception is increasing[4,7,9]. Single port laparoscopic surgery is a development in the field of minimally invasive surgery. Potential advantages of single port laparoscopic surgery over conventional laparoscopic surgery are though to be related to improvement in cosmesis and incisional pain and avoidance of port site-related complications. Other aspects, namely operative time, patient selection, patient outcomes, and surgeon efficiency, showed no difference between the two procedures in the existing literature. The conversion rate between the two procedures showed no significant difference, but it is easier for single port laparoscopic surgery to convert to open surgery. Furthermore, we think that a single port can provide access for intussusception diagnosis, manipulation, and reduction.
Although single port laparoscopic surgery can be performed with a conventional rigid laparoscope and straight instruments, the crowding over the access port usually leads to clashing of instruments. In addition, the handling of both straight instruments in parallel with the laparoscope through a small single incision decreases the freedom of motion for the surgeon and hinders handling of a laparoscope for the assistant. Furthermore, lack of tissue triangulation significantly increases difficulties in exposure and dissection of the lesion. Some of the steps must be performed using the cross-hand maneuver, which is generally avoided in conventional laparoscopy surgery. In attempts to improve surgical exposure, most surgeons use 30° laparoscopes and some used articulating or curved instruments. Some investigators recommended using longer laparoscopes to avoid cluttering of instruments.
In conclusion, we think that single port laparoscopic surgery can be performed safely for ileocolic intussusception caused by ileal lipoma in adults, and should be considered if contraindications are not present.
| 1. | Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 681] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 2. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 386] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 3. | Chiang JM, Lin YS. Tumor spectrum of adult intussusception. J Surg Oncol. 2008;98:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Alonso V, Targarona EM, Bendahan GE, Kobus C, Moya I, Cherichetti C, Balagué C, Vela S, Garriga J, Trias M. Laparoscopic treatment for intussusception of the small intestine in the adult. Surg Laparosc Endosc Percutan Tech. 2003;13:394-396. [PubMed] |
| 5. | Gaujoux S, Maggiori L, Bretagnol F, Ferron M, Panis Y. Safety, feasibility, and short-term outcomes of single port access colorectal surgery: a single institutional case-matched study. J Gastrointest Surg. 2012;16:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Waters JA, Rapp BM, Guzman MJ, Jester AL, Selzer DJ, Robb BW, Johansen BJ, Tsai BM, Maun DC, George VV. Single-port laparoscopic right hemicolectomy: the first 100 resections. Dis Colon Rectum. 2012;55:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Park KT, Kim SH, Song TJ, Moon HY. Laparoscopic-assisted resection of ileal lipoma causing ileo-ileo-colic intussusception. J Korean Med Sci. 2001;16:119-122. [PubMed] |
| 8. | Dean DL, Ellis FH, Sauer WG. Intussusception in adults. AMA Arch Surg. 1956;73:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | McKay R. Ileocecal intussusception in an adult: the laparoscopic approach. JSLS. 2006;10:250-253. [PubMed] |
| 10. | Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36:18-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 137] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Sachs M, Encke A. Entero-enteral invagination of the small intestine in adults. A rare cause of “uncertain abdomen”. Langenbecks Arch Chir. 1993;378:288-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 249] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 14. | Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172:306-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 105] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. ANZ J Surg. 2003;73:1044-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Kornecki A, Daneman A, Navarro O, Connolly B, Manson D, Alton DJ. Spontaneous reduction of intussusception: clinical spectrum, management and outcome. Pediatr Radiol. 2000;30:58-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 79] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Luckey P, Kemper J, Engelbrecht V, Mödder U. Idiopathic ileoileal intussusception in an adult with spontaneous reduction during enteroclysis: a case report. Abdom Imaging. 2000;25:48-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Lill M, Berkeley B, Cooper G. Multiple lipomatosis--a rare cause for small bowel intussusception. N Z Med J. 2007;120:U2876. [PubMed] |
| 19. | Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 171] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 20. | Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 235] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
P- Reviewers Tong WD, Ricci G, Valdastri P S- Editor Wen LL L- Editor Cant MR E- Editor Li JY